1. Introduction
Respiratory viral infections have plagued humanity for centuries, causing widespread illness, death, and economic disruption. From the common cold to more severe diseases like influenza [
1] and COVID-19 [
2], these infections pose a significant threat to global health security. It is high time we acknowledge the pressing need for a new strategy to combat respiratory viral infections effectively [
3]. By investing in research, public health infrastructure, and international collaboration, we can mitigate the devastating impact of these infections and safeguard our future [
4].
While significant progress has been made in understanding respiratory viral infections, our current strategies are falling short in several key areas [
5]. First and foremost, our reliance on reactive measures rather than proactive ones leaves us vulnerable to outbreaks. We often find ourselves scrambling to develop vaccines or treatments after an infection has already spread widely [
6].
Additionally, the lack of robust surveillance systems hampers our ability to detect emerging respiratory viruses promptly. By the time we identify a new threat, it may have already gained a foothold in communities worldwide [
7]. Furthermore, inadequate public health infrastructure exacerbates the challenges of containment and control efforts [
8].
To combat respiratory viral infections effectively, we must prioritize research and development efforts [
9]. Antibodies have been established as a crucial form of therapeutics due to their valuable benefits, including exceptional specificity and affinity [
10]. They are extensively utilized for treating lung diseases like lung cancer and severe asthma [11, 12]. The landscape of antibody therapeutics has rapidly transformed in response to the COVID-19 pandemic, aided by advancements in antibody engineering. However, the current administration of antibody therapeutics is restricted to the invasive parenteral route, which presents limitations such as increased risks of systemic toxicity like cytokine release syndrome [13, 14].
Therefore, nanobodies offer a promising alternative approach to treating respiratory viral infections [
15]. They can be engineered to specifically target viral proteins and prevent them from infecting cells. Moreover, nanobodies can be produced in large quantities using recombinant DNA technology, making them more cost-effective than traditional antibodies [
16].
Nanobodies are small antibody fragments that have gained a scientific dedication in recent years due to their potential therapeutic applications [
17]. These tiny proteins, derived from the immune system of camelids such as llamas and camels [
18], have unique properties that make them attractive candidates for treating a variety of diseases, including respiratory tract viral infections [
19].
One potential application of nanobodies is as a spray or aerosol particle (Eresol particles are dry powder formulations that can be easily dispersed in an aerosol form using inhalers or nebulizers [
20]. This delivery method allows for targeted deposition of nanobodies in the respiratory tract, ensuring maximum therapeutic effect.) for delivering them directly to the respiratory tract. This approach has several advantages over traditional injection-based therapies. First, it allows for targeted delivery of the nanobodies to the site of infection, increasing their efficacy while minimizing side effects. Second, it is non-invasive and can be easily administered by patients themselves or healthcare professionals [
21].
In this mini-review article, we will discuss the potential of nanobodies as spray and aerosol particles for the treatment of respiratory tract viral infections. We will also highlight recent advances in this field and discuss the challenges that need to be addressed for the successful translation of nanobody-based therapies into clinical practice.
2. Current treatment options
Respiratory tract viral infections are a common cause of illness in humans, ranging from mild colds to severe respiratory illnesses such as pneumonia. These infections are caused by a variety of viruses, including influenza, rhinovirus, RSV, and coronavirus [
22]. While there are several treatment options available for respiratory tract viral infections, they have their limitations [
23].
Antiviral Medications: Antiviral medications are the most commonly used treatment option for respiratory tract viral infections. These medications work by inhibiting the replication of the virus in the body. The most commonly used antiviral medications for respiratory tract viral infections include oseltamivir (Tamiflu) and zanamivir (Relenza) for influenza, ribavirin for RSV, and remdesivir for COVID-19 [
24].
However, these medications have several limitations. Firstly, they are only effective if taken within a certain timeframe after the onset of symptoms. For example, oseltamivir is only effective if taken within 48 hours of symptom onset. Secondly, these medications can have side effects such as nausea and vomiting. Lastly, there is a risk of developing resistance to these medications over time [
25].
Supportive Care: Supportive care is another treatment option for respiratory tract viral infections. This includes measures such as rest, hydration, and pain relief medication to manage symptoms such as fever and coughing. While supportive care can help alleviate symptoms and improve overall comfort during an infection, it does not directly target the virus causing the infection. As a result, it may not be sufficient in cases where the infection is severe or complications arise [
26].
Vaccines: Vaccines are a preventative measure against respiratory tract viral infections rather than a treatment option. Vaccines work by stimulating the immune system to produce antibodies against specific viruses [
27]. While vaccines have been successful in preventing many cases of influenza and other respiratory tract viral infections, they have their limitations. Firstly, vaccines are not 100% effective and may not provide complete protection against all strains of a virus. Secondly, the effectiveness of vaccines can decrease over time, requiring booster shots to maintain immunity. Lastly, the development and distribution of vaccines can take time, leaving populations vulnerable to outbreaks in the meantime [5, 28].
In brief, Antiviral medications can be effective but have a limited window of effectiveness and can cause side effects or lead to resistance over time. Supportive care can help alleviate symptoms but does not directly target the virus causing the infection. Vaccines are a preventative measure but may not provide complete protection against all strains of a virus and require booster shots to maintain immunity. As such, it is important to continue research into new treatment options for respiratory tract viral infections to improve outcomes for patients.
3. Nanobodies
3.1. Definition and Characteristics
Nanobodies are a type of antibody that is derived from the immune system of camelids, such as llamas and camels [
29]. These antibodies are much smaller than traditional antibodies, with a molecular weight of only 12-15 kDa. They are also known as single-domain antibodies or VHHs (variable domains of heavy chain-only antibodies) .
Nanobodies have several unique characteristics that make them attractive for use in research and therapeutic applications. Firstly, they have a high affinity and specificity for their target antigens, similar to traditional antibodies. However, because they are smaller in size, they can access epitopes that may be inaccessible to larger antibodies [
30].
