Figure 1.
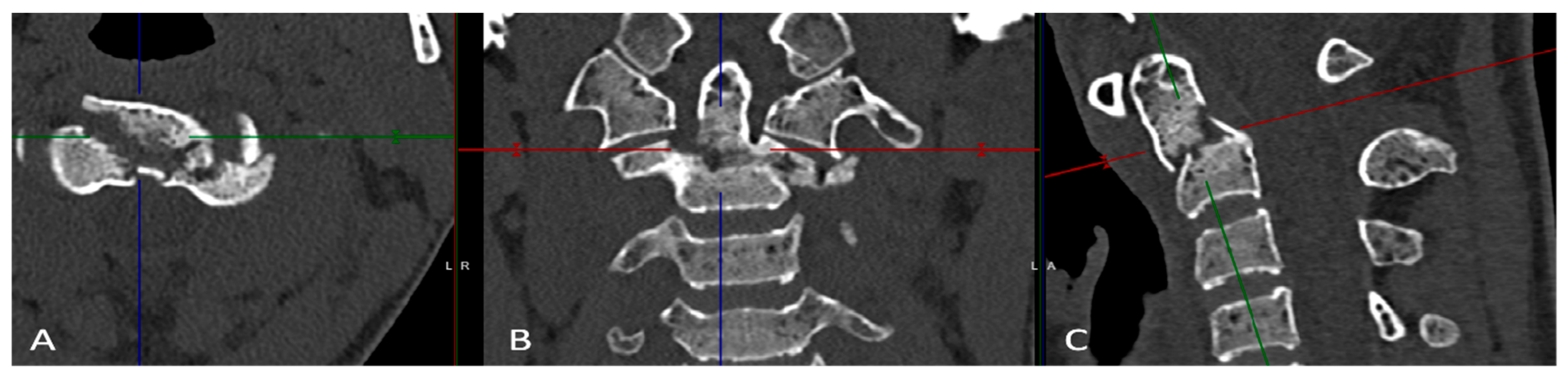
Sagittal neck MRI, revealing the C2 Durel Type II subclass C fracture, Red arrows indi-cate the fracture site. A 19-year-old female athlete endured an unfortunate incident while participating in the European championship for short-track speed skating. During this accident, she sustained a significant facial impact, which led to the onset of distressing symptoms. Upon immediate evaluation at the athletic center medical facility, the patient re-ported severe craniocervical pain, rating it at a distressing 8/10 on the visual analogue scale (VAS). Physical examination revealed that any movement involving neck flexion, extension, or rotation exacerbated her pain significantly, resulting in a VAS score 10/10. In response to the incident, an X-ray examination was promptly conducted, and it revealed no apparent injuries, leading the medical team to grant her clearance to resume the competition. Remarkably, on the day of the accident, the patient showcased remarkable resilience by continuing and successfully completing three additional rounds of rac-ing.Despite her initial resolve, the patient endured ongoing discomfort, rating her pain at 4/10 on the VAS scale. Surprisingly, she actively participated in three more competitions involving at least 20 short-track speed skating rounds during this period. This discomfort persisted for an extended 29-day duration after the incident, leading to an MRI being conducted at a different hospital than ours. The radiologist at the external facility reported an old C2 Durel Type II, Subclass C fracture (
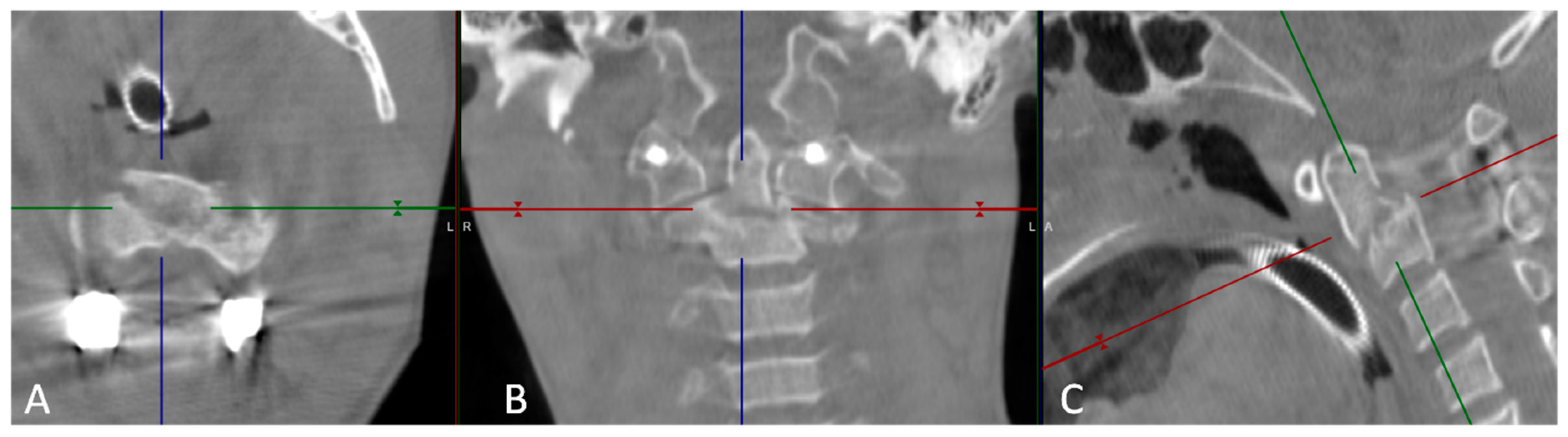
Figure 1). Ongoing pain led the radiologist to refer the case to our department. Upon the patient’s arrival at our institution 41 days after the injury, the clinical presentation, recent accident history, and the extent of the fracture, which involved approximately one-third of the odontoid diameter, raised suspicions of a fresh fracture related to the accident. Subsequently, we performed a CT scan and a functional cervical spine CT, both of which confirmed the instability of the C2 Durel Type II, Subclass C fracture. The functional CT examination revealed a 5 mm movement in the fracture line (
