Submitted:
10 October 2023
Posted:
11 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. The conceptual foundation of research
3. Methods
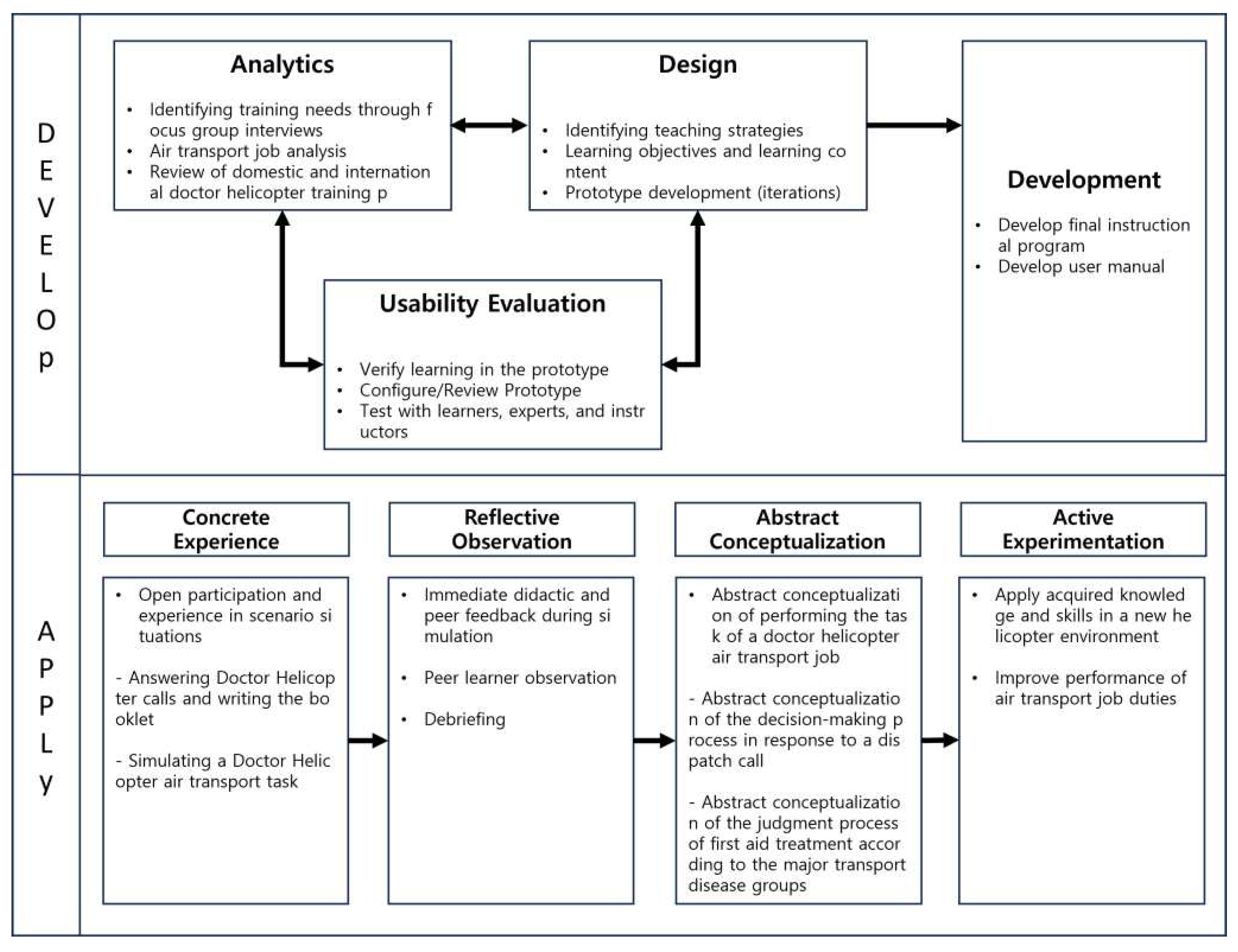
3.1. Development of a Training Program for Doctor Helicopter Air Transport Work
3.2. Applying the Doctor Helicopter Air Transport Work Training Program
3.2.1. Research Design and Research Hypothesis
3.2.2. Research subjects
3.2.3. Research Tools
3.2.4. Data Collection
3.2.5. Data analysis
3.3. Ethical considerations
4. Results
4.1. Developed a training program for doctor helicopter air transport work
4.1.1. Analysis phase
- Training Needs Analysis
- 2.