Secondly, nanobodies have excellent stability and solubility, which makes them easier to produce and store than traditional antibodies. They can also withstand harsh conditions such as high temperatures and low pH levels [
31].
Thirdly, nanobodies can be easily engineered to improve their properties or modify their function. For example, they can be conjugated to fluorescent dyes or other molecules for imaging or drug delivery purposes [
32].
Finally, nanobodies have a low immunogenicity in humans due to their non-human origin. This means that they are less likely to cause an immune response when used therapeutically [
33].
4. Nanobodies as spray and eresol particles:
Spray and aerosol delivery methods have been used for decades to deliver drugs to the lungs and other parts of the body [
34]. These methods involve creating a fine mist or spray that can be inhaled or applied topically to the skin. In recent years, researchers have begun exploring the use of these methods for delivering nanobodies [
35].
There are several different types of sprays and aerosols that can be used to deliver Nbs (
Table 1) [
36]. One common method is to use a nebulizer, which converts liquid medication into a fine mist that can be inhaled through a mouthpiece or mask [
37]. Another method is to use an inhaler, which delivers medication in a pressurized form through an inhalation device [
38].
In addition to delivering nanobodies directly to the site of action, sprays and aerosols also offer other advantages over traditional drug delivery methods [
39]. For example, they can be used to deliver drugs that are not easily absorbed by the body, such as proteins and peptides [
40]. They can also be used to deliver drugs that would otherwise be destroyed by the digestive system if taken orally [
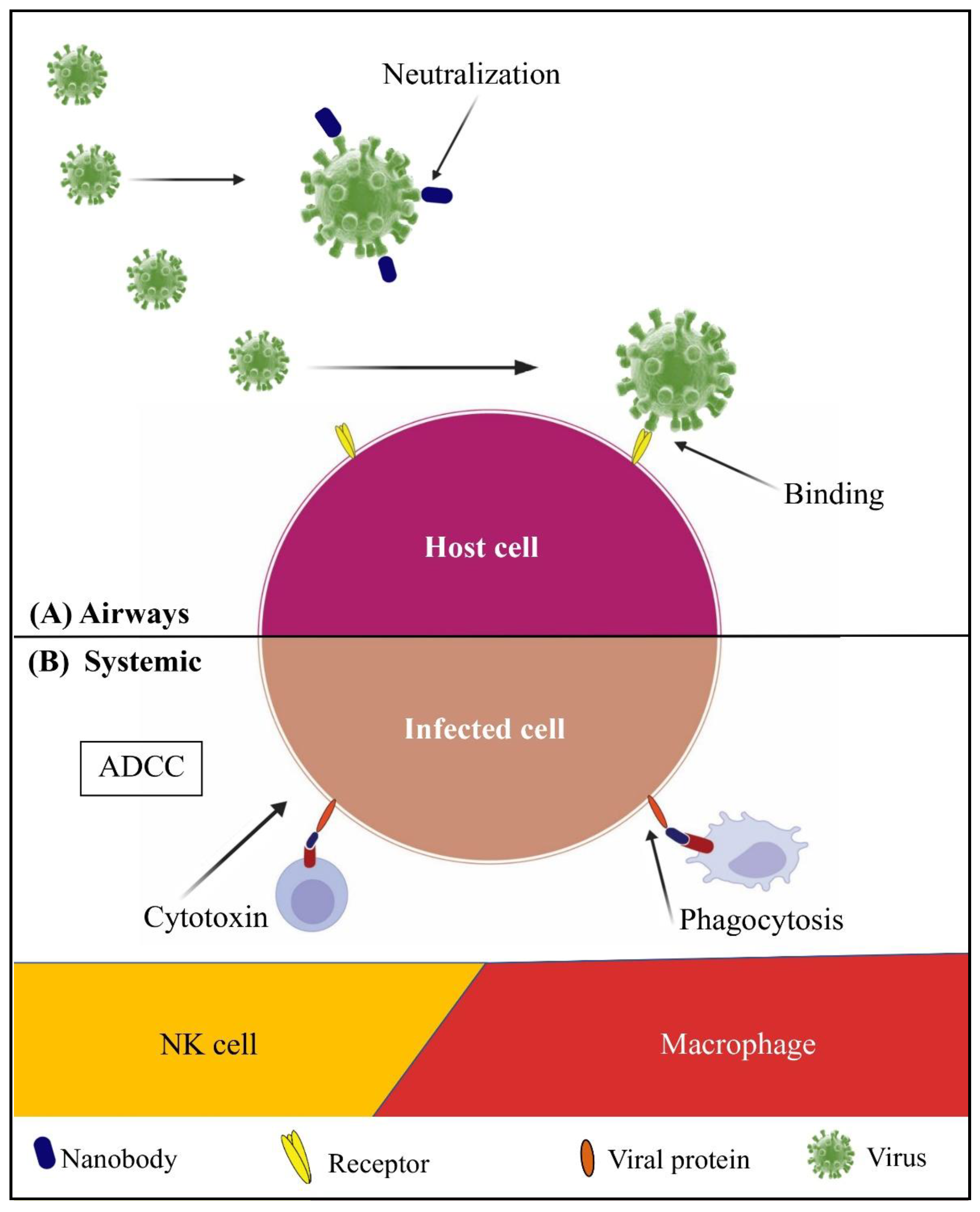
41]. One area where nanobodies have shown promise is in the treatment of respiratory tract viral infections (
Figure 1) [
39].
Recent studies have shown that nanobodies delivered as spray or aerosol particles can effectively treat respiratory viral infections in animal models [12, 36]. In one study, researchers used nanobodies targeting RSV to treat mice infected with the virus. The nanobodies were delivered as an aerosol spray directly into the lungs, and were found to significantly reduce viral load and improve lung function compared to untreated mice [
43].
