Introduction
Women with high-grade cervical intraepithelial neoplasia (CIN 2-3) should be treated to prevent progression to cancer (1) . There are different treatment modalities for the transformation zone, which can be ablative techniques (cryotherapy or thermal ablation) or excision techniques (large loop excision of the transformation zone or conization with a cold knife); The choice of treatment depends on the type of transformation zone, the size and location of the lesion (2) .
Large loop excision of the transformation zone (LLETZ) aims to remove the entire transformation zone including the entire lesion so that it can be evaluated histologically (3) . Its advantages are to allow histological confirmation and assessment of surgical margins, as well as to rule out stromal invasion (4) . Its drawbacks derive from the difficulty in histological assessment of the margins due to thermal damage (4) .
The transformation zone (ZT), according to the International Federation of Cervical Pathology and Colposcopy in 2011 (IFCPC), is classified as ZT type 1, when the transformation zone is located in the exocervix and is completely visible. The TZ type 2 is defined as one that is located in the exocervix, but is partially introduced into the endocervical canal, however, it is visible in its entirety. The TZ type 3 is one located in the endocervical canal and is not completely visible (5) .
According to the type of transformation zone, the most appropriate type of excision can be chosen, with the aim of obtaining complete excision of the lesion. According to the modified IFCPC classification, 3 types of excision are included: Type 1, if the resection of a type 1 transformation zone is performed, the diathermic loop should not include the endocervical canal or exceed 8 mm in depth; Type 2, if the resection is from a type 2 transformation zone, 10 to 15mm of the endocervical canal is resected; Type 3, when the resection is from a type 3 transformation zone, the endocervical canal is extracted to a depth of 15 to 25mm (3) .
There is controversy regarding the appropriate depth and dimensions of the conization piece and few studies have compared the types of resection with the possibility of recurrence. The objective of this study is to evaluate the relationship between the type of conization according to the IFCPC, the volume and dimensions of the cone (Length, width and perimeter), with the persistence/recurrence of CIN 2-3, presence of affected margins in the conization piece performed using a diathermic loop and post-cone HR-HPV positivity.
