Introduction
Small bowel non-meckelian (SBNMD) diverticulosis is an uncommon disorder with a prevalence ranging from 0.06% to 4% [
1,
2,
3,
4]. While diverticula are more commonly found in the colon, they can also occur in the small bowel. It typically occurs in the 6th and 7th decade of life, with a significant majority of 80% being over 40 years old at the time of the diagnosis [
4]. Multiple jejunal diverticula, especially in the proximal site, are detected in 80% of cases. The remaining 15% of diverticula are located in the ileum while the remaining 5% occur in both the jejunum and ileum [
5]. Both are usually smaller in size multiple and isolated. From a pathological point of view, SBNMD are deemed 'false,' in contrast to Meckel's diverticula located on the anti-mesenteric site [
1,
2]. The wide range of atypical symptoms, such as vague abdominal pain, flatulence, diarrhea, and melaena, in combination with its rare occurrence, can lead to delayed diagnosis and extreme mortality rates [
6,
7]. Complications frequently occur with colonic diverticula, which are commonly described. These complications include inflammation, perforation, bleeding, and obstruction. The primary diagnostic tool that we use is abdominal computed tomography (CT) [
4].
On the other hand, SARS-CoV-2 virus (COVID-19), primarily targets the respiratory tract through its affinity for ACE2 receptors. These receptors are also prevalent in intestinal cells, leading to symptoms affecting both the respiratory and gastrointestinal systems. COVID-19, affects the bloodstream, causing hyperactivity in platelets and cytokine storms. This can result in damage to the gut barrier and changes to the gut microbiota. Additionally, intestinal vessel thrombosis can occur, leading to malabsorption and malnutrition. These negative effects can increase the severity of the disease and have both short and long-term consequences, including gut inflammation and worsening of inflammatory bowel diseases [
8,
9].
Management of SBNMD, typically includes a combination of conservative and surgical interventions. The specific treatment approach depends on the rupture’s severity, complications, and the patient's overall condition. Every stable patient with localized inflammation and without any radiologic sign of perforation is treated conservatively with bowel rest and broad-spectrum IV antibiotics. If the patient does not show clinical improvement within 48-72 hours or if generalized peritonitis or perforation is detected, an exploratory laparotomy may be necessary, which involves small bowel resection with anastomosis [
5,
6,
7].