Another study looked at the use of nanobodies targeting influenza virus in ferrets. The nanobodies were delivered as an aerosol spray into the nose, mimicking how humans would receive treatment for influenza. The researchers found that the nanobodies were able to prevent infection with both seasonal and pandemic strains of influenza virus [
44].
These studies provide strong evidence for the potential efficacy of nanobodies as spray and aerosol particles for treating respiratory viral infections. However, there are still challenges that need to be addressed before these therapies can be used in humans. One challenge is the development of scalable production methods for nanobodies, as current methods are often time-consuming and expensive. Another challenge is ensuring the safety and efficacy of these therapies in humans, as there is still limited data on their use in clinical settings [
45].
Despite these challenges, the potential benefits of nanobodies as spray and aerosol particles for treating respiratory viral infections are clear. These therapies offer a promising new approach to treating these infections, and could help reduce the burden of respiratory viruses on global health.
5. Advantages of nanobodies as spray and eresol particles over traditional antibodies:
In recent years, nanobodies have emerged as a promising alternative to traditional antibodies in various fields of research and medicine (
Table 2). These small antibody fragments, possess unique properties that make them highly advantageous when used as spray and aerosol particles [
46].
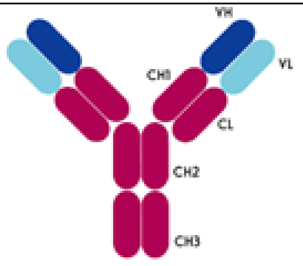
Firstly, one of the major advantages of nanobodies is their small size. Traditional antibodies are large molecules composed of two heavy chains and two light chains, making them difficult to deliver efficiently through sprays or aerosols. In contrast, nanobodies consist of a single variable domain that retains the antigen-binding capacity [
19]. Their compact structure allows for better penetration into tissues and mucosal surfaces, enabling effective delivery to target sites within the respiratory system. One advantage of using sprays and aerosols to deliver nanobodies is that they can be targeted directly to the site of action [
19].
Another advantage of using sprays and aerosols is that they can be easily administered by patients themselves [
49]. This is particularly important for chronic conditions such as asthma or COPD, where patients may need to use medication on a regular basis [
50]. By using a spray or aerosol, patients can self-administer their medication without needing assistance from a healthcare professional.
Furthermore, nanobodies offer enhanced tissue penetration due to their ability to bind epitopes inaccessible to conventional antibodies. Their small size allows them to reach deep into tissues or mucosal surfaces where larger antibodies may struggle to access [
51]. This property is particularly advantageous in the context of respiratory diseases, where effective targeting of pathogens or antigens within the lungs is crucial for therapeutic success [
52].
Moreover, nanobodies exhibit exceptional stability compared to traditional antibodies. They can withstand harsh environmental conditions such as extreme temperatures and pH variations without losing their functionality [
3]. This stability is crucial for maintaining the integrity of the nanobody during storage and transportation as spray or aerosol particles. It also ensures that the therapeutic effect remains intact upon administration [
53].
Additionally, nanobodies have a lower immunogenic potential compared to traditional antibodies. The smaller size and unique structure of nanobodies make them less likely to elicit an immune response when administered as sprays or aerosols [
54]. This reduced immunogenicity minimizes the risk of adverse reactions and increases patient tolerance, making nanobody-based therapies a safer option for respiratory conditions [
54].
Lastly, nanobodies can be easily engineered and modified to enhance their properties. Through techniques such as protein engineering or fusion with other functional molecules [
55], researchers can optimize nanobodies for specific applications. For instance, they can be engineered to have prolonged half-lives in the body or improved binding affinity towards target antigens. Such modifications enable customization of nanobodies as spray or aerosol particles, tailoring them to meet specific therapeutic needs [
19].
6. Strategies for optimizing nanobody formulations
To optimize spray and aerosol formulations, particle engineering techniques such as spray drying or nebulization are employed. Spray drying involves converting liquid formulations into dry powders by atomizing them into a hot drying gas stream. This process can produce highly dispersible powders that can be easily reconstituted into aerosols upon rehydration [
56].
Nebulization is another commonly used technique where liquid formulations are converted into fine droplets suitable for inhalation. Nebulizers generate aerosols by using compressed air or ultrasonic vibrations to break down liquid formulations into droplets of desired size range. This method is particularly useful for delivering nanobodies directly to the respiratory tract [
57].
Optimizing nanobody formulations as spray and aerosol particles also involves considering factors such as particle size, stability, and compatibility with the delivery device [
40]. The particle size should be within the respirable range (1-5 μm) to ensure efficient deposition in the lungs. Stability studies are conducted to assess the physical and chemical stability of nanobodies during storage and aerosolization processes. Compatibility studies evaluate the interaction between nanobodies and the delivery device to ensure proper functionality and prevent aggregation or denaturation [
58].
6.1. Encapsulation technique
Encapsulation is a technique used to protect and deliver drugs or therapeutic agents, in a controlled manner [
59]. In the context of nanobody formulations for spray and aerosol particles, encapsulation plays a crucial role in optimizing their effectiveness [
21].
Nanobodies have gained significant attention in recent years for their potential applications in various fields, including drug delivery [
53]. However, the successful delivery of nanobodies via spray or aerosol particles requires careful consideration of several factors [
36].
One of the main challenges in formulating nanobodies for spray and aerosol delivery is their susceptibility to degradation or denaturation. Encapsulation techniques can help protect nanobodies from environmental factors such as temperature, humidity, and pH changes that may occur during storage or administration. By encapsulating nanobodies within protective carriers, their stability can be significantly improved [
21].
Encapsulation also enables the controlled release of nanobodies upon administration [
60]. This is particularly important for targeted delivery to specific sites within the body. By encapsulating nanobodies within particles that can be easily delivered via sprays or aerosols, their release can be precisely regulated to achieve optimal therapeutic effects [
60].
