Submitted:
12 September 2024
Posted:
13 September 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Objective
Conceptual Framework
Language
Methods
Protocol
Identification of Relevant Studies
Study Selection
Data Charting
Collating, Summarising, and Reporting Results
Trustworthiness and Rigour
Ethics Approval
Results
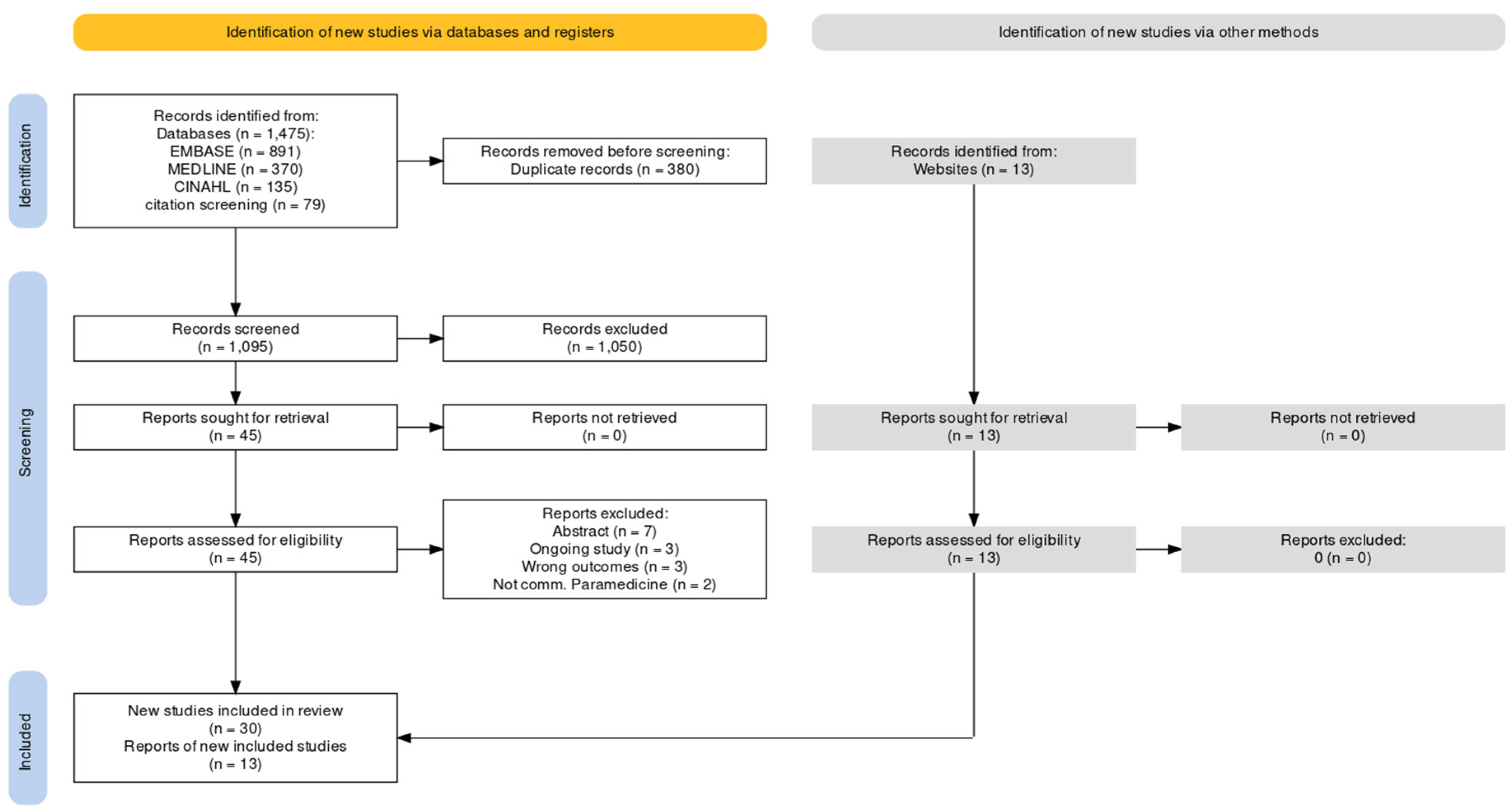
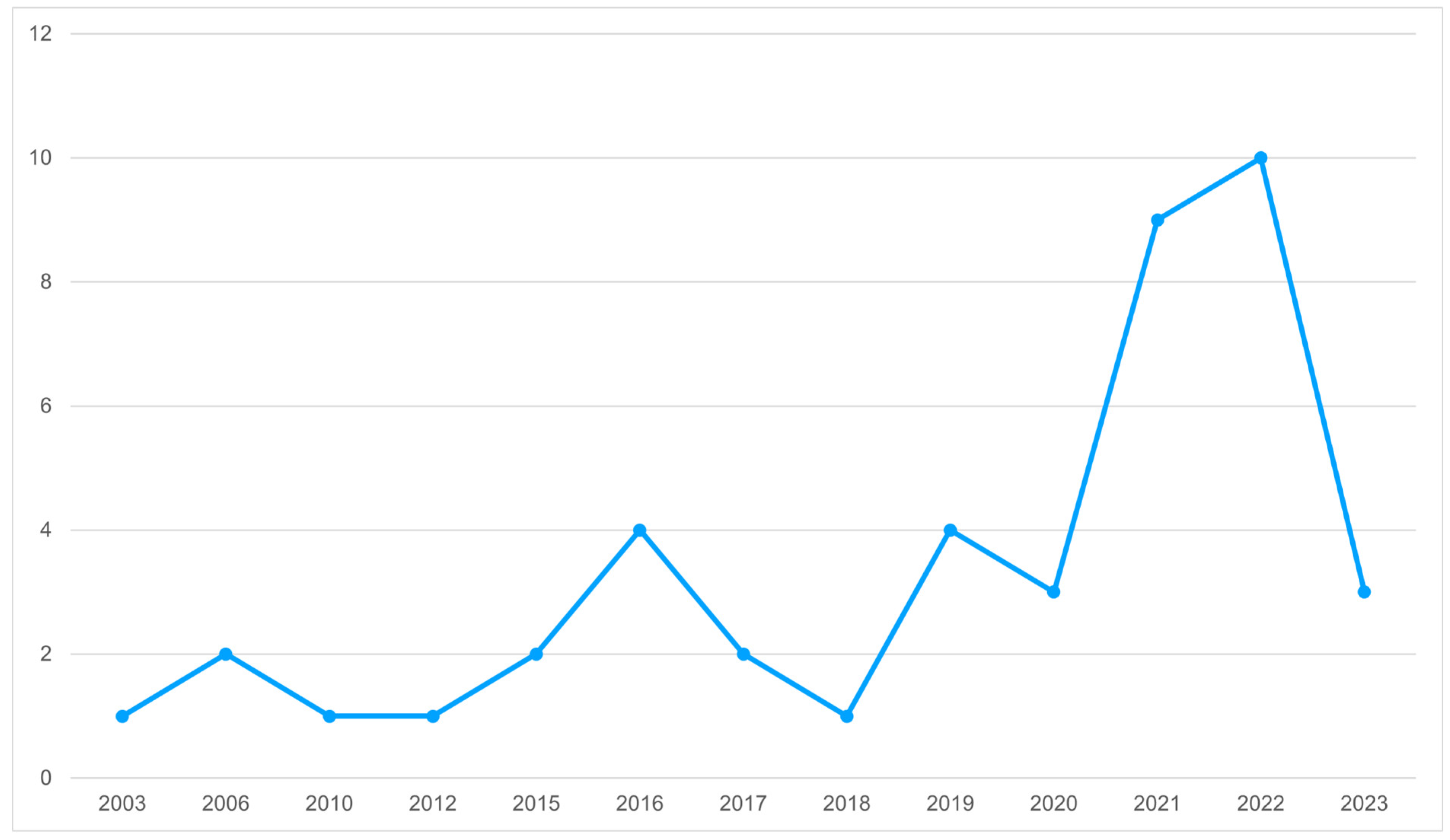
Identification of Potential Studies
Economic Security and Equality
Education
Physical Environment
Social and Community Context
Health Behaviours
Health care
Community Needs Assessment
Social Needs Education
Discussion
Future Directions
Limitations
Conclusion
Supplementary Materials
Author Contributions
Data Availability Statement
Preprint
Acknowledgements
Statements and Declarations
References
- Allana, A., & Pinto, A. (2021). Paramedics Have Untapped Potential to Address Social Determinants of Health in Canada. Healthcare Policy | Politiques de Santé, 16(3), 67–75. https://doi.org/10.12927/hcpol.2021.26432.
- Shannon, B., Eaton, G., Lanos, C., Leyenaar, M., Nolan, M., Bowles, K.-A., … Batt, A. (2022). The development of community paramedicine; a restricted review. Health & Social Care in the Community, 30(6), e3547–e3561. https://doi.org/10.1111/hsc.13985.
- CSA Group. (2017). CAN/CSA Z1630:17 Community paramedicine: Framework for program development. Toronto: CSA Group.
- Shannon, B., Baldry, S., O’Meara, P., Foster, N., Martin, A., Cook, M., … Miles, A. (2023). The definition of a community paramedic: An international consensus. Paramedicine, 20(1), 4–22. https://doi.org/10.1177/27536386221148993.
- Essington, T., Bowles, R., & Donelon, B. (2018). The Canadian Paramedicine Education Guidance Document. Ottawa: Paramedic Association of Canada.
