Submitted:
18 October 2023
Posted:
18 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Biomechanical aspects of movement asymmetries in sport.
3. Biological aspects of movement asymmetries
3.1. Genetic factors and asymmetry
- Genetic sensitivity to pain: according to the latest experimental data, a deficiency in the AMPD1 gene can cause symptoms such as pain and muscle weakness after exercise [16,17]. In asymmetric sports, dominant limbs are under more pressure than non-dominant limbs and, therefore, an athlete with higher pain tolerance will continue training with micro-injuries in the dominant limbs without feeling pain. This may lead to more serious injuries. In this case, the only way to detect abnormal changes in the athlete’s behaviour is to perform performance tests in time. If the dominant limbs move slower or have less force, then this may be a sign of a hidden injury. In the case of athletes with lower pain tolerance, even non-significant injuries will cause pain and impair movement performance. For such athletes, specialists recommend using yoga, biofeedback therapy and exercises to increase pain tolerance.
- Genetic predisposition to injuries: it was found that the genes AMPD1, GDF5, COL5A1 and IGF2 might be associated with increased injury occurrence in soccer players [16,18]. According to the latest research, the TT genotype of the GDF5 gene may be associated with an increased number of ankle and knee injuries as well as an increase in the total number of injuries and a decrease in the number of matches played [16]. This suggests that athletes who are genetically prone to certain types of injuries should be tested for such undetected injuries, especially in the dominant limbs.
- Genetic need for increased recovery after hard activity: The AMPD1 gene has been shown to be linked to such a need [17]. It was suggested that special attention should also be paid to the dominant limbs which will be under excessive physical load in asymmetric sports. The athlete should be given enough time for recovery. Obviously, the athletes with more endurance and a shorter recovery time will be favoured for such sports.
- Genetic deficit of muscle elasticity or power: There is evidence suggesting that titin (encoded by the TTN gene), a protein that is expressed in cardiac and skeletal muscles, is one of the factors responsible for the muscles' elasticity [19]. In some asymmetric sports, athletes with insufficient muscle elasticity may have issues with movements requiring a larger range of motion. Such athletes are recommended individual plans for training and nutrition [20,21].