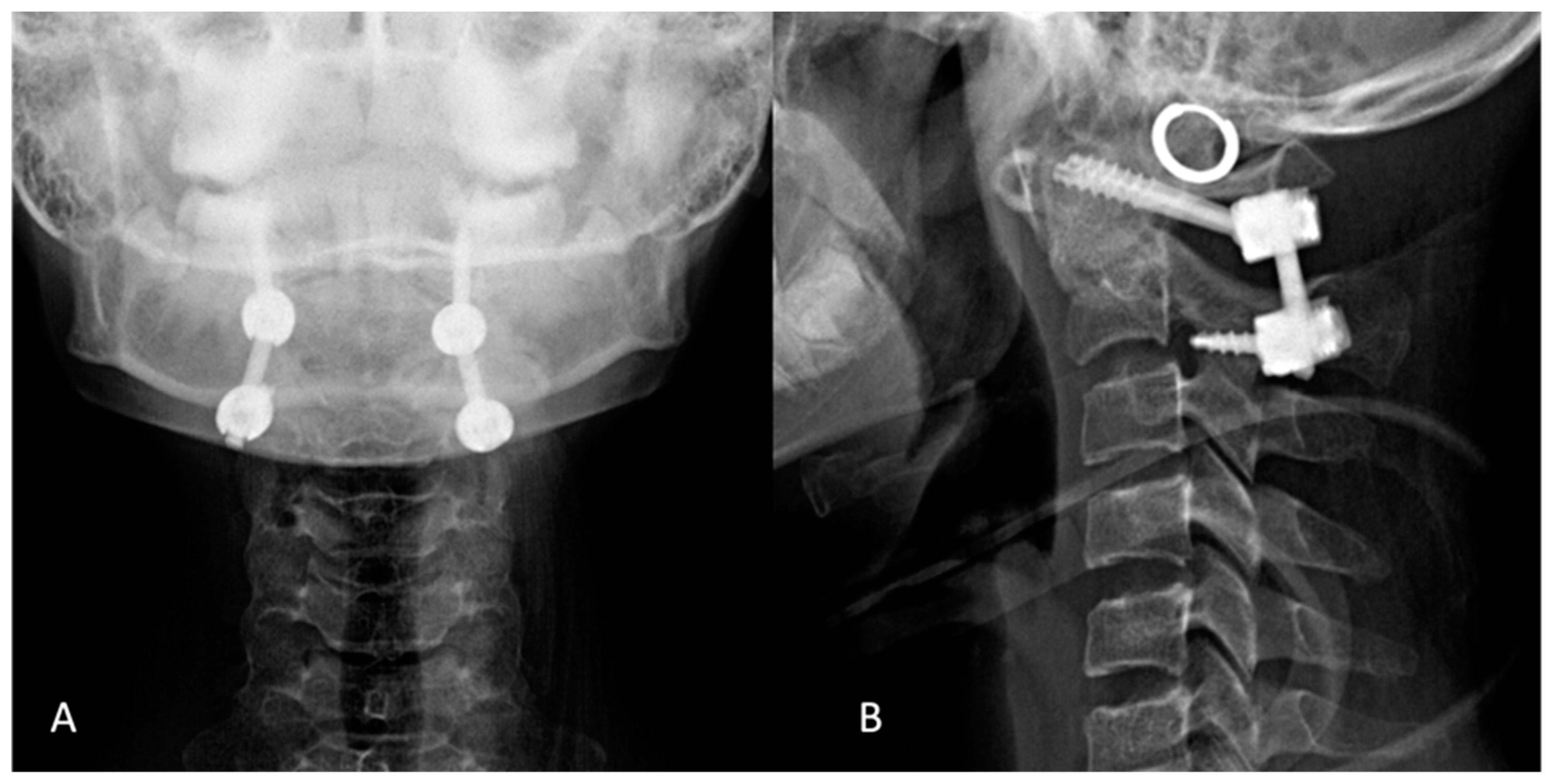
Figure 2). On the 45th day after the initial injury, the patient underwent a successful surgical procedure, utilizing intraoperative O-arm CBCT and Stealth Station Navigation System (SS8) for C1-C2 dorsal fusion, where we placed bi-lateral screws in the lateral masses of both C1 and C2 and connected them with a rod (
Figure 3). This surgical intervention led to the successful repositioning and stabilization of the C1 odontoid (
Figure 4). Following the surgical procedure, the patient embarked on a comprehensive rehabilitation program starting six weeks post-surgery. By the 12-week mark post-surgery, she had made a remarkable recovery, regaining full functionality, and was actively participating in speed skating training without experiencing any complaints. Now, 9 months after the incident, she was granted the medical clearance to be called to represent her home country in the following international ice-skating competition due to her amazing speedy recovery. In a broader context, it is noteworthy that over 14 years, from February 2009 to February 2023. Among 347 cases of C2 odontoid fractures, only 5 fractures (1.14%) in our institute were attributed to professional sports activities. These sports-related fractures encompassed cases linked to skiing, short-track speed skating, cross-motorcycling, and go-karting. Notably, 3 of these fractures occurred during winter sports. Different treatment modalities were employed for these cases, with ventral odontoid screw fixation used in two instances, dorsal C1-C2 screw fixation in 1 case, and the HALO fixation device employed in the remaining 2 cases. In general, evaluating an acute cervical spine injury is challenging. Clinicians recommend obtaining three distinct views of the cervical spine. These views encompass the anteroposterior, cross-table lateral, and open-mouth odontoid cervical radiographs [
1,