- World Health Organization. (2008). Closing the gap in a generation: health equity through action on the social determinants of health - Final report of the commission on social determinants of health. Geneva: World Health Organization. Retrieved from https://www.who.int/publications-detail-redirect/WHO-IER-CSDH-08.1.
- Porroche-Escudero, A. (2022). Health systems and quality of healthcare: bringing back missing discussions about gender and sexuality. Health Systems, 1–7. https://doi.org/10.1080/20476965.2022.2096487.
- IISD. (2023, June 7). Who Is Being Left Behind in Canada? International Institute for Sustainable Development. International Institute for Sustainable Development. Retrieved March 31, 2023, from https://www.iisd.org/articles/insight/who-being-left-behind-canada.
- Truth and Reconciliation Commission of Canada. (2015). Honouring the truth, reconciling for the future: summary of the final report of the Truth and Reconciliation Commission of Canada. Retrieved from http://epe.lac-bac.gc.ca/100/201/301/weekly_acquisition_lists/2015/w15-24-F-E.html/collections/collection_2015/trc/IR4-7-2015-eng.pdf.
- Arksey, H., & O’Malley, L. (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616.
- Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. https://doi.org/10.1186/s12874-018-0611-x.
- Shannon, B., Batt, A. M., Eaton, G., Bowles, K.-A., & Williams, B. (2021). Community Paramedicine Practice Framework Scoping Exercise. Retrieved from https://www.phecit.ie/Custom/BSIDocumentSelector/Pages/DocumentViewer.aspx?id=oGsVrspmiT0dOhDFFXZvIz0q5GYO7igwzB6buxHEgeAwoe6hhx3Qzd%252fCRqybt66szE0PsYSC8wDndnJ4ZZBtixIuvZKX1%252f4wN58oIZl8uwPebsYwRo0IvX6hVCWn5T8FxWsBQJfWSaVSf%252bRJ%252b80BMTb0c8d%252b63Hj.
- Tavares, W., Bowles, R., & Donelon, B. (2016). Informing a Canadian paramedic profile: framing concepts, roles and crosscutting themes. BMC Health Services Research, 16(1), 477. https://doi.org/10.1186/s12913-016-1739-1.
- Tavares, W., Allana, A., Beaune, L., Weiss, D., & Blanchard, I. (2021). Principles to Guide the Future of Paramedicine in Canada. Prehospital Emergency Care, 1–11. https://doi.org/10.1080/10903127.2021.1965680.
- Cho, S., Crenshaw, K. W., & McCall, L. (2013). Toward a Field of Intersectionality Studies: Theory, Applications, and Praxis. Signs: Journal of Women in Culture and Society, 38(4), 785–810. https://doi.org/10.1086/669608.
- Nixon, S. A. (2019). The coin model of privilege and critical allyship: implications for health. BMC Public Health, 19(1), 1637. https://doi.org/10.1186/s12889-019-7884-9.
- Peters, M. D., Godfrey, C., McInerney, P., Munn, Z., Tricco, A. C., & Khalil, H. (2024). 10. Scoping reviews. In E. Aromataris, C. Lockwood, K. Porritt, B. Pilla, & Z. Jordan (Eds.), JBI Manual for Evidence Synthesis. JBI. https://doi.org/10.46658/JBIMES-24-09.
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., … Straus, S. E. (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850.
- Grey Matters: a practical tool for searching health-related grey literature | CADTH. (n.d.). Retrieved June 11, 2023, from https://www.cadth.ca/grey-matters-practical-tool-searching-health-related-grey-literature.
- Haddaway, N. R., Grainger, M. J., & Gray, C. T. (2021, February 16). citationchaser: An R package and Shiny app for forward and backward citations chasing in academic searching. Zenodo. https://doi.org/10.5281/zenodo.4543513.
- Peters, M. D. J., Marnie, C., Tricco, A. C., Pollock, D., Munn, Z., Alexander, L., … Khalil, H. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis, 18(10), 2119–2126. https://doi.org/10.11124/JBIES-20-00167.
- World Health Organization. (2024). Operational framework for monitoring social determinants of health equity. Geneva, Switzerland: World Health Organization. Retrieved from https://www.who.int/publications-detail-redirect/9789240088320.
- Thomas, E., & Magilvy, J. K. (2011). Qualitative Rigor or Research Validity in Qualitative Research. Journal for Specialists in Pediatric Nursing, 16(2), 151–155. https://doi.org/10.1111/j.1744-6155.2011.00283.x.
- Batt, A. M., Williams, B., Brydges, M., Leyenaar, M., & Tavares, W. (2021). New ways of seeing: supplementing existing competency framework development guidelines with systems thinking. Advances in Health Sciences Education. https://doi.org/10.1007/s10459-021-10054-x.