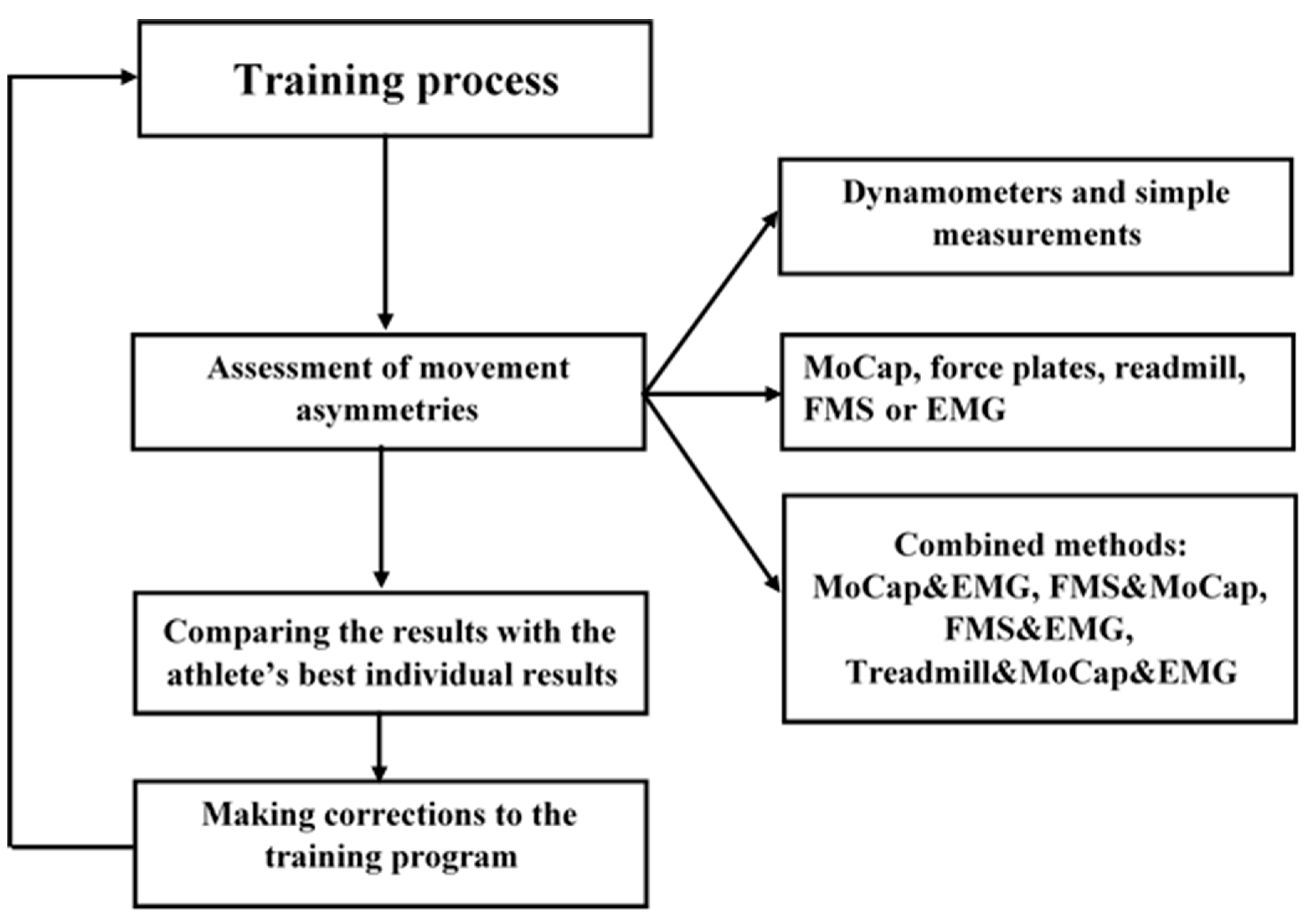
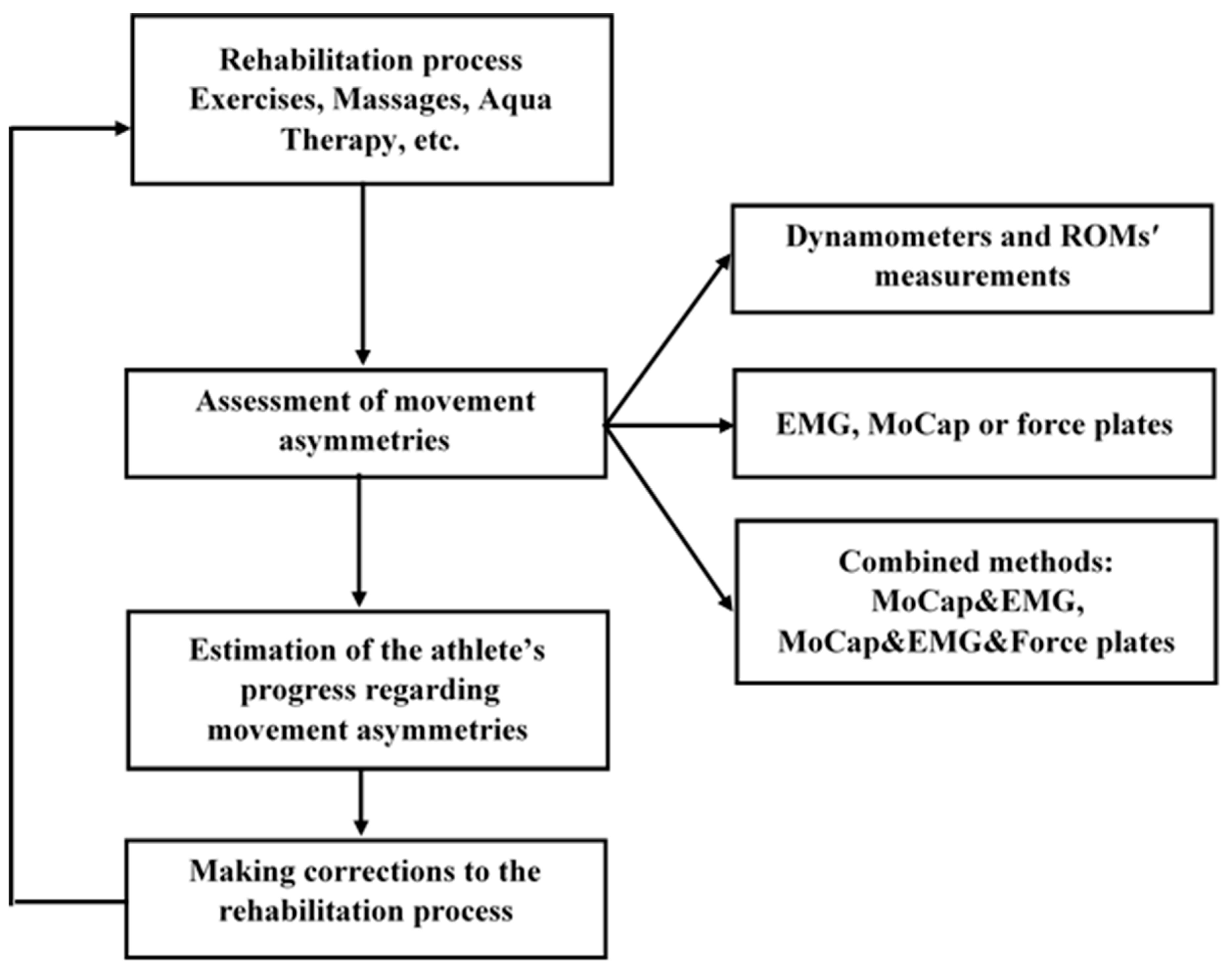
4. Detection of movement asymmetries and physical rehabilitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ocklenburg, S.; Mundorf, A. Symmetry and Asymmetry in Biological Structures. Proc Natl Acad Sci USA 2022, 119(28), e2204881119. [Google Scholar] [CrossRef]
- Mundorf, A.; Peterburs, J.; Ocklenburg, S. Asymmetry in the Central Nervous System: A Clinical Neuroscience Perspective. Front. Syst. Neurosci. 2021, 15, 733898. [Google Scholar] [CrossRef]
- Paillard, T. Asymmetry of Movement and Postural Balance and Underlying Functions in Humans. Symmetry 2023, 15(3), 759. [Google Scholar] [CrossRef]
- Kadri, M.A.; Noé, F.; Maitre, J.; Maffulli, N. Paillard, T. Effects of Limb Dominance on Postural Balance in Sportsmen Practicing Symmetric and Asymmetric Sports: A Pilot Study. Symmetry 2021, 13(11), 2199. [CrossRef]
- Afonso, J.; Peña, J.; Sá, M.; Virgile, A.; García-de-Alcaraz, A.; Bishop, C. Why Sports Should Embrace Bilateral Asymmetry: A Narrative Review. Symmetry 2022, 14(10), 1993. [Google Scholar] [CrossRef]
- Bishop, C.; Turner, A.; Read, P. Training Methods and Considerations for Practitioners to Reduce Inter-Limb Asymmetries. Strength Cond J 2018, 40, 40–46. [Google Scholar] [CrossRef]
- Carpes, F.P.; Mota, C.B.; Faria, I.E. On the Bilateral Asymmetry during Running and Cycling - a Review Considering Leg Preference. Phys Ther Sport. 2010, 11(4), 136–42. [Google Scholar] [CrossRef] [PubMed]
- Fort-Vanmeerhaeghe, A.; Bishop, C.; Buscà, B.; Aguilera-Castells, J.; Vicens-Bordas, J.; Gonzalo-Skok, O. Inter-Limb Asymmetries are Associated with Decrements in Physical Performance in Youth Elite Team Sports Athletes. PLoS One 2020, 15(3), e0229440. [Google Scholar] [CrossRef] [PubMed]
- Fort-Vanmeerhaeghe, A.; Gual, G.; Romero-Rodriguez, D.; Unnitha, V. Lower Limb Neuromuscular Asymmetry in Volleyball and Basketball Players. J Human Kinet 2016, 50, 135–144. [Google Scholar] [CrossRef]
- Hart, N.; Nimphius, S.; Spiteri, T.; Newton, R. Leg Strength and Lean Mass Symmetry Influences Kicking Performance in Australian Football. J Sports Sci Med 2014, 13, 157–165. [Google Scholar]
- Bishop, C.; Turner, A.; Gonzalo-Skok, O.; Read, P. Inter-Limb Asymmetry during Rehabilitation: Understanding Formulas and Monitoring the "Magnitude" and "Direction". Aspetar 2020, 18–22. [Google Scholar]
