1. Introduction
Globally, cardiovascular diseases (CVDs), such as coronary heart disease (CHD) and stroke, are the leading cause of death and disability among adults worldwide.[
1] In India, CVDs accounted for slightly more than a quarter (28%) of deaths and 14% of disability-adjusted life years (DALYs) in 2016. This represents a substantial 87% increase in mortality and a staggering 100% increase in DALYs since 1990.[
2]
A recent comprehensive analysis of data from 112 cohort studies across 34 countries demonstrated that over half of incident cases of CVDs in both males (52.6%) and females (57.2%) can be attributed to five modifiable risk factors: body mass index (BMI), systolic blood pressure (BP), non-HDL cholesterol, smoking, and diabetes.[
3] An analysis of data from the Prospective Urban Rural Epidemiology (PURE) study, encompassing 155,722 participants across 21 countries, showed that hypertension contributed to nearly a quarter (22.3%) of the population-attributable fraction (PAF) for CVD. Following hypertension was high non-HDL cholesterol, tobacco use, suboptimal diet, abdominal obesity, and diabetes, with each risk factor contributing 5-10% of the PAF for CVD.[
4] These modifiable and non-modifiable risk factors (e.g., age, sex) have been used to derive risk scores for estimating the 10-year absolute risk of developing CVD events using the ß-coefficient for risk factors and CVD event-free survival rates.[
5] The absolute CVD risk determines the probability of a person developing CVD events within a particular time, given the cumulative impact of separate risk factors.[
5] The higher the absolute CVD risk score, the higher the odds of a CVD event occurring.
8
CVD risk scores guide the clinical management of people at high risk of developing CVD events.[
6,
7,
8] Several CVD risk prediction models have been developed during the past few decades, including the Framingham Risk Score (FRS),[
9] Systematic Coronary Risk Evaluation (SCORE)[
10] and SCORE2 algorithms,[
11] American College of Cardiology/American Heart Association (ACC/AHA)
12 risk calculator, QRISK
13,14 and World Health Organization/International Society of Hypertension (WHO/ISH)
15 risk prediction charts, and the Revised Pooled Cohort Equations (PCE).[
12] Of these, the sex-specific FRS is the most widely used risk tool globally, given its better performance than many other risk scores in various populations.[
13,
14,
15] The FRS was initially developed in the late 1970s and underwent revision in 2008, using data from the original Framingham cohort, which primarily consisted of a predominantly White population in the United States.[
9] For its application beyond this population, FRS requires recalibration using contemporary data on CVD risk factors and CVD rates specific to the intended populations.[
16]
In India, to date, three distinct studies have recalibrated the FRS in specific regions, namely Tamil Nadu,[
17] Andhra Pradesh,[
18] and New Delhi.[
19] India is a diverse country with its states in various stages of epidemiological transition,[
20] experiencing shifts in patterns of CVD and associated risk factors,[
2] and varying CVD mortality rates.[
21] Consequently, the need for recalibrating the FRS on a state-by-state basis arises to enhance its performance in predicting the 10-year CVD risk for adults residing in each particular region. Kerala, the southernmost state in India, bears a substantial burden of type 2 diabetes, CVD, and cardiometabolic risk factors, despite having low mortality rates.[
21,
22,
23,
24] Notably, Kerala is in the most advanced stage of the epidemiological transition, positioning itself as the harbinger for the rest of India in terms of the CVD burden and associated risk factors.[
22,
25,
26] We report here the results of recalibrating the original FRS scores for adults in Kerala.