Material and Methods
This study included patients with a histological diagnosis of CIN 2-3, in the conization sample, who were treated in the Gynecology Service of the Bellvitge University Hospital, Hospitalet de Llobregat, Barcelona, from the Cervical Pathology Unit. The patient inclusion period was from January 1996 to December 2016. Women had at least one follow-up control after LLETZ.
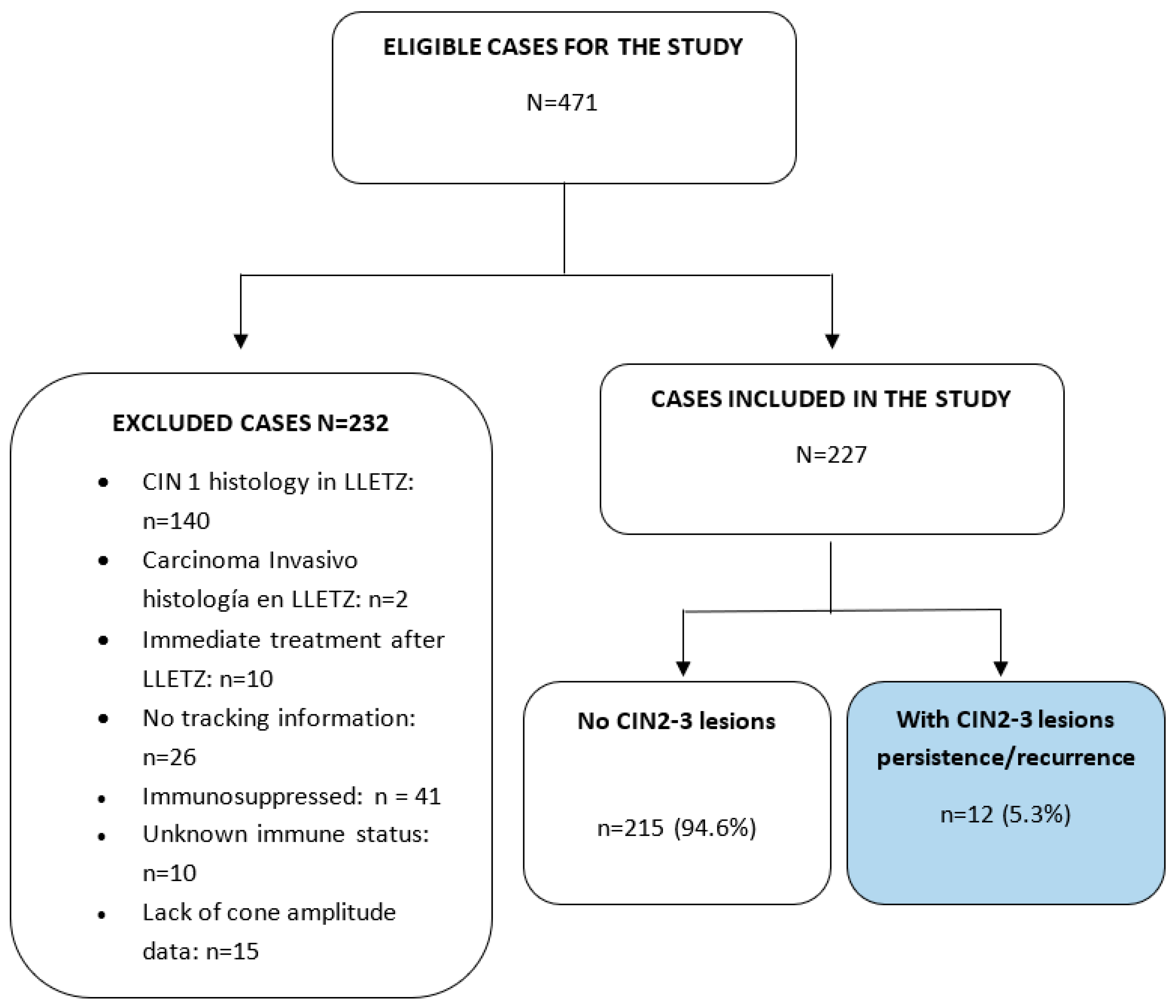
(n = 10), were excluded. immunosuppressed (n = 41), unknown immune status (n = 10), and missing channel amplitude data (n = 2). Finally, of the 471 eligible cases, 227 patients (51.4%) were included. The inclusion/exclusion algorithm is shown in
Figure 1.
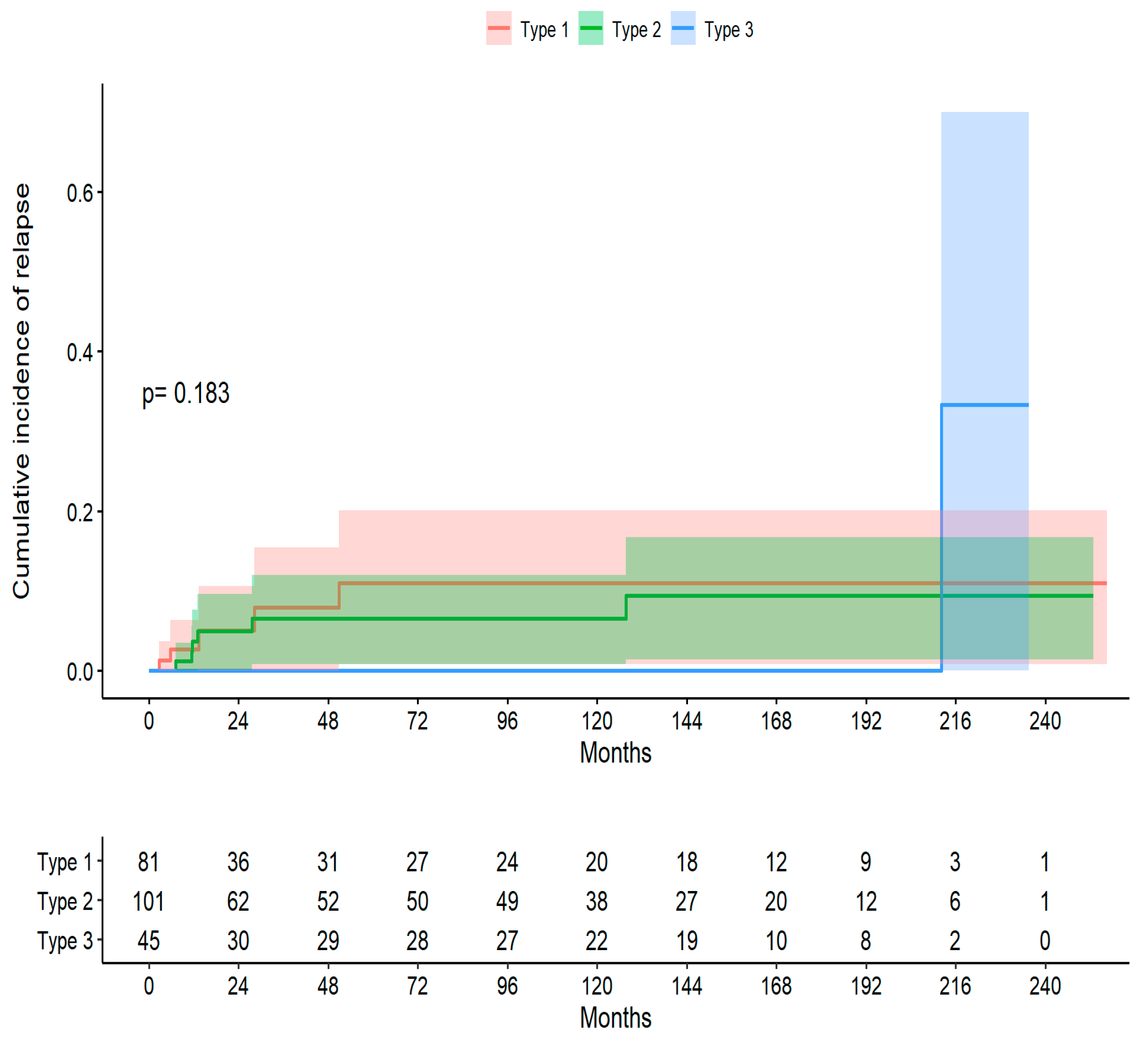
The Log-Rank Test indicates that there is no evidence to reject that the survival curves according to treatment are different (p-value p= 0.183).
Patient data were appropriately anonymized and protected in accordance with national regulations. This study was approved by the Clinical Research Ethics Committee of the Bellvitge University Hospital: Minutes 03/19, dated 02-14-2019.
Surgical procedure
Conization was performed using a diathermic loop, after applying local paracervical and Lugol anesthesia to the surface of the cervix. The diameter of the loop was chosen according to the colposcopic appearance of the lesion to be removed. Type 1 excision was performed, when a type 1 transformation zone was found, Type 2 resection, if the transformation zone was type 2, and Type 3 resection, when the transformation zone was type 3. In women over 35 years of age or With a squamocolumnar junction not visible, a second pass of the endocervical canal (top hat) was made with a 5 mm loop. Hemostatic coagulation was performed with a sphere electrode. The samples were oriented with a point at the 12 o'clock position.
Follow-up
Follow-up was carried out 6 and 12 months after conization, using cervical cytology and colposcopy. The HPV study was performed after 6 months. If the surgical margins were positive, the first control visit was after 3 months.
Patients with abnormal cytology results, suspicious colposcopy findings, or positive HPV results had a cervical biopsy. Patients with two consecutive negative Pap tests and a normal colposcopy were sent for annual gynecological control.
Ectocervical and endocervical smears were obtained using the conventional Papanicolaou staining method. Cytological findings were evaluated according to the 1989 or 2001 Bethesda System terminology (6) .
