Submitted:
23 October 2023
Posted:
24 October 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Subjects and Methods
Study Design and Study Population
Data Collection and BMI-for-Age Percentile Change Measurement
Statistical Analysis
Ethical Consideration
Results
Discussion
Limitations
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Abbreviations
| BMI | Body Mass Index |
| COVID-19 | Coronavirus Disease 2019 |
| HIS | Health Information System |
| IRB | Institutional Review Board |
| PHC | Primary Healthcare Center |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SPSS | Statistical Package for Social Sciences |
| T2DM | Type-2 Diabetes Mellitus |
References
- Vlachos, J.; Hertegård, E.; Svaleryd, H.B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021, 118, e2020834118. [Google Scholar] [CrossRef]
- García-Peñalvo, F.J.; Corell, A.; Abella-García, V.; Grande-de-Prado, M. Recommendations for mandatory online assessment in higher education during the COVID-19 pandemic. In Radical Solutions for Education in a Crisis Context; Springer: Singapore, 2021; pp. 85–98. [Google Scholar]
- Bhurosy, T.; Jeewon, R. Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? The Scientific World Journal 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Orio, F.; Muscogiuri, G.; Nese, C.; et al. Obesity, type 2 diabetes mellitus and cardiovascular disease risk: an uptodate in the management of polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2016, 207, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Miranda, E.; Costa, P.R.F.; Queiroz, V.A.O.; Pereira-Santos, M.; Santana, M.L.P. Overweight and Obesity Associated with Higher Depression Prevalence in Adults: A Systematic Review and Meta-Analysis. J Am Coll Nutr. 2017, 36, 223–233. [Google Scholar] [CrossRef]
- AlBlooshi, A.; Shaban, S.; AlTunaiji, M.; et al. Increasing obesity rates in school children in United Arab Emirates. Obes Sci Pract. 2016, 2, 196–202. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U. S. BMC Public Health. 2020, 20, 1351. [Google Scholar] [CrossRef]
- Pavlovic, A.; DeFina, L.F.; Natale, B.L.; et al. Keeping children healthy during and after COVID-19 pandemic: meeting youth physical activity needs. BMC Public Health. 2021, 21, 485. [Google Scholar] [CrossRef]
- Xiang, M.; Zhang, Z.; Kuwahara, K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020, 63, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Bschaden, A.; Stroebele-Benschop, N. Changes in lifestyle, diet, and body weight during the first COVID 19 'lockdown' in a student sample. Appetite. 2021, 167, 105638. [Google Scholar] [CrossRef]
- Jalal, S.M.; Beth, M.R.M.; Al-Hassan, H.J.M.; et al. Body Mass Index, Practice of Physical Activity and Lifestyle of Students During COVID-19 Lockdown. J Multidiscip Healthc. 2021, 14, 1901–1910. [Google Scholar] [CrossRef]