Various encapsulation methods can be employed for optimizing nanobody formulations as spray and aerosol particles. One commonly used approach is the use of polymeric carriers such as liposomes or nanoparticles. These carriers can entrap nanobodies within their core or surface and provide protection against external stresses [
20].
Liposomes are lipid-based vesicles that can encapsulate hydrophilic or hydrophobic substances within their aqueous core or lipid bilayers. They offer excellent biocompatibility and can be easily modified to enhance stability and targeting capabilities [
61]. Nanoparticles, on the other hand, are solid colloidal particles with sizes ranging from 1 to 1000 nanometers. They can be made from various materials such as polymers, metals, or ceramics and can be engineered to control their size, surface charge, and drug release properties [
62].
In addition to polymeric carriers, other encapsulation techniques such as coacervation, microencapsulation, or spray drying can also be employed for nanobody formulations. Coacervation involves the phase separation of a polymer solution to form droplets that encapsulate the nanobodies [
63]. Microencapsulation utilizes techniques like emulsion or solvent evaporation to form small capsules containing the nanobodies [
64]. Spray drying involves converting a liquid formulation into dry particles using a spray nozzle and hot air [
65].
In brief, encapsulation techniques play a vital role in optimizing nanobody formulations for spray and aerosol particles. They provide protection against degradation, enable controlled release, and enhance targeting capabilities. By carefully selecting appropriate encapsulation methods and carriers, the effectiveness of nanobody-based therapies can be significantly improved for various applications in medicine and biotechnology.
6.2. Surface modifications technique:
Surface modification techniques for optimizing nanobody formulations as spray and aerosol particles involve modifying the surface properties of nanobodies to enhance their stability, solubility, and bioavailability when administered via spray or aerosol delivery methods [
66]. These techniques aim to improve the therapeutic efficacy and delivery efficiency of nanobodies [
66].
One common surface modification technique is PEGylation, which involves attaching polyethylene glycol (PEG) chains to the surface of nanobodies. PEGylation improves the stability and solubility of nanobodies by shielding them from proteolytic degradation and reducing their immunogenicity. The PEG chains also increase the hydrophilicity of nanobodies, allowing them to disperse more easily in aqueous solutions and form stable aerosol particles [
67].
Another technique is lipid-based surface modification, where lipids are conjugated to the surface of nanobodies [
68]. Lipid modifications can enhance the stability and membrane permeability of nanobodies, enabling better absorption through mucosal surfaces in the respiratory tract. This approach is particularly useful for developing inhalable nanobody formulations for respiratory diseases [
69].
In addition to PEGylation and lipid-based modifications, other surface modification strategies include coating nanobodies with biocompatible polymers like chitosan or albumin. These coatings can protect nanobodies from enzymatic degradation, improve their stability during storage, and facilitate their interaction with target cells or tissues [
70].
Overall, surface modification techniques combined with particle engineering methods play a crucial role in optimizing nanobody formulations for spray and aerosol delivery. These strategies enhance the stability, solubility, and bioavailability of nanobodies, enabling their effective administration via inhalation for various therapeutic applications.
7. Future prospects and challenges
Respiratory viral infections do not respect borders; therefore, a coordinated global response is essential. International collaboration is crucial for sharing information, resources, and expertise. Governments and organizations must work together to establish early warning systems and facilitate the rapid exchange of data during outbreaks [
71].
The potential for the development of new nanobody-based therapies is vast. Nanobodies have already been used to treat a variety of diseases, including cancer [
72], infectious diseases [
73], and autoimmune disorders [
74]. For example, a nanobody called caplacizumab has been approved by the FDA for the treatment of acquired thrombotic thrombocytopenic purpura (aTTP), a rare blood disorder [
75].
However, there are several regulatory hurdles and commercialization challenges that must be overcome before nanobody-based therapies can become widely available. One major challenge is the lack of standardized regulatory guidelines for nanobodies. Currently, there is no specific regulatory pathway for the approval of nanobody-based therapies [73, 76]. This can make it difficult for companies to navigate the regulatory process and obtain approval for their products.
One of the primary challenges is the delivery of nanobodies to the target site in the respiratory tract [
36]. The respiratory tract is a complex system, and delivering drugs to specific areas can be challenging. Nanobodies can be rapidly cleared from the lungs by mucociliary clearance or phagocytosis by alveolar macrophages [
77].
To overcome these challenges, researchers have developed various strategies for delivering nanobodies to the respiratory tract. One approach is to use nebulizers or inhalers that generate aerosol particles with a size range suitable for deposition in the lungs. This method has been successful in delivering biologics to the lungs [
78].
Another strategy is to modify nanobodies with chemical moieties that enhance their stability and prolong their residence time in the lungs. For example, PEGylation (the attachment of polyethylene glycol) has been shown to increase the half-life of nanobodies
in vivo and improve their pharmacokinetic properties [
52].
Another challenge associated with using nanobodies as spray and aerosol particles is their potential immunogenicity. Nanobodies are derived from camelids or sharks and may be recognized as foreign by human immune systems, leading to an immune response against them. This can reduce their efficacy or cause adverse effects [
21].
Another challenge is the high cost of developing and manufacturing nanobody-based therapies. Nanobodies are complex proteins that require specialized manufacturing processes. This can make it expensive to produce large quantities of these proteins for clinical trials and commercial use [
79].
To address this challenge, researchers have developed humanized versions of nanobodies that are less likely to elicit an immune response. Humanization involves replacing the non-human portions of the nanobody with human sequences, while retaining the antigen-binding properties of the original molecule [
3].
In addition to these challenges, there is also competition from other types of biologics, such as monoclonal antibodies. Monoclonal antibodies have been widely used in the development of new therapies and have established regulatory pathways for approval [
80].
9. Conclusion
This mini-review highlights the immense potential of nanobodies in revolutionizing the treatment of respiratory viral infections. The use of nanobodies as spray and aerosol particles offers several advantages, including enhanced delivery to the respiratory tract, increased stability, and reduced side effects compared to traditional therapies.