Colposcopy was performed with a binocular Carl Zeiss colposcope (Germany). 5% acetic acid was initially applied to the cervix with a cotton swab and later Lugol . Women with abnormal cytology (ASC-US or higher) or a positive HR-HPV test underwent colposcopy and biopsy. An endocervical curettage was performed if the transformation zone was type 3.
The samples for the HPV test were processed with the test Digene (Gaithersburg, MD, USA), which involves signal-amplified hybridization capture using chemiluminescent detection of HR-HPV type-specific RNA probe cocktail ( 16 , 18 , 32 , 34 , 36 , 39, 45, 51, 52, 56, 58, 59, 68). The light emitted from the conjugated hybrid antibody was measured by a luminometer as relative light units (RLU). When the RLUs were equal to or greater than the mean of a positive control (RLU) (1.0 pg / mL ), the sample was scored as positive.
Persistent/recurrent disease criteria
Recurrence was defined as CIN 2-3 by endocervical biopsy or curettage. Affected patients with residual/recurrent disease underwent second surgical treatment.
Volume of the operating piece
The volume was estimated according to the formula proposed by Carcopino (7) the circumference corresponds to the external circumference of the cone, the length represents the distance from the external/distal margin to the internal/proximal margin of the open sample and the thickness was defined as the distance from the stromal margin to the surface of the epithelium. The volume of the cone was calculated using the hemielipsoid formula :
Volume = (1/2) × (4/3) × π × length × (circumference/2π) × thickness
Data analysis
A case form was developed in ACCESS and data were entered prospectively. The variables were analyzed according to the type of variable and summarized in tables. The nominal categorical variables were described with the absolute frequency of cases, and the percentage distribution with respect to the total by category and the number of missing data. Continuous variables with normal distribution were described by the number of cases, the mean, the standard deviation and the number of missing data. Continuous variables that did not present a normal distribution were described by the number of cases, the median, the first and third quartiles , and the number of missing data. For continuous variables with normal distribution, the Student T test was used ; For continuous variables that did not follow a normal distribution, the Kruskall -Wallis test was used, and for categorical variables, Fisher's exact test was used to compare percentages between patients.