Herein, we present two cases of SBNMD, one with rupture in COVID-19 positive patient and one incidentally discovered. In addition, a review with a statistical analysis of all the cases reported in past literature, discussing the most common clinical features, was performed. Also, we proposed the role of laparoscopic surgery as a therapeutic option in disease management.
Materials and Methods
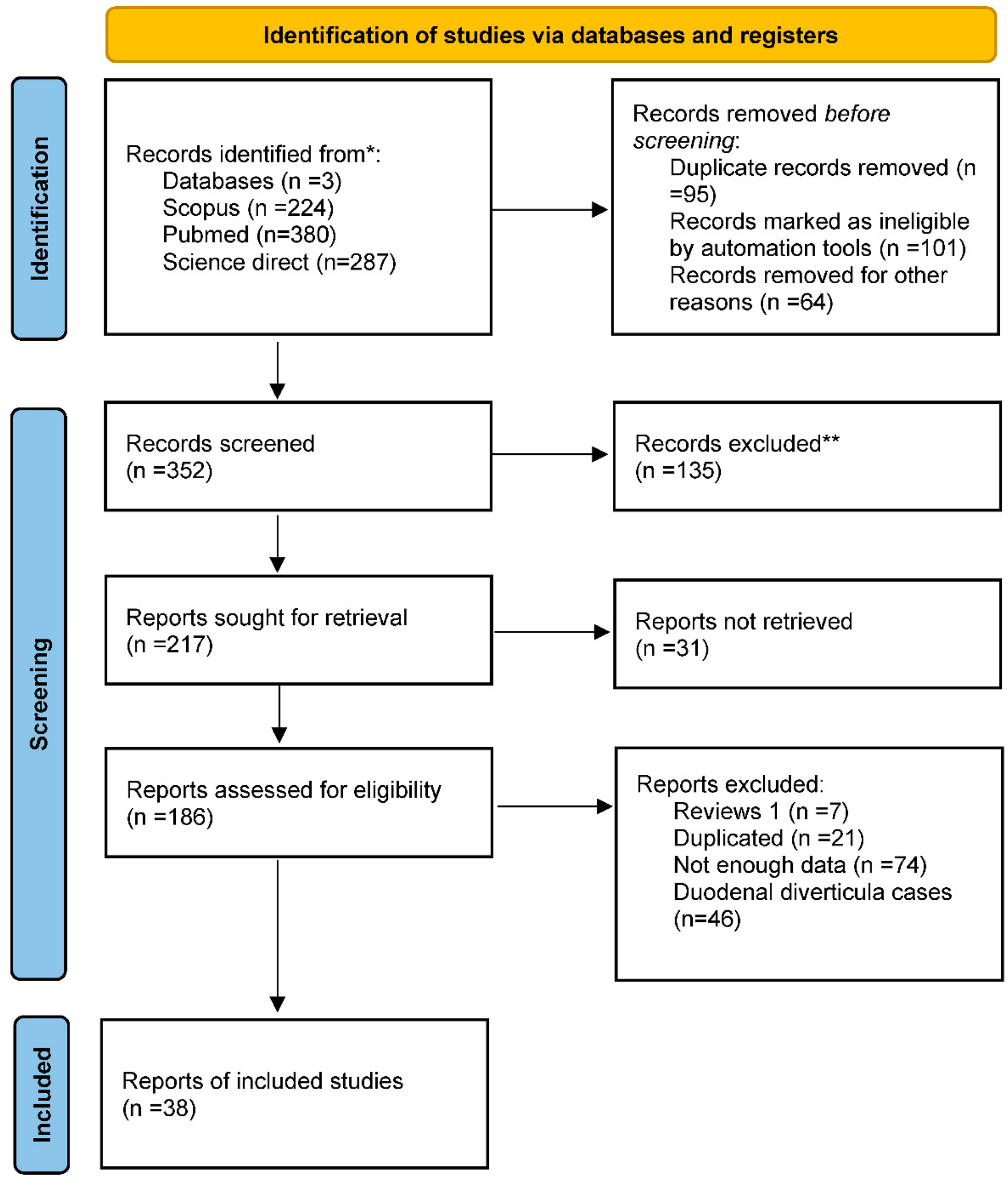
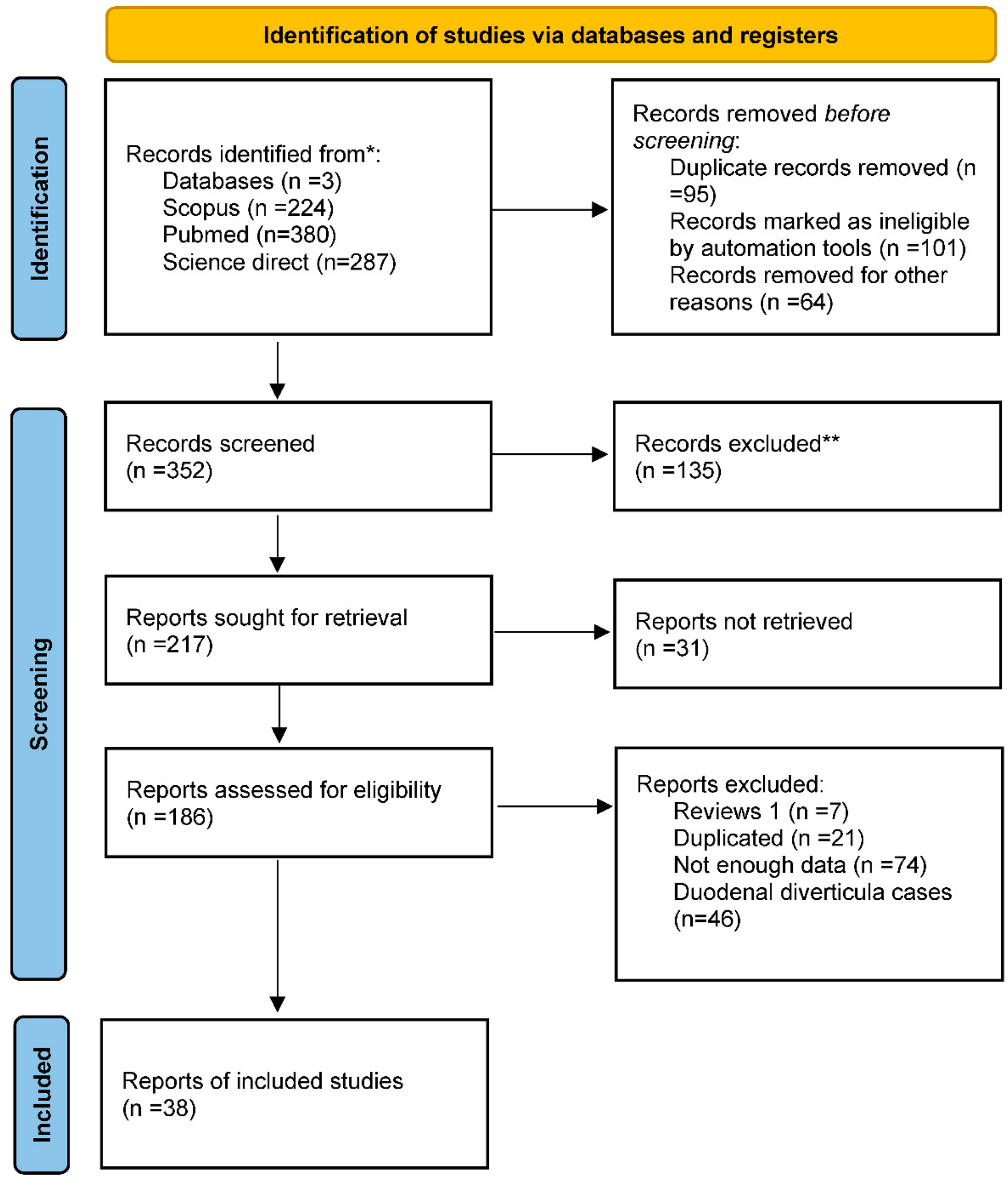
A literature review was performed using PubMed, Scopus, and Science Direct. The search terms employed were “small bowel diverticulosis,” “jejunal diverticulitis,” and “Ileus diverticulitis.” Since 2010, 352 articles have been published.
Among these, 217 well-documented papers were identified. There were no restrictions on the age of the articles included in this review. One hundred eighty-six articles were in English, while 31 were in other languages. All these studies were carefully studied. We had only full texts, case reports, and case series articles in the final assessment. We finally selected 38 articles (41 patients), and a database with the patients' characteristics was created and shown in Prisma chart below.
The database included sex, age, diverticula location, symptoms, diagnostic methods, treatment management, and complications. The cases that fulfilled all these seven criteria were included in the statistical analysis. Two additional cases were added from clinical experience of the authors of this article. Thus, a total of 43 patients were included in the statistical analysis. After obtaining ethical approval and participant consent, personal data were removed, and all clinical data were collected. Descriptive statistics were used to express the results appropriately. Means, medians, and SD were used for continuous variables and frequencies for categorical variables. Statistical significance was set at
p <0 .05. Statistical analysis was performed using SPSS version 25 (SPSS Inc., Chicago, IL, USA).
Case Report
Case 1
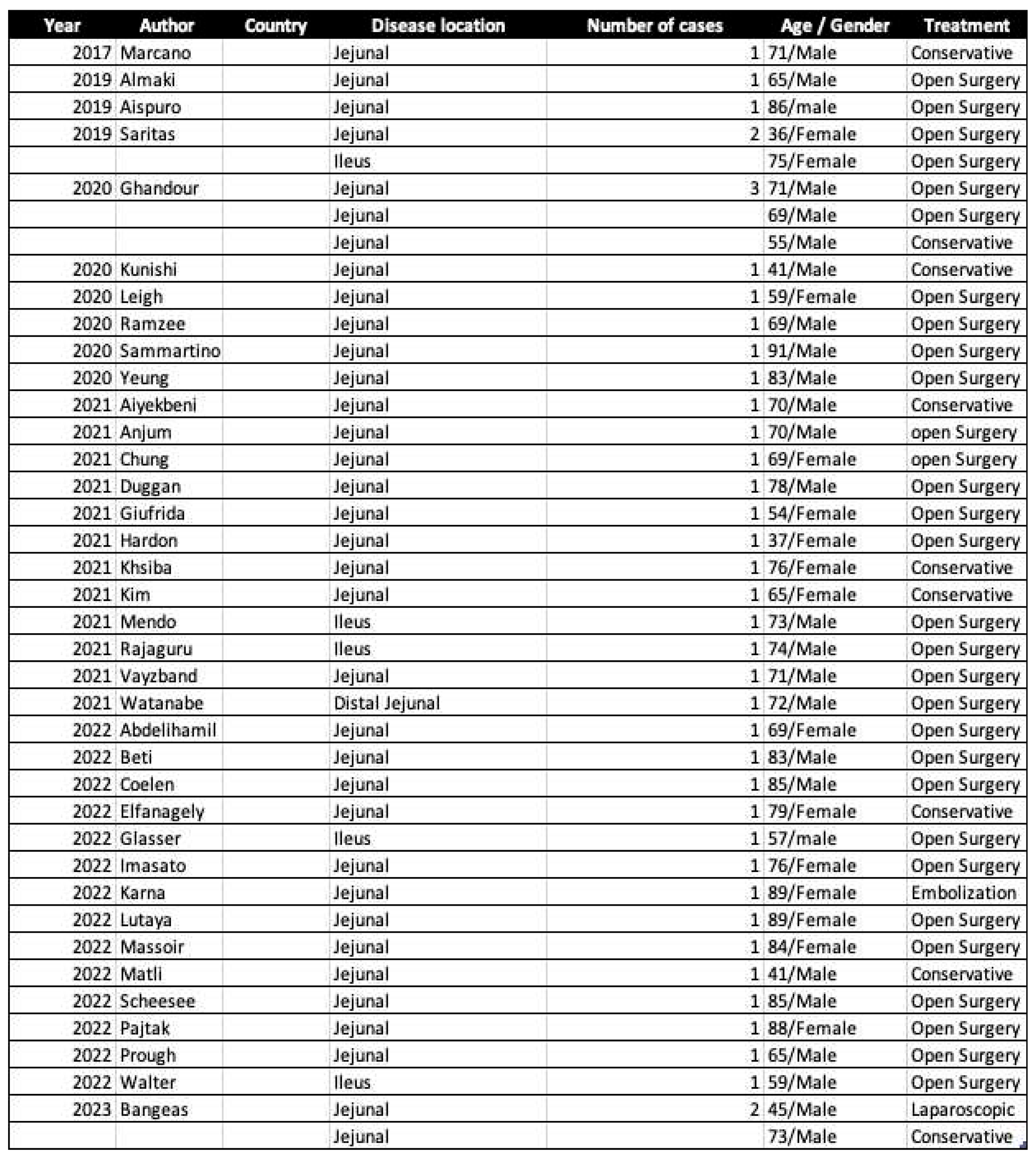
A 45-year-old man presented to our emergency department, complaining about abdominal pain, particularly on the left side, that had been ongoing for 48 hours. Clinical examination revealed abdominal distension and tenderness. Laboratory results showed mildly elevated white blood cell count (9.93 × 10
9/L) and neutrophilia (88%). During the preoperative examination, it was discovered incidentally that the patient has contracted COVID-19 infection. An emergency CT scan of the abdomen revealed free air, fluid collection in the left abdomen, and two small bowel diverticula in the jejunum with local phlegm (
Figure 1a). From patient past medical history, there is no record of diverticula except experiencing upper gastrointestinal bleeding 11 years ago. Additionally, the patient had a history of cardiac arrest and pacemaker implanted since 15 years.
