1. Introduction
The role of subconcussive impacts in sport-related concussion has come under scrutiny with little consensus as to definitive outcomes, critical levels of exposure, or age at which first exposure bears least risk (Bahrami et al., 2016; Kercher et al., 2020; T. McAllister & McCrea, 20.17; Montenigro, et al., 2016). Some retrospective studies have suggested that starting football under 12 years of age is potentially problematic (Alosco et al., 2018; Stamm et al., 2015). Alosco et al. conducted phone assessments of former amateur and professional players and concluded that those exposed before the age of 12 had a greater risk of clinical impairment (greater than 1.5 s.d. below the normative mean). Stamm et al provided a brief neuropsychological battery to 42 former National football League players (NFL), evenly divided between age of first exposure under and over age 12 (Stamm et al., 2015). Differences in standard scores were statistically significant with those under age 12 having lower scores. None appeared to be abnormally low. On the other hand, Solomon et al. (Solomon, 2018) as well as Iverson et al. (Iverson et al., 2020) did not find age of exposure effects in their separate studies. Two prospective studies following youth football players by Rose et al. found few relationships between HAE and cognition, except those diagnosed with Attention Deficit Hyperactivity Disorder (Rose et al., 2018, 2019). Thus, there is no firm consensus in regards to the age-related risks of exposure.
Mainwaring et. al completed a systematic review of studies related to “subconcussive impacts in sports (Mainwaring et al., 2018). The studies were predominantly from male athletes in contact and collision sports, Neurobiological studies generally found that repetitive hits to the head were associated with microstructural and functional changes in the brain. Whether these changes represented frank injury was unclear. Over all, use of the term ‘subconcussion’ was found to be inconsistently used, poorly defined, and misleading. There was insufficient to weak evidence for the relationship between repetitive hits to the head and deterioration in neurocognitive performance. Studies of impact exposure metrics examined various indices, including linear acceleration, rotational acceleration, and location and frequency of hits. Insufficient evidence was presented to determine a minimal injury threshold for repetitive hits to the head.
In their ongoing studies of chronic traumatic encephalopathy in athletes the Boston University laboratory analyzed findings of amateur athletes from 152 of 156 brain donors younger than 30 years of age. Neuropathologic evaluations, retrospective telephone clinical assessments, and online questionnaires with informants were performed in a blinded manner (McKee et al., 2023). The sample was primarily male (141; 92.8%), and CTE was diagnosed in 63 (41.4%). This case series found that young brain donors exposed to repetitive head impacts were highly symptomatic regardless of CTE status, and the causes of symptoms in this sample are likely multifactorial. The findings pointed to the length of time playing and level of play as associated with greater rates of CTE. The two cases of CTE that only played youth football had significant repetitive head acceleration exposure due to later life exposures. These findings confirm that CTE and other brain pathologies can be found in young, symptomatic contact sport athletes, but the clinical correlates of the pathologic conditions remain uncertain. Importantly, there was no statistical relationship between the number of concussions and the present of CTE, further implicating the effect of repetitive head impacts absent frank concussion.
The Bioengineering Research Partnership (BRP) study of sports concussion in youth football collected helmet-sensor head acceleration event (HAE) data in youth between ages 9 to 13 over several years. The goal was to determine if the frequency or intensity of accelerative forces to the head were related to frank concussion or other discernable cognitive outcomes. An analysis of the first-year data found medium effects of the composite HAE metric (HITsp) was on negative changes on the list-learning neuropsychological test test (Maerlender, Smith, et al., 2021). However, the effect was found only in the younger age group of nine to 10-years old (n = 41) but not among the group of older players (ages 11-13); player weight was also identified as a significant covariate in the young group. These findings suggested that younger football players demonstrated a subtle but negative cognitive effect related to the average amount of HAE that was moderated by weight.
The goal of this analysis was to determine if a second season of exposure would again demonstrate a relationship with neuropsychological test score changes. Based on season-one the following hypotheses were examined:
Hypotheses
Ia. After two seasons, significant relationships between test scores and HAE values would be observed such that the inverse relationships between test score changes and HAE would observed indicating that greater HAE values would result in less positive test score change;
Ib. Player age and weight would modify these cognitive outcomes.
2. Materials and Methods
2.1. Procedure
The procedures for this prospective observational study followed the procedures reported in season-one (Maerlender et al., 2021). Briefly, teams from North Carolina, Rhode Island and Virginia had been recruited previously. New teams were added when teams dropped out. Neuropsychological tests were administered before and after each season and parents completed demographic forms. Riddell football helmets were instrumented with accelerometers (Sideline Response System; Riddell, Elyria, OH). All practices and games were video recorded to validate impacts and remove erroneous measurements (e.g. tossed helmets, helmet slaps). In vivo monitoring was conducted of youth during all practices and games in three states (North Carolina, Rhode Island, Virginia). Pre- and post-season assessments were conducted at medical centers associated with the project.
