1. Introduction
According to the Turkish Ministry of Health (MoH), the first COVID-19 case was identified on March 10, 2020, and the first death due to COVID-19 occurred on March 15, 2020 [
1,
2]. The first diagnosis and the first death that immediately followed caused a shock effect in the public and society in Türkiye, as in all countries. This situation was actually not surprising, but it was not clear when it would occur. It set in motion a process in which the authorities immediately took many measures, especially in the field of health management and public health. This was to be expected, as Türkiye is located at major international transit points. Although various facilities to detect the disease were installed at the airports, the disease spread throughout the country in a very short time. Only two months after the first case, on May 11, 2020, the MoH stated that COVID-19 cases had reached 139,771, with 3841 deaths [
3].
Although different waves of pandemics are defined all over the world, it cannot be said that this distinction is clearly made in Türkiye. Being one of the centres of international human mobility, it was possible that all variants of the pandemic occur in different regions of the country [
4]. The MoH did not disclose the number of COVID-19 cases and deaths since November 27, 2022. In this context, the latest figures were reported as 17,042,722 cases and 101,492 deaths due to COVID-19 in Türkiye [
3].
At the beginning of the emergence of COVID-19 as a public health problem, the MoH formed an expert board. “The Coronavirus Scientific Advisory Board - CSAB” was a group of scientists (including experts from pulmonology, infectious diseases, clinical microbiology, and legal advisers,
etc.) set up by the MoH to develop measures in the fight against COVID-19 that are imposed by the government [
5]. The board surprisingly, was set up on January 10, 2020; before the World Health Organization (WHO) confirmed it mid-March as a pandemic. This board served as a high-level advisory body in all government decisions related to the process. Türkiye has taken a number of public health measures, some of which are slightly different from those in the rest of the world (especially in Europe). First, Türkiye has taken a number of measures, including closing cafes and bars, cancelling events and meetings, and restricting flights. Then, the CSAB stated that public health interventions -such as lockdowns, filiation and mask use- had led to major drops in caseloads, reducing the strain on emergency rooms and intensive-care units [
6]. This process continued with lockdowns, sometimes on weekends and sometimes on weekdays. The COVID-19 vaccination campaign in Türkiye began on 14 January, 2021; and 85,7% of the population is fully vaccinated -two doses- by October 08, 2023 [
7].
Many countries in the world have experienced similar process, responses and challenges in COVID-19 pandemics [
8,
9,
10,
11,
12]. This study aims to examine Türkiye’s response to the COVID-19 pandemic, focusing on Health Emergency and Disaster Risk Management (Health-EDRM), especially human resources, health services, and public-social-technical logistics.
2. Materials and Methods
This is a grey literature review of publicly available information focused on the Türkiye’s COVID-19 pandemic response.
2.1. Methods Setting
According to the key questions, literature in Türkiye was hand-searched with terms such as “COVID-19”, “human resources”, “health service delivery”, “COVID-19 public health”, “pandemic management” and “pandemics response” using the Google search engine, DergiPark, Web of Science, literature from government and private sector, official documents, reports, and academic papers from PubMed. Various documents; such as health-related guidelines by the MoH and official guidelines from the government, academic articles by the researchers, documents from public institutions and academic societies, and news articles from December 2019 to October 2023, were investigated by document analysis and reviewed.
2.2. Literature Resources
In Türkiye, responses to COVID-19 were mainly dependent on governmental policy, so it is mainly focused on government materials. The latest official government documents from Türkiye until October 2023 were included for document analysis. The governmental documents were mostly by the MoH, but also the Ministry of Foreign Affairs, the Ministry of National Education, the Ministry of Labour and Social Security, the Ministry of the Interior, the President, etc. The main conflict concerned the frequently changing situation of the COVID-19 pandemic, which made it somewhat difficult to follow the articles and documents on COVID-19 responses.
3. Results
The results are divided into three sections, each focusing on Health-EDRM; human resources, health service delivery, and logistics. Each section is subdivided into the relevant major sub-themes, and a summary of the findings is presented in
Table 1 below. This section explains the issues related to the Health-EDRM, and discusses each issue, including responses, challenges, and opportunities for the COVID-19 pandemic.
3.1. Human Resources
3.1.1. Medical Staff
At the beginning of the outbreak of COVID-19 in Türkiye, the idea that this issue was specifically a matter for infectious disease experts was at the forefront. However, it was immediately realized that the coming problem was not that simple and that it was faced with a multidimensional situation that concerns all areas of health [
13]. In particular, the emergency departments where patients first applied were the units that played an active role in the diagnosis of COVID-19 patients in Türkiye. One of the biggest advantages of this process is that Turkish people have a unique (and also a problematic) use of emergency services. Emergency departments have an important role in the hospital-based healthcare system in the country. Although there are many reasons, overcrowding in emergency departments is a serious problem [
14,
15,
16]. However, this extraordinary situation means that the emergency department structure and emergency department personnel are used to overcrowding; thus, the increase in the number of patients in emergency departments during the pandemic did not affect the treatment/process so much [
17].
Second, management of the pandemic is not only related to physicians, but also nurses, prehospital emergency teams, intensive care personnel, hospital cleaning/hygiene staff, social workers, filiation staff, family physicians, and administrative officials,
etc. So, it is a complex system that requires many human resources. From this perspective, it appears that healthcare personnel resources and distribution are sufficient in Türkiye [
18]. However, the challenge in this regard is that the density of COVID-19 patients increases from time to time in metropolitan cities and it is difficult to immediately mobilize the medical staff to meet the unexpected increase in certain centres. Because of the potential need for medical personnel during the crisis, the government has also mobilized some healthcare staff, and many routine medical practices in hospitals have been regulated such as diagnostic procedures, postponed such as elective surgical, and some restricted such as outpatient consultation [
19].
Third, as of February 28, 2022, 506 healthcare workers in Türkiye, including physicians, nurses, and other healthcare workers, have died as a result of COVID-19 infection, according to the Turkish Medical Association [
20]. This number indicates a problem that needs to be considered with regard to human resources in healthcare. However, there are sometimes numerical discrepancies between the MoH and the Turkish Medical Association in the statistical data released about healthcare workers who were infected and died during the pandemic. The difference in numbers sometimes leads to a conflict about the reliability of the data.
Fourth, the other challenge faced by medical staff was anxiety and stress due to the high risk of infection when providing healthcare to the patients [
21,
22,
23]. Ayaslier et al. found that physicians and nurses are affected by burnout in different ways under the conditions of the COVID-19 pandemic based on gender, socioeconomic status and working conditions [
24]. The high workload and stress affected both healthcare workers’ relationships with their families and their physiological state [
25,
26]. Although the government has taken some measures, such as additional financial payments, to overcome the trouble of medical staff, it could have taken more functional measures to address, in particular, the psychological impact of the pandemic on healthcare workers [
27,
28].
3.1.2. Education and Preparation of Medical Staff
Since the first outbreak of COVID-19, WHO recommended the development of country-specific operational plans for COVID-19 preparedness and response, or an adaptation of the existing Influenza Pandemic Preparedness Plan [
29]. The Pandemic Influenza National Pandemic Preparedness Plan by MoH was updated in 2016 in Türkiye just before the COVID-19 pandemic [
30]. Of course, COVID-19 is not caused by the influenza virus, but the main framework of influenza preparedness is also the main framework of the COVID-19 pandemic response. It was an important opportunity to provide a strong response to the current pandemic [
31].