Time to recurrence was assessed with the Kaplan-Meier method. The log- rank test was used to compare the hazard ratio between the study groups. The Cox proportional hazards model was used to determine risk variables. Incidences and 95% confidence intervals (CI) were calculated.
Taking the patients as the unit of analysis, the probability of recurrence was estimated taking into account CIN 2-3 and CIN 1. The date of the first conization and the end date until the time of the last follow-up or follow-up were taken as the baseline moment. recurrence CIN 2-3 or CIN 1. Using a Cox regression model, the cumulative complication incidence function was calculated taking into account CIN 2-3 and CIN 1.
The role of CIN 2-3 persistence as a competing risk for CIN2-3 recurrence was studied using the Fine and Gray models. The statistical program R in version 3.6.1 for Windows was used to process the data and analyze it .
Figure 1.
ALGORITHM FOR INCLUSION-EXCLUSION OF PATIENTS IN THE STUDY..
Figure 1.
ALGORITHM FOR INCLUSION-EXCLUSION OF PATIENTS IN THE STUDY..
Results
The mean age at diagnosis in type 1 treatment was 36.3 ± 11.2 years, in Type 2 the age was 36.7 years ± 9.9 years and in the Type 3 technique the mean age was 40 .8 ± 10.8 years, with a value of P = 0.051. A total of 54.6% of patients (124/227) had free margins in the LLETZ sample and patients with affected surgical margins were 31.3% (71/227). In 13.2% of patients (30/227) the resection margins were uncertain. Of the total group of women with positive margins, in the Type 1 technique 38.3% (31/81) were affected, in Type 2 29.7% (30/101) and in the Type 3 technique the margins 22.2% (10/45) were affected, a difference that was significant (p 0.001). The median volume according to the Carcopino formula, of the total group was 0.57cc, in the Type 1 technique the median was 0.45, in the Type 2 technique the volume was 0.66cc and in the Type 3 treatment the median volume was 0.69cc, these differences being significant (P=0.012). The median total perimeter for the Type 1 technique was 11.4cm, for the Type 2 treatment it was 11.0cm and for the Type 3 treatment it was 11.2 (P=0.96). The depth of the cone in the type 1 technique was 0.61cm, in the Type 2 technique it was 0.96cm and in the type 3 technique it was 1.94mm, with a significant statistical difference (P<0.001). Endocervical canal widening was performed in 91.1% (41/227) of women undergoing Type 3 treatment. (
Table 1).
The pre-cone HR-HPV result in the total group was positive in 62.1% (141/227), there was no significant difference in the proportion of positive or negative test results between the three techniques (p 0.752). The result of the first HR-HPV post LLETZ in the total group was positive in 16.8% (38/227) and negative in 58.4% (132/227), in the Type 1 treatment the HR-HPV was positive in 19 .8% (16/81), in the Type 2 technique it was positive in 18.0% (18/101) and in the Type 3 technique it was positive in 8.89% (4/45) without significant difference (P =0.457). The first RLU HPV post-LLETZ in the Type 1 technique was negative in 51.9% (42/81), in the Type 2 technique it was negative in 53.5% (54/101) and in the Type 3 technique It was negative in 64.4% (29/45) (
Table 2).
In the present study, persistence/recurrence of CIN2-3 was observed in 12 cases (5.28%), The cure proportion was 94.72% with the diathermic loop therapeutic procedure. This cure reached 99.17% in completely excised cases, with free margins. Recurrence was significantly associated with margin status, there were 4 recurrences in patients with positive margins (HR 7.60 95% CI 0.84 to 68.4) and 6 recurrences in patients with uncertain margins (HR 35.3 CI 95 % 4.14 to 301). The volume in women without recurrence had a median of 0.57cc, while in patients with recurrence the median volume was 0.62cc, without significant difference (p 0.441). The other dimensions: total perimeter, width/2, depth and canal expansion were not associated with the risk of persistence/recurrence (P>0.05) (
Table 3).