2. Methods
2.1. Study Design, Setting, and Participants
The study design, sample selection procedure, and participant recruitment details have been previously published.[
27,
28,
29,
30,
31,
32] Briefly, a cross-sectional survey was conducted from 2013 to 2016 in the Trivandrum district of Kerala as part of the Kerala Diabetes Prevention Program (K-DPP). Sixty polling areas (electoral divisions with geographical boundaries) were selected randomly from a total of 359 polling areas in a
taluk (sub-district) within the Trivandrum district. Individuals aged 30 to 60 years were randomly identified from the electoral roll of these 60 polling areas and approached at their households for screening. Phase 1 screening involved obtaining written informed consent and administering a brief questionnaire by trained interviewers. This questionnaire collected data on basic demographics (e.g., age, sex, income). Additionally, the Indian Diabetes Risk Score (IDRS)[
33] was administered, and waist and hip circumferences were measured using standard tools based on established protocols.[
34] During Phase 2 screening, individuals were invited to attend community-based clinics in their local neighborhoods. At these clinics, individuals underwent a 2-hour 75 g oral glucose tolerance test (OGTT), physical measurements, and provided blood samples for biochemical analysis.[
29] Standard questionnaires were also administered by interviewers to gather information on behavioral and psychosocial factors, health-related quality of life, and healthcare utilization.[
29]
2.2. Measurement of FRS variables
There are two distinct forms of FRS scores, namely “lipid-based FRS” and “BMI-based FRS”.[
9] The lipid-based FRS includes age, sex, current smoking, systolic BP, diabetes, total cholesterol, treatment for hypertension, and HDL-cholesterol.[
9] The “BMI-based FRS” retains the variables from the lipid-based version but substitutes BMI for lipids (total- and HDL-cholesterol).[
9] Information on current smoking and treatment for hypertension was collected using the questions from the WHO STEPS questionnaire. Participants were asked if they had smoked (cigarettes, bidis, cigars, or hookah) in the last 30 days (current smoking) and if they were currently taking medications for high blood pressure or hypertension (treatment for hypertension).[
34] BP was recorded three times with an Omron automatic blood pressure monitor (model IA2), with a minimum three-minute interval between readings.[
34] An individual’s BP was calculated as the average of the second and third BP readings. Blood samples were collected for the OGTT, HbA1c, measurement, and lipid profiling following established protocols.[
29] The samples were centrifuged within 30 minutes of collection and transported to a nationally accredited laboratory in containers with dry ice. Plasma glucose and serum lipid levels were measured using the Hexokinase and Enzymatic methods, respectively, on a COBAS 6000 analyzer, with kits supplied by Roche Diagnostics, Switzerland. HbA1c was measured via high-performance liquid chromatography on a D-10 BIORAD analyzer. LDL-cholesterol was estimated using the Friedewald equation[
35] for participants with triglycerides ≤400 mg/dl; for others, values from the Direct method were used. Diabetes was defined as fasting plasma glucose ≥126 mg/dl or 2-hour plasma glucose ≥200 mg/dl or both.[
36] The 10-year CVD risk of participants was categorized as follows: low risk (<10%), moderate risk (10-19.9%), and high risk (≥20%).[
37]
2.3. Calculation of the original FRS scores
We calculated the original lipid- and BMI-based FRS scores using the following Cox regression equation from the 2008 Framingham study.[
9]
In this equation,
represents an individual’s probability of developing a CVD event within 10 years. We obtained values for
(the 10-year CVD event-free survival rate),
(the beta-coefficient for each of the
ith Framingham risk factors), and
(the mean of the log-transformed
ith risk factor) from the original Framingham cohort study.[
9] These values were then used to calculate
, which is referred to as the ‘reference score’. To compute the reference scores for the original FRS scores, we log-transformed the values of each participant’s risk factors (e.g., log age, log total cholesterol). Here,
representes the log values of each of the
ith risk factors, and
p denotes the total number of risk factors.
values obtained from the original Framingham cohort were 0.88936 for males and 0.95012 for females for the lipid-based FRS scores, and 0.88431 for males and 0.94833 for females for the BMI-based FRS scores.[
9] The reference scores for the original FRS scores are given in
Table S1.