The government dispatched physicians to pandemic epicentres, screening centres, airport quarantines, hospitals, and intensive care units. In this context, on-the-job training was planned and implemented on-line or/and face-to-face, as soon as possible. Medical education curricula and programmes have been modified in response to the pandemic, and students in many medical schools have received training on prevention, treatment and vaccination [
32,
33,
34]. When general lockdowns began across the country, health workers were undoubtedly affected [
35]. In this regard, the MoH offered various accommodation options to doctors/nurses treating COVID-19 patients in hospitals.
The impact of these initial responses by the public authorities to the pandemic has diminished over time, and their scope has changed or their effectiveness has diminished. Medical education in medical schools has occasionally been disrupted, sometimes leading to severe criticism from doctors [
36]. Although not directly involved in pandemic-related health services, junior doctors (internship) were encouraged to participate in other ongoing health services. This approach was based on the view that it was a good opportunity for young doctors to learn the profession “in the field”. The risks and benefits of this approach may not have been adequately discussed in the community.
3.1.3. Supports to Medical Staff
Although there were short-term problems with issues such as the supply of masks and protective equipment in the early months of the pandemic in Türkiye, in general there were no serious problems with access to equipment to protect healthcare workers from infection [
37,
38]. The country seems to have strong infrastructure support in that respect. In particular, the provision of N95 masks to healthcare workers directly treating COVID-19 patients has been very successful.
Second, healthcare workers were given priority for COVID-19 vaccination in Türkiye. This was an effective government policy, given the high risk of contamination and the priority access to the vaccine for healthcare workers who were actively involved in the treatment process [
39,
40]. The priority vaccination of healthcare workers and the effective maintenance of this practice also provided a successful perception for managing public attitudes towards COVID-19 vaccination.
Third, from the outset, the MoH and other health authorities in Türkiye, in consultation with global health authorities, have produced Turkish guidelines for health professionals [
41,
42]. These have been updated from time to time [
43]. These guidelines provided essential guidance to healthcare professionals so that similar methods of COVID-19 prevention and treatment could be implemented throughout the country. In this way, any doubts that might arise with regard to the treatments used have been minimised.
Fourth, humanity’s solidarity reflex in the face of disaster was also evident in Türkiye during the pandemic. Additional government-level budget and allowances were paid to COVID-19 medical staff who are actively involved in the fight against COVID-19. In addition to the central government additional payments to healthcare professionals; local governments and initiatives also took various initiatives to express gratitude to healthcare workers. On social media, television and billboards, many advertisements and thank-you messages were shared. (
Figure 1).
3.2. Health Service Delivery
3.2.1. Hospitals and Intensive Care Units
According to MoH statistics, the number of hospital beds in Türkiye in 2020 will be 251,182 and the number of intensive care unit (ICU) beds will be 47,700. It means, Türkiye has large number of beds with 30 beds per ten thousand people, and 39.1 ICU beds per a hundred thousand people in 2020 [
44]. However, in the case of COVID-19 patients, it was difficult to secure hospital beds because of the need for a specialised bed, such as a negative pressure room.
As COVID-19 is a specialised treatment, ICU bed capacity is critical for all countries. Understandably, these costly structures were not widely included in pre-pandemic planning. The problem of insufficient beds across the country has been addressed by centralising bed monitoring, bed allocation and triage systems through a dispatch centre. In particular, the triage of ICU beds, which raises ethical conflicts, has sometimes become a serious issue.
Patients with mild symptoms were placed in self-quarantine, with medical staff monitoring them once/twice a day. In addition to the use of masks and attention to social distance, the use of some oral medications was standard practice for these patients [
45]. The 112 emergency dispatch centres in Türkiye also played an active role in the co-ordination of patients, hospitals and intensive care beds where there was a shortage of beds, as well as ambulance transport and patient allocation. It has become clear that the fight against the pandemic is not a process that can be carried out by qualified hospitals alone, but that more complex mechanisms are required.
The main lessons learned were the importance of structural changes in hospitals and health facilities, the importance of designing hospitals with adequate space for triage and single rooms for isolation, and the importance of dirty/clean pathways [
9].
3.2.3. Vaccination
For COVID-19 vaccination in Türkiye, healthcare workers and residents of long-term care facilities were prioritised, followed by high-risk individuals, other essential workers and the general public [
46]. As of October 2023, over 85% of the Turkish population has received at least two doses [
7]. Despite the fact that there is a serious issue of vaccine hesitancy in the country, achieving such a high vaccination rate can be considered an achievement. This success was due to the fact that the Minister of Health and other government officials were vaccinated on television at the start of the campaign, and positive propaganda about the vaccine was spread across all media platforms. As in many countries, reasons for hesitancy include concerns about side effects and vaccine safety, lack of trust in institutions, and the belief that vaccination against COVID-19 is unnecessary [
47,
48,
49].
Initially, only Sinovac was used, but various vaccines, notably Pfizer-BioNTech and the nationally produced Turkovac, were also used. There have mostly been no problems with the supply of international vaccines to the country. However, it is noteworthy that the issue of producing national vaccines has been advanced in a propagandistic discourse, including in Turkish politics [
50].
3.3. Logistics
3.3.1. Public Logistics
The government has offered various forms of support such as subsidies, tax breaks and economic incentives to some sectors affected by the pandemic [
51,
52,
53]. Many companies have experienced disruptions in their supply chains due to factory closures, and reduced capacity [
54]. For this reason, various alternatives have been tried, such as flexible working models, working remotely and distance learning in educational institutions.
The COVID-19 pandemic was the first time that formal education was disrupted globally. Children in both developed and developing countries are unable to go to school. The development of the Internet and network technology has enabled learners to study regardless of their location. Online learning has therefore been proposed as a plausible and effective alternative to face-to-face learning.
Although the Ministry of National Education closed elementary-middle, and high schools for a while, it quickly introduced the distance learning system “eba” (
Figure 2) [
55]. For a long time, students continued their education through this system, both on television and the Internet, and through various applications of their local schools. Issues such as the provision of both general and higher education through distance learning, and the efficiency and content of this education, have led to serious discussions in the country [
56,
57,
58,
59].