This article provides an overview of the current research and development efforts in this field, showcasing the promising results obtained from preclinical and clinical studies. Nanobodies have demonstrated their ability to effectively target viral antigens, neutralize viral particles, and modulate immune responses within the respiratory system.
Furthermore, the article discusses various strategies for optimizing nanobody formulations as spray and aerosol particles, such as encapsulation techniques and surface modifications. These approaches not only enhance the therapeutic efficacy but also improve patient compliance by enabling non-invasive administration.
The potential applications of nanobodies extend beyond treating respiratory viral infections. They can also be utilized for prophylaxis, post-exposure prophylaxis, and even as diagnostic tools. The versatility of nanobodies makes them a promising candidate for combating emerging viral threats and addressing challenges associated with antiviral drug resistance.
However, despite these remarkable advancements, several challenges remain to be addressed before nanobody-based therapies can be widely implemented. These include large-scale production, cost-effectiveness, regulatory considerations, and long-term safety assessments. Further research is needed to optimize these aspects and establish robust clinical evidence supporting their efficacy.
Author Contributions
MM performed overall writing of the paper including research, literature review, and analysis of data.; MA Supervision and editing of the review paper. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors acknowledge the Deanship of Scientific Research at University of Bahri for the supportive cooperation. We are grateful for technical support from Hiba Ibrahim.
Conflicts of Interest
None declared.
References
- Dabaja-Younis, H.; et al. SARS-CoV-2 and Seasonal Influenza: Similarity and Disparity. 2022. [CrossRef]
- McCallum, M.; Czudnochowski, N.; Rosen, L.E.; Zepeda, S.K.; Bowen, J.E.; Walls, A.C.; Hauser, K.; Joshi, A.; Stewart, C.; Dillen, J.R.; et al. Structural basis of SARS-CoV-2 Omicron immune evasion and receptor engagement. Science 2022, 375, 864–868. [Google Scholar] [CrossRef]
- Bhattacharya, M.; Chatterjee, S.; Lee, S.-S.; Chakraborty, C. Therapeutic applications of nanobodies against SARS-CoV-2 and other viral infections: Current update. International Journal of Biological Macromolecules 2023, 229, 70–80. [Google Scholar] [CrossRef]
- Jensen, N.; Kelly, A.H.; Avendano, M. Health equity and health system strengthening – Time for a WHO re-think. Glob. Public Heal. 2021, 17, 377–390. [Google Scholar] [CrossRef]
- Hassine, I.H. Covid-19 vaccines and variants of concern: A review. Rev. Med Virol. 2021, 32, e2313. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.C.; Goldstein, S.A.; Rasmussen, A.L.; Robertson, D.L.; Crits-Christoph, A.; Wertheim, J.O.; Anthony, S.J.; Barclay, W.S.; Boni, M.F.; Doherty, P.C.; et al. The origins of SARS-CoV-2: A critical review. Cell 2021, 184, 4848–4856. [Google Scholar] [CrossRef] [PubMed]
- Araf, Y.; Akter, F.; Tang, Y.; Fatemi, R.; Alam Parvez, S.; Zheng, C.; Hossain, G. Omicron variant of SARS-CoV-2: Genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med Virol. 2022, 94, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Hossain, A.D.; Jarolimova, J.; Elnaiem, A.; Huang, C.X.; Richterman, A.; Ivers, L.C. Effectiveness of contact tracing in the control of infectious diseases: a systematic review. Lancet Public Heal. 2022, 7, e259–e273. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, M.; Mohammed, A. Coping with the Ongoing SARS-CoV-2 Pandemic and Seasonal Influenza. J Infect Dis Epidemiol 2023, 9, 304. [Google Scholar]
- Underwood, D.J.; Bettencourt, J.; Jawad, Z. The manufacturing considerations of bispecific antibodies. Expert Opin. Biol. Ther. 2022, 22, 1043–1065. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, S.; Heukers, R.; Sornkom, J.; Kok, R.J.; Hvan Bergen En Henegouwen, P.M. Targeting tumors with nanobodies for cancer imaging and therapy. J. Control. Release 2013, 172, 607–617. [Google Scholar] [CrossRef]
- Van Heeke, G.; Allosery, K.; De Brabandere, V.; De Smedt, T.; Detalle, L.; de Fougerolles, A. Nanobodies® as inhaled biotherapeutics for lung diseases. Pharmacology & therapeutics 2017, 169, 47–56. [Google Scholar]
- Lake, F.; Yagami, H.; Kato, H.; Tsumoto, K.; Tomita, M.; Du, H.; Chen, G.; Wang, S.; Li, S.; Li, C.; et al. Antibodies: will their star continue to rise? BioTechniques 2019, 66, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, M.I.; Abdelmoneim, A.H.; Mahmoud, E.M.; Makhawi, A.M. Cytokine Storm in COVID-19 Patients, Its Impact on Organs and Potential Treatment by QTY Code-Designed Detergent-Free Chemokine Receptors. Mediat. Inflamm. 2020, 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Li, C.; Song, Y.; Ying, T.; Wu, Y. Inhalable antibodies for the treatment of COVID-19. Innov. 2022, 3. [Google Scholar] [CrossRef] [PubMed]