Informed written consent was obtained from the patient, and he was taken to the operating theater for exploratory laparoscopy, where a ruptured part of the jejunum was found (
Figure 1b). A partial small bowel laparoscopic enterectomy was carried out with primary side-to-side intracorporeal anastomosis with an endoscopic linear stapler and PDS 2-0 running suture. The patient was discharged from the surgery without drainages and was receive clear fluids in the afternoon after the surgery. He was mobilized six hours after surgery. Throughout the hospitalization period, remained stable, and on the third postoperative day, they were discharged. Patient follow fast-track post-operative protocol (ERAS), which includes mobile communication and visits from a specialist nurse.
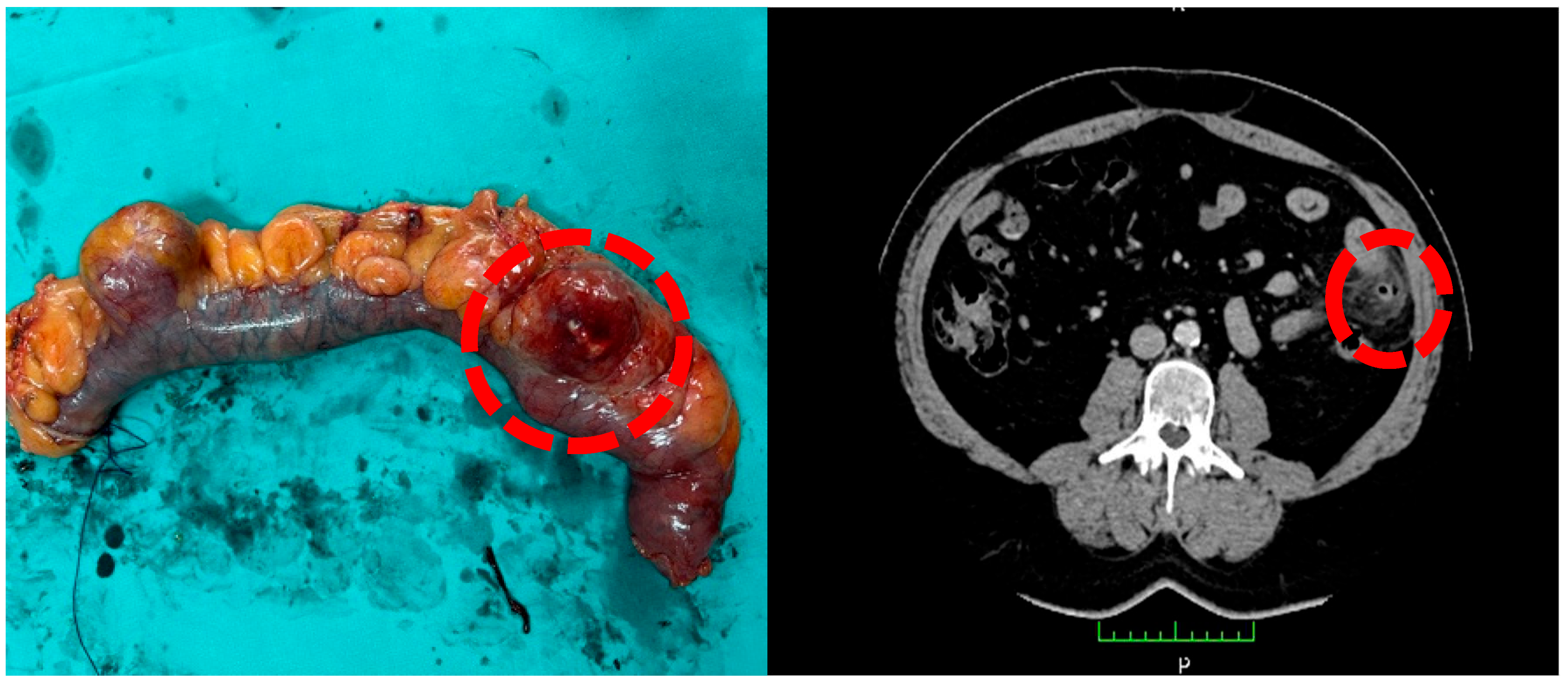
Case 2
A 75-year-old man presented to our department due to a rectal tumor of 9cm from the anal verge. The patient underwent an operating theater for a scheduled low anterior resection. During the operation, multiple jejunal diverticula were identified (
Figure 2). Upon further examination, it was determined that these diverticula were not inflamed, therefore obviating the necessity for their removal.
Results
After conducting a literature review, we have determined the characteristics of jejunal diverticula based on various factors, including sex, age, length, location of the diverticula, significant symptoms, type of procedure, survival rates, and potential complications categorized by Clavien-Dindo classification [
2,
4,
5,
6,
7,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44].