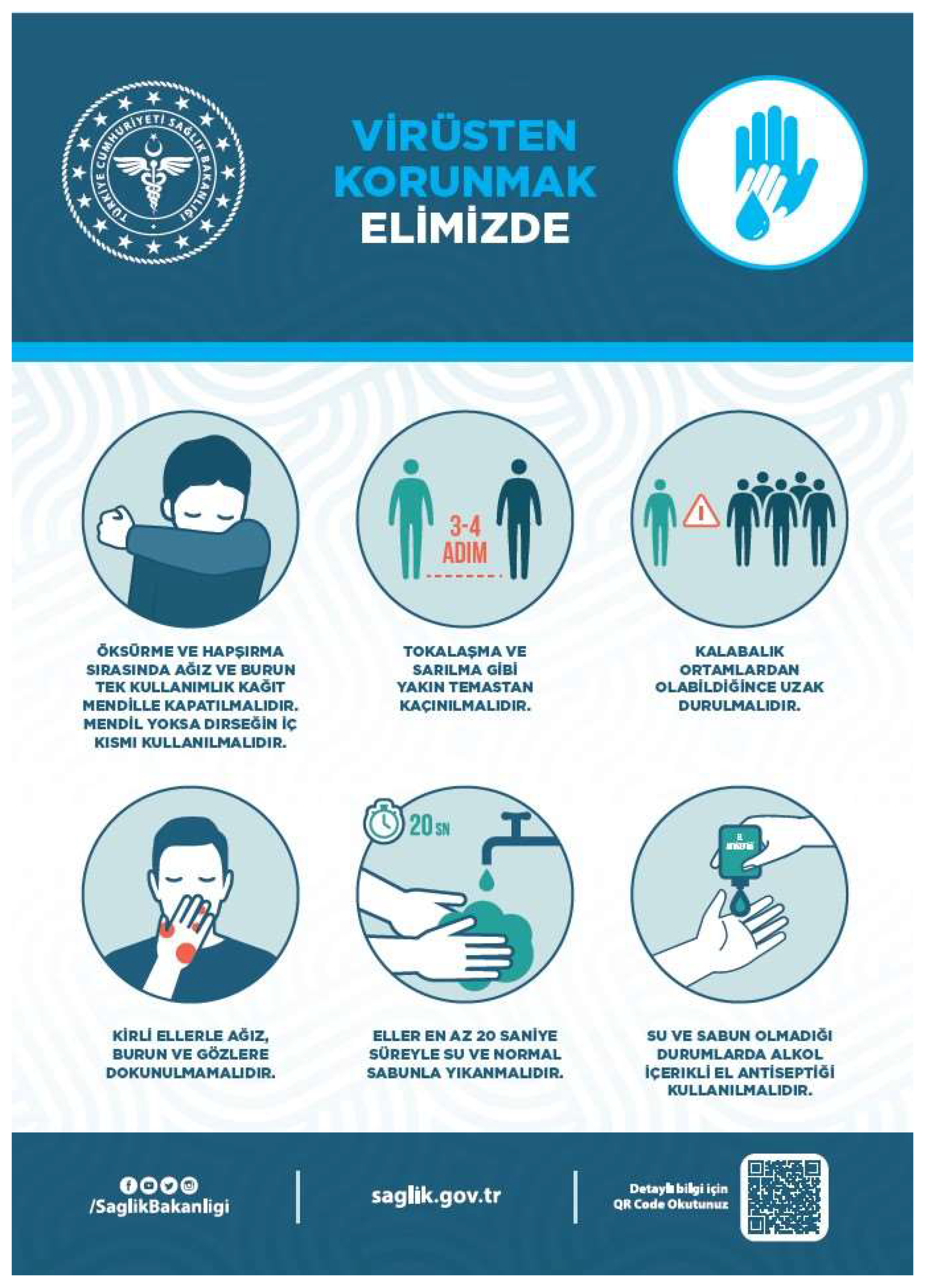
As personal protection, social distancing and hand washing are important in preventing the spread of the disease, the MoH has produced many warning and informative publications, documents and announcements on these issues (
Figure 3).
3.3.2. Social Logistics
Immediately after the pandemic began, the government launched a campaign to provide free masks to all citizens [
60]. However, this practice, which was an important public logistics/support in the beginning, was not successfully continued. Local authorities’ efforts to support food shopping and solidarity with the elderly and vulnerable citizens have not been successful enough. Various psychological and social support and rehabilitation activities were carried out, especially for the elderly who were expected to be affected by the closure [
61,
62].
Surprisingly, artistic and literary activities and productions took on a unique form during the pandemic. Popular singers gave online concerts via social media and famous authors held book readings (
Figure 4). Such activities were efforts to increase the sense of solidarity in society and were thought to partially reduce the effects of social isolation.
In the midst of the pandemic, interest in issues related to narrative medicine increased in Türkiye. As if to support the views that emphasise the healing function of narrative medicine, many books were published during the COVID-19 pandemic, written by both doctors and individuals, describing the experiences [
63,
64]. Some initiatives organised storytelling competitions open to everyone to share their COVID-19 experiences, keep the narrative tradition alive and support the healing aspects of storytelling [
65].
Another unexpected and surprising piece of logistics came from religious institutions in Türkiye. The President of Religious Affairs called for prayers from the minarets of all mosques across the country after the night adhan for a quick end to the COVID-19 pandemic and for patients to be cured safely [
66]. This practice of collective prayer, which spread from loudspeakers to the streets, was for a time a symbolic and unique approach to social logistics, although it was discontinued after a short time.
3.3.3. Technical Logistics
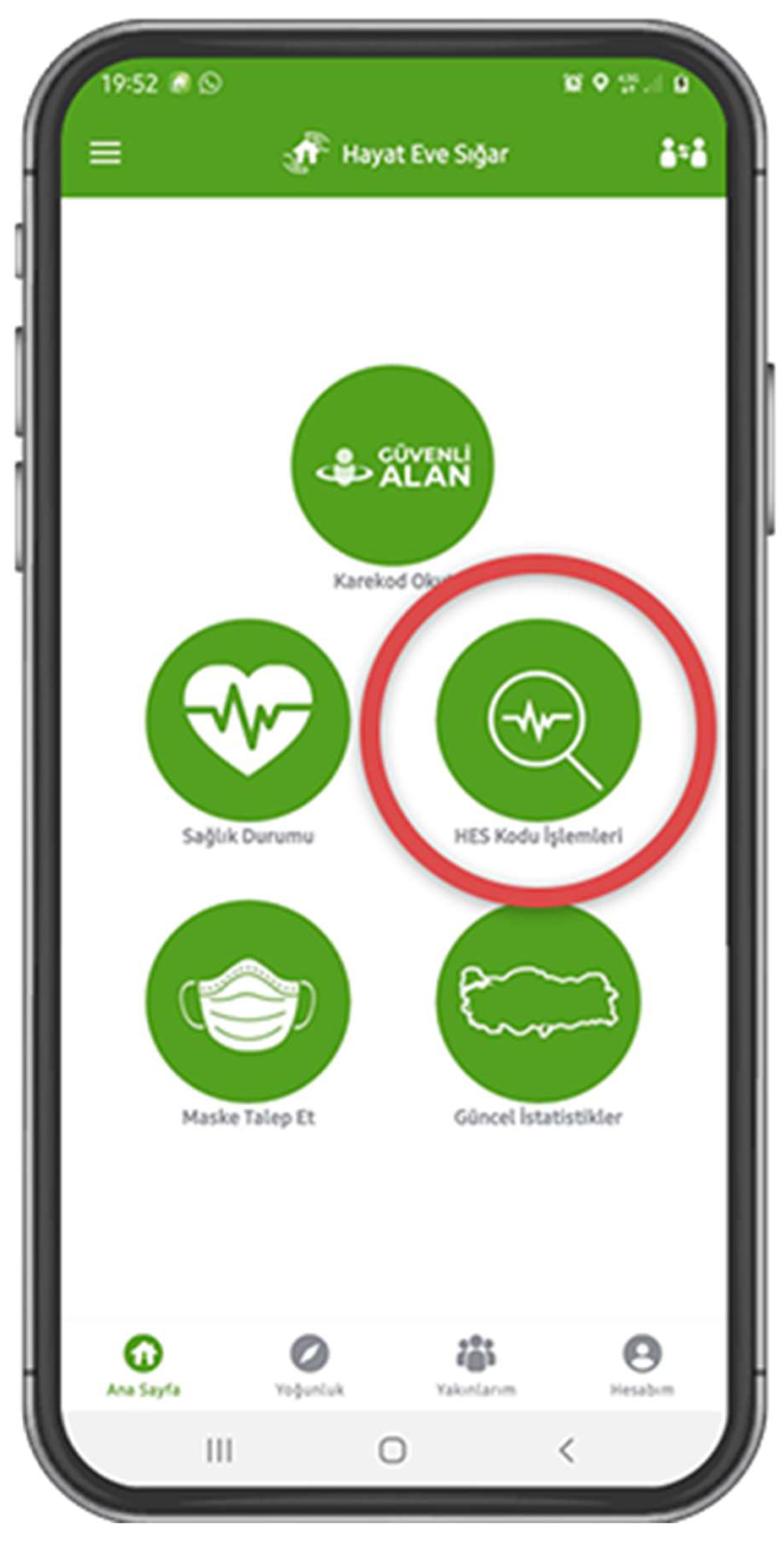
The pandemic has highlighted the importance of digital health records and digital data. A powerful dataset, both individual and social, has been created with the contribution of internet-based information technologies. Among these technologies, the most notable programme in Türkiye was the mobile application “Life Fits Home (HES)” by the MoH, which was made available to individuals (
Figure 5).