2]. However, due to the inherent limitations of conventional plain radiography, the standard approach has evolved to encompass the more widespread utilization of flexion/extension radiographs, CT scans, and MRI examinations, particularly for detecting subtle cervical spine injuries [
3]. CT scans have emerged as the modality for effectively visualizing the cervical spine. Consequently, when CT imaging is deemed necessary, there is often no prerequisite for additional plain radiographic imaging [
4]. Recent empirical data has suggested that CT imaging should be prioritized to assess the cervical spine rapidly and efficiently, potentially rendering conventional plain radiographic imaging unnecessary [
5]. Moreover, in specific clinical scenarios such as neurologic deficits, the need to assess ligamentous injuries, or the imperative to rule out underlying pathologies, MRI may also be considered an invaluable diagnostic tool [
6,
7]. In light of the absence of clear-cut guidelines regarding the optimal imaging modality for cervical fracture diagnosis, healthcare professionals must thoroughly understand the strengths and limitations of each option. In athletic events, continuous video recording can offer invaluable insights into the injury’s nature, assisting clinicians in making an informed choice regarding the most suitable imaging technique. The selection of an imaging method plays a pivotal role in determining the accuracy and speed of diagnosis, ultimately affecting patient outcomes. While CT and MRI remain the foundations of cervical fracture diagnosis, clinicians must adopt a holistic approach. This involves relying on imaging results and considering the clinical presentation, mechanism of injury, and any associated symptoms [
8,
9]. The synergy between the patient’s anamnesis, clinical picture, and imaging modalities ensures a comprehensive evaluation, minimizing the risk of misdiagnosis. As the field advances, ongoing research and collaboration between radiologists, neurosurgeons, and orthopedic specialists will be crucial in refining diagnostic protocols ensuring that patients receive timely and appropriate care.