- Friedman, B. (1997). Systems theory. In Theories and practice in social work (In J. Brandall., pp. 3–17). The Free Press.
- Sturmberg, J. P. (2007). Part 1 clinical application. Australian Family Physician, 36(3), 170–173.
- Kannampallil, T. G., Schauer, G. F., Cohen, T., & Patel, V. L. (2011). Considering complexity in healthcare systems. Journal of Biomedical Informatics, 44(6), 943–947. https://doi.org/10.1016/j.jbi.2011.06.006.
- Taplin, J., Dalgarno, D., Smith, M., Eggenberger, T., & Ghosh, S. M. (2023). Community paramedic outreach support for people experiencing homelessness. Journal of Paramedic Practice, 15(2).
- Moczygemba, L. R., Thurman, W., Tormey, K., Hudzik, A., Welton-Arndt, L., & Kim, E. (2021). GPS Mobile Health Intervention Among People Experiencing Homelessness: Pre-Post Study. JMIR mHealth and uHealth, 9(11), e25553. https://doi.org/10.2196/25553.
- Taplin, J. G., Barnabe, C. M., Blanchard, I. E., Doig, C. J., Crowshoe, L., & Clement, F. M. (2022). Health service utilization by people experiencing homelessness and engaging with community paramedics: a pre–post study. Canadian Journal of Emergency Medicine, 24(8), 885–889. https://doi.org/10.1007/s43678-022-00387-w.
- Ridgeway, J. L., Wissler Gerdes, E. O., Zhu, X., Finnie, D. M., Wiepert, L. M., Glasgow, A. E., … McCoy, R. G. (2023). A Community Paramedic Clinic at a Day Center for Adults Experiencing Homelessness. NEJM Catalyst, 4(4). https://doi.org/10.1056/CAT.22.0300.
- Stickler, Z. R., Carlson, P. N., Myers, L., Schultz, J. R., Swenson, T., Darling, C., … McCoy, R. G. (2021). Community Paramedic Mobile COVID-19 Unit Serving People Experiencing Homelessness. The Annals of Family Medicine, 19(6), 562–562. https://doi.org/10.1370/afm.2709.
- Ruest, M. (2016). County of Renfrew Paramedic Service Resilience Program Contribution to the Health Promotion Strategies that Address the Inequities Associated with Social Isolation of Seniors in the County of Renfrew. Canadian Paramedicine, 39(3).
- Cockrell, K. R., Reed, B., & Wilson, L. (2019). Rural paramedics’ capacity for utilising a salutogenic approach to healthcare delivery: a literature review. Australasian Journal of Paramedicine, 16. https://doi.org/10.33151/ajp.16.635.
- Georgiev, R., Stryckman, B., & Velez, R. (2019). The Integral Role of Nurse Practitioners in Community Paramedicine. The Journal for Nurse Practitioners, 15(10), 725–731. https://doi.org/10.1016/j.nurpra.2019.07.019.
- Langabeer, J. R., Persse, D., Yatsco, A., O’Neal, M. M., & Champagne-Langabeer, T. (2021). A Framework for EMS Outreach for Drug Overdose Survivors: A Case Report of the Houston Emergency Opioid Engagement System. Prehospital Emergency Care, 25(3), 441–448. https://doi.org/10.1080/10903127.2020.1755755.
- Thomas-Henkel, C., & Schulman, M. (n.d.). Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations.
- Pirrie, M., Harrison, L., Angeles, R., Marzanek, F., Ziesmann, A., & Agarwal, G. (2020). Poverty and food insecurity of older adults living in social housing in Ontario: a cross-sectional study. BMC Public Health, 20(1), 1320. https://doi.org/10.1186/s12889-020-09437-3.
- Swayze, D. (2017). The Community Paramedicine Approach to the Opioid Epidemic. JEMS: EMS, Emergency Medical Services - Training, Paramedic, EMT News. Retrieved from https://www.jems.com/mobile-integrated-healthcare/the-community-paramedicine-approach-to-the-opioid-epidemic/.
- Leyenaar, M. S., McLeod, B., Jones, A., Brousseau, A.-A., Mercier, E., Strum, R. P., … Costa, A. P. (2021). Paramedics assessing patients with complex comorbidities in community settings: results from the CARPE study. Canadian Journal of Emergency Medicine, 23(6), 828–836. https://doi.org/10.1007/s43678-021-00153-4.
- Naimi, S., Stryckman, B., Liang, Y., Seidl, K., Harris, E., Landi, C., … Gingold, D. B. (2023). Evaluating Social Determinants of Health in a Mobile Integrated Healthcare-Community Paramedicine Program. Journal of Community Health, 48(1), 79–88. https://doi.org/10.1007/s10900-022-01148-7.