“Life Fits Home (HES)” is a mobile application developed by the MoH to inform and guide citizens living within the country’s borders about COVID-19 and to minimise the risks associated with the epidemic disease and prevent its spread. The application is offered by the MoH to citizens who can verify with a phone number, answer the questions asked step by step, and get guidance on how to act by being evaluated according to the complaints in terms of coronavirus disease. This application, which also keeps personal health records related to COVID-19, also generates a code that citizens are asked to use during some of their travels and when entering some institutions, shopping centres, etc.
4. Discussion
4.1. Ethics
A wide range of ethical conflicts have arisen throughout the world during the pandemic, involving physicians, nurses, administrators and others. These (and undoubtedly other) issues can be identified under the following headings: mandating vaccination; triage, including ICU triage; justice; placebo-controlled trials of COVID-19 vaccines; clinical trials; health management, including honesty, trust, accountability and transparency; balancing the interests of patients and the entire community in relation to stay-at-home orders and social distancing requirements; risks and anxiety level of healthcare workers related to heavy workloads, stress, risk of contracting infectious diseases, and so on [
67,
68,
69,
70,
71,
72,
73,
74].
The COVID-19 pandemic is pushing ethical reflection in new directions, and many of these. During health crises, the need for ethical standards and accountability becomes imperative [
75]. Healthcare providers, governments worldwide and policy makers have a responsibility, a duty of care, to protect public health and it is ethically justified to focus on “the common good”. The pandemic requires difficult but unavoidable political and social decisions of ethical importance and complexity with interconnection of sectors [
9].
Ongoing ethical debates have become more visible with the COVID-19 pandemic, and even new issues (such as curfews) have been added to these debates, and public health ethics have become a special issue, involving societies beyond bioethicists and inevitably challenging decision-makers. The challenge is that decisions on ethical issues have to be made in a short time and it is almost impossible to reach a consensus. Türkiye, along with the rest of the world, is experiencing similar conflicts and discussions with regard to the pandemic and ethical issues.
With regard to the Health EDRM, the ethical lessons learned during the COVID-19 pandemic in Türkiye are the importance of core values such as transparency, accountability and trust; the difficulties in implementing equality and related concepts; the need for policy decisions to be guided by ethical values and with broad participation of society. The CSAB scientific committee was a very valuable step in this regard in Türkiye, but it was always questionable whether the committee included enough experts on the ethical and sociological dimensions of the pandemic. This process is noteworthy in that it can ensure that the same reflex is shown in similar crises in the future, and is probably holds promise for the activation of more comprehensive central decision-making mechanisms in possible future disasters.
4.2. Vulnerability
It is well known that in some public health crises, vulnerable populations, due to their age, disability, gender, income level,
etc., are much more exposed to adverse health effects than the general population. Considering vulnerability only in terms of health is definitely not enough; it should be applied by taking into account the socio-economic and cultural structures of these people. Vulnerability should therefore be considered in different dimensions, such as health vulnerability (chronically ill or disabled people), social vulnerability (having disadvantages in the distribution of social services), economic vulnerability (low income or dependent people) and institutional vulnerability (such as prisoners) [
76] .
Actually, when major global shocks occurred during the COVID-19 pandemic, people generally tended to become more vulnerable [
77]. Increasingly, the conditions of social, economic and political hardship have a strong impact on individual’s health, increasing physical vulnerability and thus the likelihood of disease [
78]. The COVID-19 pandemic disproportionately affected certain populations and created conditions that either created new forms of vulnerability or exacerbated existing ones. Strict quarantine measures placed vulnerable groups in a more precarious position, increasing risks and threats to their well-being [
79]. In the COVID-19 pandemic, as stated above, vulnerable groups include not only the elderly, those with ill health and co-morbidities, or those who are homeless or unhoused, but also people from a range of socio-economic groups who may find it difficult to cope with the crisis financially, mentally or physically [
80]. Similarly, due to restrictions and the need for distance learning, children and health workers are also included in these groups as they are at risk of illness/death and have lost many of their colleagues.
First, the inequalities experienced by children during the distance learning period were one of the most important issues during the COVID-19 pandemic in Türkiye, which were not sufficiently put on the government agenda, but in terms of the risk of fragility. Particularly during the distance learning period, the main issue of vulnerability was children who did not have the same equipment as other children in the classroom. It seems that the government has not made enough efforts in this regard. It was expected that the Ministry of National Education would put this inequality on the agenda, as it was busy implementing and developing the distance learning model [
81].
Second, the elderly population was at a significantly higher risk of the severe COVID-19 outcomes and had the greatest risk of mortality. The older people were facing the most threats and challenges during the pandemic [
82]. The elderly were affected by several measures have been taken, including social distancing, encouraging people to stay at home, cancelling mass gatherings,
etc [
83]. All these restrictions, plus the fear/possibility of contracting the disease, have made the elderly in Türkiye vulnerable. Some polices and social packages have been developed by the government for older people in Türkiye [
61,
84,
85]. However, the adequacy of these supports appears to be controversial and mostly palliative and temporary during the pandemic.
Third, COVID-19 patients face serious risks of vulnerability, including stigmatisation, from the beginning of the disease process, during and after treatment by healthcare systems and society [
86,
87]. Similarly, the greatest risk of death in COVID-19, highlighting vulnerability, was among the patients with chronic diseases and healthcare workers. The level of anxiety experienced by healthcare workers during the pandemic was the most important factor in their vulnerability in Türkiye [
88]. Due to the high number of COVID-19 patients and long shifts, physicians and nurses were experiencing anxiety, depression and poor mental health [
89,
90,
91]. During the COVID-19 period in Türkiye, studies have shown an increase in anxiety, especially among nurses [
92,
93].
In terms of the health EDRM, the lessons learned about vulnerability during the COVID-19 pandemic in Türkiye are awareness, supporting stress management skills, the importance of economic and social support, and solidarity. Although some of the measures taken by the government made a serious contribution, vaccination and support for vulnerable groups in particular could have been made more transparent and at a level that would have satisfied the public. The pandemic period was a serious experience for the government and decision-makers. It is hoped that this experience will improve preparedness for future crises.
4.3. Sustainability
As the COVID-19 pandemic caused involuntary and/or voluntary changes around the world, many governments and authorities, such as WHO, adopted specific plans and strategies. Various psychological and social support and rehabilitation mechanisms/activities were implemented, especially for the elderly, children and vulnerable groups affected by the outbreak [
94]. In addition to practices in the health sector, changes have also taken place in areas as diverse as education, the economy, working life, the environment, social life, and risk management [
86].