The overall mean age of the patients was 37.4 years, being 37.0 years in women without recurrence, and 43.9 years in the group with CIN2-3 recurrence (p 0.064). The result of the first HR-HPV in the non-recurrence group was negative in 80.8% (131/162) of women and positive in 19.2% (31/162); while in the recurrence group the HR-HPV was negative in 12.5% (1/8) of patients and positive in 87.5% (7/8); with significant difference (HR 27.18. 95% CI 3.41 to 227). The result of the first RLU HPV post LLETZ in the non-recurrence group was negative in 82.6% (124/150), it was positive in the category from 1 to 100 in 14% (21/150) and in the RLU category > 100 was positive in 3.3% (5/150) of patients; In the recurrence group, the HPV RLU was negative in 12.5% (1/8), it was positive in the 1 to 100 category in 25.0% (5/10) and in the RLU>100 category. was positive in 62.5% (5/8) of women, with statistical significance (HR 204, 95% CI 21.5 to 1940). In Type 1 treatment there were 6.17% (5/81) recurrences, in Type 2 treatment 5.94% (6/101) recurrences were observed and in Type 3 treatment 2.22% (1/45) were observed. ) of recurrences, but these differences in treatments did not have statistical significance (P=0.76) (
Table 4).
The median LLETZ volume was 0.61 cc in patients with HR-HPV negative and 0.49 cc in the group with a positive result, the total perimeter was 12.4 cm in women with HR-HPV negative and 13.6 cm in patients with a positive result, differences that were not significant. The positive result of HR-HPV post LLETZ was only statistically associated with Amplitude/2 (p 0.038), but depending on the type of treatment, in the Type 1 technique there were 19.8% (16/81) of positive tests, in the Type 2 technique was found 18.0% (18/100) and in the Type 3 treatment 8.89% (4/45) of positive HR-HPV tests were observed, without statistical significance (P=0.45) (
Table 5).
The median follow-up of the total group was 38.4 months (range 9.17 to 150 months), in type 1 treatment the median follow-up (Q1; Q3) was 16.92 (7.23; 108.32 ) months, of the 81 patients, 5 presented recurrences, at 36 months there were 46 censored and 4 recurrences were observed, the cumulative incidence being 0.08. In type 2 treatment, the median follow-up (Q1; Q3) was 70.05 (12.16; 151.82) months; of the 101 patients, 6 had recurrences; at 36 months, 12 were censored and 5 were observed. recurrences, with the cumulative incidence being 0.04. In type 3 treatment, the median follow-up (Q1; Q3) was 119.95 (11.73; 163.25) months, of the 45 patients, 1 had a recurrence, at 36 months there were 16 censored and 0 were observed. recurrences, with the cumulative incidence being 0.00 (
Table 6).
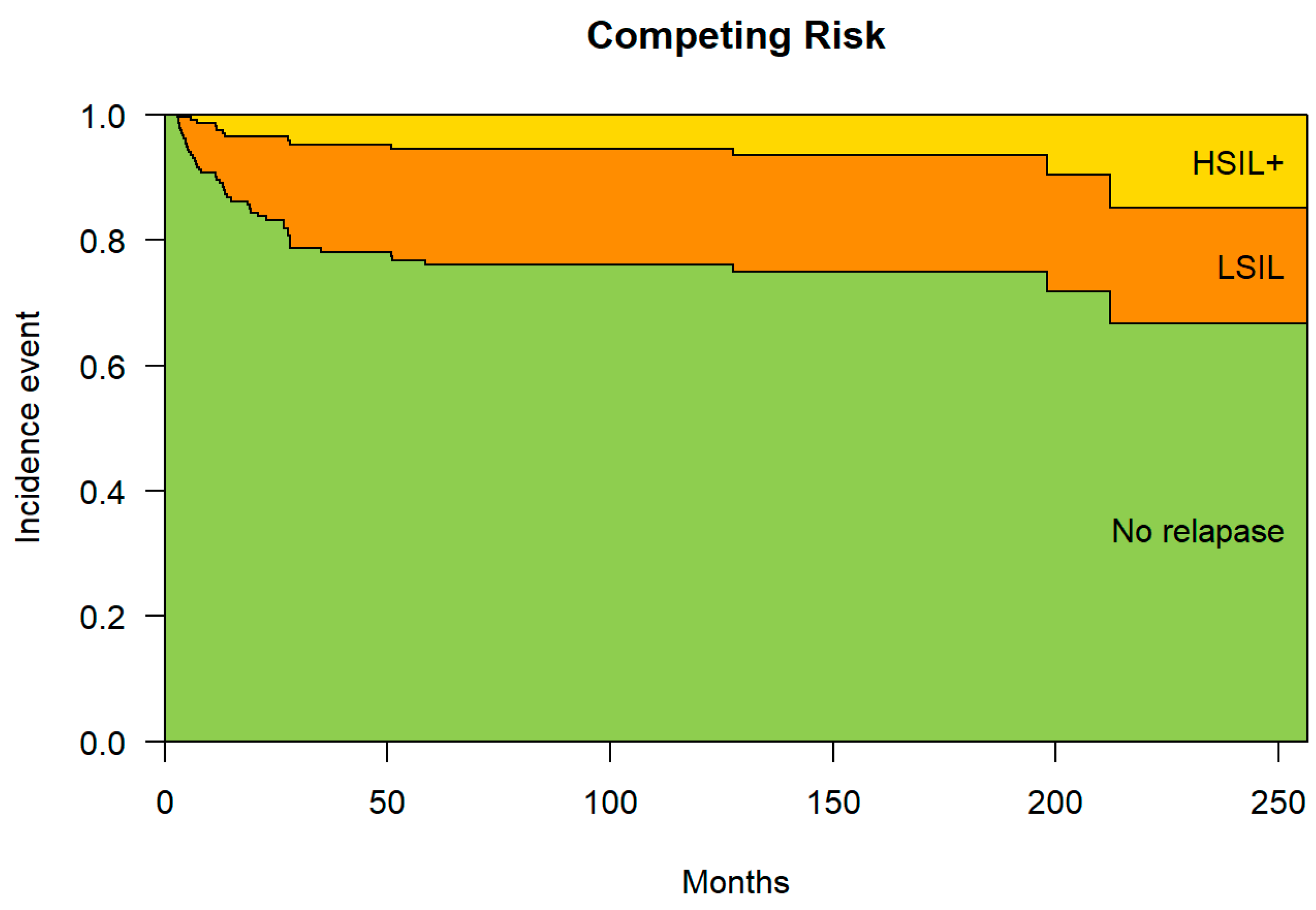