2.4. Recalibration of the FRS scores
Both the lipid- and BMI-based FRS scores underwent recalibration using Equation 1. The beta-coefficient values (
values were obtained from the original Framingham cohort study. Mean log-transformed values of the
ith risk factors were derived from the baseline survey data of the K-DPP study.[
28] CVD-free survival rates were from the Population Registry of Lifestyle Diseases (PROLIFE) study conducted in Kerala.[
38] The PROLIFE cohort was established in 2002 within a rural development block comprising seven villages in the Trivandrum district of Kerala.[
39] Health workers approached all residents in this block at their households, enrolling 161,942 adults (79,422 males and 82,398 females). Over a five-year period (from July 1, 2002, to June 30, 2007), there were 1,698 deaths due to CVD (1,005 in males and 693 in females), resulting in an annual CVD mortality rate of 0.002566590903 for males and 0.00170217992 for females.[
38] Information on these deaths was collected by health workers using a pretested, structured questionnaire, which was reviewed by a physician for assigning the cause of death for each event, following ICD-10 codes.[
40] Assuming a non-fatal to fatal CVD events ratio of 2:1, as recommended by the WHO,[
41] the estimated annual total CVD events were 0.00769977271 for males and 0.00510653976 for females. The 10-year CVD event-free survival rate
, was then calculated as (1-0.00769977271)
10 = 0.925614 for males and (1-0.00510653976)
10 = 0.9500926 for females. The reference scores for the recalibrated FRS scores are given in
Tables S2-S3.
2.5. Statistical analysis
Continuous variables are summarized using means and standard deviations (SD) or medians with interquartile ranges (IQR), depending on the data distribution, which was assessed visually through histograms. Categorical variables are expressed as frequencies along with percentages. To compare the median FRS scores between groups, we used the Mann-Whitney U test, while for categorical variables, group comparisons were conducted using the Chi-Square test. A two-sided p<0.05 was considered statistically significant. Plots were created using the ggplot2 package in R version 4.1.0. All statistical analyses were performed using Stata version 17.0 (Stata Corp LLC, Texas, USA).
3. Results
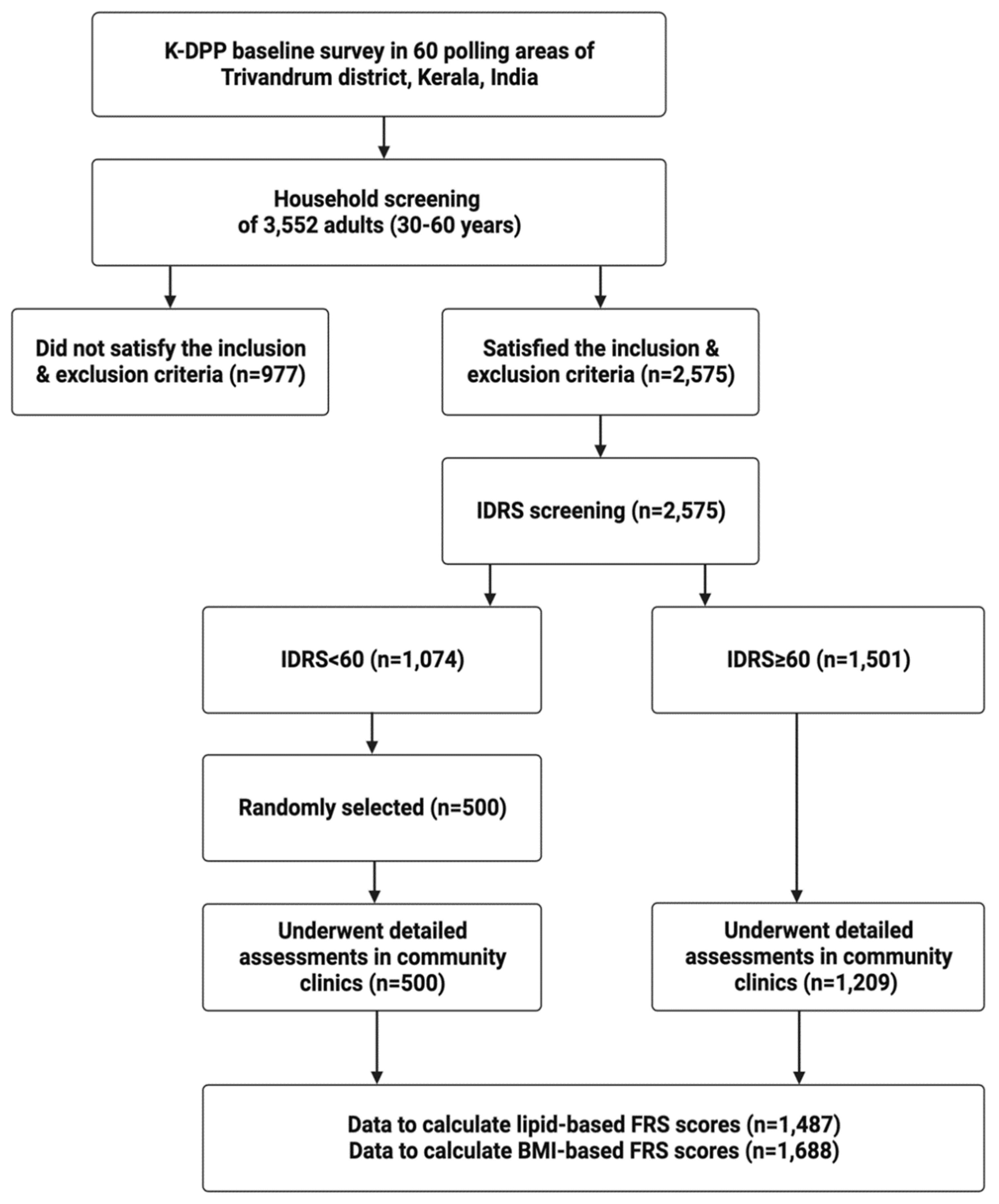