During this critical period, various practices were implemented in Türkiye, mostly by the public authorities. Community support was one of the most important elements in sustaining these practices. It was probably considered normal that some decisions were made quickly and instructions were implemented immediately due to the conditions of the pandemic period. However, participation in decision-making processes, the right to appeal and the transparent review of the results of applications are now considered fundamental values of modern societies. These core values are also necessary for the sustainability of these practices, particularly on the environmental sustainability. Since the increase in the consumption of disposable materials and masks in the COVID-19 pandemic has caused the problem of pollution in the environment [
95]. Looking at the Turkish example, it can be said that there are aspects that can be improved in terms of community participation in decision-making.
Crisis preparedness of hospitals, intensive care units and the health system in general; support for technical infrastructure and facilities, as well as the number and training of health workers; is one of the most important achievements and areas of sustainable development in the COVID-19, in Türkiye. This valuable experience and preparedness made a positive contribution to the response to the 6 February earthquake, which occurred immediately after the pandemic and was considered the largest disaster in the country’s history.
The basis for sustainability is that people believe in this change and its positive effects, i.e. they understand the importance of changing perceptions. In the example of the COVID-19 pandemic, it can be said that Türkiye has partially achieved this. For example, the distance learning model launched during the pandemic period is continuing with a partial and hybrid model, especially in higher education throughout the country [
96]. The above discussion shows that there is evidence of similar lasting changes in almost all areas where the pandemic is affecting human life in Türkiye [
97].
4.4. Management
As a natural result of the understanding of democracy and sociology in Türkiye, the word “management” mainly means the perceived central government and its duties and responsibilities. Thus, there has been a reflex to approach issues such as disasters, pandemics and risk management from a traditionally centralised perspective. The effects of this approach can be seen in the country during the COVID-19 pandemic. In this semi-structured system, where the main decision-maker is the government and the implementers of decisions are local authorities, some practices, such as curfews, have been easily implemented without much objection from the public. Therefore, the discussion on the Health EDRM in Türkiye has mainly been addressed through this framework.
In this context, issues such as contingency plans and risk management tend to be addressed from a centralised perspective, despite the contributions and efforts of local stakeholders. In the context of health workforce management in COVID-19, strategies at the level of healthcare workers and organisations are important, but system-level coordination is needed to support sustainability [
98]. Thus, from the perspective of the COVID-19 pandemic experience, it can be seen that many contingency plans announced in previous periods contributed significantly to Türkiye’s response to the pandemic. In particular, the contingency plans of the official institutions related to disaster and emergency management indicate a comprehensive preparation [
99] These plans have been detailed, studied and, in some cases, tested against different scenarios, and were an important guide especially for health emergency management during the COVID-19 pandemic. However, it is highly unlikely that almost any country in the world will be prepared for a global, extraordinary and severe pandemic.
In the run-up to the pandemic, various risk management and preparedness plans were drawn up by official, semi-official and NGO institutions, although they were not specific to the pandemic [
100,
101,
102]. During the pandemic, awareness of the issue has increased and a wide range of action/management/risk plans have been put in place [
97,
103,
104,
105]. It is important that all these processes are carried out with ethical sensitivity and that risk plans are developed with the participation and cooperation of their practitioners [
106].
5. Conclusion
In this article, it may be concluded that the COVID-19 pandemic has caused many necessary or unpredictable changes in Türkiye, as in all countries. Therefore, it has imposed heavy responsibilities on both the government, individuals and the society. These responsibilities have raised ethical issues in terms of both public health, vulnerability, management, vaccination and environmental sustainability. On the other hand, it has also had a positive effect in terms of raising public awareness of the issues and creating a sense of social cohesion and collaboration. This positive awareness has been verified in the earthquake that shook eleven provinces on February 6, 2023 in Türkiye. However, there are still significant challenges in ensuring that these ethical issues are addressed around the world and that lessons can be learned to control the COVID-19 pandemic and for the next pandemics.
The COVID-19 pandemic had a devastating impact on the physical and mental health of all those involved, especially the most vulnerable and healthcare workers. This pandemic has been a difficult process for humanity, with the complexities of treatment, vaccination, clinical trials, efforts to limit the spread of the pandemic, economic, social and environmental impacts, and perhaps many other issues that have not yet emerged. Türkiye, with its government and people, has also learnt various lessons from this complex and challenging experience, especially in the context of the Health EDRM. At present, some of these experiences can be successfully sustained and alternative strategies developed, however the others require more effort, awareness and a broader perspective.
Management issues related to the following three topics are the most striking learning points for Türkiye from the COVID-19 pandemic: human resources related to health workers and vulnerability; health service delivery related to hospitals, intensive care units, vaccination and triage; and logistics with public, social and technical dimensions.
Funding
This research received no funding. This study was funded by the World Health Organization Kobe Centre for Health Development (WKC-HEDRM-K21001).
Conflicts of Interest
There is no conflict of interest.
References
- Kisa, S.; Kisa, A. Under-Reporting of COVID-19 Cases in Turkey. Int J Heal. Plann Mgmt 2020, 35, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Aykaç, N.; Yasin, Y. Rethinking the First COVID-19 Death in Turkey. Turk Thorac J 2020, 21, 291–292. [Google Scholar] [CrossRef] [PubMed]
- The Ministry of Health Current Status in Türkiye Available online: https://covid19.saglik.gov.tr/TR-66935/genel-koronavirus-tablosu.html.
- Sirkeci, I.; Murat Yüceşahin, M. Coronavirus and Migration: Analysis of Human Mobility and the Spread of Covid-19. Migr. Lett. 2020, 17, 379–398. [Google Scholar] [CrossRef]
- Yener, D. Türkiye’nin Koronavirüsle Mücadele Politikasına “Bilim Kurulu” Yön Veriyor. Anadolu Agency 2020.
- Cantekin, K. Turkey: Government Takes Extraordinary Administrative Measures for the Coronavirus Pandemic Available online: https://www.loc.gov/item/global-legal-monitor/2020-03-24/turkey-government-takes-extraordinary-administrative-measures-for-the-coronavirus-pandemic/.
- The Ministry of Health COVID-19 Vaccination Information Platform - Last Report; Ankara, 2023.