2.2. Participants
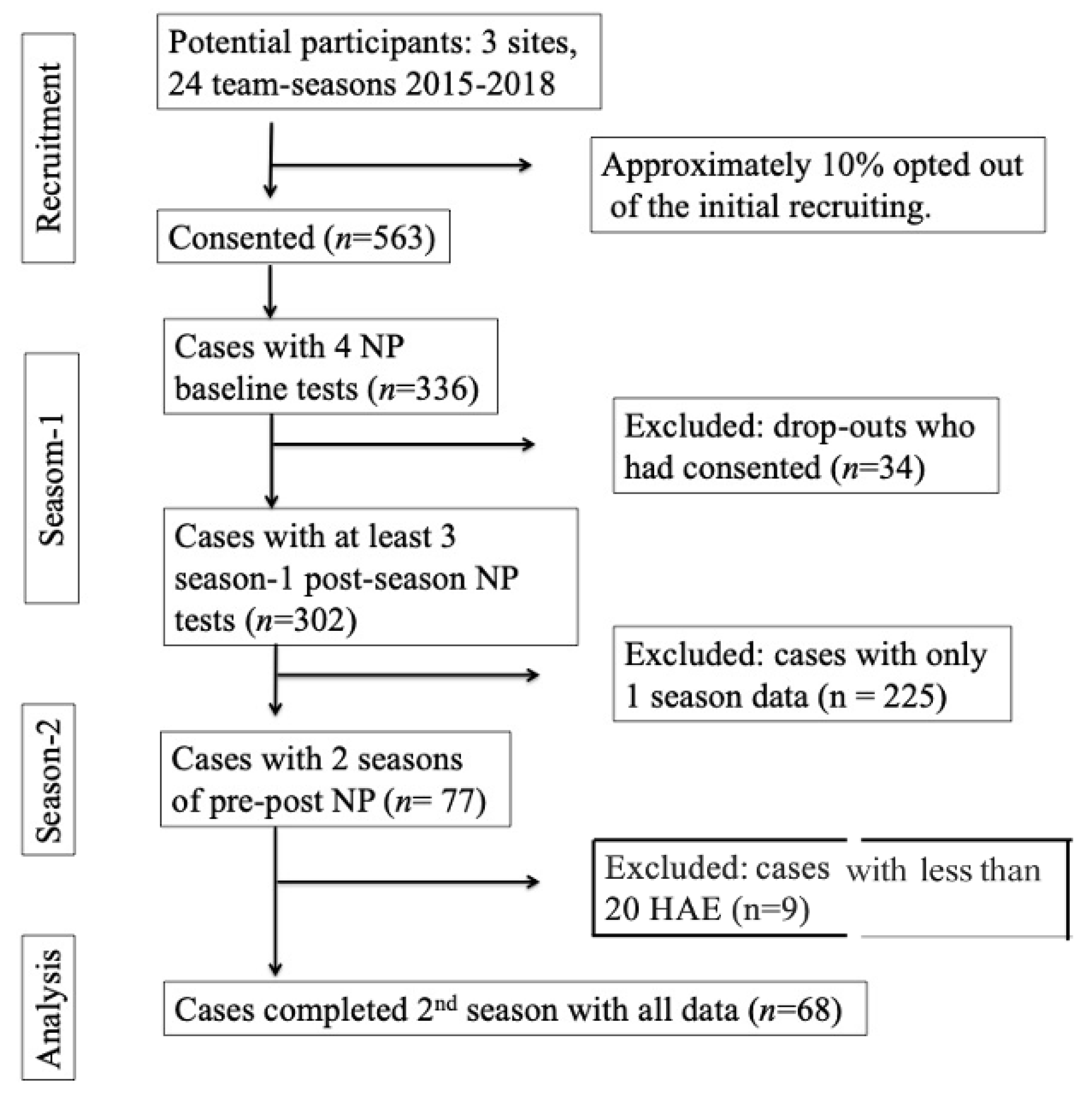
This study is part of a larger National Institutes of Health (NIH)-funded project: “The biomechanical basis of concussions in youth football” (R01NS094410). Recruitment of new teams was required as some teams declined to participate in subsequent years for the project were detailed previously (see Figure 1 for recruitment flow). Participants were recruited from teams in proximity to the research sites in the three states. At the start of each season for five years, research assistants made presentations to the teams and parents, and requested volunteers for further evaluations. Data on the percent participation from each team, or the frequency of team changes were not recorded. Institutional Review Board approvals were obtained from each institution, and assents from minors and parental consents were obtained prior to the study.
2.3. Variables and Measurement
2.3.1. Demographics
Demographic variables collected included age, sex, height, weight, race/ethnicity, mother’s level of education, psychiatric and learning diagnoses, time intervals (pre-season to post-season, and post-season end to time of assessment), the number of previous concussions, the number of years playing a contact sport and topographical state of participation.
2.3.2. Neuropsychological Tests
Five tests were chosen from the National Institutes of Health (NIH) Toolbox for the entire study. Excellent reliability and validity have previously been documented (Carlozzi et al., 2013, 2017; Tulsky et al., 2013, 2017). Tests were individually administered by trained research technicians according to standard protocols in laboratories at the respective research sites. List Sort and Rey Auditory Verbal Learning Test (RAVLT) represented memory processes, while Flanker and Pattern Comparison represent speed. Previous factor analyses confirmed this structure (Maerlender, Smith, et al., 2020). Memory and speed functions are routinely assessed in concussion management (Maerlender, 2018; Schatz & Maerlender, 2013). The Picture Vocabulary Test was used as a proxy for level of cognitive function/general developmental level (Zelazo et al., 2013).