- Noyes, F.; Barber, S.; Mangine, R. Abnormal Lower Limb Symmetry Determined by Function Hop Tests after Anterior Cruciate Ligament Rupture. Amer J Sports Med 1991, 19, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Rohman, E.; Steubs, J.; Tompkins, M. Changes in Involved and Uninvolved Limb Function during Rehabilitation after Anterior Cruciate Ligament Reconstruction: Implications for Limb Symmetry Index Measures. Amer J Sports Med 2015, 43, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Svensson, K.; Eckerman, M.; Alricsson, M.; Magounakis, T.; Werner, S. Muscle injuries of the dominant or non-dominant leg in male football players at elite level. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 933–937. [Google Scholar] [CrossRef] [PubMed]
- DeLang, D.M.; Salamh, P.A.; Farooq, A.; Tabben, M.; Whiteley, R.; van Dyk, N.; Chamari, K. The dominant leg is more likely to get injured in soccer players: Systematic review and meta-analysis. Biol. Sport 2021, 38, 397–435. [Google Scholar] [CrossRef] [PubMed]
- McCabe, K.; Collins, C. Can Genetics Predict Sports Injury? The Association of the Genes GDF5, AMPD1, COL5A1 and IGF2 on Soccer Player Injury Occurrence. Sports (Basel) 2018, 6(1), 21. [Google Scholar] [CrossRef]
- Collins, C. Resistance Training, Recovery and Genetics: AMPD1 the Gene for Recovery. J. Athl. Enhanc. 2017, 6. [Google Scholar] [CrossRef]
- Posthumus, M.; September, A.V.; O’Cuinneagain, D.; van der Merwe, W.; Schwellnus, M.P.; Collins, M. The COL5A1 Gene Is Associated with Increased Risk of Anterior Cruciate Ligament Ruptures in Female Participants. Am. J. Sports Med. 2009, 37, 2234–2240. [Google Scholar] [CrossRef]
- Maciejewska-Skrendo, A.; Leźnicka, K.; Leońska-Duniec, A.; Wilk, M.; Filip, A.; Cięszczyk, P.; Sawczuk, M. Genetics of Muscle Stiffness, Muscle Elasticity and Explosive Strength. J Hum Kinet. 2020, 74, 143–159. [Google Scholar] [CrossRef]
- Guest, N.S.; Horne, J.; Vanderhout, S.M.; El-Sohemy, A. Sport Nutrigenomics: Personalized Nutrition for Athletic Performance. Front Nutr. 2019, 6, 8. [Google Scholar] [CrossRef]
- Guest, N.; Corey, P.; Vescovi, J.; El-Sohemy, A. Caffeine, CYP1A2 Genotype, and Endurance Performance in Athletes. Med Sci Sports Exerc. 2018, 50, 1570–8. [Google Scholar] [CrossRef]
- Egoyan, A.; Khipashvili, I. Use of Psychophysiological Computer Tests during the Process of Sportsmen’s Preparation, Physical Education. Sport and Science (PSS) 2017, 3, 8–17. [Google Scholar] [CrossRef]