- Ghotbi, N. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Iran. Sustain. 2022, 14. [Google Scholar] [CrossRef]
- Lamberti-Castronuovo, A.; Parotto, E.; Della Corte, F.; Hubloue, I.; Ragazzoni, L.; Valente, M. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Italy. Front. Public Heal. 2022, 10. [Google Scholar] [CrossRef]
- Chen, A.P.; Hansoti, B.; Hsu, E.B. The COVID-19 Pandemic Response and Its Impact on Post-Pandemic Health Emergency and Disaster Risk Management in the United States. Sustain. 2022, 14. [Google Scholar] [CrossRef]
- Park, J.; Min, J.; Song, J.H.; Park, M.Y.; Yoo, H.; Kwon, O.; Yang, M.; Kim, S.; Lee, J.; Myong, J.P. The COVID-19 Pandemic Response and Its Impact on Post-Corona Health Emergency and Disaster Risk Management in Republic of Korea. Sustain. 2023, 15. [Google Scholar] [CrossRef]
- Ishimaru, T.; Shimizu, S.; Teshima, A.; Ibayashi, K.; Arikado, M.; Tsurugi, Y.; Tateishi, S.; Okawara, M. The Impact of COVID-19 Outbreak on Health Emergency and Disaster in Japan. Sustainability 2022, 14, 15686. [Google Scholar] [CrossRef]
- Demirbilek, Y.; Pehlivantürk, G.; Özgüler, Z.Ö.; Meşe, E.A.L.P. Covid-19 Outbreak Control, Example of Ministry of Health of Turkey. Turkish J. Med. Sci. 2020, 50, 489–494. [Google Scholar] [CrossRef]
- Ülker, V.; Taşkın, H.C.; Yardımcı, N.; Hocagil, A.C.; Hocagil, H. Overcrowding Is Still a Big Problem for Our Emergency Services, Real Disaster Is in Our Emergency Departments in Turkey. Prehosp. Disaster Med. 2017, 32, S32. [Google Scholar] [CrossRef]
- Erenler, A.K.; Akbulut, S.; Guzel, M.; Cetinkaya, H.; Karaca, A.; Turkoz, B.; Baydin, A. Reasons for Overcrowding in the Emergency Department: Experiences and Suggestions of an Education and Research Hospital. Turkish J. Emerg. Med. 2014, 14, 59–63. [Google Scholar] [CrossRef]
- Cakir, O.D.; Cevik, S.E.; Bulut, M.; Guneyses, O.; Aydin, S.A. Emergency Department Overcrowding in Turkey: Reasons, Facts and Solutions. J. Nepal Med. Assoc. 2014, 52. [Google Scholar] [CrossRef]
- Çirakli, Ü.; Orhan, M.; Sayar, B.; Demiray, E.K.D. Impact of COVID-19 on Emergency Service Usage in Turkey: Interrupted Time Series Analysis. Intern. Emerg. Med. 2023, 18, 2105–2112. [Google Scholar] [CrossRef] [PubMed]
- Çınaroğlu, S. Distribution of Health Human Resources in Turkey in Provincial Level and a Need for More Effective Policy. Hacettepe J. Heal. Adm. 2021, 24, 235–254. [Google Scholar]
- The Ministry of Health Elektif İşlemlerin Ertelenmesi ve Diğer Alınacak Tedbirler; The Turkish Ministry of Health, 2020; pp. 1–2.
- Nesanır, N.; Bahadır, A.; Karcıoğlu, Ö.; Korur Fincancı, Ş. Pandemi Sürecinde Türkiye’de Sağlık Çalışanı Ölümlerinin Anlattığı; Ankara, 2022.
- Selçuk, F.Ü.; Solak Grassie, S. Psychosocial Predictors and Mediators Relating to the Preventive Behaviors of Hospital Workers During the COVID-19 Pandemic in Turkey. J. Occup. Environ. Med. 2023, 65, 255–260. [Google Scholar] [CrossRef]
- Kackin, O.; Ciydem, E.; Aci, O.S.; Kutlu, F.Y. Experiences and Psychosocial Problems of Nurses Caring for Patients Diagnosed with COVID-19 in Turkey: A Qualitative Study. Int. J. Soc. Psychiatry 2021, 67, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Şahin, M.K.; Aker, S.; Şahin, G.; Karabekiroğlu, A. Prevalence of Depression, Anxiety, Distress and Insomnia and Related Factors in Healthcare Workers During COVID-19 Pandemic in Turkey. J. Community Health 2020, 45, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Ayaslıer, A.A.; Albayrak, B.; Çelik, E.; Özdemir, Ö.; Özgür, Ö.; Klrlmll, E.; Kayl, İ.; Sakarya, S. Burnout in Primary Healthcare Physicians and Nurses in Turkey during COVID-19 Pandemic. Prim. Heal. Care Res. Dev. 2023, 24. [Google Scholar] [CrossRef] [PubMed]
- Batu, M.; Kalaman, S.; Tos, O.; Subaşı, H. Active Healthcare Professionals’ Perception of COVID-19 and Their Communication with Their Children: A Qualitative Analysis of the Background of the Pandemic. Türkiye İletişim Araştırmaları Derg. 2021, 8, 35–54. [Google Scholar] [CrossRef]
- Özlü, A.; Akdeniz Leblebicier, M.; Ünver, G.; Bulut Özkaya, D. Evaluation of Musculoskeletal Pain and Physical Activity of Health Care Workers Taking Part in the Covid-19 Pandemia. Kocatepe Med. J. 2023, 24, 105–111. [Google Scholar]
- The Ministry of Health Sağlık Bakanlığına Bağlı Sağlık Tesislerinde Görevli Personele Ek Ödeme Yapılmasına Dair Yönetmelik; Türkiye, 2020.
- Arık, Ö.; Aydoğdu, A. Investigation of Opinions of Health Staff About Covid-19 Additional Payment by the Ministry of Health. Int. J. Acad. Value Stud. (Javstudies JAVS) 2021, 3, 231–242. [Google Scholar] [CrossRef]
- World Health Organization (WHO) COVID-19 Strategic Preparedness and Response Plan: Operational Planning Guidelines to Support Country Preparedness and Response.; Geneva, 2020.
- The Ministry of Health Pandemic Influenza National Preparedness Plan; Ankara, 2016.
- Kartoglu, U.; Pala, K. Evaluation of COVID-19 Pandemic Management in Türkiye. Front. Public Heal. 2023, 11. [Google Scholar] [CrossRef]
- Bezircioğlu, I.; Dinç Horasan, G.; Seval-Çelik, Y.; Güner Akdoğan, G.; Hayran, M.; İnan, S.; Şemin, İ.; Dayanç, B.E.; Demir, A.B.; Abacıoğlu, Y.H. COVID-19 Pandemic Effect in Medical Education: “Izmir University of Economics Experience. Tıp Eğitimi Dünyası 2021, 20, 102–108. [Google Scholar] [CrossRef]
- University, S. Selçuk University Faculty of Medicine Activity Report on Medical Education during Pandemic; Konya, 2021.
- Council of Higher Education (YÖK) YÖK’ten Salgın Sürecinde Doktor Adaylarının Mezuniyetlerini Kolaylaştıracak Yeni Karar; Ankara, 2020.
- The Ministry of the Interior Koronavirüs Ile Mücadele Kapsamında - Yeni Kısıtlama ve Tedbirler Genelgeleri; the Ministry of the Interior, 2020.
- Turkish Medical Association (TTB) Tıp Fakültesi Son Sınıf Eğitiminde Yaratılan Kargaşa Giderilmeli, Öğrencilerin Mağdur Olmaları Önlenmelidir. 2019.
- (TEB), T.P.A. Maske Teminindeki Sorunlar Çözülmelidir Available online: https://covid19.teb.org.tr/news/8833/Maske_Teminindeki_Sorunlar_Çözülmelidir.
- Asu, G.; Gemlik, H.N. A Qualitative Study on the Problems and Solution Proposals of Healthcare Employees in the Field during the Covid-19 Pandemic Process. J. Heal. Serv. Educ. 2020, 4, 45–52. [Google Scholar] [CrossRef]
- Kader, C.; Erbay, A.; Demirel, M.S.; Kocabiyik, O.; Ciftci, E.; Yalcın-Colak, N.; Unsal, G.; Eren-Gok, S. Evaluation of Attitudes and Behaviors of Healthcare Professionals towards COVID-19 Vaccination. Klimik Dergisi/Klimik J. 2022, 35, 30–35. [Google Scholar] [CrossRef]
- Sert Karaaslan, Y. Sağlık Çalışanlarına Yönelik Ilk Doz Aşılamada Sona Gelindi. Anadolu Agency 2021.