- Job Analysis of Doctor Helicopter Air Transfer Work
4.1.2. Initial Prototype Design and Usability Evaluation
- Revised PrototypeⅠ and First Usability Evaluation
- 3.
- Revised Prototype I and Second Usability Evaluation
4.1.3. Develop the final training program (Doctor Helicopter Transport Training Program: Dr. HTTP)
4.2. Applying the Doctor Helicopter Air Transport Work Training Program
4.2.1. Performing Dr. HTTP
4.2.2. Evaluation of Dr. HTTP
- 1.
- General Characteristics of the Recipients
- 4.
- Hypothesis Testing
5. Discussion
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Center, C.E.M. 2013 Emergency Patient Air (Helicopter) Transportation Support Project. Available online: file:///C:/Users/user/Downloads/2013%EB%85%84%20%EC%9D%91%EA%B8%89%ED%99%98%EC%9E%90%20%ED%95%AD%EA%B3%B5(%ED%97%AC%EA%B8%B0)%20%EC%9D%B4%EC%86%A1%EC%A7%80%EC%9B%90%20%EC%82%AC%EC%97%85%20%EA%B2%B0%EA%B3%BC%EB%B3%B4%EA%B3%A0%EC%84%9C[20150310145909]%20(3).pdf (accessed on September 25).
- Zhang, M.; Zhang, Y.; Qiu, Z.; Wu, H. Two-Stage Covering Location Model for Air–Ground Medical Rescue System. Sustainability 2019, 11, 3242. [Google Scholar] [CrossRef]
- Choi, H.J.; Kim, H.I. Introduction and characteristics of helicopter emergency medical services. Journal of the Korean Medical Association/Taehan Uisa Hyophoe Chi 2020, 63. [Google Scholar] [CrossRef]
- Kim, T.-y.; LEE, S.-A.; Park, E.-C.; Huh, Y.; Jung, K.; Kwon, J.; Moon, J.; Kim, J.; Kim, J.; Hwang, K. Effectiveness of the trauma team-staffed helicopter emergency medical service. Health policy and management 2018, 411–422. [Google Scholar]
- Hennelly, D.; Deasy, C.; Jennings, P.; O'Donnell, C.; Masterson, S. The Development of Helicopter Emergency Medical Services in the Republic of Ireland. Air Medical Journal 2023, 42, 150–156. [Google Scholar] [CrossRef]
- Bronfman, A.; Beneventti G, D.; Alvarez, P.P.; Reid, S.; Paredes-Belmar, G. The Casualty Stabilization–Transportation Problem in a Large-Scale Disaster. Sustainability 2022, 14, 621. [Google Scholar] [CrossRef]
- Strohmandl, J.; Tomek, M.; Molnár, V.; Jakubčeková, J.M.; Fedorko, G.; Maláková, S. Using travel times for optimization numbers of medical rescue service points—case study from Slovakia. Sustainability 2020, 13, 207. [Google Scholar] [CrossRef]
- Ruan, J.; Chan, F.T.; Zhao, X. Re-planning the intermodal transportation of emergency medical supplies with updated transfer centers. Sustainability 2018, 10, 2827. [Google Scholar] [CrossRef]
- Lee, M.; Ahn, Y.M.; Cho, I.; Sohn, M.; Lee, M.; Ahn, Y.; Cho, I.; Sohn, M. Effectiveness of Simulation Integrated with Problem Based Learning on Clinical Competency and Self-efficacy in Nursing Students. Child Health Nursing Research 2014, 20, 123–131. [Google Scholar] [CrossRef]
- Center, C.E.M. Collective training for emergency medical helicopter occupants. Available online: https://edu.nemc.or.kr/main.do# (accessed on.
- Lee, Y.H.; Kim, B.S. Applications of experiential learning theory to graduate medical education. Korean Medical Education Review 2009, 11, 11–20. [Google Scholar] [CrossRef]
- Lim, C.; Song, Y.; Hong, S.; Park, C. A study on the application and improvement of the Rapid Prototyping to Instructional Systems Design (RPISD) model. Journal of Educational Technology 2020, 36, 589–617. [Google Scholar] [CrossRef]
- Zemke, R.; Rossett, A. A hard look at ISD. Training 2002, 39. [Google Scholar]
- Lim, C.; Kim, M.; Kim, Y. A developmental study on the paper-based rapid prototyping methodology for Web-based Instruction. Journal of Educational Technology 2005, 21, 3–28. [Google Scholar] [CrossRef]
- Kolb, D.A. Experiential learning: Experience as the source of learning and development; FT press: 1984.