- Wilkerson, G.B.; Simpson, K.A.; Clark, R.A. Assessment and Training of Visuomotor Reaction Time for Football Injury Prevention. J Sport Rehabil. 2017, 26(1), 26–34. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Rampinini, E.; Maffiuletti, N.; Marcora, S.M. A Vertical Jump Force Test for Assessing Bilateral Strength Asymmetry in Athletes. Med. Sci. Sport Exerc. 2007, 39, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Madruga-Parera, M.; Bishop, C.; Read, P.; Lake, J.; Brazier, J.; Romero-Rodriguez, D. Jumping-based Asymmetries are Negatively Associated with Jump, Change of Direction, and Repeated Sprint Performance, but not Linear Speed, in Adolescent Handball Athletes. J. Hum. Kinet. 2020, 71, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Hewit, J.; Cronin, J.; Hume, P. Asymmetry in Multi-Directional Jumping Tasks. Phys Ther Sport 2012, 13, 238–42. [Google Scholar] [CrossRef]
- Menzel, H.J.; Chagas, M.H.; Szmuchrowski, L.A.; Araujo, S.R.S.; de Andrade, A.G.P.; de Jesus-Moraleida, F.R. Analysis of Lower Limb Asymmetries by Isokinetic and Vertical Jump Tests in Soccer Players. J Strength Cond Res 2013, 27, 1370–7. [Google Scholar] [CrossRef]
- Paterno, M.V.; Ford, K.R.; Myer, G.D.; Heyl, R.; Hewett, T.E. Limb Asymmetries in Landing and Jumping 2 Years Following Anterior Cruciate Ligament Reconstruction. Clin J Sport Med 2007, 17, 258–62. [Google Scholar] [CrossRef]
- Roso-Moliner, A.; Lozano, D.; Nobari, H.; Bishop, C.; Carton-Llorente, A.; Mainer-Pardos, E. Horizontal Jump Asymmetries are Associated with Reduced Range of Motion and Vertical Jump Performance in Female Soccer Players. BMC Sports Sci Med Rehabil. 2023, 15(1), 80. [Google Scholar] [CrossRef]
- Bishop, C.; Pereira, L.A.; Reis, V.P.; Read, P.; Turner, A.N.; Loturco, I. Comparing the Magnitude and Direction of Asymmetry during the Squat, Countermovement and Drop Jump Tests in Elite Youth Female Soccer Players. J Sports Sci. 2020, 38, 1296–1303. [Google Scholar] [CrossRef]
- Costa Silva, J.R.L.; Detanico, D.; Dal Pupo, J.; Freitas, C. Bilateral Asymmetry of Knee and Ankle Isokinetic Torque in Soccer Players u20 Category. Braz J Kinanthro Hum Perf 2015, 17, 195–204. [Google Scholar] [CrossRef]
- Dos'Santos, T.; Thomas, C.; Jones, P.; Comfort, P. Asymmetries in Single and Triple Hop are not Detrimental to Change of Direction Speed. J Trainology 2017, 6, 35–41. [Google Scholar] [CrossRef]
- Dos'Santos, T.; Thomas, C.; Jones, P.A.; Comfort, P. Assessing Muscle Strength Asymmetry via a Unilateral Stance Isometric Mid-Thigh Pull. Int J Sports Physiol Perf 2017, 12, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Bishop, C.; Turner, A.; Jarvis, P.; Chavda, S.; Read, P. Considerations for Selecting Field-Based Strength and Power Fitness Tests to Measure Asymmetries. J Strength Cond Res. 2017, 31(9), 2635–2644. [Google Scholar] [CrossRef] [PubMed]