- (TEB) Turkish Pharmacists’ Association FIP Sağlık Danışmanlığı COVID-19 Kılavuzları; Ankara, 2020.
- The Ministry of Health COVID-19 Rehberi; Ankara, 2020.
- KLIMIK - Turkish Society of Clinical Microbiology and Infectious Diseases COVID-19: Bilgi Notları ve Dernek Görüşleri; Ankara, 2020.
- The Ministry of Health Health Statistics Yearbook - 2020; Ankara, 2022.
- The Ministry of Health COVID-19: Temaslı Takibi, Salgın Yönetimi, Evde Hasta İzlemi ve Filyasyon; Ankara, 2021.
- The Ministry of Health COVID-19 National Strategy for the Implementation of Vaccines; Ankara, 2021.
- Haznedaroğlu Benlioğlu, E.; Bayrak Durmaz, S.; Göksal, K. COVID-19 Vaccination Hesitancy among Patients Admitted to the Immunology and Allergy Clinic with Drug Allergies. Heal. Sci. Q. 2023, 3, 219–227. [Google Scholar] [CrossRef]
- Şahin, H. The Reasons for the COVID-19 Anti-Vaccine in Turkey: Twitter Example. Anemon 2022, 10, 579–593. [Google Scholar] [CrossRef]
- Sonmezer, M.C.; Sahin, T.K.; Erul, E.; Ceylan, F.S.; Hamurcu, M.Y.; Morova, N.; Al, I.R.; Unal, S. Knowledge, Attitudes, and Perception towards COVID-19 Vaccination among the Adult Population: A Cross-Sectional Study in Turkey. Vaccines 2022, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Erciyes University Covid-19 Aşı Yerli ve Milli Aşısı Hakkında Available online: https://ikum.erciyes.edu.tr/tr/duyuru-detay/covid-19-asi-yerli-ve-milli-asisi-hakkinda.
- official newspaper Bazı Alacakların Yeniden Yapılandırılması İle Bazı Kanunlarda Değişiklik Yapılması Hakkında Kanun; Türkiye, 2020.
- Ergezen, A.K. Social Support Programs during COVID-19 Outbreak in Turkey. Gazi Med. J. 2020, 31, 322–324. [Google Scholar] [CrossRef]
- Derneği, İ.H.; Dertli, N. COVID-19 Pandemisi Sürecinde Ekonomik ve Sosyal Haklar Raporu; Ankara, 2020.
- Bulut, H.G.; Demir, M. Social Support Polcies Applied InTürkiye During the COVID-19 Pandemin Process. J. Bus. Entrep. Res. 2022, 36–47. [Google Scholar]
- The Ministry of National Education Eba Available online: https://www.eba.gov.tr/.
- Boylu, E.; Isık, P.; Isık, Ö.F. COVID-19 Pandemic and Emergency Distance Turkish Teaching. Turkisk Online J. Distance Educ. 2022, 23, 212–234. [Google Scholar] [CrossRef]
- Işık, O.; Tengilimoğlu, D.; Şenel Tekin, P.; Tosun, N.; Zekioğlu, A. Evaluation of Students’ Opinions Regarding Distance Learning Practices in Turkish Universities during the Covid-19 Pandemic. Yuksekogretim Derg. 2021, 11, 607–616. [Google Scholar] [CrossRef]
- Alan, Ü. Distance Education During the COVID-19 Pandemic in Turkey: Identifying the Needs of Early Childhood Educators. Early Child. Educ. J. 2021, 49, 987–994. [Google Scholar] [CrossRef]
- Yaylak, E. Distance Education in Turkiye During the Covid-19 Pandemic: What Do Stakeholders Think? Turkish Online J. Distance Educ. 2022, 23, 0–3. [Google Scholar] [CrossRef]
- Ünal, E.C. Ücretsiz Maske Dağıtımında Başvurular E-Devlet Kapısı Üzerinden Alınacak. Anadolu Agency 2020.
- Demirel, A.C.; Sütçü, S. Evaluation of Applications and Services for the Elderly During the Covid-19 Outbreak in Turkey. OPUS Int. J. Soc. Res. 2021, 17, 1–35. [Google Scholar] [CrossRef]
- Çimen, H. Rethinking the Importance of Social Assistance in Turkey During the Pandemic That Shocked the World (COVID 19). Anadolu Üniversitesi İktisadi ve İdari Bilim. Fakültesi Derg. 2021, 22, 15–38. [Google Scholar] [CrossRef]
- Erbay, H. On Medical Ethics, Story and Narrating. Turkish J. Bioeth. 2017, 4, 29–35. [Google Scholar] [CrossRef]
- Çamlıtepe, M. The Effect of Digital Technologies About Performing Arts and Music Practices in the Pandemic Process. Balk. Music Art J. 2022, 4, 1–10. [Google Scholar] [CrossRef]
- Commission Covid-19 Stories; Cander, B., Yakıncı, C., Eds.; 1st ed.; Inonu University Press: Malatya, 2020;
- The Presidency of Religious Affairs Prayers Rose from the Minarets Available online: https://diyanet.gov.tr/tr-TR/Kurumsal/Detay/29429/minarelerden-semaya-dualar-yukseldi#.
- Largent, E.A.; Miller, F.G. The Legality and Ethics of Mandating COVID-19 Vaccination. Perspect. Biol. Med. 2021, 64, 479–493. [Google Scholar] [CrossRef]
- Erbay, H. Herding Cats: Ethics in Prehospital Triage. Signa Vitae 2022, 18, 15–22. [Google Scholar] [CrossRef]
- De Oliveira, A.C.A.X.; Paumgartten, F.J.R. Ethical Issues in Placebo-Controlled Trials of COVID-19 Vaccines. Cad. Saude Publica 2021, 37. [Google Scholar] [CrossRef] [PubMed]
- Freckelton, I. Human Challenge Trials: Ethical and Legal Issues for COVID-19 Research. J. Law Med. 2021, 28. [Google Scholar]
- Öncü, M.A.; Yildirim, S.; Bostanci, S.; Erdoğan, F. The Effect of COVID-19 Pandemic on Health Management and Health Services: A Case of Turkey. Duzce Med. J. 2021, 23, 61–70. [Google Scholar] [CrossRef]
- Coccolini, F.; Cicuttin, E.; Cremonini, C.; Tartaglia, D.; Viaggi, B.; Kuriyama, A.; Picetti, E.; Ball, C.; Abu-Zidan, F.; Ceresoli, M.; et al. A Pandemic Recap: Lessons We Have Learned. World J. Emerg. Surg. 2021, 16, 1–8. [Google Scholar] [CrossRef]
- Yildirim, D.; Kocatepe, V. Professional Values and Ethical Sensitivities of Nurses in COVID-19 Pandemic. Nurs. Forum 2022, 57, 1111–1119. [Google Scholar] [CrossRef]
- Soylar, P.; Ulucan, M.; Dogan Yuksekol, O.; Baltaci, N.; Ersogutcu, F. Ethical Problems among Nurses during Pandemics: A Study from Turkey. Ethics, Med. Public Heal. 2022, 22, 100796. [Google Scholar] [CrossRef]
- Aliyu, A.A. Public Health Ethics and the COVID-19 Pandemic. Ann. Afr. Med. 2021, 20, 157–163. [Google Scholar]
- Tan, S.Y.; Foo, C. De; Verma, M.; Hanvoravongchai, P.; Cheh, P.L.J.; Pholpark, A.; Marthias, T.; Hafidz, F.; Prawidya Putri, L.; Mahendradhata, Y.; et al. Mitigating the Impacts of the COVID-19 Pandemic on Vulnerable Populations: Lessons for Improving Health and Social Equity. Soc. Sci. Med. 2023, 328, 116007. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, Q.; Zhang, T.; Yang, L. Vulnerability and Fraud: Evidence from the COVID-19 Pandemic. Humanit. Soc. Sci. Commun. 2022, 9, 1–12. [Google Scholar] [CrossRef]
- Girotto, S. Vulnerability and the Covid-19 Pandemic: Educating to a New Notion of Health. Int. J. Ethics Educ. 2023. [Google Scholar] [CrossRef]
- Peñalba, E. Pandemic and Social Vulnerability: The Case of the Philippines. In The Societal Impacts of Covid-19: A Transnational Perspective; Istanbul University Press, 2021; pp. 203–219.