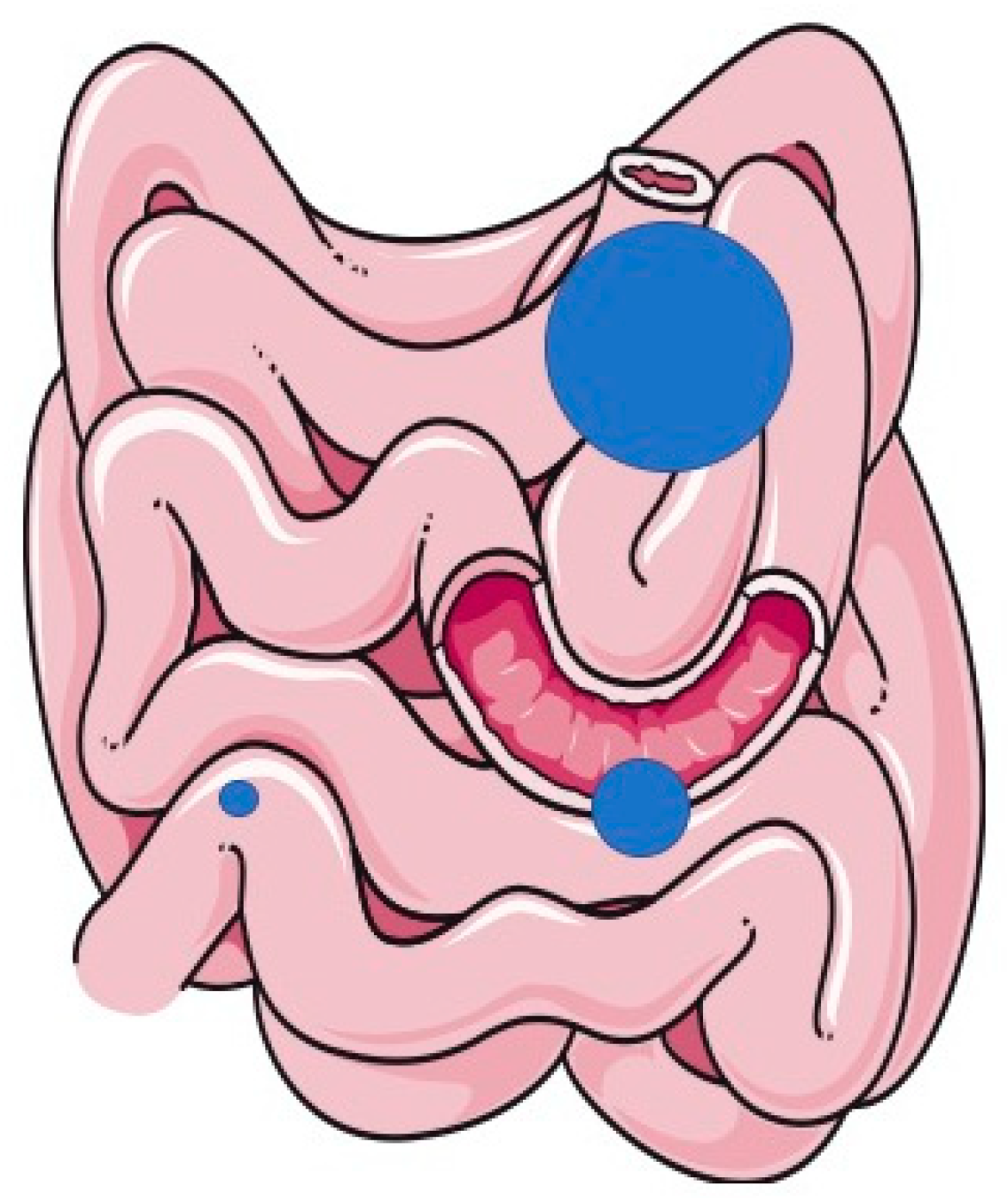
Regarding sex, 62.79% were male (27 patients), whereas 37.20% were female (16 patients). The ratio between men and women was 2:1, suggesting a male predominance in the reported population. Our Database is shown below (Index 1).
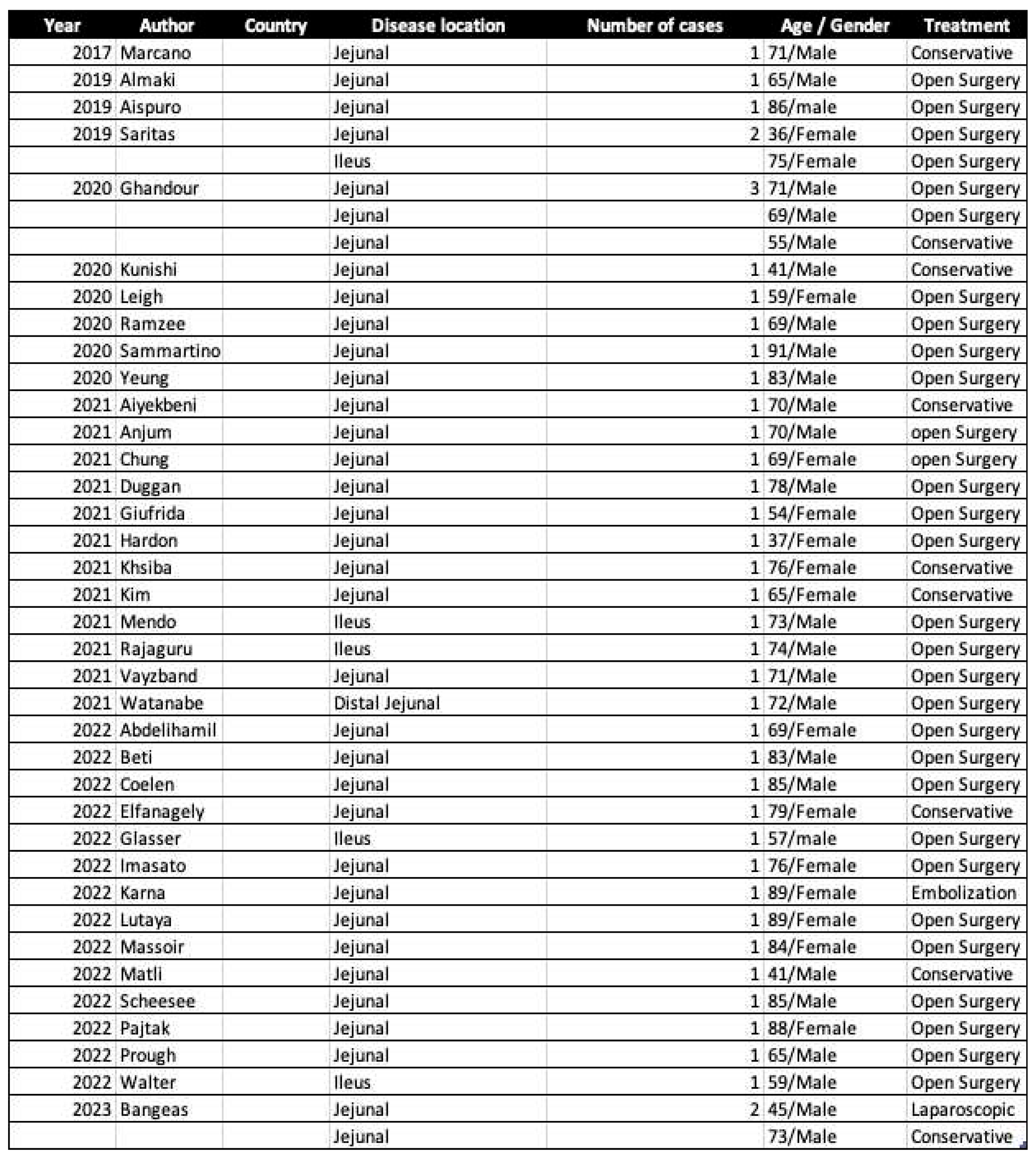
Based on our database (Index 1), it appears that diverticula are typically found in the Jejunum, as illustrated in
Figure 3 (31 patients, 72.09%), with only 8 patients found in the proximal ileus (18.60%) and 4 patients in distal ileus (9.30%).