The median time to recurrence in the total group was 13.2 months (10.4; 33.9), in type 1 treatment it was 13.4 months (5.72; 28.2), in type 1 treatment 2 was 12.3 months (11.5; 24.0) and treatment type 3 was 212 months (212; 212). The probability of not presenting a recurrence at six months was 93.5%, the probability of presenting a CIN1 recurrence (LSIL) 5.6% and of presenting a CIN2-3 recurrence (HSIL) 0.9%. At 240 months, the possibility of not having a recurrence was 66.7%, and of having a C1N1 recurrence it was 18.5%, and of having a CIN2-3 recurrence it was 14.8%. Over time, the probability of non-recurrence decreases and the probability of recurrence increases at the expense of CIN1 and to a lesser extent CIN2-3 (
Figure 2).
Discussion and Comments
Extensive involvement of the endocervical margin after LLETZ by CIN2-3 is a strong predictor of residual disease (8) . Arbyn reported a risk of persistence/recurrence of 7.2% if only the exocervical margin was affected, 16.3% if the exocervical margin was involved. endocervical margin, but if both were affected the recurrence was 18.9% (1) . Type 1 treatment had 38.3% affected margins, Type 2 treatment had 29.7%, while Type 3 treatment reached 22.2% affected margins, however, persistence/recurrence in Type 1 treatment It was 6.17% (5/81), in Type 2 it was 5.94% (6/101) and in Type 3 it reached 2.22% (1/45), not all patients with affected margins recur. , but type 3 presented a lower proportion of affected margins and less recurrence. Alder (9) demonstrated that women with positive/uncertain margins had a higher risk of residual/recurrent CIN2-3 or worse than women with negative margins, and Lumbrano (10 ) reported persistence/recurrence in 24.8% of cases with positive margins vs 11.1% of cases with negative margins (P< 0.0001), therefore, recurrence is greater in women with affected margins.
The median total perimeter was similar between the three types of treatment, but the volume of the cone, the width/2 and the depth of the cone were greater in the Type 3 treatment than the other two techniques, which is related to the lower percentage of margins affected by type 3 treatment. Papoutsis (11) determined that for the prediction of positive margins the optimal cut for the volume of the cone was 2.1cc and for the depth of the cone the optimal cut was 1.0 cm but in In our study, the volume of Type 1 treatment was 0.45cc, in Type 2 technique it was 0.66 and in Type 3 treatment it was 0.69cc, this result being greater than the other two techniques, which determined a higher percentage of margins. free (71.1%) in the Type 3 treatment. Probably more important than the volume of the cone is the depth in determining the state of the margins, Kawano (12) estimated the optimal cut-off point was 15 mm when it was a single quadrant disease and 20 mm when 2 or more quadrants were affected.
