1. Introduction
Bilateral diffuse uveal melanocytic proliferation (BDUMP) is a relatively uncommon paraneoplastic syndrome that affects the eye. It was initially described by Machemer in 1966 [
1] and further characterized by Gass and colleagues in 1990 [
2]. BDUMP presents with five distinct features: First, in the posterior fundus, there are numerous inconspicuous round or oval patches located at the level of the retinal pigmented epithelium (RPE). Second, these patches correspond to multifocal regions of early hyper-fluorescence. Third, there is evidence of multiple uveal melanocytic tumours, which can be pigmented or non-pigmented, and they are slightly elevated. Additionally, there is a noticeable thickening of the uveal tract. Fourth, an exudative retinal detachment can be observed. Lastly, individuals affected by BDUMP experience a rapid progression of cataracts. The characteristic ocular fundus pattern described by Gass is informally referred to as "leopard spots" due to its reticulated colour configuration, also known as the "gyrate pattern. The reticulated depigmentation pattern, while a characteristic of BDUMP, is not a specific ocular diagnostic feature, as it has also been observed in other conditions like metastatic cancer, leukemic infiltration of the choroid, and lymphoma, all of which can occur bilaterally [
3]. It is only in rare cases of BDUMP that multiple pigmented nodules are observed without the classic "leopard spots." BDUMP was first used to characterise a set of pathologies by Barr and colleagues [
4]. They outlined four ocular clinical features associated with this syndrome, which include bilateral involvement of the uveal tracts diffusely, a predominantly benign cytological composition of the melanocytic lesion, the absence of evidence suggesting metastasis from the melanocytic tumours, and confirmation of a linked systemic malignancy attained through biopsy. The pathogenesis of the melanocytic infiltration in BDUMP remains unclear. However, it is presumed either a tumour-secreted substance or a tumour-stimulated antibody causes the benign proliferation of choroidal melanocytes [
5]. So far, close to 100 cases have been published discussing the pathologic correlates of BDUMP [
3]. BDUMP is typically diagnosed in patients during their sixth to seventh decade of life, most of whom have been previously diagnosed with various non-ocular cancers. Notably, female urogenital cancers (69%) and male lung carcinomas (52%) are more frequently reported, while sporadic cases include cancers of the pancreas, oesophagus, breast, liver, Bartholin gland, renal cells, and central nervous system lymphoma [
3]. After the diagnosis of BDUMP, the average survival period is slightly over 15 months, ranging from 10 months to 5 years [
6]. Unfortunately, the visual prognosis for BDUMP is dim, as most patients experience progressive visual deterioration primarily caused by the combined effects of dense bilateral cataract formation and chronic subretinal fluid accumulation with secondary degeneration of the RPE cells and photoreceptors. The prognosis is notably worse in cases of macular detachment [
1,
2].
Duong et al. reported the longest survival of a patient with BDUMP, with their patient living for an additional 10.5 years after undergoing bilateral enucleation [
7].
We report a case of a 62-year-old female patient who developed BDUMP syndrome one month after being diagnosed with clear cell adenocarcinoma of the right ovary.