Repeating neuropsychological tests has been shown to lead to score increases (citations). Adjusting for such increases as well as known effects due to regression to the mean is standard practice in rehabilitation neuropsychology. Adjusted test scores were generated by modeling the expected change due to practice effects and regression to the mean using a standardized regression method similar to the method used in season-one (Maerlender, et al., 2021). This approach is supported by multiple studies (Chelune, 2003; Heilbronner et al., 2010; Jacobson & Truax, 1991; Temkin et al., 1999). To estimate the season-two post-test change value, the test scores from the three previous tests of this sample were entered into a regression model predicting the fourth test. The regression parameters were used to generate a predicted amount of change for each participant. That z-score can be transformed to a standard score to reflect the new adjusted standard score. To create the Cognitive Total change, the change values from the four tests were summed and averaged. An advantage of regression-based z-scores (RBz-scores) over reliable change intervals is that z-scores are continuous variables and can be more easily used in analyses.
Technically, if test scores do not change in test-retest studies, there should be no need to use adjusted RBz change scores. To verify the changes in this sample and the need for using adjusted change scores, the unadjusted test standard scores were analyzed using paired sample t-tests (preseason-one to postseason-two).
2.3.3. Neuropsychological Test Performance Indicators
Although formal performance validity tests or metrics were not obtained, test administrators completed behavioral rating observation forms and an administration fidelity form to assess performance validity. Fidelity measures included use of trained personnel, use of scripts for instructions, and having an appropriate setting for testing. For each test administered testing personnel kept track of distractions or disruptions: 1. Requests to repeat directions or asking for help understanding task; 2. Being distracted by external factors (e.g., fidgeting with phone or looking away from iPad to focus on something, outside phone ringing, talk in hallway outside of testing room); 3. Taking a break between tasks (e.g., bathroom break, getting snack, or water); 4. Needing encouragement, prompts for best effort; 5. Other distractions such as technical or computer problems (e.g., computer/iPad freezing). These instruments were developed by the authors and not formally validated.
2.3.4. Biomechanical Measurement of Head Acceleration Events (HAE)
Head impact measuring devices allow researchers to study on-field head impacts and collect kinematic data of concussive and sub-concussive head impacts (Brennan et al., 2017). The Sideline Response System (formerly the Head Impact Telemetry System or HIT, Simbex, Inc, Lebanon, NH) was developed to continuously monitor head impact exposure in real-time during helmeted sports (Broglio et al., 2011; Duma et al., 2005; Gysland et al., 2012; Wilcox et al., 2015). The HIT system has been validated through several on-field and laboratory studies (Beckwith et al., 2012; Crisco et al., 2010; Duma et al., 2005; Funk et al., 2007, 2012).
Research assistants attended each practice or game session to collect biomechanical HAE data and maintain the equipment. Standard video analysis of HAE included validating impacts as contact during sessions, confirming occurrence during organized team sessions (games or practices). Further, all impacts over 40g’s were video-inspected to assure inclusion.
Based on the season-one results, the metric of primary interest was the composite HAE metric, HITsp. This metric is a global metric created by a transformation of the computed head impact measures of peak linear and peak angular acceleration into a single latent variable using principal component analysis and applies a weighting factor based on impact location (Greenwald et al., 2008).
2.4. Analyses
Statistical analyses were performed with the Statistical Package for Social Sciences, v 27 (SPSS, Chicago, IL). Demographic variables were checked for relationship to dependent variables using graphical displays and correlation/regression analysis with a p <.05 threshold for statistical significance. Categorical variables were analyzed using chi-square statistics.
Standard scores and regression-based z-scores were evaluated with graphical displays and repeated measures MANOVA or paired samples t-tests to determine the pattern and magnitude of the obtained changes from beginning of season-one to the end of season-two.
Effect size descriptors for partial eta-squared (ηp2) were: large = .25, medium = .09, small = .01; for Cohen’s d large = .80, medium = .50, small = .20; for regression full models R2: large .35, medium = .15 and small = .02 (Cohen, 1988).
To establish test re-test reliability within this sample, intraclass correlations (ICC) of the neuropsychological test standard scores used two-way mixed effects models for test-retest reliabilities were calculated using an absolute agreement definition and the average of the measures (Koo & Li, 2016; Shrout & Fleiss, 1979).
The dependent variable was the average of the change values of the four neuropsychological tests (preseason-one to postseason-two) combined, termed the Cognitive Total score. Age and player weights were analyzed for differences between groups and used as modifiers. Residuals were checked graphically and with tests for normality. Significance level was set at p < .05, using 1-tailed criteria based on the directionality identified in season-one results and consistent with the current hypothesis.