Data on risk factors to calculate the lipid-based FRS scores were available for 1,488 individuals (921 males and 567 females) and the BMI-based FRS scores for 1,688 individuals (1,042 males and 646 females), as shown in
Figure 1.
Table 1 presents the characteristics of risk factors for males and females in our study. In both datasets, the mean age of males was significantly higher than that of females (p<0.001). In the lipid-based dataset, males had a significantly lower mean HDL-cholesterol (p<0.001) and a higher mean systolic BP (in those taking BP-lowering medications) (p<0.001). They were also more likely to be current smokers (p<0.001) and have diabetes (p<0.001) compared to females. In the BMI-based dataset, males had a significantly lower mean BMI (p<0.001) and were more likely to be current smokers (p<0.001) and have diabetes (p=0.007) than females.
Table 2 shows the median (IQR) 10-year CVD risks estimated by FRS scores. For both the lipid-based and BMI-based FRS scores, the median recalibrated scores were significantly lower than the median original scores in males. However, for females, the median recalibrated scores were significantly higher than the median original scores. For instance, in males, the median recalibrated lipid-based FRS score was 7.34, compared to 8.88 for the original score (p<0.001). In females, the median recalibrated lipid-based FRS score was 4.83, compared to 2.85 for the original score (p<0.001).
Table 3 illustrates the proportion of participants classified into various risk categories of FRS. In comparison with the original lipid-based and BMI-based FRS scores, a significantly lower proportion of males were categorized as high risk (≥20%) by the recalibrated lipid-based (12.92% vs. 9.55%) and BMI-based (14.68% vs. 8.73%) scores; p<0.001 for both comparisons. Conversely, in females, compared with the original lipid-based and BMI-based FRS scores, a significantly higher proportion was categorized as high risk (≥20%) by the recalibrated lipid-based (1.06% vs. 3.35%) and BMI-based (2.32% vs. 4.64%) FRS scores; p<0.001 for both comparisons.
Of the 190 males classified as ‘high risk’ for a 10-year CVD using the original FRS scores and the 133 males identified as ‘high risk’ using the recalibrated scores, only 1 (0.5%) and 1 (0.8%), respectively, were taking statins. None of the 17 females categorized as ‘high risk’ using the original scores and the 14 females identified as ‘high risk’ using the recalibrated scores were receiving statin therapy.