- Romao, E.; Morales-Yanez, F.; Hu, Y.; Crauwels, M.; Pauw, P.; Hassanzadeh, G.; Devoogdt, N.; Ackaert, C.; Vincke, C.; Muyldermans, S. Identification of Useful Nanobodies by Phage Display of Immune Single Domain Libraries Derived from Camelid Heavy Chain Antibodies. Curr. Pharm. Des. 2017, 22, 6500–6518. [Google Scholar] [CrossRef] [PubMed]
- Mei, Y.; Chen, Y.; Sivaccumar, J.P.; An, Z.; Xia, N.; Luo, W. Research progress and applications of nanobody in human infectious diseases. Front. Pharmacol. 2022, 13, 963978. [Google Scholar] [CrossRef]
- Wilken, L.; McPherson, A. Application of camelid heavy-chain variable domains (VHHs) in prevention and treatment of bacterial and viral infections. Int. Rev. Immunol. 2017, 37, 69–76. [Google Scholar] [CrossRef]
- Kim, J.Y.J.; Sang, Z.; Xiang, Y.; Shen, Z.; Shi, Y. Nanobodies: Robust miniprotein binders in biomedicine. Adv. Drug Deliv. Rev. 2023, 195, 114726. [Google Scholar] [CrossRef]
- Hye, T.; Moinuddin, S.M.; Sarkar, T.; Nguyen, T.; Saha, D.; Ahsan, F. An evolving perspective on novel modified release drug delivery systems for inhalational therapy. Expert Opin. Drug Deliv. 2023, 20, 335–348. [Google Scholar] [CrossRef]
- Loo, C.-Y.; Lee, W.-H.; Zhou, Q.T. Recent Advances in Inhaled Nanoformulations of Vaccines and Therapeutics Targeting Respiratory Viral Infections. Pharm. Res. 2023, 40, 1015–1036. [Google Scholar] [CrossRef]
- Gandhi, L.; Maisnam, D.; Rathore, D.; Chauhan, P.; Bonagiri, A.; Venkataramana, M. Respiratory illness virus infections with special emphasis on COVID-19. Eur. J. Med Res. 2022, 27, 1–21. [Google Scholar] [CrossRef]
- Krishnan, A.; Gangadaran, P.; Chavda, V.P.; Jogalekar, M.P.; Muthusamy, R.; Valu, D.; Vadivalagan, C.; Ramani, P.; Laishevtcev, A.; Katari, N.K.; et al. Convalescent serum-derived exosomes: Attractive niche as COVID-19 diagnostic tool and vehicle for mRNA delivery. Exp. Biol. Med. 2022, 247, 1244–1252. [Google Scholar] [CrossRef]
- Wang, M.-Y.; Zhao, R.; Gao, L.-J.; Gao, X.-F.; Wang, D.-P.; Cao, J.-M. SARS-CoV-2: Structure, Biology, and Structure-Based Therapeutics Development. Front. Cell. Infect. Microbiol. 2020, 10, 587269. [Google Scholar] [CrossRef] [PubMed]
- Bakherad, H.; Gargari, S.L.M.; Rasooli, I.; RajabiBazl, M.; Mohammadi, M.; Ebrahimizadeh, W.; Ardakani, L.S.; Zare, H. In Vivo Neutralization of Botulinum Neurotoxins Serotype E with Heavy-chain Camelid Antibodies (VHH). Mol. Biotechnol. 2013, 55, 159–167. [Google Scholar] [CrossRef]
- Asad, A.; Aamir, A.; Qureshi, N.E.; Bhimani, S.; Jatoi, N.N.; Batra, S.; Ochani, R.K.; Abbasi, M.K.; Tariq, M.A.; Diwan, M.N. Past and current advances in Marburg virus disease: a review. Le infezioni in medicina 2020, 28, 332–345. [Google Scholar] [PubMed]
- Du, L.; Yang, Y.; Zhang, X.; Li, F. Recent advances in nanotechnology-based COVID-19 vaccines and therapeutic antibodies. Nanoscale 2022, 14, 1054–1074. [Google Scholar] [CrossRef]
- Jia, Z.; Gong, W. Will Mutations in the Spike Protein of SARS-CoV-2 Lead to the Failure of COVID-19 Vaccines? J. Korean Med Sci. 2021, 36, e124. [Google Scholar] [CrossRef] [PubMed]
- Muyldermans, S. Nanobodies: Natural Single-Domain Antibodies. Annu. Rev. Biochem. 2013, 82, 775–797. [Google Scholar] [CrossRef]
- Rossotti, M.A.; et al. Arsenal of nanobodies shows broad-spectrum neutralization against SARS-CoV-2 variants of concern in vitro and in vivo in hamster models. Communications Biology 2022, 5, 933. [Google Scholar] [CrossRef]
- Valdés-Tresanco, M.S.; Molina-Zapata, A.; Pose, A.G.; Moreno, E. Structural Insights into the Design of Synthetic Nanobody Libraries. Molecules 2022, 27, 2198. [Google Scholar] [CrossRef]
- Wagner, H.J.; Wehrle, S.; Weiss, E.; Cavallari, M.; Weber, W. A Two-Step Approach for the Design and Generation of Nanobodies. Int. J. Mol. Sci. 2018, 19, 3444. [Google Scholar] [CrossRef] [PubMed]
- Jovcevska, I.; Muyldermans, S. The Therapeutic Potential of Nanobodies. BioDrugs 2020, 34, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Nainwal, N.; Sharma, Y.; Jakhmola, V. Dry powder inhalers of antitubercular drugs. Tuberculosis 2022, 135, 102228. [Google Scholar] [CrossRef] [PubMed]
- Kole, E.; Jadhav, K.; Shirsath, N.; Dudhe, P.; Verma, R.K.; Chatterjee, A.; Naik, J. Nanotherapeutics for pulmonary drug delivery: An emerging approach to overcome respiratory diseases. J. Drug Deliv. Sci. Technol. 2023, 81. [Google Scholar] [CrossRef]
- Chow, M.Y.; Pan, H.W.; Seow, H.C.; Lam, J.K. Inhalable neutralizing antibodies – promising approach to combating respiratory viral infections. Trends Pharmacol. Sci. 2022, 44, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Khairnar, S.V.; Jain, D.D.; Tambe, S.M.; Chavan, Y.R.; Amin, P.D. Nebulizer systems: a new frontier for therapeutics and targeted delivery. Ther. Deliv. 2022, 13, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Komalla, V.; et al. Advances in soft mist inhalers. Expert Opinion on Drug Delivery 2023, 20, 1055–1070. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-B.; Xu, D.; Bai, L.; Zhou, Y.-M.; Zhang, H.; Cui, Y.-L. A Review of Non-Invasive Drug Delivery through Respiratory Routes. Pharmaceutics 2022, 14, 1974. [Google Scholar] [CrossRef]