- Weaver, R.G.; Hunt, E.T.; Armstrong, B.; et al. COVID-19 Leads to Accelerated Increases in Children's BMI z-Score Gain: An Interrupted Time-Series Study. Am J Prev Med. 2021, 61, e161–e169. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Borrow, R.; Safadi, M.A.P.; et al. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum Vaccin Immunother. 2021, 17, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Xiang, M.; Cheung, T.; et al. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Correia, L.; Medeiros, M.; Chaves, R.; et al. Nutritional status of children in school age: A look of concern in an era of COVID-19 pandemic. Clin Nutr ESPEN. 2020, 40, 619. [Google Scholar] [CrossRef]
- Azoulay, E.; Yackobovitch-Gavan, M.; Yaacov, H.; et al. Weight Status and Body Composition Dynamics in Children and Adolescents During the COVID-19 Pandemic. Front Pediatr. 2021, 9, 707773. [Google Scholar] [CrossRef] [PubMed]
- Brooks, C.G.; Spencer, J.R.; Sprafka, J.M.; et al. Pediatric BMI changes during COVID-19 pandemic: An electronic health record-based retrospective cohort study. EClinicalMedicine. 2021, 38, 101026. [Google Scholar] [CrossRef] [PubMed]
- Cipolla, C.; Curatola, A.; Ferretti, S.; et al. Eating habits and lifestyle in children with obesity during the COVID19 lockdown: a survey in an Italian center. Acta Biomed. 2021, 92, e2021196. [Google Scholar]
- Hu, J.; Liu, J.; Wang, J.; et al. Unfavorable progression of obesity in children and adolescents due to COVID-19 pandemic: A school-based survey in China. Obesity (Silver Spring). 2021, 29, 1907–1915. [Google Scholar] [CrossRef]
- Hanbazaza, M.; Wazzan, H. Changes in eating habits and lifestyle during COVID-19 curfew in children in Saudi Arabia. Nutr Res Pract. 2021, 15, S41–S52. [Google Scholar] [CrossRef]
- Al Agha, A.E.; Alharbi, R.S.; Almohammadi, O.A.; et al. Impact of COVID-19 lockdown on glycemic control in children and adolescents. Saudi Med J. 2021, 42, 44–48. [Google Scholar] [CrossRef]
- Poelman, M.P.; Gillebaart, M.; Schlinkert, C.; et al. Eating behavior and food purchases during the COVID-19 lockdown: A cross-sectional study among adults in the Netherlands. Appetite. 2021, 157, 105002. [Google Scholar] [CrossRef] [PubMed]
- Alhaj, O.A.; Elsahoryi, N.A.; Alathamneh, A.; et al. Knowledge and perception of the ketogenic diet followers among Arab adults in seventeen countries. Obesity Medicine. 2021, 25, 100354. [Google Scholar] [CrossRef]
| Variable | 2019 group (N=17,860) | 2020 group (N=17,860) | 2021 group (N=17,860) | Total (N=53,580) | |
| Gender | Male gender | 9220 (52%) | 7681 (43%) | 7603 (43%) | 24504 (46%) |
| Female gender | 8640 (48%) | 10179 (57%) | 10257 (57%) | 29076 (54%) | |
| Age group | 6-9 years old students | 5257 (29%) | 5339 (30%) | 6341 (36%) | 16937 (31.6%) |
| 10-14 years old students | 7351 (41%) | 5954 (33%) | 5236 (29%) | 18541 (34.6%) | |
| 15-18 years old students | 5252 (29%) | 6567 (37%) | 6283 (35%) | 18102 (33.7%) | |
| Region | Students in West Saudi region | 2859 (16%) | 1539 (9%) | 1709 (10%) | 6107 (11%) |
| Students in North Saudi region | 2019 (11%) | 1528 (9%) | 1289 (7%) | 4836 (9%) | |