- Kim, J. A Qualitative Study on Self-directed Learning Process In the Enterprises : Based on Kolb's.
- Experiential Learning Theory. Hanyang University, 2021.
- Su, C.-H.; Cheng, T.-W. A sustainability innovation experiential learning model for virtual reality chemistry laboratory: An empirical study with PLS-SEM and IPMA. Sustainability 2019, 11, 1027. [Google Scholar] [CrossRef]
- Hsu, T.-C.; Abelson, H.; Lao, N.; Chen, S.-C. Is it possible for young students to learn the AI-STEAM application with experiential learning? Sustainability 2021, 13, 11114. [Google Scholar] [CrossRef]
- Chen, C.-C. Effects of flipped classroom on learning outcomes and satisfaction: An experiential learning perspective. Sustainability 2021, 13, 9298. [Google Scholar] [CrossRef]
- Urquidi-Martín, A.C.; Tamarit-Aznar, C.; Sánchez-García, J. Determinants of the effectiveness of using renewable resource management-based simulations in the development of critical thinking: An application of the experiential learning theory. Sustainability 2019, 11, 5469. [Google Scholar] [CrossRef]
- Hertzog, M.A. Considerations in determining sample size for pilot studies. Research in nursing & health 2008, 31, 180–191. [Google Scholar]
- Welfare, M.o.H.a. Basic and detailed guidelines for emergency medical helicopters; 2016; pp. 1-110.
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. biometrics 1977, 159–174. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and quantification of content validity. Nursing research 1986, 35, 382–386. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. The content validity index: are you sure you know what's being reported? Critique and recommendations. Research in nursing & health 2006, 29, 489–497. [Google Scholar]
- Lee, J.I.; Lee, K.H.; Cha, K.C.; Cha, Y.S.; Kim, O.H.; Kim, H.; Hwang, S.O. Effective medical training courses for medical helicopter crews in South Korea. Journal of The Korean Society of Emergency Medicine 2013, 24, 353–361. [Google Scholar]
- Lim, C.-I.; Yeon, E.-K. Corporate Education Program Development and Teaching System Design; Education Science History: Paju, Republic of Korea 2015. [Google Scholar]
- Kim, E.-H.; Kim, K.-H.; Bae, K.-E. Development of Online Continuing Education Courses on National Health Examination for Community Health Nurses: Using the Rapid Prototyping Method. Journal of Korea Academia-Industrial cooperation Society 2019, 20, 250–263. [Google Scholar]
- Park, J.-J. The future of flexible learning and emerging technology in medical education: reflections from the COVID-19 pandemic. Korean Medical Education Review 2021, 147–153. [Google Scholar] [CrossRef]
- Ku, J.-H.; Choi, W.-S. Development and Application of Blended Learning Strategy for Collaborative Learning. Journal of the Korean Institute of industrial educators 2009, 34, 267–285. [Google Scholar]
- Park, S. A development and an analysis of effectiveness of a blended learning program for enhancing parental efficacy. Soongsil University, 2014.
- Driscoll, M. Blended learning: Let’s get beyond the hype. E-learning 2002, 1, 1–4. [Google Scholar]
- Eryilmaz, M. The effectiveness of blended learning environments. Contemporary Issues in Education Research (CIER) 2015, 8, 251–256. [Google Scholar] [CrossRef]
- Lee, H. A Study on Practical Plans for Systematic Instruction in General Education at University Level. Korean Journal of General Education 2013, 7, 343–376. [Google Scholar]
- Lee, H.; Shin, S. Effects of elementary school health teachers' COVID-19 knowledge and resilience on their performance at infection control. Journal of Korean Public Health Nursing 2021, 35, 297–309. [Google Scholar]
- You, H.; Yang, B. The effects of virtual reality simulation scenario application on clinical competency, problem solving ability and nursing performance confidence. J. Korea Acad. Industr. Coop. Soc 2021, 22, 116–126. [Google Scholar]
- Lavelle, M.; Reedy, G.B.; Simpson, T.; Banerjee, A.; Anderson, J.E. Interprofessional teamwork for managing medical deterioration in pregnancy: what contributes to good clinical performance in simulated practice? BMJ Simulation & Technology Enhanced Learning 2021, 7, 463. [Google Scholar]