- The Lancet Redefining Vulnerability in the Era of COVID-19. Lancet 2020, 395, 1089. [CrossRef]
- Özer, M. Educational Policy Actions by the Ministry of National Education in the Times of COVID-19 Pandemic in Turkey. Kastamonu Eğitim Derg. 2020, 28, 1124–1129. [Google Scholar] [CrossRef]
- World Health Organization (WHO) WHO Delivers Advice and Support for Older People during COVID-19 Available online: https://www.who.int/news-room/feature-stories/detail/who-delivers-advice-and-support-for-older-people-during-covid-19.
- Ilgili, Ö.; Gökçe Kutsal, Y. Impact of COVID-19 among the Elderly Population. Turkish J. Geriatr. 2020, 23, 419–423. [Google Scholar] [CrossRef]
- The Ministry of Family and Social Services Engelli ve Yaşlı Gündüz Yaşam Merkezleri Yeniden Hizmet Vermeye Başladı Available online: https://www.aile.gov.tr/eyhgm/haberler/engelli-ve-yasli-gunduz-yasam-merkezleri-yeniden-hizmet-vermeye-basladi/.
- Demir, B.; Mandıracıoğlu, A. Discriminatory Practices towards the Elderly during the COVID-19 Pandemic and Assessment of the Situation on the Elderly People. Ege J. Med. 2021, 60, 181–190. [Google Scholar] [CrossRef]
- Wyszyński, M.; Grudziński, M.; Pokonieczny, K.; Kaszubowski, M. The Assessment of COVID-19 Vulnerability Risk for Crisis Management. Appl. Sci. 2022, 12. [Google Scholar] [CrossRef]
- Yaşar, Ö.; Avcı, N. Changing Elderliness Perception: The Elders Stigmatized By COVID-19. J. Turkish Stud. 2020, 15, 1251–1273. [Google Scholar] [CrossRef]
- Karasu, F.; Öztürk Çopur, E.; Ayar, D. The Impact of COVID-19 on Healthcare Workers’ Anxiety Levels. J. Public Heal. 2022, 30, 1399–1409. [Google Scholar] [CrossRef] [PubMed]
- Gokkaya, B.; Yazici, T.N.; Kargul, B. Perceived Stress and Perceived Vulnerability at Healthcare Workers during Covid-19 Pandemic. Clin. Exp. Heal. Sci. 2022, 12, 431–438. [Google Scholar] [CrossRef]
- Onan, N.; Dinc, S.; Demir, Z. Pandemic Process from the Window of Healthcare Professionals. Value Heal. Sci. 2022, 12, 474–482. [Google Scholar]
- Keten Edis, E. Experiences of Intensive Care Nurses in the COVID-19 Process: A Qualitative Study. Gümüşhane Univ. J. Heal. Sci. 2022, 11, 476–486. [Google Scholar]
- Dincer, B.; Inangil, D. The Effect of Emotional Freedom Techniques on Nurses’ Stress, Anxiety, and Burnout Levels during the COVID-19 Pandemic: A Randomized Controlled Trial. Explore 2021, 17, 109–114. [Google Scholar] [CrossRef]
- Murat, M.; Köse, S.; Savaşer, S. Determination of Stress, Depression and Burnout Levels of Front-Line Nurses during the COVID-19 Pandemic. Int. J. Ment. Health Nurs. 2021, 30, 533–543. [Google Scholar] [CrossRef]
- Kahraman, B.; Uğur, T.D.; Girgin, D.; Koçak, A.B. COVID-19 Döneminde Yaşlı Olmak: 65 Yaş ve Üzeri Bireylerin Pandemi Sürecinde Yaşadığı Sorunlar. Hacettepe Univ. J. Fac. Lett. 2022, 39, 124–143. [Google Scholar] [CrossRef]
- Yurtsever, M. Short-Term Effects of COVID-19 Pandemic on the Environment. Uludağ Univ. J. Fac. Eng. 2020, 25, 1611–1636. [Google Scholar] [CrossRef]
- Council of Higher Education (YÖK) Yükseköğretim Kurumlarında Uzaktan Öğretime İlişkin Usul ve Esaslar; Council of Higher Education (YÖK): Ankara, 2020;
- Ahsan, M. Strategic Decisions on Urban Built Environment to Pandemics in Turkey: Lessons from COVID-19. J. Urban Manag. 2020, 9, 281–285. [Google Scholar] [CrossRef]
- Chimed-Ochir, O.; Amarsanaa, J.; Ghotbi, N.; Yumiya, Y.; Kayano, R.; Van Trimpont, F.; Murray, V.; Kubo, T. Impact of COVID-19 on Health Emergency and Disaster Risk Management System: A Scoping Review of Healthcare Workforce Management in COVID-19. Sustain. 2023, 15. [Google Scholar] [CrossRef]
- The Ministry of Interior AFAD - Strategic Plan 2019-2023; Ankara, 2018.
- Commission Ethical Disaster Resilience for Our Global Community: Tenth Youth Looking Beyond Disaster (LBD19) Training Workshop - Istanbul Available online: https://www.eubios.info/youth_looking_beyond_disaster_lbd/lbd10_istanbul.
- The Ministry of Health Pandemik Influenza Ulusal Hazırlık Planı Available online: https://hsgm.saglik.gov.tr/depo/Yayinlarimiz/Eylem_Planlari/Ulusal_Pandemi_Hazirlik_Plani.pdf.
- AFAD Kahramanmaraş 2019 Ulusal TAMP Tatbikatı Gerçekleştirildi Available online: https://kahramanmaras.afad.gov.tr/kahramanmaras-ulusal-deprem-tatbikati-gerceklestirildi.
- The Governorship of Osmaniye Covıd-19 Pandemi Acil Durum Planı Available online: https://osmaniyeisg.meb.gov.tr/meb_iys_dosyalar/2020_04/20115003_ACYL_DURUM_EYLEM_PLANI_COVYD_19-SON.pdf.
- Gürbüz, Y.; Şencan, İ. Pandemic Preparedness and Action Plan. Türkiye Klin. J Inf Dis 2010, 3, 40–48. [Google Scholar]
- The Ministry of Family and Social Services COVID-19 Pandemisi Yönetimi ve Eylem Planı Rehberi Available online: https://www.csgb.gov.tr/media/68340/kiplas-covid-19-pandemisi-yonetimi-ve-eylem-plani-26022021.pdf.
- Mert, S.; Sayilan, A.A.; Karatoprak, A.P.; Baydemir, C. The Effect of Covid-19 on Ethical Sensitivity. Nurs. Ethics 2021, 28, 1124–1136. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).