Submitted:
13 October 2023
Posted:
17 October 2023
You are already at the latest version
Abstract
Keywords:
Background
Case presentation
Discussion
Funding
Conflicts of Interest
References
- Kalayanarooj, S. Clinical Manifestations and Management of Dengue/DHF/DSS. TropMedHealth. 2011, 39 (4SUPPLEMENT), S83–S87. [Google Scholar] [CrossRef]
- de Azeredo, E.L.; Monteiro, R.Q.; de-Oliveira Pinto, L.M. Thrombocytopenia in Dengue: Interrelationship between Virus and the Imbalance between Coagulation and Fibrinolysis and Inflammatory Mediators. Yeh TM, editor. Mediators of Inflammation. 2015, 2015, 313842. [Google Scholar] [CrossRef]
- Aktürk, O.M.; Kayılıoğlu, S.I.; Aydoğan, İ.; Dinç, T.; Yildiz, B.; Cete, M.; et al. Spontaneous Rectus Sheath Hematoma: An Overview of 4-Year Single Center Experience. Indian J Surg. 2015, 77, 1219–1221. [Google Scholar] [CrossRef] [PubMed]
- Eckhoff, K.; Wedel, T.; Both, M.; Bas, K.; Maass, N.; Alkatout, I. Spontaneous rectus sheath hematoma in pregnancy and a systematic anatomical workup of rectus sheath hematoma: A case report. J Med Case Reports. 2016, 10, 292. [Google Scholar] [CrossRef]
- Wills, B.A.; Oragui, E.E.; Stephens, A.C.; Daramola, O.A.; Dung, N.M.; Loan, H.T.; et al. Coagulation Abnormalities in Dengue Hemorrhagic Fever: Serial Investigations in 167 Vietnamese Children with Dengue Shock Syndrome. CLIN INFECT DIS. 2002, 35, 277–285. [Google Scholar] [CrossRef]
- Martina, B.E.E.; Koraka, P. , Osterhaus ADME. Dengue Virus Pathogenesis: An Integrated View. Clin Microbiol Rev. 2009, 22, 564–581. [Google Scholar] [PubMed]
- Pahari, S.; Basukala, S.; Kunwar, P.; Thapa, K.; Khand, Y.; Thapa, O. Spontaneous splenic hematoma secondary to dengue infection: A rare case report. Annals of Medicine & Surgery. 2023, 85, 1030–1033. [Google Scholar]
- Kaushik, R.M.; Kumar, R.; Kaushik, M.; Saini, M.; Kaushik, R. Spontaneous spinal intradural hemorrhage in dengue fever: A case report. J Med Case Reports. 2022, 16, 213. [Google Scholar] [CrossRef] [PubMed]
- Corré, J.; Vally, S.; Boiron, P.; Bouillaud, Y.; Travers, J. Spontaneous coronary hematoma concomitant with myocarditis: The first report of double cardiac complication of dengue. ESC Heart Failure. 2023, 10, 1445–1448. [Google Scholar] [CrossRef]
- Siahaan, A.M.P.; Tandean, S.; Saragih, E.B.; Nainggolan, B.W.M. Spontaneous acute subdural hematoma in dengue fever: Case report and review of the literature. International Journal of Surgery Case Reports. 2022, 98, 107512. [Google Scholar] [CrossRef]
- Chang, C.Y. A Fatal Case of Dengue-Associated Hemophagocytic Lymphohistiocytosis and Retroperitoneal Hematoma in a Patient With Autoimmune Hemolytic Anemia. Cureus [Internet]. 2021 May 13. Available online: https://www.cureus.com/articles/58589-a-fatal-case-of-dengue-associated-hemophagocytic-lymphohistiocytosis-and-retroperitoneal-hematoma-in-a-patient-with-autoimmune-hemolytic-anemia (accessed on 9 September 2023).
- Ungthammakhun, C.; Chueansuwan, W.; Changpradub, D. Dengue Hemorrhagic Fever Complicated with Spontaneous Rupture of the Spleen among Patients with Thalassemia and G6PD Deficiency: A Case Report. Arch Clin Med Case Rep [Internet]. 2021, 5. Available online: https://www.fortunejournals.com/articles/dengue-hemorrhagic-fever-complicated-with-spontaneous-rupture-of-the-spleen-among-patients-with-thalassemia-and-g6pd-deficiency-a-.html (accessed on 9 September 2023).