- Bishop, C.; Turner, A.; Read, P. Effects of Inter-Limb Asymmetries on Physical and Sports Performance: A Systematic Review. J. Sport. Sci. 2018, 36, 1135–1144. [Google Scholar] [CrossRef] [PubMed]
- Read, P.J.; McAuliffe, S.; Bishop, C.; Oliver, J.L.; Graham-Smith, P.; Farooq, M.A. Asymmetry Thresholds for Common Screening Tests and Their Effects on Jump Performance in Professional Soccer Players. J Athl Train. 2021, 56(1), 46–53. [Google Scholar] [CrossRef] [PubMed]
- Barrera-Domínguez, F.J.; Carmona-Gómez, A.; Tornero-Quiñones, I.; Sáez-Padilla, J.; Sierra-Robles, Á.; Molina-López, J. Influence of Dynamic Balance on Jumping-Based Asymmetries in Team Sport: A Between-Sports Comparison in Basketball and Handball Athletes. Int J Environ Res Public Health. 2021, 18(4), 1866. [Google Scholar] [CrossRef] [PubMed]
- Maloney, S.J. The Relationship Between Asymmetry and Athletic Performance: A Critical Review. J. Strength Cond. Res. 2019, 33, 2579–2593. [Google Scholar] [CrossRef] [PubMed]
- Bishop, C.; Turner, A.; Maloney, S.; Lake, J.; Loturco, I.; Bromley, T.; Read, P. Drop Jump Asymmetry is Associated with Reduced Sprint and Change-of-Direction Speed Performance in Adult Female Soccer Players. Sports (Basel). 2019, 7(1), 29. [Google Scholar] [CrossRef]
- Bishop, C.; Lake, J.; Loturco, I.; Papadopoulos, K.; Turner, A.; Read, P. Interlimb Asymmetries: The Need for an Individual Approach to Data Analysis. J Strength Cond Res. 2021, 35(3), 695–701. [Google Scholar] [CrossRef]
- Auvinet, E.; Multon, F.; Meunier, J. Lower Limb Movement Asymmetry Measurement with a Depth Camera. Annu Int Conf IEEE Eng Med Biol Soc. 2012, 6793–6. [Google Scholar] [CrossRef]
- Auvinet, E.; Multon, F.; Meunier, J. New Lower-Limb Gait Asymmetry Indices Based on a Depth Camera. Sensors 2015, 15, 4605–4623. [Google Scholar] [CrossRef]
- Thomas, C.; Dos'Santos, T.; Comfort, P.; Jones, P.A. Effect of Asymmetry on Biomechanical Characteristics During 180° Change of Direction. J Strength Cond Res. 2020, 34(5), 1297–1306. [Google Scholar] [CrossRef]
- Wu, J.; Liu, Y.; Wu, X. Early Identification of Gait Asymmetry Using a Dual-Channel Hybrid Deep Learning Model Based on a Wearable Sensor. Symmetry 2023, 15, 897. [Google Scholar] [CrossRef]
- Steinmetzer, T.; Wilberg, S.; Bönninger, I. Analyzing Gait Symmetry with Automatically Synchronized Wearable Sensors in Daily Life. Microprocess. Microsyst. 2020, 77, 103118. [Google Scholar] [CrossRef]