- Sokan, O., Stryckman, B., Liang, Y., Osotimehin, S., Gingold, D. B., Blakeslee, W. W., … Rodriguez, M. (2022). Impact of a mobile integrated healthcare and community paramedicine program on improving medication adherence in patients with heart failure and chronic obstructive pulmonary disease after hospital discharge: A pilot study. Exploratory Research in Clinical and Social Pharmacy, 8, 100201. https://doi.org/10.1016/j.rcsop.2022.100201.
- Olynyk, C. (2010). Toronto EMS Community Paramedicine Program Overview 2010. Toronto, Canada. Retrieved from https://ircp.info/Portals/11/Downloads/Expanded%20Role/Toronto%20CREMS/Toronto%20EMS%20Community%20Paramedicine%20Program%20Overview%202010.pdf?ver=Vn9xFmVDYfFxk0pJG0QiFw%3d%3d.
- Schwab-Reese, L. M., Renner, L. M., King, H., Miller, R. P., Forman, D., Krumenacker, J. S., & DeMaria, A. L. (2021). “They’re very passionate about making sure that women stay healthy”: a qualitative examination of women’s experiences participating in a community paramedicine program. BMC Health Services Research, 21(1), 1167. https://doi.org/10.1186/s12913-021-07192-8.
- Pennel, C. L., Tamayo, L., Wells, R., & Sunbury, T. (2016). Emergency Medical Service-based Care Coordination for Three Rural Communities. Journal of Health Care for the Poor and Underserved, 27(4A), 159–180. https://doi.org/10.1353/hpu.2016.0178.
- Batt, A. M., Hultink, A., Lanos, C., Tierney, B., Grenier, M., & Heffern, J. (2021). Advances in Community Paramedicine in Response to COVID-19.
- Boland, L. L., Jin, D., Hedger, K. P., Lick, C. J., Duren, J. L., & Stevens, A. C. (2022). Evaluation of an EMS-Based Community Paramedic Pilot Program to Reduce Frequency of 9-1-1 Calls among High Utilizers. Prehospital Emergency Care, 1–8. https://doi.org/10.1080/10903127.2022.2086653.
- Logan, R. I. (2022). ‘I Certainly Wasn’t as Patient-Centred’: Impacts and Potentials of Cross-Training Paramedics as Community Health Workers. Anthropology in Action, 29(3), 14–22. https://doi.org/10.3167/aia.2022.290302.
- McManamny, T. E., Boyd, L., Sheen, J., & Lowthian, J. A. (2022). Feasibility and acceptability of paramedic-initiated health education for rural-dwelling older people. Health Education Journal, 81(7), 848–861. https://doi.org/10.1177/00178969221125622.
- Mund, E. (2016). Taking Care to the Streets. EMSWorld. Retrieved from https://lw.hmpgloballearningnetwork.com/site/emsworld/article/12179630/taking-mih-cp-care-to-the-streets.
- Rahim, F., Jain, B., Patel, T., Jain, U., Jain, P., & Palakodeti, S. (2022). Community Paramedicine: An Innovative Model for Value-Based Care Delivery. Journal of Public Health Management and Practice, Publish Ahead of Print. https://doi.org/10.1097/PHH.0000000000001683.
- Gainey, C. E., Brown, H. A., & Gerard, W. C. (2018). Utilization of Mobile Integrated Health Providers During a Flood Disaster in South Carolina (USA). Prehospital and Disaster Medicine, 33(4), 432–435. https://doi.org/10.1017/S1049023X18000572.
- Strum, R. (2015). Paramedics as Health Advocates. Canadian Paramedicine, 38(6).
- Newall, N. (2015). Who’s At My Door Project: How organizations find and assist socially isolated older adults (p. 44). Winnipeg, Manitoba: Centre on Aging. Retrieved from https://umanitoba.ca/centre-on-aging/sites/centre-on-aging/files/2021-02/centre-aging-research-publications-report-who%27s-at-my-door-project.pdf.
- Nolan, M., Hillier, T., & D’Angelo, C. (2012). Community Paramedicine in Canada. Retrieved from https://ircp.info/Portals/11/Downloads/Policy/Comm%20Paramedicine%20in%20Canada.pdf?ver=XJMZv0HNBUMEpxqc9etOFg%3d%3d.
- Raven, S., Tippett, V., Ferguson, J.-G., & Smith, S. (2006). An exploration of expanded paramedic healthcare roles for Queensland (p. 100). Queensland, Australia: Australian Centre for Prehospital Research. Retrieved from https://ircp.info/portals/11/downloads/expanded%20role/queensland%20expanded%20role.pdf.
- Hay, D., Varga-Toth, J., & Hines, E. (2006). Frontline Health Care in Canada: Innovations in Delivering Services to Vulnerable Populations (Rresearch Report No. F, 63) (p. 96).