The post-LLETZ HR-HPV result in Type 3 treatment was negative in 68.9% (31/45) of cases, higher than in Type 1 and Type 2 treatments, and also had the lowest percentage of post-cone positivity. of 8.8% (4/45), which could be explained by the greater volume and depth of the cones made with the Type 3 treatment, with an average of 1.9 cm, this removal of a greater amount of endocervical tissue could resecting the disease in its entirety and successfully eliminating the virus from the cervical tissue (13) , while in the Type 1 and Type 2 treatments, which were shallower, it is likely that not all of the HPV-infected tissue was removed and therefore both present a higher viral load in the RLU HPV control at 6 months (14) .
Persistence/recurrence was associated with the status of the affected surgical margin and especially with the uncertain margin (P<0.001), similar to what was described by Alder (10) who reported a significant association with the group of positive/uncertain margins. Recurrence was not associated with the volume or dimensions of the cone, similar to what was described by Chen (15) , who found no association with the perimeter, circumference or width of the surgical piece, because ultimately what matters is the state of the margin regardless of the other dimensions. The recurrence group had a greater volume than the non-recurrence group, but despite removing a greater amount of tissue, the patients had a greater proportion of persistence/recurrence, which could be explained by the nature of the more extensive lesion and more HPV genotypes. aggressive and also because the surgeon, upon colposcopically observing a larger lesion, performed a larger volume LLETZ (16) .
In our series, it was determined that the positive result of the first HR-HPV post LLETZ had statistical significance (p<0.001) in the association with the risk of persistent recurrence. These data coincide with Arbyn (1) who demonstrated that the result of HR - HPV Post-LLETZ HPV positivity predicts treatment failure more accurately than margin status. Huang (17) determined a greater recurrence of CIN2+ in patients with positive results for HR-HPV post LLETZ that reached 14.8% at 5 years, and Bogani (18) found that the persistence of positive HPV post LLETZ was the main predictive factor of CIN2+ regardless of HPV genotype. In our series, patients with viral load > 100 URL/ml post LLETZ had 204 times the risk of recurrence than women with viral load < 100 URL/ml, but Nam (19) found no association with post-LLETZ viral load , this load Viral infection may also be affected by the detection method, the sampling site, and by the number of epithelial cells in the sample.
The volume of the LLETZ, the total perimeter and the depth of the LLETZ specimen were not associated with post-cone HR-HPV positivity, only a significant association was found with the amplitude/2, perhaps because patients with more extensive lesions presented genotypes of more aggressive high risk. The Type 3 treatment type (8.89%) had the lowest percentage of HR-HPV positivity post LLETZ than the type 1 technique (19.8%) and the type 2 technique (18.0%). Chen (20) did not find difference significant in he LLETZ sample size between _ cluster persistent and _ non- persistent group , demonstrated that the persistence of positive HR-HPV in a 6-month follow -up visit was a risk factor for injuries high grade neoplastic persistent post- operative symptoms .
In conclusion, according to these results, Type 3 treatment would be the best resection method, because it has a lower chance of presenting persistent recurrence of CIN 2/3 at 240 months and a lower proportion of positivity for HR-HPV post LLETZ.
References
- Arbyn M, Redman CWE, Verdoodt F, Kyrgiou M, Tzafetas M, Ghaem-Maghami S, et al. Incomplete excision of cervical precancer as a predictor of treatment failure: a systematic review and meta-analysis. Lancet Oncol [Internet]. 2017;18(12):1665–79. Available from:. https://doi.org/10.1016/S1470-2045(17)30700-3. [CrossRef]
- Basu P, Taghavi K, Hu SY, Mogri S, Joshi S. Management of cervical premalignant lesions. Curr Probl Cancer [Internet]. 2018;42(2):129–36. Available from:. https://doi.org/10.1016/j.currproblcancer.2018.01.010. [CrossRef]
- NHSCSP. NHS Cervical Screening Program Colposcopy and Program Management NHSCSP Publication No. 20, 3rd Edition March 2016. NHS Cerv Screen Program [Internet]. 3rd Edition. 2016;(20):1–108. Available from: https://www.bsccp.org.uk/assets/file/uploads/resources/NHSCSP_20_Colposcopy_and_Programme_Management_(3rd_Edition)_(2).pdf.