2. Materials and Methods
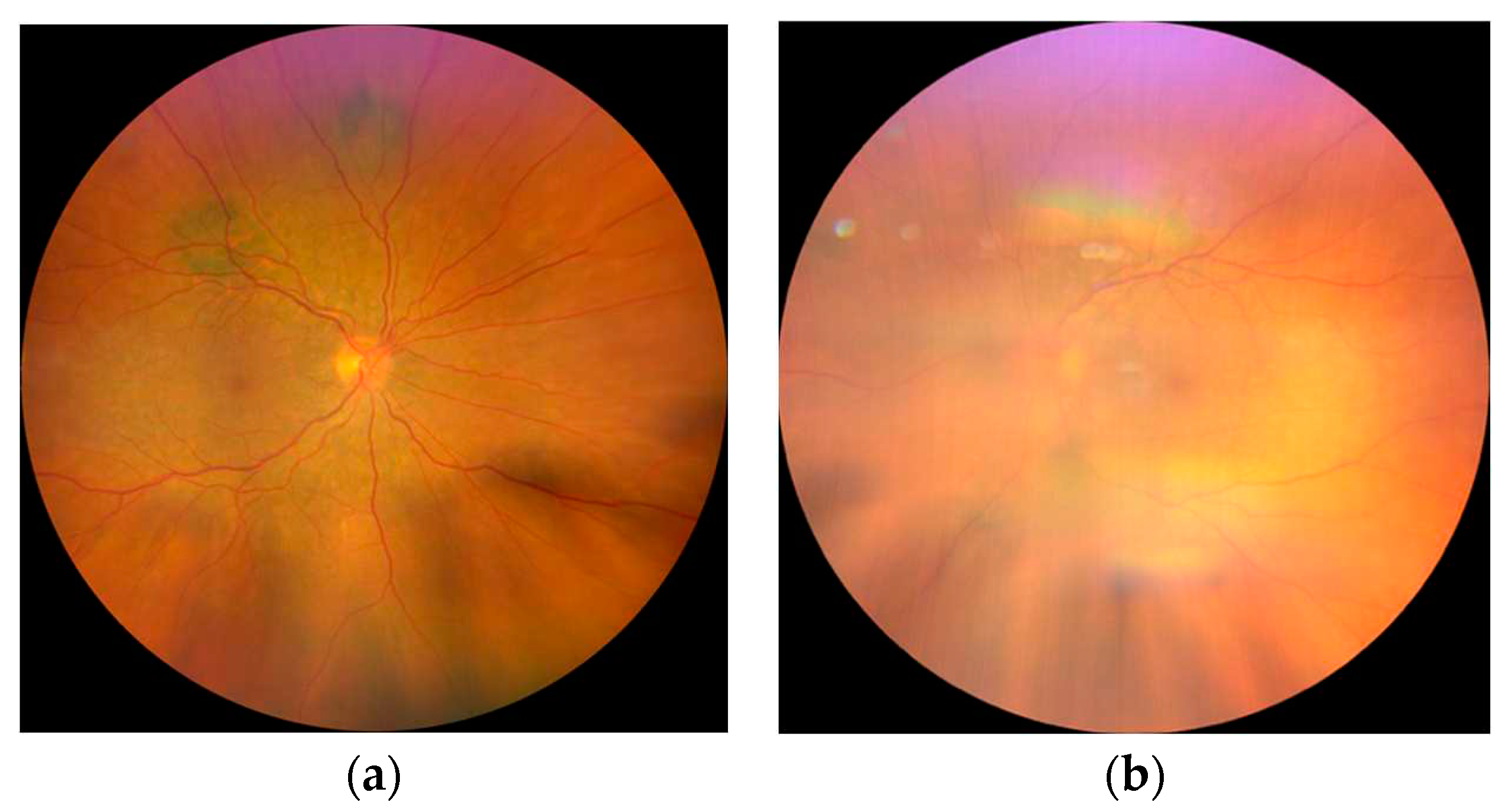
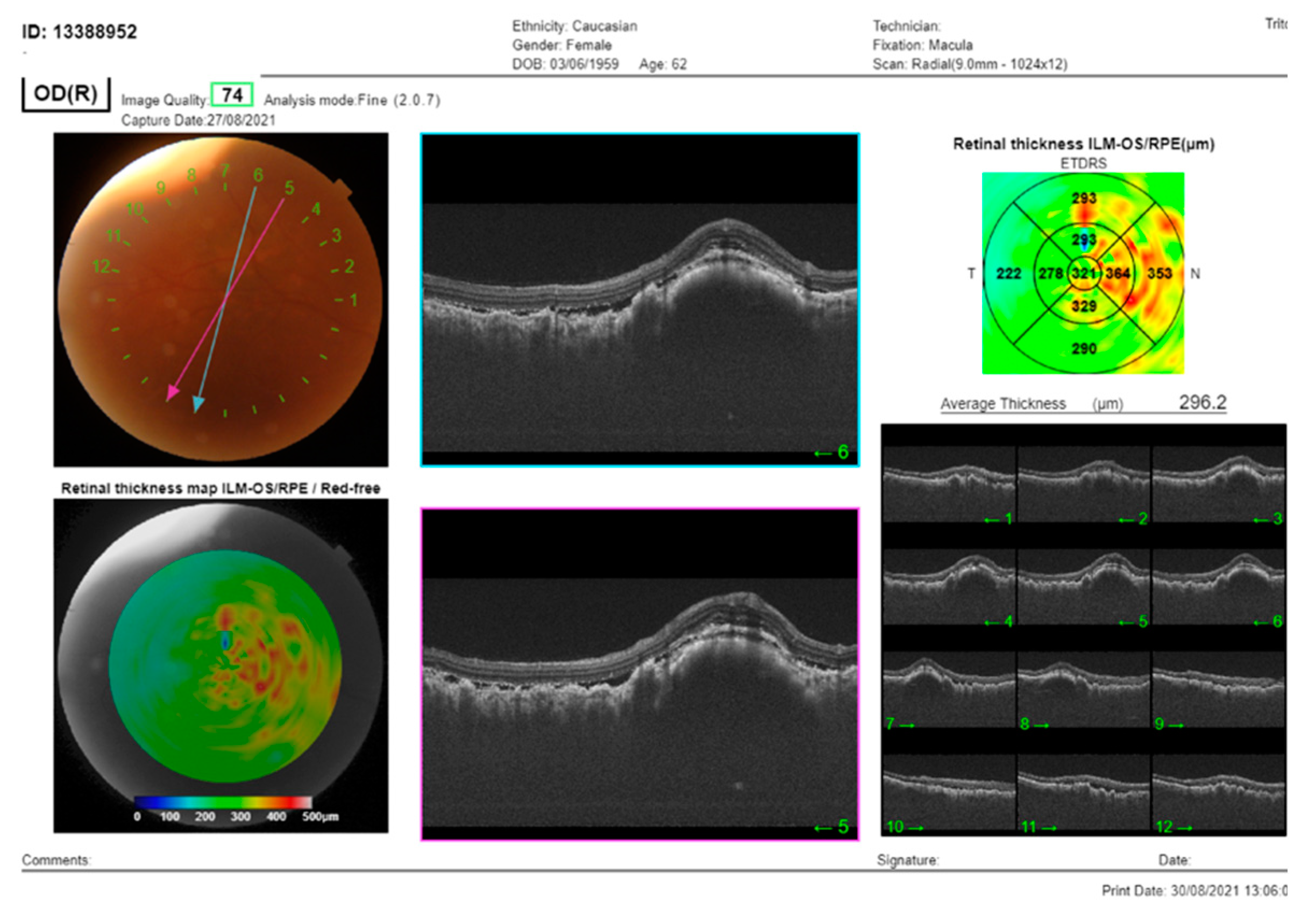
The patient was initially referred to our clinic for cataract surgery because of rapidly progressive bilateral cataracts in the last three months. An initial best corrected visual acuity (BCVA) of the right (RE) and left eye (LE) of 20/20 dropped to 20/200 and counting fingers (CF) respectively. Anterior segment examination revealed Tyndall + cells in the anterior chamber, extremely dense cataracts bilaterally, more prominent on the LE. On fundus examination, diffuse multifocal lesions, with mild prominence at the locations of the orange pigment were observed bilaterally, but barely visible on the LE due to the cataract (
Figure 1).