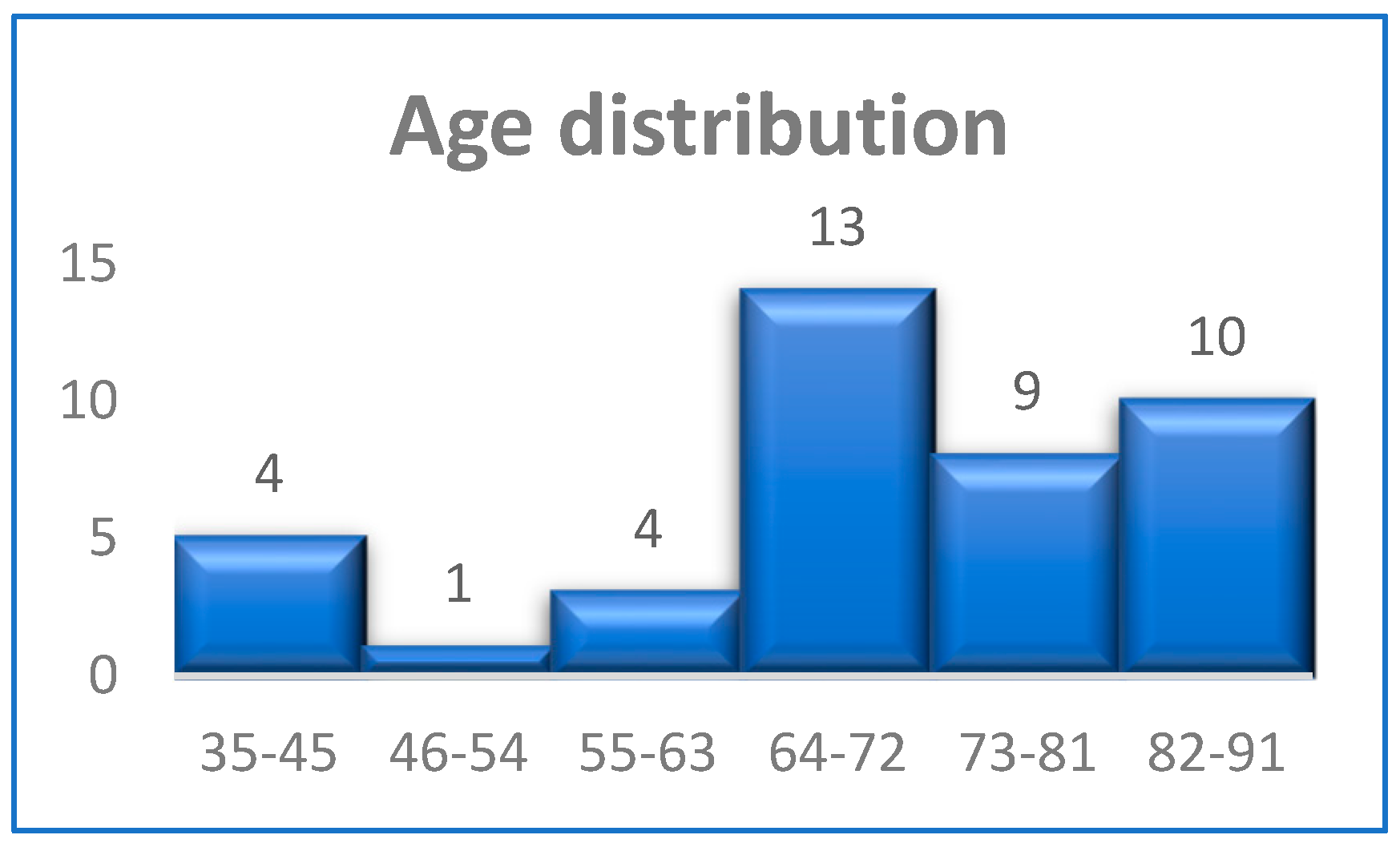
The age distribution is shown in
Figure 4, from which it is concluded that jejunum diverticula most frequently appeared in the age ranges of 64-72, 73-81, and 82–91 years. Median age of the 43 cases (100%) was 71 ± 14.40 years, ranging from 36 to 91 years. The distribution of age among male and female patients was compared, and it was found that the age at which the tumor appeared did not differ statistically between males and females (70.12± 13.27 and 70 ± 15.99 years, respectively,
p = 0.98).
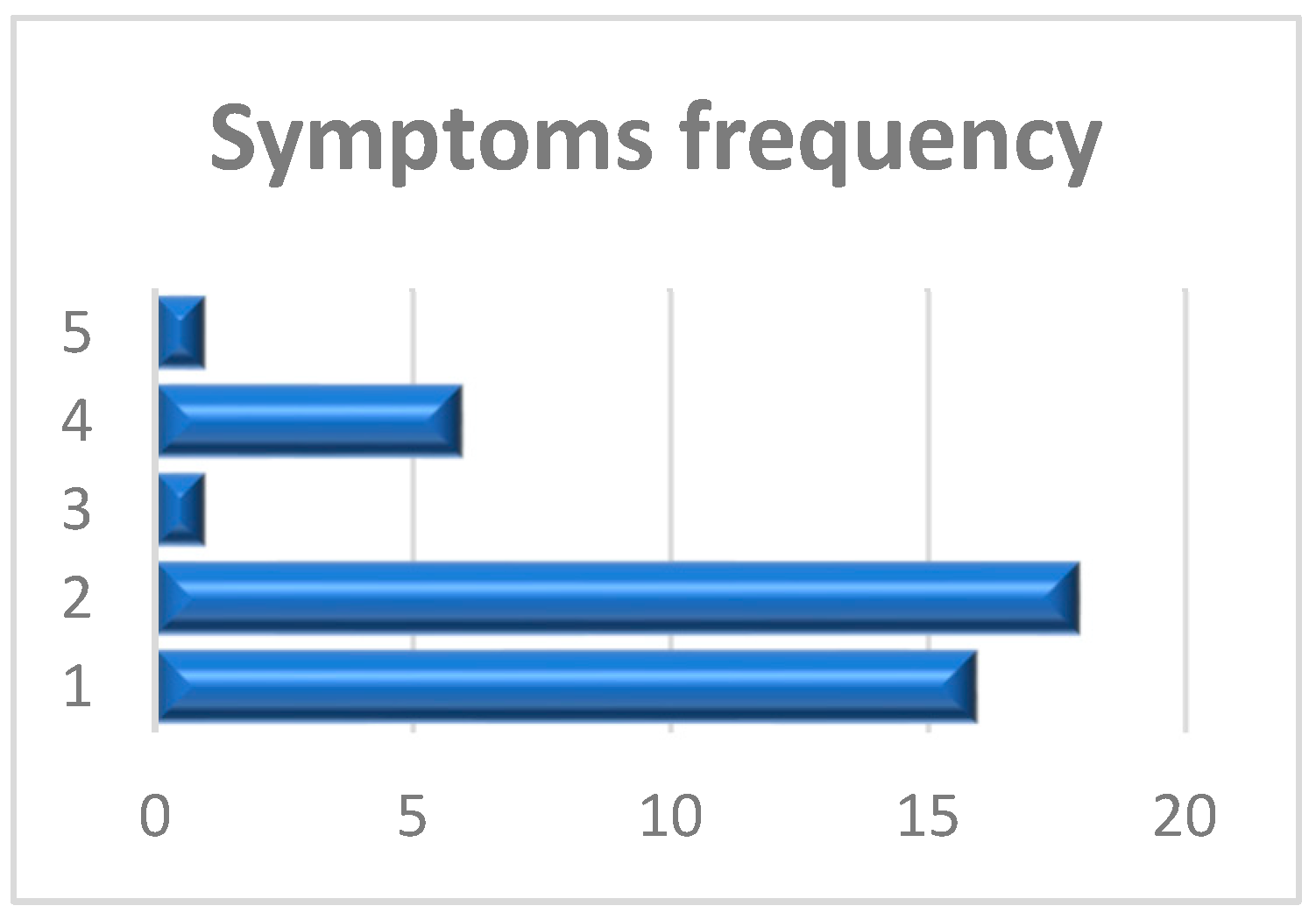
Symptoms of SBNMD were also evaluated and shown in
Figure 5. Symptoms were characterized as inflammatory without rupture (
1) (16 patients, 37.20%), perforation (
2) (18 patients, 41.86%), bleeding (
3) (1 patient, 2.32%), (
4) obstruction (6 patients, 13.95%) and non-specific/Random (
5) (2 patient, 4.65%).