3. Results
3.1. Participant Characteristics
Sixty-eight participants from season-one participated in the second season, all were male. Twenty-seven were from the original younger cohort (9-10 years old) and 47 were from the original older cohort (11 – 13 years old). Testing was conducted at the beginning and end of the season (median interval from last recorded HAE to testing was 5 days, range 2 to 51 days). Although there were differences in the timing of tests, the effect of interval of test administrations on scores was not significant.
Over the five seasons of the project there was considerable attrition of teams and participants that greatly reduced the number of second-season participants considerably. It was not possible to determine if there were any reasons for systematic loss of participants although informal responses from coaches were uninformative and there seemed to be no concerns.
Participants who were concussed during either season were removed from the sample (n = 6), as were those with less than 20 total head impacts for either season (n = 16). The low-HAE frequency players that were dropped had HAE frequencies below the 2nd%ile of the distribution and thus felt to be outliers. Further, having so few impacts would skew the average HAE values (the sums of HAE divided by number of impacts).
Of the 68 participants, 53 participated in the year immediately following season-1 while 14 players participated two years later and one participated three years later. Recruitment process is presented in Figure 1.
Figure 2.
Study Recruitment Flow. Note. NP = neuropsychological; HAE = frequency of head acceleration events.
Figure 2.
Study Recruitment Flow. Note. NP = neuropsychological; HAE = frequency of head acceleration events.
Only three participants reported a previous concussion, while the median years of contact sports prior to the second season in this project was 2.5 (range 1-8). Eight participants reported taking psychotropic medication. The estimated general level of intellectual functioning was in the average range with a mean vocabulary standard score of 104. The maternal level of education was 30 with less than bachelors degree and 38 with bachelors or greater. Other demographics appear in
Table 1. None of these variables had an effect of outcomes.
3.2. Analysis of Neuropsychological Test Scores
Computer issues resulted in missing values for 4 individuals and six tests. Multiple imputation methods were used (SAS 2013, Proc MiAnalyze) to impute values in the analyses rather than deleting the individuals in the analysis. The algorithm generates m data sets of complete data by providing estimates missing values that include their uncertainty (hence generating m different data sets). The m data sets are then used in calculations and results combined for inference. Twenty data sets were generated for the analyses.
The Cognitive Total demonstrated acceptable levels of test-retest reliability: ICC = .792 (95th CI .663 – 872). The median interval of contact to post-testing was five days (range 2-51).
Three of the four test standard scores increased significantly from pre-season-one to post-season-two with the exception of the Flanker test: RAVLT t(67) = 3.60, p = .001, d = .437; List Sort t(67) = 4.19, p < .001, d = .508; Pattern Comparison t(67) = 9.19, p < .001, d = 1.11; Flanker t(67) = 1.76, p = .082, d = .213; Cognitive Total t(67) = 10.15, p<.001, d = 1.23.
There was a significant difference in change scores between the two age groups (younger mean -1.46; older mean 0.28): t(66) = 3.391, p <.001, d = .841, 95CI = -2.76 to -0.72.
3.3. Head Acceleration Event Metrics
For the full sample, mean HITsp values were higher in season-one (14.54 to 14.38), as well as slightly more impacts on average in season-one: frquency238.38 compared to 237.98), Neither were significantly different. When compared between the age groups, there was no statistical difference in HITsp values: t(66)= 1.859, p = .068, 95th CI = -1.05 to 0.04.
3.4. Head Acceleration Event Metrics and Neuropsychological Effects
Consistent with season-one, the mean of HITsp value was a significant predictor of total cognitive change across age groups, albeit with a small effect: R2 = .06, F = 4.06, p = .024.
Having confirmed that the dependent variable was significantly different by age group, separate models by age group were run with weight entered into the models. The starting weight was chosen to reflect the earliest developmental exposure. There was the differential relationship of weight by age. For the younger group, the negative betas (and correlations) indicated that greater positive change was related to less HAE and less weight. In the older group, the relationship of HAE to cognitive change was still inverse, but weight had a positive relationship. In this group, greater positive cognitive change was related to greater weight.
| Model |
Independent Variable |
B |
SE B |
β |
R2 |
F |
p |
| Younger |
HITsp |
-0.773 |
0.387 |
-0.371 |
0.14 |
3.991 |
0.027 |
| |
HITsp |
-0.613 |
0.393 |
-0.294 |
|
|
|
| |
Weight |
-0.024 |
0.016 |
-0.282 |
0.211 |
3.214 |
0.026 |
| |
|
|
|
|
|
|
|
| Older |
HITsp |
-0.639 |
0.265 |
-0.36 |
0.13 |
5.809 |
0.01 |
| |
HITsp |
-0.506 |
0.274 |
-0.285 |
|
|
|
| |
Weight |
0.013 |
0.008 |
0.243 |
0.18 |
4.263 |
0.01 |
3.5. Clinical Significance
In the clinical setting significance is set at plus or minus 1.27 standard deviations (90% confidence interval). As a group the younger group score change exceeded this threshold (-1.47) with twelve of the 27 cases (44%) exceeding this threshold. In the older group, the group change was not significant while 10 of the 41 individual cases (24%) exceeded the threshold.