- Gulgin, H.; Hall, K.; Luzadre, A. 3D Gait Analysis with and without an Orthopedic Walking Boot. Gait Posture 2018, 59, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Viteckova, S.; Kutilek, P.; Svoboda, Z. Gait Symmetry Measures: A Review of Current and Prospective Methods. Biomed. Signal Process. Control 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Karimpour, R.; Krupenevich, R.L.; Miller, R.H.; Shim, J.K. Evaluation of Gait Asymmetry using Force Plates versus Accelerometer. J Mech Med Biol 2018, 18(2), 1850015. [Google Scholar] [CrossRef]
- Hamill, J.; Bates, B.T.; Knutzen, K.M. Ground Reaction Force Symmetry during Walking and Running. Res Q Exerc Sport 2013, 55(3), 289–293. [Google Scholar] [CrossRef]
- Dai, B.; Butler, R.J.; Garrett, W.E.; Queen, R.M. Using Ground Reaction Force to Predict Knee Kinetic Asymmetry Following Anterior Cruciate Ligament Reconstruction. Scand J Med Sci Sports 2014, 24, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Wojdala, G.; Trybulski, R.; Bichowska, M.; Krzysztofik, M. A Comparison of Electromyographic Inter-Limb Asymmetry During a Standard Versus a Sling Shot Assisted Bench Press Exercise. J Hum Kinet. 2022, 83, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Abdul Halim, H.N.; Azaman, A.; Manaf, H.; Saidin, S.; Zulkapri, I.; Yahya, A. Gait Asymmetry Assessment using Muscle Activity Signal: A Review of Current Methods. J Phys: Conference Series 2019, 1372, 012075. [Google Scholar] [CrossRef]
- Aedo-Muñoz, E.; Sanchez-Ramirez, C.; Moya-Jofre, C.; Bustamante-Garrido, A.; Araya-Ibacache, M.; Dal Bello, F.; Brito, C.J.; Miarka, B. Electromyographic Inter-Limb Asymmetry in Bench Press Exercise in Elite Paralympics Weightlifters. ISBS Proceedings Archive 2019, 37, 67. [Google Scholar]
- Palmieri-Smith, R.M; Villwock, M.; Downie, B.; Hecht, G.; Zernicke, R. Pain and Effusion and Quadriceps Activation and Strength. Journal of Athletic Training 2013, 48, 186–191. [Google Scholar] [CrossRef]
- Ithurburn, M. P.; Paterno M., V.; Ford, K. R.; Hewett, T. E.; Schmitt, L. C. Young Athletes with Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. American Orthopaedic Society for Sports Medicine 2015, 43. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional Movement Screening: the Use of Fundamental Movements as an Assessment of Function - Part 1. Int J Sports Phys Ther. 2014, 9(3), 396–409. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional Movement Screening: the Use of Fundamental Movements as an Assessment of Function - Part 2. Int J Sports Phys Ther. 2014, 9(4), 549–63. [Google Scholar]