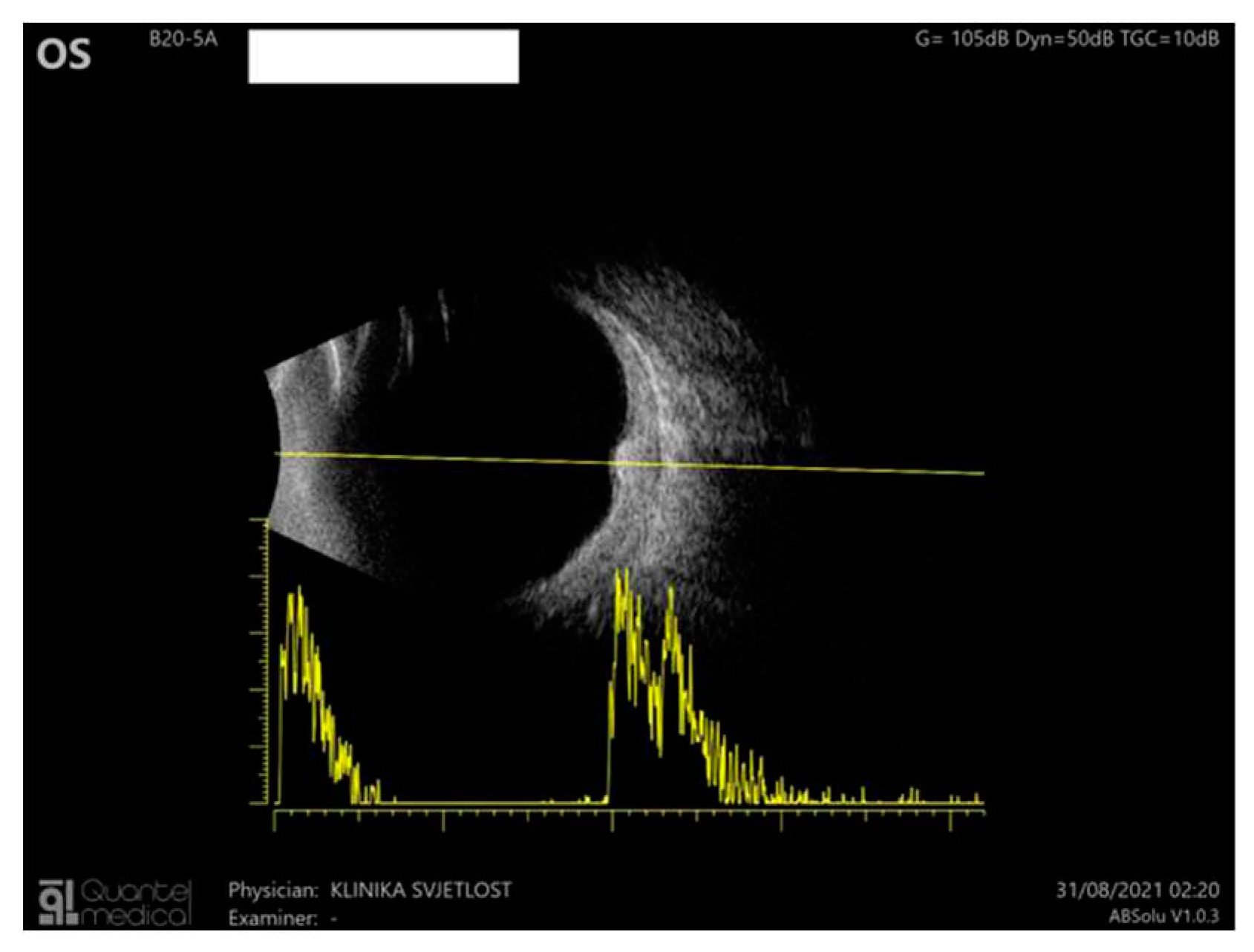
B-scan ultrasound through the choroidal lesions showed moderate homogenous internal reflectivity (
Figure 3).