- PHECC. (2020). The introduction of Community Paramedicine into Ireland. Retrieved from https://www.phecit.ie/Custom/BSIDocumentSelector/Pages/DocumentViewer.aspx?id=oGsVrspmiT0dOhDFFXZvIz0q5GYO7igwzB6buxHEgeDKMmmW%252fnE3lbsxRkYxd6aQYk7snfcymr0EG16DvMZvqmNsz5SqfTY2bCjDsrkmvfchr0f6fWdxsRfEpP0eHF2WFYnnA1HA6sq8buhbiuE7hUxFSMEFO%252btRyWB31RTiP1quSbFCsa%252bZGt6Ri4g1h1nnWZcXksZCSqw%253d.
- Ashton, C., & Leyenaar, M. S. (2019). Health Service Needs in the North: A Case Study on CSA Standard for Community Paramedicine. Canada: Canadian Standards Association. Retrieved from https://www.csagroup.org/wp-content/uploads/CSA-Group-Research-Health-Service-Needs-in-the-North-1.pdf.
- Ford-Jones, P. C., & Daly, T. (2022). Filling the gap: Mental health and psychosocial paramedicine programming in Ontario, Canada. Health & Social Care in the Community, 30(2), 744–752. https://doi.org/10.1111/hsc.13189.
- Misner, D. (2003). Community Paramedicine: A Part of an Integrated Health Care System. Retrieved from https://ircp.info/Portals/11/Downloads/Expanded%20Role/Community%20Paramedicine.pdf?ver=TfO8p2_1qDzq4LlLyNLlqA%3d%3d.
- Buitrago, I., Seidl, K. L., Gingold, D. B., & Marcozzi, D. (2022). Analysis of Readmissions in a Mobile Integrated Health Transitional Care Program Using Root Cause Analysis and Common Cause Analysis. Journal for Healthcare Quality, 44(3), 169–177. https://doi.org/10.1097/JHQ.0000000000000328.
- Hirello, L., & Cameron, C. (2021). Improving Paramedicine through Social Accountability. Canadian Paramedicine, 44(3). Retrieved from https://canadianparamedicine.ca/special-editions/.
- Chan, J., Griffith, L. E., Costa, A. P., Leyenaar, M. S., & Agarwal, G. (2019). Community paramedicine: A systematic review of program descriptions and training. CJEM, 21(6), 749–761. https://doi.org/10.1017/cem.2019.14.
- PHECC. (2022). Community Paramedicine in Ireland: a framework for the specialist paramedic. Retrieved from https://www.phecit.ie/Custom/BSIDocumentSelector/Pages/DocumentViewer.aspx?id=oGsVrspmiT0dOhDFFXZvIz0q5GYO7igwzB6buxHEgeDq00klOJxrAiwRg8WilA7iQpuh0JuuyxLZ%252fgoqHj9YAdVJBi%252feIjLQQQejAdgErxHc1gOlnYuCfGcZtM%252fFZTDuGELCeo4hOpwR2WpMNptaZMMl%252biPM01lTiSTAjYn0UiWidbzfXGJzNluN5VUHbqIsRWHtJZQ5aTg%253d.
- Agarwal, G., Lee, J., McLeod, B., Mahmuda, S., Howard, M., Cockrell, K., & Angeles, R. (2019). Social factors in frequent callers: a description of isolation, poverty and quality of life in those calling emergency medical services frequently. BMC Public Health, 19(1), 684. https://doi.org/10.1186/s12889-019-6964-1.
- Agarwal, G., & Brydges, M. (2018). Effects of a community health promotion program on social factors in a vulnerable older adult population residing in social housing. BMC Geriatrics, 18(1), 95. https://doi.org/10.1186/s12877-018-0764-9.
- Agarwal, G., Keenan, A., Pirrie, M., & Marzanek-Lefebvre, F. (2022). Integrating community paramedicine with primary health care: a qualitative study of community paramedic views. CMAJ Open, 10(2). https://doi.org/10.9778/cmajo.20210179.
- Bolster, J., Batt, A. M., & Pithia, P. (2022). Emerging Concepts in the Paramedicine Literature to Inform the Revision of a Pan-Canadian Competency Framework for Paramedics: A Restricted Review. https://doi.org/10.7759/cureus.32864.
- Batt, A. M., Bank, J., Bolster, J., & Pithia, P. (2023). Canadian Paramedic Landscape Review and Standards Roadmap. Toronto: CSA Group. Retrieved from https://www.csagroup.org/article/research/canadian-paramedic-landscape-review-and-standards-roadmap/.
- First Nation Information Governance Centre. (n.d.). OCAP Principles. The First Nations Information Governance Centre. Canada. Retrieved June 11, 2023, from https://fnigc.ca/.