4. Discussion
While the relationship of overt head injury to neurodegenerative disease has been identified since the early papers on dementia pugilistica, the effect of subclinical head impacts to more serious neurodegenerative disease has been suspected (Castellani & Perry, 2017). However, establishing both immediate causal effects of early HAE and longer-term consequences have been elusive. It would also seem that if there were a cumulative effect, the consequences of early exposure would likely be subtle. This study confirmed and extended the results from the previous study of one season of youth football and demonstrate a relationship between cognitive test scores and HAE.
Further, the relationships were again inverse with the higher magnitude of accumulated HAE values related to less than expected change from season-one to season-two, both across the full sample and when analyzed by age groups. Weight had a disproportional effect with younger and heavier players showing more negative change awhile in the older group, lighter players showed more negative change. The findings suggest that developmental factors besides age may be important considerations when analyzing the effects of HAE and cognitive outcomes in youth contact sports. Indeed, this may be the most salient outcome.
Some inferential neurological support for these findings has been reported previously. Powers et al. demonstrated functional connectivity changes that appeared to be related to sub-concussive HAE in a similar age-cohort where the default mode network including hippocampus was implicated (Powers et al., 2018). In college athletes, McAllister et al. also demonstrated white matter disruption in hippocampal areas (McAllister et al., 2012, 2014).
Although the Rose et al. studies found very little effect of HAE on cognition in their analyses of youth football, the use of adjustments for test scores and normally distributed HAE metrics were possible improvements in this analysis (Rose et al., 2018, 2019). The different outcomes certainly bear further study.
As noted, the test score results reflected subtle changes from expectations with only small to medium group HAE effects on those scores. Clinical significance at the individual level was greater for the younger group but it is not possible to make any judgements as to effects beyond these score changes. In and of itself a score change may have several causes. Still, the fact that these changes had a statistically significant relationship to HAE raises some clinical concern. Whether this finding translates to short- or long-term functional outcomes deserves further studies
There are several caveats and limitations to be described. The cumulative exposure prior to the study was only estimated by parental reporting of the participant’s years of experience in any contact sport, thus a weak proxy for actual exposure. Analysis of that data did not find a significant difference between groups or an effect on outcomes. Interestingly, in a recently published study, Brett et al demonstrated small negative effects on neuropsychological test scores in retired football athletes who estimated the amount of lifetime HAE they received (N = 58). Lower test scores were related to years of play which was a proxy that weakly correlated with HAE.
The large reduction in sample size certainly impacted the analyses. Unfortunately, it was not possible to obtain any data or information about the causes of attrition.
Another potential modifier of exposure would be differences in coaching practice and skill technique that may have contributed systematically to the amount of HAE (Campolettano et al., 2016; Gellner et al., 2020; Kelley et al., 2019; Maerlender, Masterson, et al., 2020). Further, the small sample size in season-two limits statistical power and may have reduced generalizability of findings; however, by replicating and extending findings from the original study with the same participants, confidence in the findings should be increased.
While it may be that findings from football are unique in sports due to the use of helmets, these data suggests that tolerability of HAE may be limited in youth. One implication of these findings appears to be support for reducing the amount of HAE in younger athletes (AAP American Academy of Pediatrics, 2015). Reducing HAE through rule changes and improved skill techniques are important but may not reduce risks sufficiently.
More research is clearly needed to confirm these findings and identify specific mediating and moderating factors that might be involved: how much exposure is safe, determining if accumulation has different effects on different stages of neural development; and can we identify low and high-risk individuals? Although the numbers of youth who have played youth football with no apparent harm is notable, a concern about cognitive test score changes and what this may mean in the longer term should be considered by clinicians and sports administrators who work with youth football teams and players.
Author Contributions
Conceptualization, A.M., P.B., S.M.D., J.C.and R.G.; Methodology, A.M. and E.S.; Software, A.A., S.R. and S.M.D.; Validation, A.M., A.A., S.R., J.S., S.M.D. and R.G.; Formal analysis, A.M. and E.S.; Investigation, J.S., J.C. and R.G.; Resources, S.R. and S.M.D.; Data curation, A.A.; Writing – original draft, A.M.; Writing – review & editing, A.M., E.S., P.B., J.U., J.S., S.M.D., J.C. and R.G..
Funding
Research reported in this publication was supported by the grant titled “Biomechanical Basis of Pediatric mTBI Due to Sports Related Concussion” (PI: Duma) from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R01NS094410.
Acknowledgments
We would like to thank the youth, parents and coaches for their time and effort participating in this project. Several members of the research team collected and input data: Eamon T. Campolettano and Ryan A. Gellner at Virginia Tech; Tina Strates, Emily Kieffer and Mireille E. Kelley at Wake Forest provided significant help.
Conflicts of Interest
Joseph J. Crisco, Richard M. Greenwald, Jonathan G. Beckwith, and Simbex have a 340 financial interest in the instruments (HIT System, Sideline Response System, Riddell, Inc) that were used to collect the biomechanical data reported in this study.