Since the patient has been diagnosed with ovarian cancer and has undergone a hysterectomy with bilateral adnexectomy due to adenocarcinoma of the right ovary, BDUMP was presumed to be the diagnosis.
After the surgery, the chemotherapy was initiated by the oncologists but was stopped after three cycles due to the development of severe toxic sensorimotor polyneuropathy. Adjacent diseases included chronic renal insufficiency stage IV, secondary anaemia, hypoalbuminemia, and hypocalcaemia.
Cataract surgery was performed on both eyes. However, the vision deteriorated due to chronic serous retinal detachment (RE: CF, LE:30/200).
Plasmapheresis was performed but without significant change in visual acuity or lesions of the posterior pole. Aflibercept (Eylea) was applied to both eyes but exerted minimal effects on subretinal fluid minimization. The immunomodulatory therapy was suggested but due to renal insufficiency (high creatinine) and high level of liver enzymes, this treatment option was dismissed.
The patient developed sub-retinal fibrosis with a progressive elevation of the nasal retina on the right eye and is currently being observed for possible vitrectomy.
3. Results
The patient started treatment in 2021 and is currently undergoing therapy. She is alive and in remission after surgical treatment (ovariectomy and hysterectomy) and curative chemotherapy, which was stopped due to neurological complications. Unfortunately, the vision deteriorated to CF on the RE and 2/200 on the LE despite cataract surgery on both eyes, plasmapheresis, intravitreal anti-VEGF (aflibercept), as well as systemically and locally administered corticosteroid therapy. Suggested immunomodulatory therapy could not be applied due to renal and liver complications. The inflammation in the anterior segment had resolved but subretinal fluid along with lesions did not regress and subsequently subretinal fibrosis with possible tractional retinal detachment is now being observed for vitrectomy on the RE.
4. Discussion
Treatment of BDUMP must consist of treating primary malignancy first by either surgical removal, radiation, or systemic chemotherapy [
4]. In some cases, visual symptoms have improved, suggesting that systemic factors triggered by primary malignancies may contribute to the development of BDUMP. Miles and colleagues conducted a study revealing the presence of a factor in the serum and plasma of BDUMP patients that could stimulate the growth of cultured melanocytes [
8]. This substance was identified as an IgG antibody in serum and plasma samples and was given the name "CMEP factor" due to its role in promoting elongation and proliferation of cultured melanocytes. In theory, plasmapheresis could be used to eliminate plasma CMEP, although its effectiveness to do so appears to vary. In our case, plasmapheresis had no significant effect on improved patient clinical outcomes. Intravitreal anti-VEGF agents were proven effective in some cases, minimizing intra-retinal fluid accumulation [
4]. Following intravitreal aflibercept application, discrete minimization in the subretinal fluid was observed, but the visual acuity deteriorated further. Previous interventions such as ocular radiation, sub-retinal fluid drainage, and corticosteroids were generally ineffective [
9,
10]. We also treated our patient with systemic corticosteroids in a tapered dose fashion, as well as locally with non-steroid and steroid anti-inflammatory drops. It has been reported that BDUMP can be a possible complication of immune-modulating therapy. However, a case highlighted a patient who had also renal carcinoma and it is not clear whether immunomodulatory therapy caused BDUMP or underlying malignancy [
11]. Immunomodulatory therapy was suggested, but not applied in our patient due to renal and liver complications.
5. Conclusions
Upon review, it is recommended that additional investigation be conducted to identify any primary malignancies related to BDUMP. Although rare, with an incidence of 4.4 cases per year around 2017 [
3], it requires specific management. Furthermore, the symptoms including the rapid onset of cataracts along with advanced vision loss must be considered warning signs in identifying this syndrome, especially with anamnestic proof of underlying primary malignancy. It is important to conduct detailed systemic examinations in patients suspected of having BDUMP to identify potential primary malignancies and establish a connection between the malignancy and ocular changes. This will enable early treatment and improve prognoses, especially since the prognosis of BDUMP is extremely poor. The primary malignancy's slow spread can increase survival time from the mean of 15.6 months to 4-9 years in exceptional cases [
11].