Out of 43 patients, only 8 (18.60%) received conservative treatment, while the majority (35 patients, 81.40%) required surgical intervention. Diverticula were discovered accidentally in 2 patients (4.65%) without signs of inflammation, and no interventions were performed. Concerning the type of procedure, open laparotomy was performed in 33 (94.28%) out of 35 patients. On the other hand, only two patients (5.71%) underwent the laparoscopic approach.
Median hospitalization was 7 ± 2.37 days, ranging from 3 to 16 days, depending on the treatment option. Hospitalization periods were found to be prolonged for patients who underwent open surgery or were treated using conservative methods.
Regrettably, one patient (2.85%) succumbed to their illness during the post-operative period, while the remaining patients experienced an uncomplicated and stable state of health.
Discussion
Jejuno-ileal diverticulitis, a condition involving inflammation of the diverticula in the small intestine, was initially identified by Sommering in 1794 and further researched by Sir Astley Cooper in 1804 [
1]. Due to its low prevalence, there have been only a few reported cases since then. Pathophysiology still needs to be fully understood. These are false diverticula of the small intestine, similar to colonic diverticula, where the mucosa and submucosa protrude through the muscular wall. We assume that an elevated intraluminal pressure combined with bowel wall weakness causes these cases. While they are usually asymptomatic, they can lead to life-threatening outcomes when complicated [
2,
5,
8,
11].
In the case of uncomplicated SBNMDs, no specific symptoms can lead to the diagnosis. These patients usually complain of abdominal pain, which sometimes radiates in the back, nausea, emesis, fever, and constipation. Due to the greater frequency in the elderly population, where many other health issues or previous surgical history can co-exist, diagnosis could be challenging [
2,
5,
7,
27,
28,
29,
30,
31,
32,
33,
34].
Numerous reports have emerged during the COVID-19 period regarding inflammation and bowel ruptures. This is a matter of concern, and we should examine these reports closely to determine the root cause of such incidents and identify measures to mitigate them in the future. In some studies, it seems that Gut enterocytes have been determined to be a significant target of the COVID–19 virus. The virus can enter the cells of the ileum, colon, and esophagus by using Angiotensin-converting enzyme 2 receptors and transmembrane serine protease 2 (TMPRSS2) as a mediator [
8,
9]. This can lead to gut inflammation and exacerbation of inflammatory bowel diseases, causing negative effects that can worsen the disease severity in both the short and long term [
9].
A comprehensive patient history must be obtained to rule out other conditions such as appendicitis, cholecystitis, colonic diverticulitis, pancreatitis, bowel obstruction, or foreign body perforation [
3,
4,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
24,
34]. An abdominal X-ray can help detect perforation or obstruction but cannot establish a diagnosis on its own. The surgeon must maintain a heightened level of suspicion to ensure the procedure's accuracy and safety. This involves being vigilant and attentive to any potential risks or complications that may arise during the surgery.
Currently, the gold standard imaging study for abdominal scans still involves using CT scans with both oral and intravenous contrast. Due to the rarity of the disease, there are instances in the literature where the diagnosis was not clearly established before the exploratory intervention but only during exploratory laparoscopy. In our cases, the preoperative CT scan was exact for the site and the number of the ill-defined diverticula [
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40].
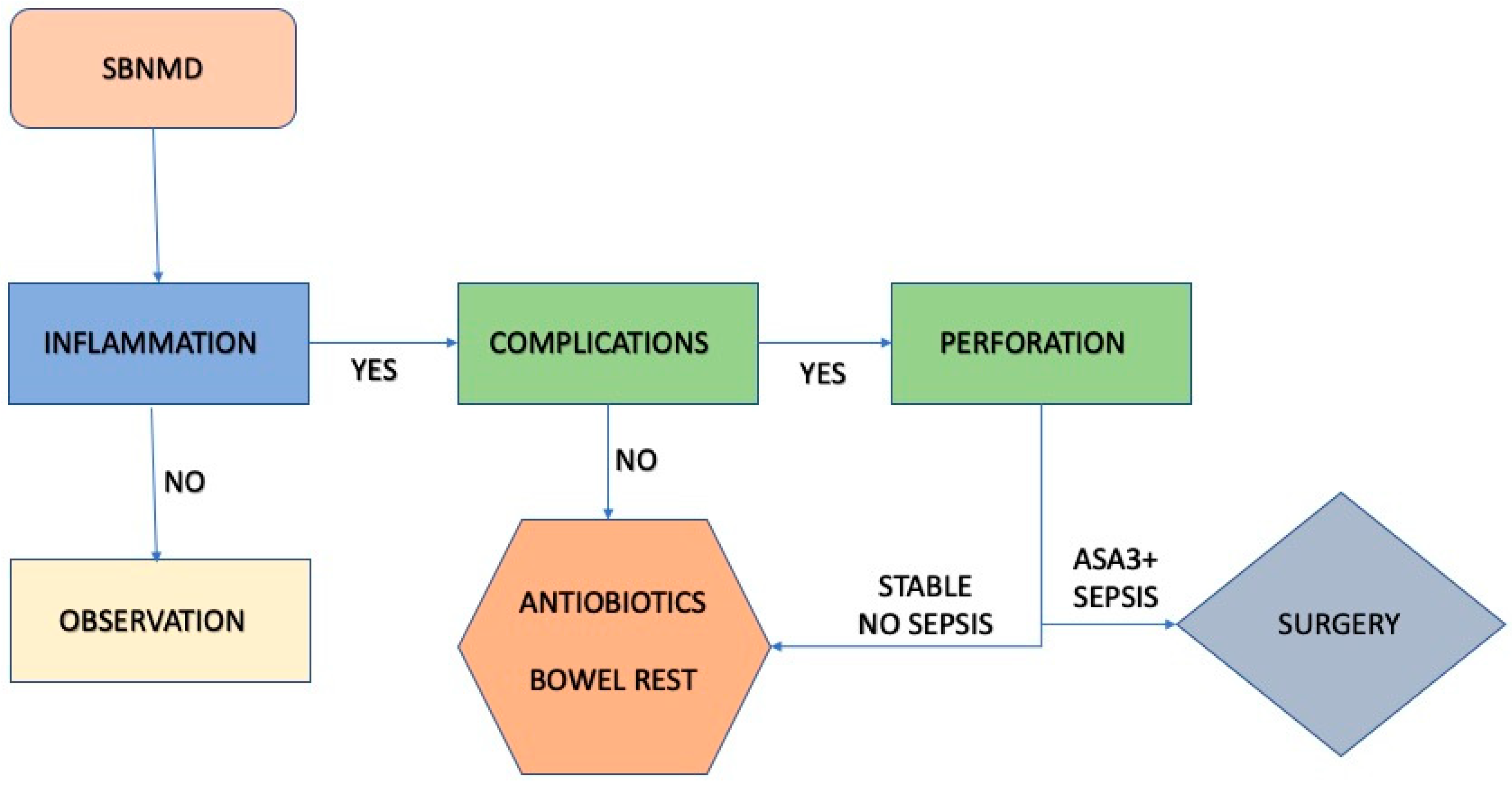
As mentioned before, inflammation is the most common complication, followed by perforation. First-line treatment for uncomplicated cases involves IV antibiotics and bowel rest strategies. An annual monitoring protocol, including a clinical examination and CT scan of the abdomen, is necessary in case of accidental detection. Prior history-based clinical suspicion is also important [
4,
28,
35,
40,
41,
42,
43,
44,
45].