- Triplett, C.R.; Dorrel, B.S.; Symonds, M.L.; Selland, C.A.; Jensen, D.D.; Poole, C.N. Functional Movement Screen Detected Asymmetry & Normative Values Among College-Aged Students. Int J Sports Phys Ther. 2021, 16(2), 450–458. [Google Scholar] [CrossRef] [PubMed]
- Marques, V.B.; Medeiros, T.M.; de Souza Stigger, F.; Nakamura, F.Y.; Baroni, B.M. The Functional Movement Screen (FMS™) in Elite Young Soccer Players Between 14 and 20 Years: Composite Score, Individual-Test Scores and Asymmetries. Int J Sports Phys Ther. 2017, 12(6), 977–985. [Google Scholar] [CrossRef] [PubMed]
- Mokha, M.; Sprague, P.A.; Gatens, D.R. Predicting Musculoskeletal Injury in National Collegiate Athletic Association Division II Athletes from Asymmetries and Individual-Test Versus Composite Functional Movement Screen Scores. J Athl Train. 2016, 51(4), 276–82. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.C.; Fuller, J.T.; Chalmers, S.; Debenedictis, T.A.; Zacharia, A.; Tarca, B.; Townsley, A.; Milanese, S. Combining Physical Performance and Functional Movement Screen Testing to Identify Elite Junior Australian Football Athletes at Risk of Injury. Scand J Med Sci Sports 2020, 30(8), 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Mrozek, A. et al. Assessment of the Functional Movement Screen Test with the Use of Motion Capture System by the Example of Trunk Stability Push-Up Exercise Among Adolescent Female Football Players. Vibrations in Physical Systems 2020, 31, 2020220-1. [Google Scholar]
- Chang, H.Y. et al. Automatic Image-Capture and Angle Tracking System Applied on Functional Movement Screening for Athletes. 1st IEEE International Conference on Knowledge Innovation and Invention (ICKII) 2018, 106–107. [Google Scholar]
- Whiteside, D.; Deneweth, J.M.; Pohorence, M.A.; Sandoval, B.; Russell, J.R.; McLean, S.G.; et al. Grading the Functional Movement Screen: A Comparison of Manual (Real-Time) and Objective Methods. J Strength Cond Res. 2016, 30(4), 924–33. [Google Scholar] [CrossRef]
- Saki, F. Functional Movement Screen in Elite Boy Basketball Players: A Reliability Study. PTJ 2017, 6(4), 211–216. [Google Scholar] [CrossRef]
- Jurak, I.; et al. Assessing Young Gymnasts’ Dynamic Posture: A Comparison of Methods. J. Appl. health sci. 2020, 6, 129–135. [Google Scholar] [CrossRef]