Statement of ethics: This case report was approved by the Medical Ethics Review Committee of the Academic Medical Center, and it is not subject to the Medical Research Involving Human Subjects Act (WMO).
Informed Consent Statement
All participants in the study provided their informed consent.
Acknowledgments
None.
Conflicts of interest: None.
References
- Machemer, R. [On the pathogenesis of the flat malignant melanoma]. Klin Monbl Augenheilkd. 1966, 148, 641–52. [Google Scholar] [PubMed]
- Gass, J.D.M. Bilateral Diffuse Uveal Melanocytic Proliferation in Patients With Occult Carcinoma. Arch. Ophthalmol. 1990, 108, 527. [Google Scholar] [CrossRef]
- Weppelmann, T.A.; Khalil, S.; Zafrullah, N.; Amir, S.; Margo, C.E. Ocular Paraneoplastic Syndromes: A Critical Review of Diffuse Uveal Melanocytic Proliferation and Autoimmune Retinopathy. Cancer Control. 2022, 29, 107327482211444. [Google Scholar] [CrossRef] [PubMed]
- Barr, C.C.; Zimmerman, L.E.; Curtin, V.T.; Font, R.L. Bilateral Diffuse Melanocytic Uveal Tumors Associated With Systemic Malignant Neoplasms. Arch. Ophthalmol. 1982, 100, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Chen, Z.; Luo, Y.; Zhao, L.; Dai, R.; Zhong, Y. Diagnosis of bilateral diffuse uveal melanocytic proliferation unveils primary gastric adenocarcinoma: a case report. BMC Ophthalmol. 2020, 20, 1–3. [Google Scholar] [CrossRef]
- Rahimy, E.; Coffee, R.E.; McCannel, T.A. Bilateral Diffuse Uveal Melanocytic Proliferation as a Precursor to Multiple Systemic Malignancies. Semin. Ophthalmol. 2013, 30, 206–209. [Google Scholar] [CrossRef]
- Duong, H.-V.Q.; McLean, I.W.; Beahm, D.E. Bilateral Diffuse Melanocytic Proliferation Associated With Ovarian Carcinoma and Metastatic Malignant Amelanotic Melanoma. Arch. Ophthalmol. 2006, 142, 693–695. [Google Scholar] [CrossRef] [PubMed]
- Miles, S.L.; Niles, R.M.; Pittock, S.M.; Vile, R.; Davies, J.; Winters, J.L.; Abu-Yaghi, N.E.M.; Grothey, A.; Siddiqui, M.M.; Kaur, J.; et al. A factor found in the igg fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina 2012, 32, 1959–1966. [Google Scholar] [CrossRef]
- Jaben, E.A.; Pulido, J.S.; Pittock, S.; Markovic, S.; Winters, J.L. The potential role of plasma exchange as a treatment for bilateral diffuse uveal melanocytic proliferation: A report of two cases. J. Clin. Apher. 2011, 26, 356–361. [Google Scholar] [CrossRef] [PubMed]
- van Noort, B.C.; Keunen, J.E.; Schlingemann, R.O.; Marinkovic, M. Long Survival and Preservation of Good Visual Acuity in a Patient with Bilateral Diffuse Uveal Melanocytic Proliferation. Ocul. Oncol. Pathol. 2019, 5, 75–78. [Google Scholar] [CrossRef]
- Klemp, K.; Kiilgaard, J.F.; Heegaard, S.; Nørgaard, T.; Andersen, M.K.; Prause, J.U. Bilateral diffuse uveal melanocytic proliferation: Case report and literature review. Acta Ophthalmol. 2017, 95, 439–445. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).