- Mushtaque, R.S.; Ahmad, S.M.; Mushtaque, R.; Baloch, S. A Curious Case of Dengue Fever: A Case Report of Unorthodox Manifestations. Case Reports in Medicine. 2020, 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Matthias, A.T.; Apsara, S.; Epa, A. A case report of dengue haemorrhagic fever complicated with psoas haematoma requiring blood transfusion. BMC Infect Dis. 2019, 19, 385. [Google Scholar] [CrossRef] [PubMed]
- Baruah, S.; Dubey, S.; Ghavghave, U.; Jha, A.N. Dengue Fever Presenting with Cervicodorsal Acute Spinal Spontaneous Subdural Hematoma—Case Report and Review of Literature. World Neurosurgery. 2019, 122, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Singh, R.; Ghosh, S.; Chawla, A. Unusual surgical emergency in a patient of dengue haemorrhagic fever: Spontaneous rectus sheath haematoma leading to abdominal compartment syndrome. BMJ Case Reports 2018, bcr-2018-225936. [Google Scholar] [CrossRef] [PubMed]
- Tamilarasan, V.; Chandra, M.R.K.R.; Mohan, B.V.M.; Kadambi, M. Vocal cord hematoma: An unusual complication of dengue fever. Egypt J Intern Med. 2018, 30, 168–169. [Google Scholar] [CrossRef]
- Anam, A.M.; Rabbani, R.; Shumy, F. Spontaneous calf haematoma in severe dengue. BMJ Case Reports. 2018, bcr-2017-222932. [Google Scholar] [CrossRef] [PubMed]
- Nelwan, E.J.; Angelina, F.; Adiwinata, R.; Matondang, S.; Andriono, P. Spontaneous rectus sheath hematomas in dengue hemorrhagic fever: A case report. IDCases. 2017, 10, 35–37. [Google Scholar] [CrossRef]
- Jayasinghe, N.S.; Thalagala, E.; Wattegama, M.; Thirumavalavan, K. Dengue fever with diffuse cerebral hemorrhages, subdural hematoma and cranial diabetes insipidus. BMC Res Notes. 2016, 9, 265. [Google Scholar] [CrossRef]
- Singh, J. Retroperitoneal Haematoma in a Patient with Dengue Haemorrhagic Fever: A Rare Case Report. JCDR [Internet]. 2016. Available online: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2016&volume=10&issue=11&page=OD01&issn=0973-709x&id=8771 (accessed on 9 September 2023).
- Sharma, A.; Bhatia, S.; Singh, R.; Malik, G. Dengue fever with rectus sheath hematoma: A case report. J Family Med Prim Care. 2014, 3, 159. [Google Scholar] [CrossRef]
- Waseem, T.; Latif, H.; Shabbir, B. An unusual cause of acute abdominal pain in dengue fever. The American Journal of Emergency Medicine. 2014, 32, 819–e3. [Google Scholar] [CrossRef]
- Mehtani, A.; Jha, A.; Kataria, H.; Jangira, V.; Shukla, A. Acute Compressive Ulnar Neuropathy in a Patient of Dengue Fever: An Unusual Presentation. Journal of Orthopaedic Case Reports. 2013, 3, 25–28. [Google Scholar] [CrossRef]
- Sarkar, J.; Mohan, C.; Misra, D.; Goel, A. Lingual hematoma causing upper airway obstruction: An unusual manifestation of dengue fever. Asian Pacific Journal of Tropical Medicine. 2011, 4, 412–413. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Jain, N. Subdural haematoma and axonal polyneuropathy complicating dengue fever. Case Reports. 2011, 2011(jun16 1), bcr1220103672–bcr1220103672. [Google Scholar] [CrossRef]
- Tong, P.; Yeoh, C.; Yong, E. Abdominal mass and a forgotten haemorrhagic fever. The Lancet. 2010, 376, 140. [Google Scholar] [CrossRef] [PubMed]
- Seravali, M.R.M.; Santos, A.H.G.D.; Costa, C.E.F.; Rangel, D.T.A.; Valentim, L.F.; Gonçalves, R.M. Spontaneous splenic rupture due to dengue fever: Report of two cases. Braz J Infect Dis. 2008, 12, 538–540. [Google Scholar] [CrossRef] [PubMed]
- Miranda, L.E.C.; Miranda, S.J.C.; Rolland, M. Case report: Spontaneous rupture of the spleen due to dengue fever. Braz J Infect Dis [Internet]. 2003, 7. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-86702003000600011&lng=en&nrm=iso&tlng=en (accessed on 9 September 2023).
- Liao, E.D.; Puckett, Y. A Proposed Algorithm on the Modern Management of Rectus Sheath Hematoma: A Literature Review. Cureus [Internet]. 2021. Available online: https://www.cureus.com/articles/75702-a-proposed-algorithm-on-the-modern-management-of-rectus-sheath-hematoma-a-literature-review (accessed on 9 September 2023).