- Koukourikos, K.; Tsaloglidou, A.; Kourkouta, L.; Papathanasiou, I.V.; Iliadis, C.; Fratzana, A.; Panagiotou, A. Simulation in clinical nursing education. Acta Informatica Medica 2021, 29, 15. [Google Scholar] [CrossRef]
- Zulkosky, K.; Minchhoff, D.; Dommel, L.; Price, A.; Handzlik, B.M. Effect of repeating simulation scenarios on student knowledge, performance, satisfaction and self-confidence. Clinical Simulation in Nursing 2021, 55, 27–36. [Google Scholar] [CrossRef]
- Goldshtein, D.; Krensky, C.; Doshi, S.; Perelman, V.S. In situ simulation and its effects on patient outcomes: a systematic review. BMJ Simulation & Technology Enhanced Learning 2020, 6, 3. [Google Scholar]
- Jeffries, P.R.; Rizzolo, M.A. Summary report: Designing and implementing models for the innovative use of simulation to teach nursing care of ill adults and children: A national, multi-site, multi-method study. Retrieved November 2006, 10, 2011. [Google Scholar]
- Scherer, Y.K.; Foltz-Ramos, K.; Fabry, D.; Chao, Y.-Y. Evaluating simulation methodologies to determine best strategies to maximize student learning. Journal of Professional Nursing 2016, 32, 349–357. [Google Scholar] [CrossRef] [PubMed]
| Step | Research Procedures | Research | ||
| Step 1 Program Development |
Analytics | ⦁Training needs analysis ⦁Job analysis of air transportation ⦁Domestic and international doctor helicopters Training Program Review |
⦁Doctor chopper for first responders Check your training needs ⦁Detailed Guidelines for Doctor Helicopter Air Transfer Job Analysis ⦁Review domestic and international helicopter training programs |
|
| Prototype design and Usability Evaluation |
⦁Initial prototype development and Feasibility assessment |
⦁Review expert content validity through interviews | ||
| ⦁Development of revised Prototype I and primary usability assessments |
⦁Usability evaluation (CVI) | |||
| ⦁Revised Prototype ⅡDevelopment and secondary usability assessments |
⦁Usability assessment (Tools - Principles of Instructional Design, Principles of Organization) |
|||
| Programs Development |
⦁Define the final training program ⦁User manual development |
⦁Develop the final training program (Dr. HTTP)* | ||
| Step 2 Apply the program |
Programs Perform |
⦁Newly developed training programs Apply |
⦁Pilot test 11 people |
⦁Provide scenarios ⦁Instructor and peer feedback, Debriefing ⦁Theory lectures, step-by-step labs |
| Programs Evaluation |
Evaluate training program effectiveness | ⦁Pre- and post-assessment of air transportation job performance | ||
| Group | Pre-test | Moderation Apply the program |
Post-test |
|---|---|---|---|
| Experimental group |
E1 | X | E2 |
| Day | Session | Topics | Contents | Minutes | Progress | Methods |
|---|---|---|---|---|---|---|
| 1 day Tea |
1 | Orientation and Safety Eduation |
[Training Program Information] ⦁ Training objectives and methods ⦁ About the instructor ⦁ An introduction to course delivery ⦁ Introduction to the Dr. Helicopter business overview |
30* | Online | Lectures |
| [Safety training and infection control] ⦁ Introduction to Dr. Helicopter Guidelines ⦁ An Introduction to Aeronautical Physiology for Drone ⦁ Managing medical devices to prevent infectious diseases ⦁ Onsite infection control to prevent infectious diseases ⦁ Managing boarding of asymptomatic (suspected) patients to prevent infectious diseases | ||||||
| 2 | Dispatch steps Ⅰ |
[Dispatch Simulation 1. Dispatch Reception]. ⦁ Scenario provision Virtual scenario provision Learners write down the dispatch receipt Instructors provide feedback on the receipt records written by learners (whether all necessary elements for dispatch reporting have been understood) ⦁ Guidance on dispatch request receipt and points to note during dispatch |
50* | off Line |
Team Activities |
|
| 3 | Dispatch steps Ⅱ |