Surgical intervention must be undertaken without delay in cases of sepsis, instability or severe comorbidities following perforation. These complications could be severe and lead to serious difficulties if not addressed promptly. The type of procedure (open or laparoscopic) does not seem to play an important role and appears to be determined by the surgeon’s preference and center experience. If a patient has a good performance status, surgeons could perform an exploratory laparoscopy and proceed with a conversion procedure (Laparotomy) if needed. The length of bowel resection is also a matter of discussion. There are cases in the literature where the extreme length of bowel disease does not make wide resection feasible [
40,
43,
44,
45]. Most surgeons resect only the complicated diverticular disease and leave the uncomplicated diverticula behind. Based on summarized publications, we create an algorithm in order to manage jejunum diverticulum (
Figure 6).
According to our algorithm, in the first case, the patient was hemodynamically stable but had comorbidities (ASA3). CT scan revealed free abdominal air caused by perforation of one of two jejunal diverticula. The decision was made to perform surgery on the patient without delay. An exploratory laparoscopy was our first choice, while laparoscopic lavage is seen as an acceptable and safe alternative in selected patients [
45]. The patient has no previous abdominal operations and no neglected fasciitis. We recognized the phlegmon and the two complicated diverticula at about 10cm from each other. An enterectomy was made with primary anastomosis. The specimen was about 15cm long, so there was no risk of intestinal failure and small bowel syndrome disease (SBS).
In the second case of accidental detection, we decided on an annual monitoring protocol with clinical examination and CT abdomen.
Conclusion
Small bowel non-meckelian (SBNMD) diverticulosis remains a challenging clinical entity, and the surgeon should have a high index of suspicion. While surgical intervention has been the traditional treatment approach, further advancement in diagnostic tools may offer less invasive and potentially more effective options. Strong evidence-based guidelines are needed to guide clinicians in the diagnosis, management and follow-up of patients with SBNMD. Improving our understanding of this rare condition will lead to better outcomes and quality of life for our patients.
Author Contributions
P.B. was responsible for designing and supervising the study, collecting the data, and writing the manuscript. P.B., N.K., T.C., A.G., and V.P. contributed to writing the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted by the Declaration of Helsinki. Ethical review and approval were waived for this study due to the study’s retrospective design.
Informed Consent Statement
All patients are required to sign a consent form and be provided with complete information regarding their medical condition, including the proposed treatments, potential risks, and benefits.
Data availability statement: Datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13(15):2240-2. PMID: 17465510; PMCID: PMC4146853. [CrossRef]
- Zafouri EB, Ben Ismail I, Sghaier M, Rebii S, Zoghlami A. Jejunal diverticulitis: A new case report and a review of the literature. Int J Surg Case Rep. 2022;97(10):73-95.
- H. Harbi, N. Kardoun, S. Fendri, Dammak N, Toumi N, Guirat A, Mzali R. Jejunal diverticulitis. Review and treatment algorithm, Presse Med. 2017;46: 1139-1143.
- Alam S, Rana A, Pervez R. Jejunal diverticulitis: imaging to management. Ann Saudi Med. 2014;34(1):87-90.
- Lebert P, Ernst O, Zins M. Acquired diverticular disease of the jejunum and ileum: imaging features and pitfalls. Abdom Radiol (NY). 2019;44(5):1734-1743.
- Khsiba A, Bradai S, Mahmoudi M, Mohamed AB, Bradai J, Bouzaidi K, Mona M, Hamzaoui L, Azouz MM. Jejunal diverticulitis as a rare cause of abdominal pain: a case report. Pan African Medical Journal. 2022;41:222.
- 7. Ben Ismail, I, Ben Chaabene, H, Rebii, S, Zoghlami, A. Perforated Jejunal Diverticulitis: a rare cause of acute abdominal pain. Clin Case Rep. 2021;9:e04594.
- Saviano A, Brigida M, Petruzzielo C, Zanza C, Candelli M, Loprete MRM, Salem F, Ojjeti V. Intestinal damage, inflammation and microbiota alteration during COVID-19 infection. Biomedicines. 2023;11(4):1014.
- Delgado-Gonzalez P, Gonzalles-Villareal CA, Roacho-Perez JA, Quiros-Reyes AG, Islas JF, Delgado-Gallegos JL, Arellanos-Soto D, Galan-Huerta KA, Garza-Trevino EN. Inflammatory effect on the gastrointestinal system associated with COVID-19. World J of Gastroenterol. 2021;27(26):4160-4171.
- Aispuro, I.O. and N.P. Yazzie. Diverticulitis of isolated jejunal diverticulum complicated by small bowel obstruction secondary to de novo enterolith formation. J Surg Case Rep. 2019;5:151.
- Aiyegbeni B, Jonnalagadda S, Teibe A. Rare Cause of Left Upper Abdominal Pain. Prague Med Rep. 2021;122(2):106-111.
- Almalki MA, Yaseen WY, Baatiyyah M. Small bowel diverticulum complicated by enterocutaneous fistula and abdominal wall abscess - Case report. Int J Surg Case Rep. 2019;57: 39-41.
- Anjum R, Kumar N, Singla T, Mani R, Karki B. A Case of Isolated Jejunal Diverticulum Presented as Free Perforation: A Rare Cause of Acute Abdomen. Cureus. 2021;13(10): 18809.