- Won, D.Y.; Kim, S.D.; Park, S.C.; Moon, I.S.; Kim, J.I. Abdominal Compartment Syndrome Due to Spontaneous Retroperitoneal Hemorrhage in a Patient Undergoing Anticoagulation. Yonsei Med J. 2011, 52, 358. [Google Scholar] [CrossRef]
| Day of illness | Sample | Hb (gm/dl) | Hct | TLC (/cmm) | Platelet count (/cmm) | SGPT (IU/l) | SGOT (IU/l) |
Phase /clinical events |
|---|---|---|---|---|---|---|---|---|
| Day 4 | Admission | 8.6 | 21.5 | 2,300 | 80,000 | 61 | 158 | Febrile Phase |
| Evening | 8.7 | 22.8 | 2,200 | 70,000 | - | - | ||
| Day 5 | Morning | 9.1 | 26.9 | 1,400 | 60,000 | 98 | 232 | Critical Phase |
| Evening | 9.1 | 25.0 | 1,200 | 69,000 | - | - | ||
| Day 6 | Morning | 9.4 | 28.4 | 1,700 | 30,000 | 176 | 548 | Critical Phase; Severe Nausea and Vomiting; 1 unit of PRBC given |
| Evening | 7.0 | 21.4 | 1,600 | 22,000 | - | - | ||
| Day 7 | Morning | 8.2 | 23.5 | 2,500 | 30,000 | 190 | 534 | Critical Phase; Nausea, vomiting present |
| Evening | 7.8 | 22.4 | 2,700 | 32,000 | - | - | ||
| Day 8 | Morning | 6.8 | 19.2 | 2,800 | 33,000 | 186 | 504 | Critical Phase ended; Nausea, vomiting present; 1 unit of PRBC given; Stool for OBT- strongly positive |
| Evening | 6.7 | 18.7 | 3,300 | 35,000 | - | - | ||
| Day 9 | Morning | 7.8 | 22.7 | 4,300 | 40,000 | 178 | 456 | Nausea, vomiting present; Severe RIF pain; 1 unit of PRBC given |
| Evening | 7.6 | 23.9 | 4,200 | 45,000 | - | - | ||
| Day 10 | Morning | 8.2 | 24.6 | 4,300 | 55,000 | 170 | 345 | Nausea, vomiting subsided, RIF pain continued |
| Evening | 8.0 | 25.8 | 4,700 | 76,000 | - | - | ||
| Day 11 | Morning | 7.6 | 23.7 | 5,800 | 90,000 | 134 | 235 | RIF pain continued, RIF tender mass felt; antibiotics and IV fluids started; 1 unit of PRBC given |
| Evening | 7.2 | 2.6 | 5,700 | 1,12,000 | - | - | ||
| Day 12 | Morning | 8.6 | 26.7 | 6,300 | 1,25,000 | 87 | 176 | RIF tender mass felt; 1 unit of PRBC given |
| Evening | 8.9 | 27.9 | 7,600 | 1,56,000 | - | - | ||
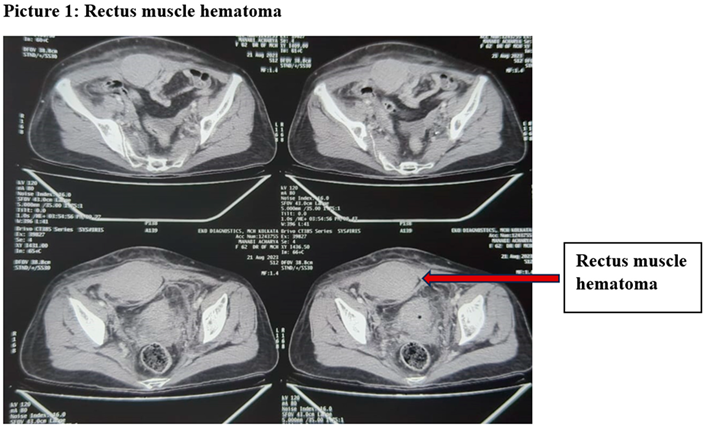
| Day 13 | Morning | 8.5 | 27.0 | 8,900 | 2,12,000 | 67 | 112 | Imaging showed right lower abdominal rectus muscle hematoma, 1 unit of PRBC given; antibiotics discontinued |
| Day 14 | Morning | 9.2 | 28.3 | 8,700 | 2,54,000 | 56 | 78 | Mild RIF tenderness; discharged |
| Location | Sex | Age | Co-morbidities/ drugs | Presentation | Diagnosis | Treatment | Outcome | |
| Our case 2023 |
India | F | 72 | HTN | RIF pain; Recurrent Vomiting (dengue hepatitis) | RSH (CT scan) | Conservative | Survival |
| Pahari et al. 2023(7) | Nepal | M | 54 | Nil | Left upper abdominal pain | Splenic sub-capsular hematoma (CT scan) | Conservative | Death |
| Kaushik et al. 2022(8) | India | F | 48 | Nil | Acute onset paraplegia with bladder and bowel dysfunction and anaesthesia below the umbilicus | Compression of spinal cord due to intradural hematoma at the D7–D8 level (MRI) | Emergency D7–D8 laminectomy with excision of the clot and Dural repair |
Survival with residual neuro-deficit |
| Corré et al. 2022(9) | France | M | 33 | Nil | Chest pain | Coronary hematoma (angiography): Acute myocarditis (CMRI) | Conservative with dual antiplatelets | Survival |
| Siahann et al. 2022(10) | Indonesia | M | 65 | Nil | Altered consciousness and focal neuro- deficits | Subdural hematoma (CT scan) | Craniotomy | Survival |
| Chang et al. 2021(11) | Malaysia | F | 59 | DM | Hypotensive shock | Retroperitoneal hematoma (Ultrasonography) Associated with HLH and AIHA |
Conservative | Death |