- Chellappan, D.K.; Prasher, P.; Saravanan, V.; Yee, V.S.V.; Chi, W.C.W.; Wong, J.W.; Wong, J.K.; Wong, J.T.; Wan, W.; Chellian, J.; et al. Protein and peptide delivery to lungs by using advanced targeted drug delivery. Chem. Interactions 2021, 351, 109706. [Google Scholar] [CrossRef]
- Douafer, H.; Andrieu, V.; Brunel, J.M. Scope and limitations on aerosol drug delivery for the treatment of infectious respiratory diseases. J. Control. Release 2020, 325, 276–292. [Google Scholar] [CrossRef]
- Li, B.; Qin, X.; Mi, L.-Z. Nanobodies: from structure to applications in non-injectable and bispecific biotherapeutic development. Nanoscale 2022, 14, 7110–7122. [Google Scholar] [CrossRef]
- Najmeddin, A.; Shapourabadi, M.B.; Behdani, M.; Dorkoosh, F. Nanobodies as powerful pulmonary targeted biotherapeutics against SARS-CoV-2, pharmaceutical point of view. Biochimica et Biophysica Acta (BBA)-General Subjects 2021, 1865, 129974. [Google Scholar] [CrossRef]
- Zare, H.; Aghamollaei, H.; Hosseindokht, M.; Heiat, M.; Razei, A.; Bakherad, H. Nanobodies, the potent agents to detect and treat the Coronavirus infections: A systematic review. Mol. Cell. Probes 2020, 55, 101692–101692. [Google Scholar] [CrossRef] [PubMed]
- Jin, B.-K.; Odongo, S.; Radwanska, M.; Magez, S. Nanobodies: a review of generation, diagnostics and therapeutics. International journal of molecular sciences 2023, 24, 5994. [Google Scholar] [CrossRef] [PubMed]
- Mir, M.A.; Mehraj, U.; Sheikh, B.A.; Hamdani, S.S. Nanobodies: The “magic bullets” in therapeutics, drug delivery and diagnostics. Human antibodies 2020, 28, 29–51. [Google Scholar] [CrossRef] [PubMed]
- Boonyaratanakornkit, J.; Boeckh, M.; Waghmare, A. Monoclonal antibodies for prophylaxis and treatment of respiratory viral infections. Curr. Opin. Infect. Dis. 2022, 35, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, D.; Kumar, U.; Gaur, V.; Salunke, D.M. Epitope-directed anti-SARS-CoV-2 scFv engineered against the key spike protein region could block membrane fusion. Protein Science 2023, 32, e4575. [Google Scholar] [CrossRef] [PubMed]
- Alabsi, W.; Eedara, B.B.; Encinas-Basurto, D.; Polt, R.; Mansour, H.M. Nose-to-Brain Delivery of Therapeutic Peptides as Nasal Aerosols. Pharmaceutics 2022, 14, 1870. [Google Scholar] [CrossRef] [PubMed]
- Bonini, M.; Usmani, O.S. The importance of inhaler devices in the treatment of COPD. COPD Res. Pr. 2015, 1, 9. [Google Scholar] [CrossRef]
- Bates, A.; Power, C.A. David vs. Goliath: The Structure, Function, and Clinical Prospects of Antibody Fragments. Antibodies 2019, 8, 28. [Google Scholar] [CrossRef]
- Mustafa, M.I.; Mohammed, A. Revolutionizing antiviral therapy with nanobodies: Generation and prospects. Biotechnol. Rep. 2023, 39, e00803. [Google Scholar] [CrossRef] [PubMed]
- Joseph, T.M.; Mahapatra, D.K.; Esmaeili, A.; Piszczyk, Ł.; Hasanin, M.S.; Kattali, M.; Haponiuk, J.; Thomas, S. Nanoparticles: Taking a Unique Position in Medicine. Nanomaterials 2023, 13, 574. [Google Scholar] [CrossRef]
- Valdés-Tresanco, M.S.; Molina-Zapata, A.; Pose, A.G.; Moreno, E. Structural Insights into the Design of Synthetic Nanobody Libraries. Molecules 2022, 27, 2198. [Google Scholar] [CrossRef] [PubMed]
- Obeng, E.M.; Dzuvor, C.K.; Danquah, M.K. Anti-SARS-CoV-1 and− 2 nanobody engineering towards avidity-inspired therapeutics. Nano Today 2022, 42, 101350. [Google Scholar] [CrossRef] [PubMed]
- Scherließ, R.; Bock, S.; Bungert, N.; Neustock, A.; Valentin, L. Particle engineering in dry powders for inhalation. Eur. J. Pharm. Sci. 2022, 172, 106158. [Google Scholar] [CrossRef]
- Forest, V.; Pourchez, J. Nano-delivery to the lung - by inhalation or other routes and why nano when micro is largely sufficient? Adv. Drug Deliv. Rev. 2022, 183, 114173. [Google Scholar] [CrossRef]
- Shi, M.; McHugh, K.J. Strategies for overcoming protein and peptide instability in biodegradable drug delivery systems. Adv. Drug Deliv. Rev. 2023, 199, 114904. [Google Scholar] [CrossRef]
- Machtakova, M.; Thérien-Aubin, H.; Landfester, K. Polymer nano-systems for the encapsulation and delivery of active biomacromolecular therapeutic agents. Chem. Soc. Rev. 2021, 51, 128–152. [Google Scholar] [CrossRef]
- Sanjanwala, D.; Patravale, V. Aptamers and nanobodies as alternatives to antibodies for ligand-targeted drug delivery in cancer. Drug Discov. Today 2023, 28, 103550. [Google Scholar] [CrossRef]
- Gbian, D.L.; Omri, A. Lipid-Based Drug Delivery Systems for Diseases Managements. Biomedicines 2022, 10, 2137. [Google Scholar] [CrossRef]
- Khan, S.; Hossain, M.K. Classification and properties of nanoparticles. In Nanoparticle-based polymer composites; Elsevier: 2022; pp. 15–54.