4. Discussion
In this study, the recalibrated FRS scores resulted in significantly lower median 10-year CVD risks than the original scores in males but higher risks in females. Additionally, the proportion of individuals classified as high risk (with a score of ≥20%) for experiencing CVD events within 10 years using the recalibrated scores was significantly lower in males but higher in females.
In a study conducted by Sasikumar et al. in rural Vellore, Tamil Nadu, which involved about 3,000 adults (aged 30-64 years), the median 10-year FRS CVD risk and the percentage of participants classified as high risk (≥30%) were higher when using the recalibrated scores compared to the original scores in both sexes.[
17] Similarly, a study from urban Delhi reported that the average 10-year FRS recalibrated scores were higher than the original scores for both males and females, using data from the Centre for cArdiometabolic Risk Reduction in South-Asia (CARRS) study.[
19] However, in a study by Chow et al. conducted among 4,535 adults (aged ≥30 years) in rural Andhra Pradesh, the mean 10-year CHD risks calculated using the original and recalibrated FRS scores were found to be similar.[
18] These differences in findings among various studies, including the current study, underscore the significance of recalibrating the original FRS scores individually for each Indian state, using local data on risk factors and CVD mortality. This tailored recalibration approach would enhance the accuracy of risk assessment for individuals residing in each distinct region.
The WHO 2020 guidelines recommend that individuals with a CVD risk score of ≥20% should be prescribed statins.[
37] However, in our study, an alarmingly low proportion (<1%) of high-risk males and no high-risk females were taking this medication. This may be attributed to several factors, including the suboptimal use of FRS in clinical practice, a lack of consensus among physicians regarding who should receive statins, as different guidelines propose varying risk thresholds for statin prescription,[
6,
7,
8] or potential issues with patient adherence to statins. Notably, our study’s figures were lower than those reported in the Vellore study, where 2.5% of high-risk males based on the original FRS scores and 2.0% of high-risk males according to the recalibrated scores were receiving statin therapy.[
17] Data on statin use were not reported in the Delhi and Andhra Pradesh studies.
To the best of our knowledge, this study represents the first effort to recalibrate FRS scores in the state of Kerala. While the study was conducted in a single taluk in the Trivandrum district, it’s worth noting that the distribution of age, sex, education, and occupation among our participants was broadly similar to that of the general population (aged 30-59 years) in rural Kerala at the time of the study.[
42] Therefore, the findings of this study may have relevance and applicability to other parts of rural Kerala. Other strengths include its large sample size, random participant selection, and the use of standard and robust methods for recalibrating both lipid- and BMI-based FRS scores. However, it’s important to acknowledge certain limitations. The cross-sectional survey was primarily conducted to recruit participants for a diabetes prevention program. This led to the exclusion of individuals who were illiterate in the local language, had a history of chronic illnesses, pregnant women, or those taking medications that could affect glucose tolerance (e.g., steroids, antipsychotics). Consequently, the generalizability of the study findings to these excluded groups is limited. Further, as the study was conducted in a predominantly rural population, the results do not apply to urban areas in Kerala. Finally, there were participants with missing data for calculating lipid-based FRS scores, and these individuals were different in terms of mean age, BMI, systolic BP, and prevalent diabetes compared to those without missing data (
Table S8), which could introduce a selection bias.
5. Conclusions
Recalibrating FRS scores is a feasible and practical approach for estimating the 10-year CVD risk for adults in India, particularly when there is a limited number of long-term cohort studies available to accurately determine CVD events in the country. Wider adoption of FRS in clinical practice can help identify high-risk individuals for early initiation of treatment, potentially contributing to a reduction in CVD-related deaths.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, T.S., M.S. and A.M.O. Methodology, T.S., M.S., B.O. and A.M.O.; formal analysis T.S. and M.S.; writing—original draft preparation, T.S.; writing—review and editing.; all authors; funding acquisition, B.O. All authors have read and agreed to the submitted version of the manuscript.