| Students in South Saudi region | 5878 (33%) | 5144 (29%) | 4869 (27%) | 15891 (30%) | |
| Students in East Saudi region | 1450 (8%) | 1759 (10%) | 2000 (11%) | 5209 (10%) | |
| Students in Center Saudi region | 5654 (32%) | 7890 (44%) | 7993 (45%) | 21537 (40%) | |
| Variable | Year | |||||||||||
| 2019 (N total=17,860) | 2020 (N total=17,860) | 2021 (N total=17,860) | ||||||||||
| BMI category | Underweight (<5th percentile) |
Normal (5th – 85th percentile) |
Overweight (85th – 95th percentile) |
Obesity (>95th percentile) |
Underweight (<5th percentile) |
Normal (5th – 85th percentile) |
Overweight (85th – 95th percentile) |
Obesity(>95th percentile) | Underweight (<5th percentile) |
Normal (5th – 85th percentile) |
Overweight (85th – 95th percentile) |
Obesity (>95th percentile) |
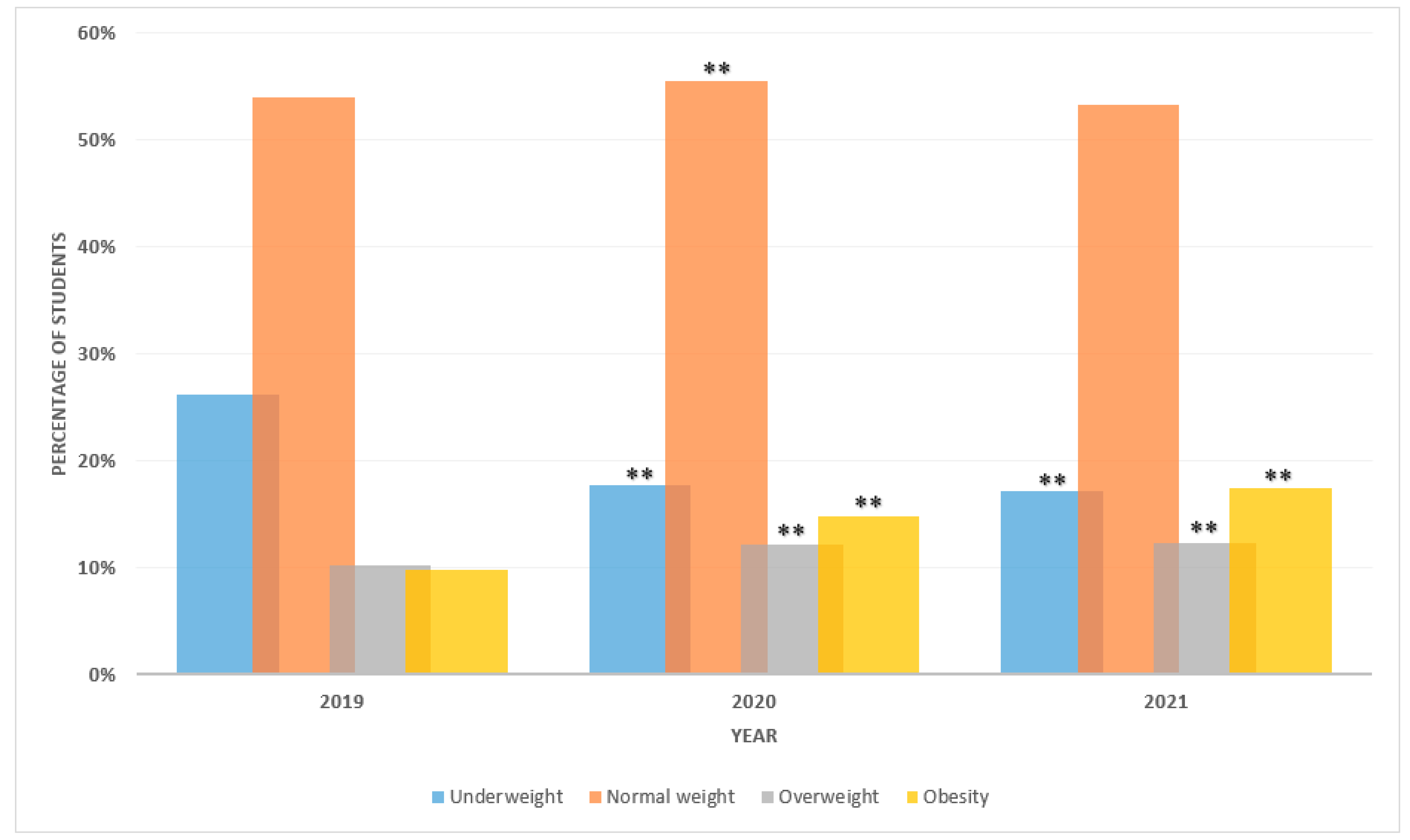
| Total N=53,580 | 4671 (26) | 9636 (54) | 1820 (10) | 1733 (10) | 3149 (18) | 9914 (56) | 2155 (12) | 2642 (15) | 3052 (17) | 9508 (53) | 2198 (12) | 3102 (17) |
| Age category | ||||||||||||
| 6-9 years | N= 5257 | N= 5339 | N= 6341 | |||||||||
| 1723 (33) | 2818 (54) | 368 (7) | 348 (7) | 1339 (25) | 3091 (58) | 422 (8) | 487 (9) | 1660 (26) | 3357 (53) | 548 (9) | 776 (12) | |
| 10-14 years | N= 7351 | N= 5954 | N= 5236 | |||||||||
| 2021 (27) | 3848 (52) | 806 (11) | 676 (9) | 926 (16) | 3263 (55) | 860 (14) | 905 (15) | 595 (11) | 2744 (52) | 814 (16) | 1083 (21) | |
| 15-18 years | N= 5252 | N= 6567 | N= 6283 | |||||||||
| 927 (18) | 2970 (57) | 646 (12) | 709 (13) | 884 (13) | 3560 (54) | 873 (13) | 1250 (19) | 797 (13) | 3407 (54) | 836 (13) | 1243 (20) | |
| Sex | ||||||||||||
| Male | N= 9220 | N= 7681 | N= 7603 | |||||||||
| 2434 (26) | 4921 (53) | 916 (10) | 949 (10) | 1451 (19) | 4253 (55) | 845 (11) | 1132 (15) | 1411 (19) | 4009 (53) | 895 (12) | 1288 (17) | |
| Female | N= 8640 | N= 10179 | N= 10257 | |||||||||
| 2237 (26) | 4715 (55) | 904 (10) | 784 (9) | 1698 (17) | 5661 (56) | 1310 (13) | 1510 (15) | 1641 (16) | 5499 (54) | 1303 (13) | 1814 (18) | |
| Saudi region | ||||||||||||
| West | N= 2859 | N= 1539 | N= 1709 | |||||||||
| 809 (28) | 1501 (53) | 269 (9) | 280 (10) | 283 (18) | 854 (55) | 198 (13) | 204 (13) | 304 (18) | 884 (52) | 212 (12) | 309 (18) | |
| North | N= 2019 | N= 1528 | N= 1289 | |||||||||
| 459 (23) | 1203 (60) | 186 (9) | 171 (8) | 207 (14) | 905 (59) | 193 (13) | 223 (15) | 183 (14) | 733 (57) | 162 (13) | 211 (16) | |
| South | N= 5878 | N= 5144 | N= 4869 | |||||||||
| 1764 (30) | 3004 (51) | 592 (10) | 518 (9) | 1146 (22) | 2751 (53) | 576 (11) | 671 (13) | 995 (20) | 2583 (53) | 525 (11) | 766 (16) | |
| East | N= 1450 | N= 1759 | N= 2000 | |||||||||
| 335 (23) | 825 (57) | 138 (10) | 152 (10) | 262 (15) | 985 (56) | 211 (12) | 301 (17) | 298 (15) | 1082 (54) | 243 (12) | 377 (19) | |
| Centre | N= 5654 | N= 7890 | N= 7993 | |||||||||
| 1304 (23) | 3103 (55) | 635 (11) | 612 (11) | 1251 (16) | 4419 (56) | 977 (12) | 1243 (16) | 1272 (16) | 4226 (53) | 1056 (13) | 1439 (18) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