- Goncalves, A.G.; Hartzell, E.J.; Sullivan, M.O.; Chen, W. Recombinant protein polymer-antibody conjugates for applications in nanotechnology and biomedicine. Adv. Drug Deliv. Rev. 2022, 191, 114570. [Google Scholar] [CrossRef] [PubMed]
- Bharatia, R.; Kumar, S.; Yadav, V. Nano Technology-A Comprehensive Review. International Journal of Pharma Professional’s Research (IJPPR) 2023, 14, 94–105. [Google Scholar]
- Binesh, N.; Babaloo, H.; Farhadian, N. Microencapsulation: Spray drying. In Principles of Biomaterials Encapsulation: Volume One; Elsevier, 2023; pp. 271–296.
- Tundisi, L.L.; Ataide, J.A.; Costa, J.S.R.; Coêlho, D.d.F.; Liszbinski, R.B.; Lopes, A.M.; Oliveira-Nascimento, L.; de Jesus, M.B.; Jozala, A.F.; Ehrhardt, C.; et al. Nanotechnology as a tool to overcome macromolecules delivery issues. Colloids Surfaces B: Biointerfaces 2023, 222. [Google Scholar] [CrossRef]
- Panda, M.; Kalita, E.; Singh, S.; Kumar, K.; Prajapati, V.K. Nanobody-peptide-conjugate (NPC) for passive immunotherapy against SARS-CoV-2 variants of concern (VoC): a prospective pan-coronavirus therapeutics. Molecular Diversity 2022, 1–27. [Google Scholar] [CrossRef]
- Seo, Y.; Lim, H.; Park, H.; Yu, J.; An, J.; Yoo, H.Y.; Lee, T. Recent Progress of Lipid Nanoparticles-Based Lipophilic Drug Delivery: Focus on Surface Modifications. Pharmaceutics 2023, 15, 772. [Google Scholar] [CrossRef] [PubMed]
- El-Hammadi, M.M.; Arias, J.L. Recent Advances in the Surface Functionalization of PLGA-Based Nanomedicines. Nanomaterials 2022, 12, 354. [Google Scholar] [CrossRef] [PubMed]
- Khodabakhsh, F.; Shokri, S.; Jalili, N.; Moradi-Kalbolandi, S.; Dashtestani, F.; Farahmand, L. Anti-MUC1 nanobody conjugated by chitosan nanoparticle with enhancement of anti-proliferation activity in breast cancer cell lines. Chem. Pap. 2022, 77, 2229–2235. [Google Scholar] [CrossRef]
- Tusabe, F.; Tahir, I.M.; Akpa, C.I.; Mtaki, V.; Baryamujura, J.; Kamau, B.; Lidoroh, S.; Kobugabe, P.L.; Maaga, N.O.; Bongomin, F. Lessons Learned from the Ebola Virus Disease and COVID-19 Preparedness to Respond to the Human Monkeypox Virus Outbreak in Low- and Middle-Income Countries. Infect. Drug Resist. 2022, ume 15, 6279–6286. [Google Scholar] [CrossRef]
- Maali, A.; Gholizadeh, M.; Feghhi-Najafabadi, S.; Noei, A.; Seyed-Motahari, S.S.; Mansoori, S.; Sharifzadeh, Z. Nanobodies in cell-mediated immunotherapy: On the road to fight cancer. Front. Immunol. 2023, 14, 1012841. [Google Scholar] [CrossRef]
- Mei, Y.; Chen, Y.; Sivaccumar, J.P.; An, Z.; Xia, N.; Luo, W. Research progress and applications of nanobody in human infectious diseases. Front. Pharmacol. 2022, 13, 963978. [Google Scholar] [CrossRef]
- Zaravar, A.; May, X.; Stoddard, S. Rational Design of Epitope Binding Monobodies: New Tools for Autoimmune Therapy. FASEB J. 2017, 31. [Google Scholar] [CrossRef]
- Reid, J.H.; Durant, K.M.; Chen, S.-L.; Perissinotti, A.J.; King, R.; Khoriaty, R.; Marini, B.L. Role of caplacizumab in the treatment of acquired thrombotic thrombocytopenic purpura. J. Oncol. Pharm. Pr. 2020, 26, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Geigert, J. Regulatory Pathways Impacting Biopharmaceuticals. In The Challenge of CMC Regulatory Compliance for Biopharmaceuticals; Springer: 2023; pp. 31–55.
- Lim, P.N.; Cervantes, M.M.; Pham, L.K.; Rothchild, A.C. Alveolar macrophages: novel therapeutic targets for respiratory diseases. Expert Rev. Mol. Med. 2021, 23, e18. [Google Scholar] [CrossRef]
- Akhuemokhan, P.; Green, N.A.; Haddrell, A.; Lewis, D.; Reid, J.P.; Forbes, B. How to engineer aerosol particle properties and biopharmaceutical performance of propellant inhalers. Int. J. Pharm. 2023, 634, 122676. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Hu, Y.; Li, B.; Wang, H.; Shen, J. Applications of nanobodies in the prevention, detection, and treatment of the evolving SARS-CoV-2. Biochemical Pharmacology 2022, 115401. [Google Scholar] [CrossRef] [PubMed]
- Harris, E. RSV Vaccine, Monoclonal Antibody Safe, Effective in Phase 3 Trials. JAMA 2023, 329, 1444. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).