References
- AAP American Academy of Pediatrics. (2015). Tackling in Youth Football. Pediatrics, 136(5), e1419–e1430. [CrossRef]
- Alosco, M. L., Mez, J., Tripodis, Y., Kiernan, P. T., Abdolmohammadi, B., Murphy, L., Kowall, N. W., Stein, T. D., Huber, B. R., Goldstein, L. E., Cantu, R. C., Katz, D. I., Chaisson, C. E., Martin, B., Solomon, T. M., McClean, M. D., Daneshvar, D. H., Nowinski, C. J., Stern, R. A., & McKee, A. C. (2018). Age of first exposure to tackle football and chronic traumatic encephalopathy: Age of First Exposure to Football and CTE. Annals of Neurology, 83(5), 886–901. [CrossRef]
- Bahrami, N., Sharma, D., Rosenthal, S., Davenport, E. M., Urban, J. E., Wagner, B., Jung, Y., Vaughan, C. G., Gioia, G. A., Stitzel, J. D., Whitlow, C. T., & Maldjian, J. A. (2016). Subconcussive Head Impact Exposure and White Matter Tract Changes over a Single Season of Youth Football. Radiology, 281(3), 919–926. [CrossRef]
- Beckwith, J. G., Greenwald, R. M., & Chu, J. J. (2012). Measuring head kinematics in football: Correlation between the head impact telemetry system and hybrid III headform. Annals of Biomedical Engineering, 40(1), 237–248. [CrossRef]
- Brennan, J. H., Mitra, B., Synnot, A., McKenzie, J., Willmott, C., McIntosh, A. S., Maller, J. J., & Rosenfeld, J. V. (2017). Accelerometers for the Assessment of Concussion in Male Athletes: A Systematic Review and Meta-Analysis. Sports Medicine, 47(3), 469–478. [CrossRef]
- Broglio, S. P., Eckner, J. T., Martini, D., Sosnoff, J. J., Kutcher, J. S., & Randolph, C. (2011). Cumulative Head Impact Burden in High School Football. Journal of Neurotrauma, 28(10), 2069–2078. [CrossRef]
- Campolettano, E. T., Gellner, R. A., Smith, E. P., Bellamkonda, S., Tierney, C. T., Crisco, J. J., Jones, D. A., Kelley, M. E., Urban, J. E., Stitzel, J. D., Genemaras, A., Beckwith, J. G., Greenwald, R. M., Maerlender, A. C., Brolinson, P. G., Duma, S. M., & Rowson, S. (2020). Development of a Concussion Risk Function for a Youth Population Using Head Linear and Rotational Acceleration. Annals of Biomedical Engineering, 48(1), 92–103. [CrossRef]
- Campolettano, E. T., Rowson, S., & Duma, S. M. (2016). Drill-specific head impact exposure in youth football practice. Journal of Neurosurgery: Pediatrics, 18(5), 536–541. [CrossRef]
- Carlozzi, N. E., Beaumont, J. L., Tulsky, D. S., & Gershon, R. C. (2017). The NIH Toolbox Pattern Comparison Processing Speed Test: Normative Data. Mongraphs of the Society for Research in Child Development, 30(May 2015), 359–368. [CrossRef]
- Carlozzi, N. E., Tulsky, D. S., Kail, R. V., & Beaumont, J. L. (2013). NIH Toolbox cognition battery(CB): Measuring processing speed. Mongraphs of Thw Society for Research in Child Development, 78(4), 88–102. [CrossRef]
- Castellani, R. J., & Perry, G. (2017). Dementia Pugilistica Revisited. Journalof Alzheimers Disease, 60, 1209–1221.
- Chelune, G. (2003). Assessing reliable neuropsychological change. In Predictio in forensics and neuropsychology:sound statostocal practices (pp. 123–147). Lawrence Ehrlbaum.
- Cohen, J. (1988). Statistical Power Analysis for the Social Sciences: Vol. Second Ed. Lawrence Erlbaum Associates.
- Crisco, J. J., Fiore, R., Beckwith, J. G., Chu, J. J., Brolinson, G. P., Duma, S., McAllister, T. W., Duhaime, A. C., & Greenwald, R. M. (2010). Frequency and location of head impact exposures in individual collegiate football players. Journal of Athletic Training, 45(6), 549–559. [CrossRef]
- Duma, S. M., Manoogian, S. J., Bussone, W. R., Brolinson, P. G., Goforth, M. W., Donnenwerth, J. J., Greenwald, R. M., Chu, J. J., & Crisco, J. J. (2005). Analysis of Real-time Head Accelerations in Collegiate Football Players. Clinical Journal of Sport Medicine, 15(1), 3–8. [CrossRef]
- Funk, J. R., Duma, S. M., Manoogian, S. J., & Rowson, S. (2007). Biomechanical Risk Estimates for Mild Traumatic Brain Injury. Annual Proceedings / Association for the Advancement of Automotive Medicine, 51, 343–361.