- Lebreton, G.; Géminard, C.; Lapraz, F.; Pyrpassopoulos, S.; Cerezo, D.; Spéder, P.; Ostap, E.M.; Noselli, S. Molecular to Organismal Chirality is Induced by the Conserved Myosin 1D. Science 2018, 362(6417), 949–952. [Google Scholar] [CrossRef]
- Alsafwani, R.S.; Nasser, K.K.; Shinawi, T.; Banaganapalli, B.; Elsokary, H.A.; Zaher, Z.F.; Shaik, N.A.; Abdelmohsen, G.; Al-Aama, J.Y.; Shapiro, A.J.; Al-Radi, O.; Elango, R.; Alahmadi, T. Novel MYO1D Missense Variant Identified Through Whole Exome Sequencing and Computational Biology Analysis Expands the Spectrum of Causal Genes of Laterality Defects. Front. Med. 2021, 8, 724826. [Google Scholar] [CrossRef]
- Błach, W.; Rydzik, Ł.; Stanula, A.; Cynarski, W.J.; Ambroży, T. Injury Symmetry in Judo. Symmetry 2023, 15, 13. [Google Scholar] [CrossRef]
- Sterkowicz, S.; Lech, G.; Blecharz, J. Effects of Laterality on the Technical/Tactical Behaviour in View of the Results of Judo Fights. Arch. Budo 2010, 6, 173–177. [Google Scholar]
- Korobeinikova, L.; Korobeynikov, G.; Cynarski, W.; Borysova, O.; Kovalchuk, V.; Matveev, S.; Vorontsov, A.; Novak, V. Tactical Styles of Fighting and Functional Asymmetry of the Brain Among Elite Wrestlers. Ido Mov. Cult. J. Martial Arts Anthropol. 2020, 20, 433–443. [Google Scholar]
- Ruas, C.V.; Brown, L.E.; Pinto, R.S. Lower-extremity side-to-side strength asymmetry of professional soccer players according to playing position. Kinesiology 2015, 2, 188–192. [Google Scholar]
- Banse, H. , & Cribb, A. E.. Comparative efficacy of oral meloxicam and phenylbutazone in 2 experimental pain models in the horse. Canad Vet J. 2017, 58(2), 157. [Google Scholar]
- Persson-Sjodin, E., Hernlund, E., Pfau, T., Haubro Andersen, P., Holm Forsström, K., & Rhodin, M. Effect of meloxicam treatment on movement asymmetry in riding horses in training. PLoS One 2019, 14, e0221117.
- Ricci, A.; Roviello, G. N. Exploring the Protective Effect of Food Drugs against Viral Diseases: Interaction of Functional Food Ingredients and SARS-CoV-2, Influenza Virus, and HSV. Life 2023, 13, 402. [Google Scholar] [CrossRef]
- Baker, S.; Gilhen-Baker, M.; Roviello, G. N. The Role of Nutrition and Forest-Bathing in the Physical Rehabilitation of Physically Inactive Patients: From the Molecular Aspects to New Nature-Inspired Techniques. International Journal of Environmental Research and Public Health 2022, 20, 793. [Google Scholar] [CrossRef]
- Roviello, V.; Gilhen-Baker, M.; Vicidomini, C.; Roviello, G. N. Forest-bathing and physical activity as weapons against COVID-19: A review. Environmental chemistry letters 2022, 20, 131–140. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