- Rosa, A., Dissanayake, M., Carter, D., & Sibbald, S. (2022). Community paramedicine to support palliative care. Progress in Palliative Care, 30(1), 11–15. https://doi.org/10.1080/09699260.2021.1912690.
- Gebhard, A., McLean, S., & St Denis, V. (2022). White benevolence: racism and colonial violence in the helping professions. Canada: Fernwood Publishing Company.
- O’Meara, P., Ruest, M., & Stirling, C. (2014). Community Paramedicine: Higher Education as An Enabling Factor. Australasian Journal of Paramedicine, 11, 1–9. https://doi.org/10.33151/ajp.11.2.22.
- NAEMSE. (2023). NAEMSE Consensus Statement on Diversity, Equity, Inclusion, and Belonging. Prehospital Emergency Care. Retrieved from https://www.tandfonline.com/doi/pdf/10.1080/10903127.2023.2212753?download=true.
- Alsan, M., Garrick, O., & Graziani, G. (2019). Does Diversity Matter for Health? Experimental Evidence from Oakland. American Economic Review, 109(12), 4071–4111. https://doi.org/10.1257/aer.20181446.
- Crowe, R. P., Krebs, W., Cash, R. E., Rivard, M. K., Lincoln, E. W., & Panchal, A. R. (2020). Females and Minority Racial/Ethnic Groups Remain Underrepresented in Emergency Medical Services: A Ten-Year Assessment, 2008–2017. Prehospital Emergency Care, 24(2), 180–187. https://doi.org/10.1080/10903127.2019.1634167.
- Rosenkranz, K. M., Arora, T. K., Termuhlen, P. M., Stain, S. C., Misra, S., Dent, D., & Nfonsam, V. (2021). Diversity, Equity and Inclusion in Medicine: Why It Matters and How do We Achieve It? Journal of Surgical Education, 78(4), 1058–1065. https://doi.org/10.1016/j.jsurg.2020.11.013.
- Rudman, J. S., Farcas, A., Salazar, G. A., Hoff, J., Crowe, R. P., Whitten-Chung, K., … Joiner, A. P. (2023). Diversity, Equity, and Inclusion in the United States Emergency Medical Services Workforce: A Scoping Review. Prehospital Emergency Care, 27(4), 385–397. https://doi.org/10.1080/10903127.2022.2130485.
- Metzl, J. M., & Hansen, H. (2014). Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine, 103, 126–133. https://doi.org/10.1016/j.socscimed.2013.06.032.
- Castillo, E. G., Isom, J., DeBonis, K. L., Jordan, A., Braslow, J. T., & Rohrbaugh, R. (2020). Reconsidering Systems-Based Practice: Advancing Structural Competency, Health Equity, and Social Responsibility in Graduate Medical Education. Academic Medicine, 95(12), 1817–1822. https://doi.org/10.1097/ACM.0000000000003559.
- Coletto, D. (2023, June 8). Canadians Are Ready for Paramedics to Do More in Healthcare: Abacus Data Poll. Retrieved June 9, 2023, from https://abacusdata.ca/pac-2023/.
- Allana, A., Tavares, W., Pinto, A. D., & Kuluski, K. (2022). Designing and Governing Responsive Local Care Systems – Insights from a Scoping Review of Paramedics in Integrated Models of Care. International Journal of Integrated Care, 22(2), 5, 1–19. https://doi. org/10.5334/ijic.6418.
- Taplin, J. G., Bill, L., Blanchard, I. E., Barnabe, C. M., Holroyd, B. R., Healy, B., & McLane, P. (2023). Exploring paramedic care for First Nations in Alberta: a qualitative study. CMAJ Open, 11(6), E1135–E1147. https://doi.org/10.9778/cmajo.20230039.
- Allan, B. (2015). First Peoples, Second Class Treatment. Toronto: Li Ka Shing Knowledge Institute. Retrieved from https://www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf.
- Lunn, T., Bolster, J., & Batt, A. (2024, February 13). Community Paramedicine Supporting Community Needs: A Scoping Review. Preprints. https://doi.org/10.20944/preprints202310.0999.v2.