Funding
K-DPP was funded by the National Health and Medical Research Council (Project Grant ID 1005324).
Institutional Review Board Statement
The K-DPP study was approved by the Institutional Ethics Committee of the Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram (SCT/IEC-333/May 2011) and the Human Research Ethics Committee of Monash University (CF11/0457- 2011000194), and the University of Melbourne (1441736) in Australia.
Informed Consent Statement
Written informed consent was obtained from all the participants.
Data Availability Statement
The data used for this analysis will be made available upon reasonable request to the Principal Investigator (B.O) of the K-DPP study, subject to ethics approval.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ACC |
American College of Cardiology |
| AHA |
American Heart Association |
| BMI |
body mass index |
| BP |
blood pressure |
| CARRS |
Centre for cArdiometabolic Risk Reduction in South-Asia |
| CHD |
coronary heart disease |
| CVDs |
cardiovascular diseases |
| FRS |
Framingham Risk Score |
| IDRS |
Indian Diabetes Risk Score |
| IQR |
interquartile range |
| ISH |
International Society of Hypertension |
| K-DPP |
Kerala Diabetes Prevention Program |
| OGTT |
oral glucose tolerance test |
| PAF |
population-attributable fraction |
| PCE |
Pooled Cohort Equation |
| PROLIFE |
Population Registry of Lifestyle Diseases |
| SCORE |
Systematic Coronary Risk Evaluation |
| SD |
standard deviation |
| WHO |
World Health Organization |
References
- Vaduganathan, M.; Mensah, G.A.; Turco, J.V.; Fuster, V.; Roth, G.A. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J Am Coll Cardiol 2022, 80, 2361–2371. [Google Scholar] [CrossRef] [PubMed]
- India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health 2018, 6, e1339–e1351. [Google Scholar] [CrossRef] [PubMed]
- Magnussen, C.; Ojeda, F.M.; Leong, D.P.; Alegre-Diaz, J.; Amouyel, P.; Aviles-Santa, L.; De Bacquer, D.; Ballantyne, C.M.; Bernabé-Ortiz, A.; Bobak, M.; et al. Global Effect of Modifiable Risk Factors on Cardiovascular Disease and Mortality. N Engl J Med 2023, 389, 1273–1285. [Google Scholar] [CrossRef]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Badawy, M.; Naing, L.; Johar, S.; Ong, S.; Rahman, H.A.; Tengah, D.; Chong, C.L.; Tuah, N.A.A. Evaluation of cardiovascular diseases risk calculators for CVDs prevention and management: scoping review. BMC Public Health 2022, 22, 1742. [Google Scholar] [CrossRef]
- Weintraub, W.S.; Daniels, S.R.; Burke, L.E.; Franklin, B.A.; Goff, D.C., Jr.; Hayman, L.L.; Lloyd-Jones, D.; Pandey, D.K.; Sanchez, E.J.; Schram, A.P.; et al. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation 2011, 124, 967–990. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- D'Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J 2021, 42, 2439–2454. [Google Scholar] [CrossRef] [PubMed]
- Yadlowsky, S.; Hayward, R.A.; Sussman, J.B.; McClelland, R.L.; Min, Y.I.; Basu, S. Clinical Implications of Revised Pooled Cohort Equations for Estimating Atherosclerotic Cardiovascular Disease Risk. Ann Intern Med 2018, 169, 20–29. [Google Scholar] [CrossRef]
- Raj, M.P.; Krishnamurthy, V.; Basu, E.; Balaji, V.; Prakash Rao, V.V.; R, N. Comparison of Framingham Risk Scores (FRS), Joint British Society (JBS3), and American College of Cardiology/American Heart Association (ACC/AHA) Cardiovascular Risk Scores Among Adults With First Myocardial Infarction. Cureus 2023, 15, e33221. [Google Scholar] [CrossRef]