[Dispatch Simulation 2. Preparation for Treatment: Medications and Medical Equipment] ⦁ Gathering medications and medical equipment for the dispatch phase at the hospital based on a secondary scenario ⦁ Receive feedback from instructors and peers on their performance* |
50* | off Line |
Team Activities | |
| 4 |
On-site medical care Ⅰ |
[Learning about key boarding patient populations (1)]: Primary boarding patient population 1. severe trauma 2. acute cerebral hemorrhage 3. acute stroke 4. acute myocardial infarction 5. other emergency-like symptoms (Shock, respiratory problems) Provide a standardized care manual (classroom) |
30 | Online | Lecture | |
| 5 |
On-site medical care Ⅱ |
[Learning about key boarding patient populations (2)] ⦁ Q&A and feedback for online courses ⦁ Role as a prehospital emergency care provider* |
30 | off Line |
Lecture | |
| 6 | Field boarding and transport | [Learning about on-site boarding] ⦁ Learn about movement considerations for patient boarding: Practice lifting and moving patients ⦁ Share patient transfer stories ⦁ Guide what to expect when transferring patients |
50* | off Line |
Team Activities Lecture |
|
| 7 | Patient Takeover |
[Performance Assessment: Emergency Medical Helicopter Simulation] ⦁ Conduct performance assessments to evaluate the learner's performance by conducting a dispatch-to-handoff phase. ⦁ Rubrics to help instructors evaluate observations, and worksheets to encourage learners to self-assess. ⦁ Instructor-observed assessment during performance and, for learners, self-assessment after performance is complete |
50 | off Line |
Perform Evaluation |
|
| 8 | Flight Exit |
[End of Operation and Reflection] ⦁ Documentation and recordkeeping for the end of life phase ⦁ How to Use the Flight Management System ⦁ Create and submit an action plan based on your instructor's observations and self-assessment. ⦁ Full discussion and lecture evaluations |
50 | off Line |
Team Activities |
| Variables | Categories | N (%) | M±SD |
| Gender | Male | 5 (45.5) | |
| Femal | 6 (54.5) | ||
| Age (years) | 28.91±4.35 | ||
| Occupation | Nurse | 4(36.4) | |
| First Aid | 7 (63.6) | ||
| Education | Bachelor of Science | 6 (54.5) | |
| Bachelor's | 3(27.3) | ||
| Master of Arts Award | 2(18.2) | ||
| Total Clinical Experience (months) | 53.73±50.51 | ||
| Emergency Department Clinical Experience (months) | 43.82±30.32 | ||
| HEMS* Training Needs | Yes | 11(100) |
| Contents | M±SD | Z | p | |||
|---|---|---|---|---|---|---|
| Pre-Training | After Training | Difference | ||||
| 1 | I can conduct a questionnaire and physical examination based on the patient's primary symptoms. | 2.64±0.81 | 3.36±0.50 | -.72±0.78 | -2.30 | .021 |
| 2 | I can plan interventions appropriate to the patient's condition in air transport. | 2.36±0.51 | 3.27±0.47 | -.90±0.53 | -2.88 | .004 |
| 3 | I can execute pre-hospital care according to the intervention plan in air transport. | 2.64±0.81 | 3.09±0.54 | -.45±0.68 | -1.89 | .059 |
| 4 | I can evaluate the outcomes of interventions tailored to the patient's condition in air transport. | 2.45±0.69 | 3.09±0.70 | -.63±0.67 | -2.33 | .020 |
| 5 | I am able to consult and liaise with other healthcare teams during air transport operations. | 2.36±0.81 | 3.45±0.52 | -1.09±0.83 | -2.81 | .005 |
| 6 | I can establish and maintain cooperation with other healthcare teams in air transport. | 2.45±0.69 | 3.45±0.52 | -1.00±0.63 | -2.81 | .005 |
| 7 | I am able to hand over patient information during air transport. | 3.18±0.41 | 3.91±0.30 | -.72±0.46 | -2.83 | .005 |
| 8 | I can act as a researcher to build the scientific evidence base for pre-hospital care interventions. | 1.73±0.47 | 2.55±0.69 | -.81±0.75 | -2.46 | .014 |
| 9 | I can act as an educator in providing education to patients, communities, and other providers. | 2.27±0.79 | 2.82±0.75 | -.54±0.82 | -1.90 | .058 |
| 10 | I can continue to participate in the education and training of prehospital emergency care providers to maintain my expertise. | 2.64±0.67 | 3.36±0.67 | -.72±0.78 | -2.27 | .023 |