- Torné Bladé A, AEPCC. SEGO Oncoguide: Prevention of cervical cancer. Clinical practice guidelines in gynecological and breast cancer. Spanish Association Patol Cerv and Colposc. 2014;1:1–56.
- Bornstein J, Bentley J, Bösze P, Girardi F, Haefner H, Menton M, et al. 2011 Colposcopic Terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol. 2012;120(1):166–72. [CrossRef]
- Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. J Am Med Assoc. 2002;287(16):2114–9. [CrossRef]
- Carcopino X, Mancini J, Prendiville W, Gondry J, Chevreau J, Lamblin G, et al. The Accuracy of Large Loop Excision of the Transformation Zone Specimen Dimensions in Determining Volume: A Multicentric Prospective Observational Study. J Low Genit Tract Dis. 2017;21(2):120–4. [CrossRef]
- Kietpeerakool C, Khunamornpong S, Srisomboon J, Siriaunkgul S, Suprasert P. Cervical intraepithelial neoplasia II-III with endocervical cone margin involvement after cervical loop conization: Is there any predictor for residual disease? J Obstet Gynaecol Res. 2007;33(5):660–4. [CrossRef]
- Lubrano A, Medina N, Benito V, Arencibia O, Falcón JM, Leon L, et al. Follow-up after LLETZ: A study of 682 cases of CIN 2-CIN 3 in a single institution. Eur J Obstet Gynecol Reprod Biol. 2012;161(1):71–4. [CrossRef]
- Alder S, Megyessi D, Sundström K, Östensson E, Mints M, Belkić K, et al. Incomplete excision of cervical intraepithelial neoplasia as a predictor of the risk of recurrent disease—a 16-year follow-up study. Am J Obstet Gynecol. 2020;222(2):172.e1-172.e12. [CrossRef]
- Papoutsis D, Rodolakis A, Mesogitis S, Sotiropoulou M, Antsaklis A. Appropriate cone dimensions to achieve negative excision margins after large loop excision of transformation zone in the uterine cervix for cervical intraepithelial neoplasia. Gynecol Obstet Invest. 2013;75(3):163–8. [CrossRef]
- Kawano K, Tsuda N, Nishio S, Yonemoto K, Tasaki K, Tasaki R, et al. Identification of appropriate cone length to avoid positive cone margin in high grade cervical intraepithelial neoplasia. J Gynecol Oncol. 2016;27(5):1–7. [CrossRef]
- Ghaem-Maghami S, Sagi S, Majeed G, Soutter WP. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol. 2007;8(11):985–93. [CrossRef]
- Ouh YT, Cho HW, Kim SM, Min KJ, Lee SH, Song JY, et al. Risk factors for type-specific persistence of high-risk human papillomavirus and residual/recurrent cervical intraepithelial neoplasia after surgical treatment. Obstet Gynecol Sci. 2020;63(5):631–42. [CrossRef]
- Chen L, Liu L, Tao X, Guo L, Zhang H, Sui L. Risk Factor Analysis of Persistent High-Grade Squamous Intraepithelial Lesion after Loop Electrosurgical Excision Procedure Conization. J Low Genit Tract Dis. 2019;23(1):24–7. [CrossRef]
- Zang L, Hu Y. Risk factors associated with HPV persistence after conization in high-grade squamous intraepithelial lesion. Arch Gynecol Obstet [Internet]. 2021;304(6):1409–16. Available from: https://doi.org/10.1007/s00404-021-06217-1. [CrossRef]
- Huang HJ, Tung HJ, Yang LY, Chao A, Tang YH, Chou HH, et al. Role of human papillomavirus status after conization for high-grade cervical intraepithelial neoplasia. Int J Cancer. 2021;148(3):665–72. [CrossRef]
- Bogani G, Pinelli C, Chiappa V, Martinelli F, Lopez S, Ditto A, et al. Age-specific predictors of cervical dysplasia recurrence after primary conization: Analysis of 3,212 women. J Gynecol Oncol. 2020;31(5):1–8. [CrossRef]
- Nam K, Chung S, Kim J, Jeon S, Bae D. Factors associated with HPV persistence after conization in patients with negative margins. J Gynecol Oncol. 2009;20(2):91–5. [CrossRef]
- Chen JY, Wang ZL, Wang ZY, Yang XS. The risk factors of residual lesions and recurrence of the high-grade cervical intraepithelial lesions (HSIL) patients with positive-margin after conization. Med (United States). 2018;97(41). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).