| Author - Year | Location | Publication Title |
|---|---|---|
| Allana & Pinto 2021 | Canada | Paramedics Have Untapped Potential to Address Social Determinants of Health in Canada |
| Boland et al. 2022 | United States | Evaluation of an EMS-Based Community Paramedic Pilot Program to Reduce Frequency of 9-1-1 Calls among High Utilizers |
| Buitrago et al. 2022 | United States | Analysis of Readmissions in a Mobile Integrated Health Transitional Care Program Using Root Cause Analysis and Common Cause Analysis |
| Chan et al. 2019 | Canada | Community paramedicine: A systematic review of program descriptions and training |
| Cockrell et al. 2019 | Australia | Rural paramedics’ capacity for utilising a salutogenic approach to healthcare delivery: a literature review |
| Ford-Jones & Daly 2022 | Canada | Filling the gap: Mental health and psychosocial paramedicine programming in Ontario, Canada |
| Gainey et al. 2018 | United States | Utilization of Mobile Integrated Health Providers During a Flood Disaster in South Carolina (USA) |
| Georgiev et al. 2019 | United States | The Integral Role of Nurse Practitioners in Community Paramedicine |
| Hirello & Cameron 2021 | Canada | Improving Paramedicine Practice Through Social Accountability |
| Langabeer et al. 2020 | United States | A Framework for EMS Outreach for Drug Overdose Survivors: A Case Report of the Houston Emergency Opioid Engagement System |
| Leyenaar et al. 2021 | Canada | Paramedics assessing patients with complex comorbidities in community settings: results from the CARPE study |
| Logan 2022 | United States | ‘I Certainly Wasn’t as Patient-Centred’ Impacts and Potentials of Cross-Training Paramedics as Community Health Workers |
| McManamny et al. 2022 | Australia | Feasibility and acceptability of paramedic-initiated health education for rural-dwelling older people |
| Moczygemba et al. 2021 | United States | GPS Mobile Health Intervention Among People Experiencing Homelessness: Pre-Post Study |
| Mund 2016 | United States | Taking Care to the Streets |
| Naimi et al. 2023 | United States | Evaluating Social Determinants of Health in a Mobile Integrated Healthcare-Community Paramedicine Program |
| Pennel et al. 2016 | United States | Emergency Medical Service- based Care Coordination for Three Rural Communities |
| Pirrie et al. 2020 | Canada | Poverty and food insecurity of older adults living in social housing in Ontario: a cross-sectional study |
| Rahim et al. 2022 | United States | Community Paramedicine: An Innovative Model for Value-Based Care Delivery |
| Ridgeway et al. 2023 | United States | A Community Paramedic Clinic at a Day Center for Adults Experiencing Homelessness |
| Rosa et al. 2021 | Canada | Community paramedicine to support palliative care |
| Ruest 2016 | Canada | County of Renfrew Paramedic Service Paramedic Resilience Program Contribution to the Health Promotion Strategies that Address the Inequities Associated with Social Isolation of Seniors in the County of Renfrew |
| Schwab-Reese et al. 2021 | United States | “They’re very passionate about making sure that women stay healthy”: a qualitative examination of women’s experiences participating in a community paramedicine program |
| Shannon et al. 2022 | Australia | The development of community paramedicine; a restricted review |
| Sokan et al. 2022 | United States | Impact of a mobile integrated healthcare and community paramedicine program on improving medication adherence in patients with heart failure and chronic obstructive pulmonary disease after hospital discharge: A pilot study |
| Stickler et al. 2021 | United States | Community Paramedic Mobile COVID-19 Unit Serving People Experiencing Homelessness |
| Strum 2015 | Canada | Paramedics as Health Advocates: Populations of Low Social Determinants of Health |
| Swayze 2016 | United States | Chronic Disease Management for the Community Paramedic |
| Taplin et al. 2022 | Canada | Health service utilization by people experiencing homelessness and engaging with community paramedics: a pre–post study |
| Taplin et al. 2023 | Canada | Community paramedic outreach support for people experiencing homelessness |
| Newall 2015 | Canada | Who’s At My Door Project - How Organizations Find and Assist Socially Isolated Older Adults |
| Raven et al. 2006 | Australia | An exploration of expanded paramedic healthcare roles for Queensland |
| Thomas-Henkel & Schluman 2017 | United States | Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations |
| Olynyk 2010 | Canada | Community Referrals by EMS - an extension of service |
| Nolan et al. 2012 | Canada | Community Paramedicine in Canada |
| Misner 2003 | Canada | Community Paramedicine: A Part of an Integrated Health Care System |
| Hay et al. 2006 | Canada | Frontline Health Care in Canada: Innovations in Delivering Services to Vulnerable Populations |
| Ashton & Leyenaar 2019 | Canada | Health Services Needs in the North: a case study on CSA standard for community paramedicine |
| CSA Group 2017 | Canada | Community paramedicine: Framework for program development |
| Batt et al. 2021 | Canada | Advances in Community Paramedicine in Response to COVID-19 |
| PHECC 2020 | Ireland | The introduction of Community Paramedicine into Ireland |
| Shannon et al. 2021 | Australia | Community Paramedicine Practice Framework Scoping Exercise |
| PHECC 2022 | Ireland | Community Paramedicine in Ireland: a framework for the specialist paramedic |
| Framework category | Economic security and equality | Education | Physical environment | Social and community context | Health behaviours | Health care |
|---|---|---|---|---|---|---|
| Included codes |
|
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