- Garg, N.; Muduli, S.K.; Kapoor, A.; Tewari, S.; Kumar, S.; Khanna, R.; Goel, P.K. Comparison of different cardiovascular risk score calculators for cardiovascular risk prediction and guideline recommended statin uses. Indian Heart J 2017, 69, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, T.A.; Abrahams-Gessel, S.; Alam, S.; Alam, D.; Ali, M.; Bloomfield, G.; Carrillo-Larco, R.M.; Dorairaj, P.; Gutierrez, L.; Irazola, V.; et al. Comparison of Nonblood-Based and Blood-Based Total CV Risk Scores in Global Populations. Glob Heart 2016, 11, 37–46. [Google Scholar] [CrossRef]
- Mishra, A.; McClelland, R.L.; Inoue, L.Y.T.; Kerr, K.F. Recalibration Methods for Improved Clinical Utility of Risk Scores. Med Decis Making 2022, 42, 500–512. [Google Scholar] [CrossRef]
- Sasikumar, M.; Oommen, A.M.; Mohan, V.R.; Gupta, P.; Rebekah, G.; Abraham, V.J.; George, K. Recalibration of the Framingham risk score for predicting 10-year risk of cardiovascular events: A non-concurrent rural cohort study from Tamil Nadu. Indian Heart J 2023, 75, 47–52. [Google Scholar] [CrossRef]
- Chow, C.K.; Joshi, R.; Celermajer, D.S.; Patel, A.; Neal, B.C. Recalibration of a Framingham risk equation for a rural population in India. J Epidemiol Community Health 2009, 63, 379–385. [Google Scholar] [CrossRef]
- Gupta, P.; Prieto-Merino, D.; Ajay, V.S.; Singh, K.; Roy, A.; Krishnan, A.; Narayan, K.M.V.; Ali, M.K.; Tandon, N.; Prabhakaran, D.; et al. Cardiovascular risk prediction in India: Comparison of the original and recalibrated Framingham prognostic models in urban populations. Wellcome Open Res 2019, 4, 71. [Google Scholar] [CrossRef]
- India State-Level Disease Burden Initiative Collaborators. Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet 2017, 390, 2437–2460. [Google Scholar] [CrossRef] [PubMed]
- Office of the Registrar General of India. Vital Statistics of India Based on the Civil Registration System 2020.
- Sathish, T.; Kannan, S.; Sarma, S.P.; Razum, O.; Sauzet, O.; Thankappan, K.R. Seven-year longitudinal change in risk factors for non-communicable diseases in rural Kerala, India: The WHO STEPS approach. PLoS One 2017, 12, e0178949. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, M.N.; Zachariah, G.; Venugopal, K.; Mohanan, P.P.; Harikrishnan, S.; Sanjay, G.; Jeyaseelan, L.; Thankappan, K.R. Prevalence of coronary artery disease and its risk factors in Kerala, South India: a community-based cross-sectional study. BMC Cardiovasc Disord 2016, 16, 12. [Google Scholar] [CrossRef] [PubMed]
- Sarma, P.S.; Sadanandan, R.; Thulaseedharan, J.V.; Soman, B.; Srinivasan, K.; Varma, R.P.; Nair, M.R.; Pradeepkumar, A.S.; Jeemon, P.; Thankappan, K.R.; et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open 2019, 9, e027880. [Google Scholar] [CrossRef] [PubMed]
- Sathish, T.; Kannan, S.; Sarma, P.S.; Razum, O.; Thankappan, K.R. Incidence of hypertension and its risk factors in rural Kerala, India: a community-based cohort study. Public Health 2012, 126, 25–32. [Google Scholar] [CrossRef]
- Haregu, T.N.; Byrnes, A.; Singh, K.; Sathish, T.; Pasricha, N.; Wickramasinghe, K.; Thankappan, K.R.; Oldenburg, B. A scoping review of non-communicable disease research capacity strengthening initiatives in low and middle-income countries. Glob Health Res Policy 2019, 4, 31. [Google Scholar] [CrossRef]