| Ungthammakhun et al. 2021(12) | Thailand | M | 22 | Nil | Left upper abdominal pain | Splenomegaly with active contrast extravasation at spleen surrounded with hematoma, and generalized hemoperitoneum (CT scan) |
Splenectomy | Survival |
| Mushtaque et al. 2020(13) | Pakistan | M | 32 | Nil | Decreased power in bilateral lower limbs and pain in right leg |
Bilateral iliopsoas hematoma (CT scan) | Conservative | Survival |
| Matthias etal. 2019(14) | Sri Lanka | M | 28 | Nil | Left groin and inguinal region | Left psoas haematoma (Ultrasonography) |
Conservative | Survival |
| Baruah et al. 2018(15) | India | F | Not Mentioned | HTN, Bronchial Asthma, OSA | Acute quadriparesis with urinary incontinence | Cervicodorsal anterior epidural hematoma (MRI) | Surgical evacuation (durotomy) | Death |
| Ghosh et al. 2018(16) | India | F | 74 | HTN | Recurrent Vomiting | RSH (CT scan) | Surgical evacuation for Abdominal Compartment Syndrome | Survival |
| Tamilasran et al. 2018(17) | India | M | 36 | Nil | Sore throat | Hematoma involving both the vocal cords and immediate sub-glottis (Video Laryngoscopy) |
Conservative | Survival |
| Anam et al. 2017(18) | Bangladesh | M | 45 | Nil | Left calf swelling | Calf muscle hematoma (Ultrasonography) | Surgical evacuation via fasciotomy | Survival |
| Nelwan et al. 2017(19) | Indonesia | F | 58 | Nil | lower abdominal pain | RSH (Cullen’s sign + CT scan) | Conservative | Survival |
| Jayasinghe et al. 2016(20) | Sri Lanka | F | 24 | Nil | Headache, loss of consciousness, seizure | Intracranial haemorrhages and sub arachnoid haemorrhages (CT scan) |
Conservative as platelet count was 40,000/cmm | Death |
| Singh et al. 2016(21) | India | M | 30 | Nil | RIF pain | Intra-parenchymal haematoma in the liver with extension to right peritoneum and right psoas muscle haematoma |
Conservative | Survival |
| Sharma et al. 2014(22) | India | M | 40 | Nil | Severe pain in paraumbilical region, extending to right hypochondrium and lumbar regions |
RSH (CT scan) | Conservative | Survival |
| Waseem et al. 2014(23) | Pakistan | M | 55 | HTN, DM, Aspirin | Pain in right upper quadrant of abdomen | RSH (CT scan) | Surgical Evacuation | Survival |
| Mehtani et al. 2013 (24) | India | M | 36 | Nil | Right forearm pain with tingling and numbness along the distribution of ulnar nerve | Hematoma compressing ulnar neurovascular bundle (MRI) | Surgical evacuation | Survival with residual neuro-deficit |
| Sarkar et al. 2011(25) | India | M | Young | Nil | Inability to protrude his tongue and was unable to speak | Tongue- enlarged and swollen (Clinical) |
Conservative | Survival |
| Mittal et al. 2011(26) | India | F | 27 | Nil | Recurrent seizure | Bilateral subdural haematoma (MRI) | Conservative | Survival with residual neuro-deficit |
| Tong et al. 2010(27) | Republic of Singapore | F | 37 | Adenomyosis, OCP | RIF pain | RSH (CT scan), DVT (US doppler) | Conservative; Anti-coagulation after stabilisation | Survival |
| Seravali et al. 2008(28) | Brazil | M | 27 | Nil | Shock | Spleen congested with rupture of middle third and peri-splenic hematoma (Intra-operative) |
Splenectomy | Survival |
| Seravali et al. 2008(28) | Brazil | M | 20 | Nil | Left upper abdomen pain | Splenic hematoma (Ultrasonography) | Splenectomy | Survival |
| Miranda et al. 2003(29) | Brazil | M | 27 | Nil | Diffuse abdominal pain | Splenic hematoma (CT scan) | Splenectomy | Survival |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