- Funk, J. R., Rowson, S., Daniel, R. W., & Duma, S. (2012). Validation of concussion risk curves for collegiate football players derived from HITS data. Annals of Biomedical Engineering, 40(1), 79–89. [CrossRef]
- Gellner, R. A., Campolettano, E. T., & Rowson, S. (2020). Does tackling form affect head acceleration in youth football players? Proceedings of the Institution of Mechanical Engineers, Part P: Journal of Sports Engineering and Technology, 234(3), 257–267. [CrossRef]
- Greenwald, R. M., Gwin, J. T., Chu, J. J., & Crisco, J. J. (2008). Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery, 62(4), 789–798. [CrossRef]
- Gysland, S. M., Mihalik, J. P., Register-Mihalik, J. K., Trulock, S. C., Shields, E. W., & Guskiewicz, K. M. (2012). The relationship between subconcussive impacts and concussion history on clinical measures of neurologic function in collegiate football players. Annals of Biomedical Engineering, 40(1), 14–22. [CrossRef]
- Heilbronner, R. L., Sweet, J. J., Attix, D. K., Krull, K. R., Henry, G. K., & Hart, R. P. (2010). Official position of the American Academy of clinical neuropsychology on serial neuropsychological assessments: The utility and challenges of repeat test administrations in clinical and forensic contexts. Clinical Neuropsychologist, 24(8), 1267–1278. [CrossRef]
- Iverson, G. L., Terry, D. P., Caccese, J. B., Büttner, F., & Merz, Z. C. (2020). Age of First Exposure to Football Is Not Associated with Midlife Brain Health Problems. Journal of Neurotrauma, neu.2020.7041. [CrossRef]
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [CrossRef]
- Jang et al. - 2019—Differences in corpus callosum injury between cere.pdf. (n.d.).
- Jang, S. H., Kim, O. L., Kim, S. H., & Lee, H. D. (2019). Differences in corpus callosum injury between cerebral concussion and diffuse axonal injury. Medicine, 98(41), e17467. [CrossRef]
- Johnson, E. K., Dow, C., Lynch, R. T., & Hermann, B. P. (2006). Measuring clinical significance in rehabilitation research. Rehabilitation Counseling Bulletin, 50(1), 35–45. [CrossRef]
- Johnson et al. - 2013—Axonal pathology in traumatic brain injury.pdf. (n.d.).
- Johnson, V. E., Stewart, W., & Smith, D. H. (2013). Axonal pathology in traumatic brain injury. Experimental Neurology, 246, 35–43. [CrossRef]
- Kelley, M. E., Espeland, M. A., Flood, W. C., Powers, A. K., Whitlow, C. T., Maldjian, J. A., Stitzel, J. D., & Urban, J. E. (2019). Comparison of head impact exposure in practice drills among multiple youth football teams. Journal of Neurosurgery: Pediatrics, 23(3), 381–389. [CrossRef]
- Kercher, K., Steinfeldt, J. A., Macy, J. T., Ejima, K., & Kawata, K. (2020). Subconcussive head impact exposure between drill intensities in U.S. high school football. PLOS ONE, 15(8), e0237800. [CrossRef]
- Kleiven, S. (2013). Why Most Traumatic Brain Injuries are Not Caused by Linear Acceleration but Skull Fractures are. Frontiers in Bioengineering and Biotechnology, 1. [CrossRef]
- Kleiven—2013—Why Most Traumatic Brain Injuries are Not Caused b.pdf. (n.d.).
- Koo, T. K., & Li, M. Y. (2016). A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. Journal of Chiropractic Medicine, 15(2), 155–163. [CrossRef]
- Maerlender, A. (2018). The validity of neuropsychological tests in sports concussion assessment (Ch. 9). P. Arnette (Ed.). In Neuropsychological Perspectives in Sports Concussions. APA Press.
- Maerlender, A., Masterson, C. J., Norris, R., & Hinthorne, A. (2020). Validating Tackle Mechanics in American Football: Improving Safety and Performance. Annals of Biomedical Engineering. [CrossRef]
- Maerlender, A., Smith, E., Brolinson, P. G., Crisco, J., Urban, J., Ajamil, A., Rowson, S., Campolettano, E. T., Gellner, R. A., Bellamkonda, S., Kieffer, E., Kelley, M. E., Jones, D., Powers, A., Beckwith, J., Stitzel, J., Greenwald, R. M., & Duma, S. (2020). Neuropsychological Change After a Single Season of Head Impact Exposure in Youth Football. Journal of the International Neuropsychological Society, 1–11. [CrossRef]
- Mainwaring, L., Ferdinand Pennock, K. M., Mylabathula, S., & Alavie, B. Z. (2018). Subconcussive head impacts in sport: A systematic review of the evidence. International Journal of Psychophysiology, 132, 39–54. [CrossRef]
- Manual, R., Release, D., Consortium, W., Human, N. I. H., & Project, C. (2013). WU-Minn HCP Quarter 1 ( Q1 ) Data Release: Reference Manual. 1(March), 1–62.