- Sathish, T.; Aziz, Z.; Absetz, P.; Thankappan, K.R.; Tapp, R.J.; Balachandran, S.; Shetty, S.S.; Oldenburg, B. Participant recruitment into a community-based diabetes prevention trial in India: Learnings from the Kerala Diabetes Prevention Program. Contemp Clin Trials Commun 2019, 15, 100382. [Google Scholar] [CrossRef]
- Sathish, T.; Oldenburg, B.; Tapp, R.J.; Shaw, J.E.; Wolfe, R.; Sajitha, B.; D'Esposito, F.; Absetz, P.; Mathews, E.; Zimmet, P.Z.; et al. Baseline characteristics of participants in the Kerala Diabetes Prevention Program: a cluster randomized controlled trial of lifestyle intervention in Asian Indians. Diabet Med 2017, 34, 647–653. [Google Scholar] [CrossRef]
- Sathish, T.; Williams, E.D.; Pasricha, N.; Absetz, P.; Lorgelly, P.; Wolfe, R.; Mathews, E.; Aziz, Z.; Thankappan, K.R.; Zimmet, P.; et al. Cluster randomised controlled trial of a peer-led lifestyle intervention program: study protocol for the Kerala diabetes prevention program. BMC Public Health 2013, 13, 1035. [Google Scholar] [CrossRef]
- Thankappan, K.R.; Sathish, T.; Tapp, R.J.; Shaw, J.E.; Lotfaliany, M.; Wolfe, R.; Absetz, P.; Mathews, E.; Aziz, Z.; Williams, E.D.; et al. A peer-support lifestyle intervention for preventing type 2 diabetes in India: A cluster-randomized controlled trial of the Kerala Diabetes Prevention Program. PLoS Med 2018, 15, e1002575. [Google Scholar] [CrossRef]
- Sathish, T.; Shaw, J.E.; Tapp, R.J.; Wolfe, R.; Thankappan, K.R.; Balachandran, S.; Oldenburg, B. Targeted screening for prediabetes and undiagnosed diabetes in a community setting in India. Diabetes Metab Syndr 2019, 13, 1785–1790. [Google Scholar] [CrossRef]
- Aziz, Z.; Mathews, E.; Absetz, P.; Sathish, T.; Oldroyd, J.; Balachandran, S.; Shetty, S.S.; Thankappan, K.R.; Oldenburg, B. A group-based lifestyle intervention for diabetes prevention in low- and middle-income country: implementation evaluation of the Kerala Diabetes Prevention Program. Implement Sci 2018, 13, 97. [Google Scholar] [CrossRef]
- Mohan, V.; Deepa, R.; Deepa, M.; Somannavar, S.; Datta, M. A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J Assoc Physicians India 2005, 53, 759–763. [Google Scholar] [PubMed]
- World Health Organization. STEPwise approach to NCD risk factor surveillance (STEPS) Manual.
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46, S19–S40. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. HEARTS: Technical package for cardiovascular disease management in primary health care: evidence-based treatment protocols. Geneva, 2018.
- Soman, C.R.; Kutty, V.R.; Safraj, S.; Vijayakumar, K.; Rajamohanan, K.; Ajayan, K. All-cause mortality and cardiovascular mortality in Kerala state of India: results from a 5-year follow-up of 161,942 rural community dwelling adults. Asia Pac J Public Health 2011, 23, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Soman, C.R.; Shahulhameed, S.; Ramankutty, V.; Vijayakumar, K.; Kunjukrishnapillai, R.; Ajayan, K.; Sajikumar, S. Cohort profile: the PROLIFE study in Kerala, India. Int J Epidemiol 2011, 40, 10–14. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Tunstall-Pedoe, H.; Kuulasmaa, K.; Mähönen, M.; Tolonen, H.; Ruokokoski, E.; Amouyel, P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 1999, 353, 1547–1557. [Google Scholar] [CrossRef]
- Office of the Registrar General and Census Commissioner of India. Census 2011. Available online: http://censusindia.gov.in (accessed on 25 September 2023).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).