| 11 | I can collaborate with other agencies in air transport operations to ensure scene control, mass casualty triage, and resource utilization. | 2.18±0.75 | 3.09±0.70 | -.90±0.70 | -2.64 | .008 |
| 12 | I can act as an on-site expert in scene control, mass casualty triage, and resource utilization during air transport operations. | 2.73±1.20 | 2.82±0.75 | -.09±1.04 | -.31 | .763 |
| 13 | I can act as a counselor to enhance communication between agencies and facility personnel in air transport operations. | 2.82±0.87 | 3.36±0.67 | -.54±0.68 | -2.12 | .034 |
| 14 | I can collaborate with other healthcare providers to perform and improve the care provided to patients during air transport operations. | 2.45±0.82 | 3.18±0.60 | -.72±0.78 | -2.27 | .023 |
| 15 | I can act as an advocate to protect patient rights and promote recovery and health during air transport operations. | 2.27±0.79 | 2.82±0.75 | -.54±0.68 | -2.12 | .034 |
| Total Score | 37.18±8.34 | 47.63±7.20 | -10.45±6.68 | -2.94 | .003 | |
| Contents | M±SD | Z | p | |||
|---|---|---|---|---|---|---|
| Pre-Training | After Training |
Difference | ||||
| 1 | Gather patient information and confirm airworthiness. | 1.68±0.47 | 1.95±0.22 | -.27±0.55 | -2.12 | .034 |
| 2 | Share the decision to dispatch and prepare the necessary first aid kit and medical equipment. | 1.63±0.49 | 1.91±0.29 | -.27±0.45 | -2.44 | .014 |
| 3 | Use in-flight communications equipment to share additional information about the patient. | 1.00±0.87 | 1.23±0.69 | -.22±1.26 | -.86 | .390 |
| 4 | Share patient care plan and follow physician instructions. Perform preparatory procedures for patient care as directed by the physician. | 1.27±0.55 | 1.77±0.43 | -.50±0.74 | -2.67 | .008 |
| 5 | Select first aid kit and necessary medical equipment, safely transport to the patient. | 1.59±0.50 | 2.00±0.00 | -.40±0.50 | -3.00 | .003 |
| 6 | Check the patient's condition and apply medical treatment, utilizing medical equipment. | 1.72±0.46 | 1.86±0.35 | -.13±0.56 | -1.14 | .258 |
| 7 | Perform necessary treatments as directed by a physician. | 1.55±0.51 | 2.00±0.00 | -.45±0.50 | -3.16 | .002 |
| 8 | Collaborate with rescuers to move the patient to a mobile trolley (stretcher). | 1.50±0.51 | 1.96±0.22 | -.45±0.50 | -3.16 | .002 |
| 9 | Direct patient movement and determine direction of travel. | 1.13±0.64 | 1.77±0.53 | -.63±0.84 | -2.84 | .005 |
| 10 | Organize applied medical treatment and medical equipment to safely load the patient. | 1.55±0.51 | 1.91±0.29 | -.36±0.65 | -2.31 | .021 |
| 11 | Check for medical equipment and debris, organizing the medical equipment and first aid kit. | 1.09±0.97 | 1.27±0.55 | -.18±1.22 | -.79 | .426 |
| 12 | Check the patient's vital signs and consciousness and apply patient monitoring equipment. | 1.73±0.46 | 2.00±0.00 | -.27±0.45 | -2.45 | .014 |
| 13 | Implement patient safety measures and administer medical treatment using medical equipment. | 1.50±0.51 | 1.96±0.22 | -.45±0.59 | -2.89 | .004 |
| 14 | Perform necessary treatments as directed by the physician. | 1.68±0.47 | 1.95±0.22 | -.27±0.55 | -2.12 | .034 |
| 15 | Communicate patient status and continuously check for any additional changes. | 1.59±0.50 | 1.91±0.29 | -.31±0.56 | -2.33 | .020 |
| 16 | Safely move the patient using a stretcher and put away medical supplies and equipment. | 1.32±0.47 | 2.00±0.00 | -.68±0.47 | -3.87 | .000 |
| 17 | Provide basic patient information, including demographics, treatment, and current condition to emergency medical center staff. | 1.50±0.50 | 1.95±0.21 | -.45±0.50 | -3.16 | .002 |
| 18 | Access the flight management system and complete the air transport logbook. | 1.41±0.50 | 2.00±0.00 | -.59±0.50 | -3.61 | .000 |
| 19 | Check and replenish consumed medicines, medical supplies, and oxygen. | 1.46±0.51 | 1.95±0.22 | -.50±0.51 | -3.32 | .001 |
| 20 | Implement post-flight infection control and check the charging and operating status of medical equipment. | 1.54±0.51 | 2.00±0.00 | -.45±0.50 | -3.16 | .002 |
| Total Score | 29.81±2.63 | 37.72±1.49 | -7.91±3.99 | -2.94 | .003 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