- McAllister, T., & McCrea, M. (2017). Long-Term Cognitive and Neuropsychiatric Consequences of Repetitive Concussion and Head-Impact Exposure. Journal of Athletic Training, 52(3), 309–317. [CrossRef]
- McAllister, T. W., Flashman, L. A., Maerlender, A., Greenwald, R. M., Beckwith, J. G., Tosteson, T. D., Crisco, J. J., Brolinson, P. G., Duma, S. M., Duhaime, A.-C., Grove, M. R., & Turco, J. H. (2012). Cognitive effects of one season of head impacts in a cohort of collegiate contact sport athletes. Neurology, 78(22). [CrossRef]
- McAllister, T. W., Ford, J. C., Flashman, L. A., Maerlender, A., Greenwald, R. M., Beckwith, J. G., Bolander, R. P., Tosteson, T. D., Turco, J. H., Raman, R., & Jain, S. (2014). Effect of head impacts on diffusivity measures in a cohort of collegiate contact sport athletes. Neurology, 82(1). [CrossRef]
- McKee, A. C., Mez, J., Abdolmohammadi, B., Butler, M., Huber, B. R., Uretsky, M., Babcock, K., Cherry, J. D., Alvarez, V. E., Martin, B., Tripodis, Y., Palmisano, J. N., Cormier, K. A., Kubilus, C. A., Nicks, R., Kirsch, D., Mahar, I., McHale, L., Nowinski, C., … Alosco, M. L. (2023). Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts. JAMA Neurology. [CrossRef]
- Meaney and Smith—2011—Biomechanics of Concussion.pdf. (n.d.).
- Meaney, D. F., & Smith, D. H. (2011). Biomechanics of Concussion. Clinics in Sports Medicine, 30(1), 19–31. [CrossRef]
- Montenigro, P. H., Alosco, M., Martin, B. M., Daneshvar, D., Mez, J., Chaisson, C. E., Nowinski, C., AU, R., McKee, A. C., Cantu, R., McClean, M., Stern, R. A., & Troposdis, Y. (2016). Cumulative head impact exposure predicts later-life depression, apathy, executive dysfunction, and cognitive impairment in former high school and college football players. Journal of Neurotrauma, 34, 328–340.
- Powers, A., Murugesan, G. K., Saghafi, B., Montillo, A., Maldjian, J., Davenport, E., Wagner, B., Jones, D., Urban-Hobson, J., Stitzel, J., Whitlow, C., & Kelley, M. (2018). Single season changes in resting state network power and the connectivity between regions distinguish head impact exposure level in high school and youth football players. In K. Mori & N. Petrick (Eds.), Medical Imaging 2018: Computer-Aided Diagnosis (p. 14). SPIE. [CrossRef]
- Rose, S. C., Yeates, K. O., Fuerst, D. R., Ercole, P. M., Nguyen, J. T., & Pizzimenti, N. M. (2018). Head Impact Burden and Change in Neurocognitive Function During a Season of Youth Football: Journal of Head Trauma Rehabilitation, 34(2), 87–95. [CrossRef]
- Rose, S. C., Yeates, K. O., Nguyen, J. T., McCarthy, M. T., Ercole, P. M., & Pizzimenti, N. M. (2019). Neurocognitive Function and Head Impact Burden over Two Seasons of Youth Tackle Football. Journal of Neurotrauma, 36(19), 2803–2809. [CrossRef]
- Schatz, P., & Maerlender, A. (2013). A Two-Factor Theory for Concussion Assessment Using ImPACT: Memory and Speed. Archives of Clinical Neuropsychology, 28(8), 791–797. [CrossRef]
- Shrout, P., & Fleiss, J. (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428.
- Solomon, G. (2018). Chronic traumatic encephalopathy in sports: A historical and narrative review. Developmental Neuropsychology, 1–33. [CrossRef]
- Stamm, J. M., Bourlas, A. P., Baugh, C. M., Fritts, N. G., Daneshvar, D. H., Martin, B. M., McClean, M. D., Tripodis, Y., & Stern, R. A. (2015). Age of first exposure to football and later-life cognitive impairment in former NFL players. Neurology, 84, 1114–1120. [CrossRef]
- Temkin, N. R., Heaton, R. K., Grant, I., & Dikmen, S. S. (1999). Detecting significant change in neuropsychological test performance: A comparison of four models. J Int Neuropsychol Soc, 5(4), 357–369. [CrossRef]
- Tulsky, D., Carlozzi, N., Beaumont, J., & Mugas. (2013). NIH Toolbox cognitive functioning battery: Measuring working memory. Mongraphs of the Society for Research in Child Development, 78(4), 70–87. [CrossRef]
- Tulsky, D., Carlozzi, N., Holdnack, J., Heaton, R., Wong, A., Goldsmith, A., & Heinemann, A. (2017). Using the NIH Toolbox Cognition Battery ( NIHTB-CB ) in Individuals With Traumatic Brain Injury. Rehabilitation Psychology, 62, 413–424.
- Wilcox, B. J., Beckwith, J. G., Greenwald, R. M., Raukar, N. P., Chu, J. J., McAllister, T. W., Flashman, L. A., Maerlender, A. C., Duhaime, A.-C., & Crisco, J. J. (2015). Biomechanics of head impacts associated with diagnosed concussion in female collegiate ice hockey players. Journal of Biomechanics, 48(10). [CrossRef]
- Zelazo, P. D., Anderson, J. E., Richler, J., Wallner-allen, K., Beaumont, J. L., & Weintraub, S. (2013). II. NIH Toolbox Cognition Battery ( CB): Measuring Executive Function and Attention. Mongraphs of the Society for Research in Child Development, 78, 16–33.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).