- Chung D. Jejunal diverticulosis - A case series and literature review. Ann Med Surg (Lond). 2022;75:103477).
- Coelen RJS, de Brauw LM. Complicated small intestine diverticulitis. Ned Tijdschr Geneeskd. 2019;163:D3317.
- De Simone B, Alberici L, Ansaloni L, Sartelli M, Coccolini F, Catena F. Not all diverticulitis are colonic: small bowel diverticulitis - A systematic review. Minerva Chir. 2019;74(2):137-145.
- Di Dier K, Van Meerbeeck S. Ileal Diverticulitis. J Belg Soc Radiol. 2023; 107(1): 12.
- Duggan WP, Ravi A, Chaoudhry MA, Ofori-Kuma F, Ivanowski I. Isolated perforated jejunal diverticulitis: a case report. Journal of Surgical Case Reports. 2021;1:rjaa587.
- Elfanagely Y, Tse CS, Patil P, Lueckel S. Jejunal Diverticulosis Complicated by Diverticulitis and Small Bowel Obstruction. Cureus. 2020;12(5):e8347.
- Ghrissi R, Harbi H, Elghali MA, Belhajkhlifa MH, Letaief MR. Jejunal diverticulosis: a rare case of intestinal obstruction. J Surg Case Rep, 2016;2:rjv176.
- Giuffrida M, Perrone G, Di Saverio S, Annicchiarico A, Pattonieri V, Bonati E, Tarasconi A, Catena F. Jejunal diverticulitis: Things to know to prevent diagnostic mistake. Acta Biomed. 2021;92(1): 154.
- Glaser J, Farrel MS, Caplan R, Rubino M. Operative rates in acute diverticulitis with concurrent small bowel obstruction. Trauma Surg Acute Care Open. 2022;7(1): e000925.
- Hardon, SF, den Boer FC, Aallali T, Fransen GA, Muller S. Perforated jejunal diverticula in a young woman: A case report. International Journal of Surgery Case Reports. 2021;81: 105838.
- Imasato N, Kijima T, Takada-Owada A, Fujita J, Takei K, Suzuki I, Nishihara D, Nakamura T, Ishida K, Kamai T. Abdominal wall abscess resembling urachal carcinoma caused by ileal diverticulitis. IJU Case Reports. 2023;6(1): 73-76.
- Karna R, Rana T, Mohy-Ud-Din N, Chaoudhary D, Appasamy R. Acute hypotensive hematochezia due to jejunal diverticular bleed. Proc (Bayl Univ Med Cent). 2022;35(6): 854-855.
- Kasuga S, Abe S, Nozawa H, Sasaki K, Murono K, Emoto S, Matzuzaki S, Yokohama Y, Nagai Y, Yoshioka Y, Shinagawa T, Sonoda H, Ushiku T, Ishihara S. Diverticular perforation of terminal ileum associated with chemotherapy for non-small cell lung carcinoma: a case report. J Surg Case Rep. 2023;(4): rjad179.
- Kunishi Y, Kurakami Y, Yoshie K, Yanagibashi T, Oishi R, Tsukamoto M, Niwa K, Kato Y, Ota M, Maeda S. [Non-surgical management of small bowel diverticulitis with localized perforation:a case report]. Nihon Shokakibyo Gakkai Zasshi. 2020;117(4): 327-333.
- Leigh N, Sullivan BJ, Anteby R, Talbert S. Perforated jejunal diverticulitis: a rare but important differential in the acute abdomen. Surg Case Rep. 2020;6(1): 162.
- Lutaya I, Logvinsky I, Mefford M, Nway N, Qureshi A. Jejunal-Ileal Diverticulosis Induced Witzel Tube Failure: A Rare Cause of Small Bowel Obstruction. Cureus. 2022;14(4): e24209.
- Mansour M, Abboud Y, Bilal R, Seilin N, Alsuliman T, Mohamed FK. Small bowel diverticula in elderly patients: a case report and review article. BMC Surg. 2022;22(1):101.
- Matli VVK, Chandrasekar VT, Campbell JL, Karanam C, Jaganmohan S. Jejunal Diverticulitis: A Rare Diverticular Disease of the Bowel. Cureus. 2022; 14(1): e21386.
- Mendo R, Figueiredo P, Saldanha G. Isolated diverticulitis of the terminal ileum: an unusual cause of abdominal pain. BMJ Case Rep. 2021;14(4).
- Pajtak R, Ramadan P, Strauss P. Strangulated diverticulum: a new acute complication of small bowel diverticulosis. J Surg Case Rep. 2023;(5): rjad253.
- Ponce Beti MS, Palacios Huatako RM, Picco S, Capra AE, Perussia DG, Suizer AM. Complicated jejunal diverticulosis with intestinal perforation and obstruction: delay in hospital visit during confinement due to COVID-19. J Surg Case Rep. 2022;2): rjac010.
- Prough H, Jaffe S, Jones B. Jejunal diverticulitis. J Surg Case Rep. 2019;(1): rjz005.
- Rajaguru K, Sheong SC. Case report on a rare cause of small bowel perforation perforated ileal diverticulum. Int J Surg Case Rep. 2021;87:106465.
- Ramzee AF, Khalaf MH, Ahmed K, Latif E, Aribi N, Bouchiba N, Singh R, Zarour A. Small Intestinal Diverticulosis: A Rare Cause of Intestinal Perforation Revisited. Case Rep Surg. 2020;2020:8891521.
- Romera-Barba E, Galvez Pastor S, Navvaro Garcia MI, Torregrosa Perez NM, Sanchez Perez A, Vazques Rojas JL. Jejunal diverticulosis: A rare cause of intestinal obstruction. Gastroenterología y Hepatología (English Edition). 2017; 40(6): 399-401.
- Sammartino F, Selvaggio I, Montalto GM, Pasesinic C, Dhimolea S, Krizzuk D. Acute Abdomen in a 91-Year-Old Male due to Perforated Jejunal Diverticulitis. Case Rep Gastroenterol, 2020;14(3):598-603.
- Sarıtaş AG, Topal U, Eray CI, Dalci K, Akcami AT, Erdogan K. Jejunal diverticulosis complicated with perforation: A rare acute abdomen etiology. Int J Surg Case Rep. 2019;63:101-103.
- Vayzband V, Ashraf H, Esparragoza P. Surgically Managed Perforated Jejunal Diverticulitis. Cureus. 2021;13(6): e15930.
- Walter FA, Rimkus G. Complicated Diverticulitis With Associated Small Bowel Obstruction: A Case Report. Cureus. 2022;14(9): e28942.
- Watanabe Y, Murata M, Hirota M, Suzuki R. Whole jejunoileal diverticulosis with recurrent inflammation and perforation: A case report. Int J Surg Case Rep. 2021;84:106020.
- Agresta F, Ciardo LF, Mazzarolo G, Michelet I, Orsi G, Trentin G, Bedin N. Peritonitis: laparoscopic approach. World J Emerg Surg. 2006;1:9.
- Sijberden J, Snijders H, Van Alteen S. Laparoscopic lavage in complicated diverticulitis with colonic perforation, Always be closing? Case Rep Gastroenterol. 2021;15(2):765-771.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).