Submitted:
23 October 2023
Posted:
24 October 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
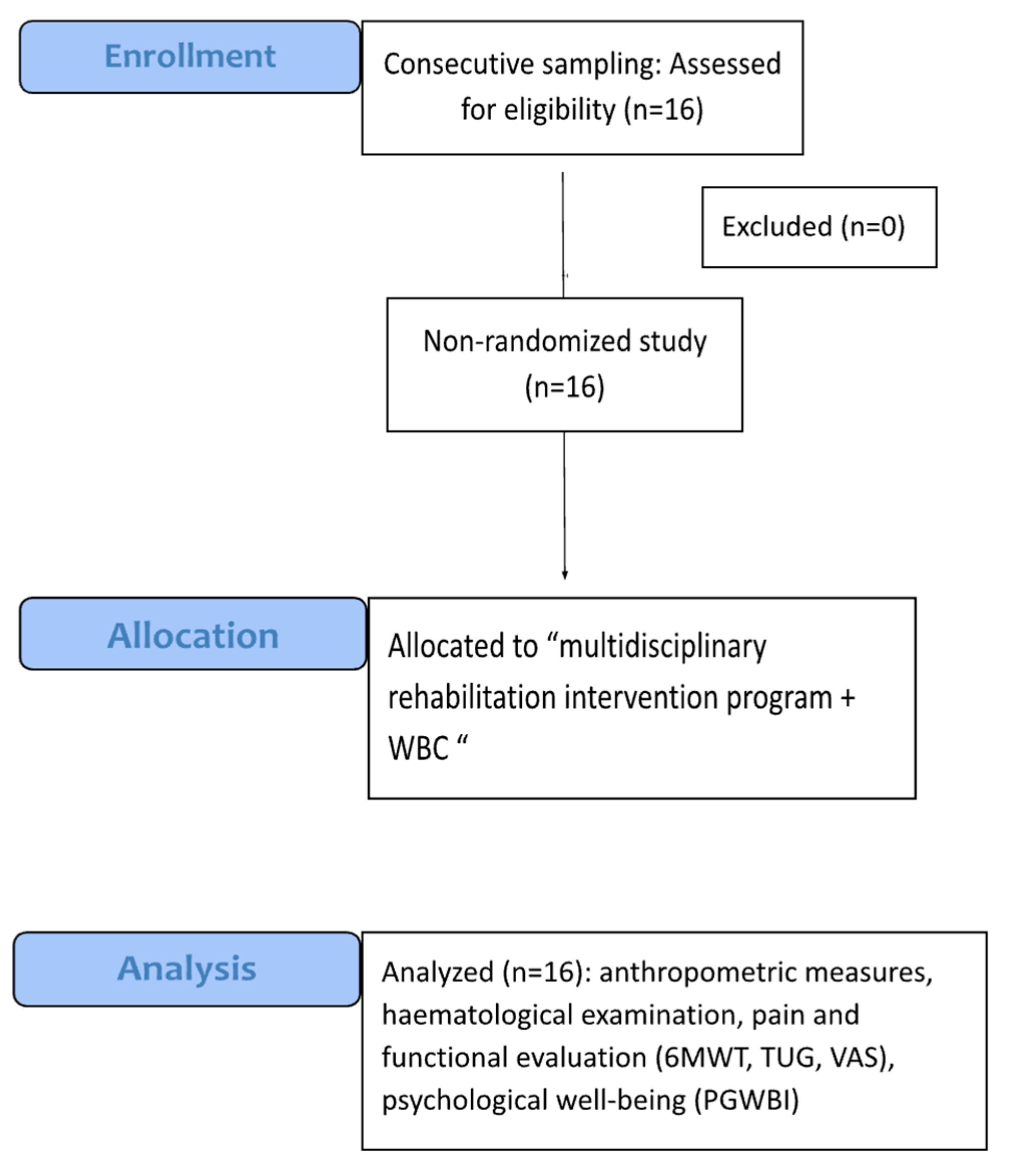
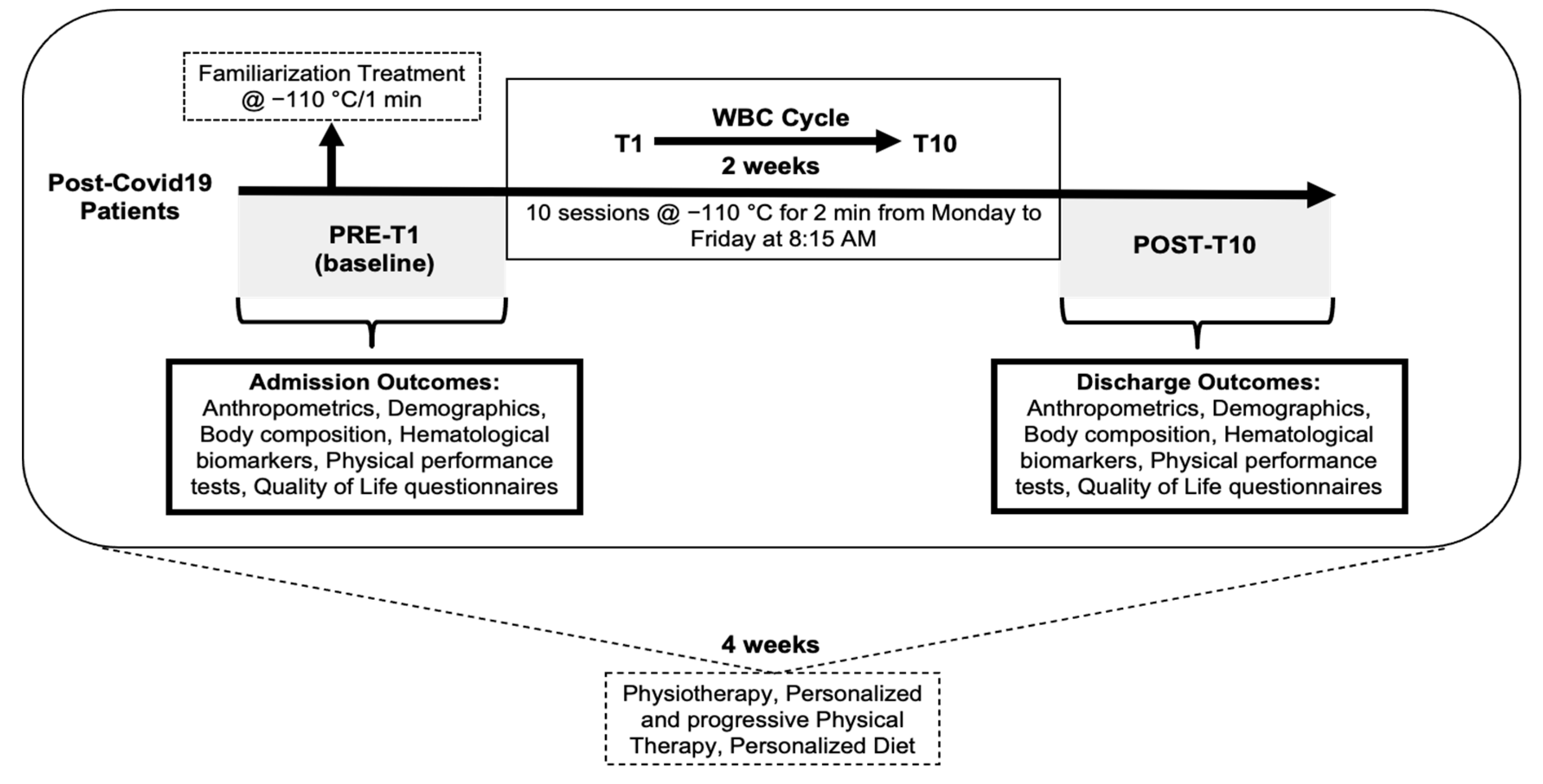
2.1. Study design
2.2. Participant Eligibility
2.3. Participants
2.4. Study Variables
2.5. Intervention
2.6. Description of the WBC session
2.7. Feasibility
2.8. Statistical analysis
2.9. Ethical considerations
3. Results
3.1. Participant Flow
Admission and discharge data comparison
Feasibility
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brugliera, L.; Spina, A.; Castellazzi, P.; Cimino, P.; Tettamanti, A.; Houdayer, E.; Arcuri, P.; Alemanno, F.; Mortini, P.; Iannaccone, S. Rehabilitation of COVID-19 patients. J Rehabil Med 2020, 52, jrm00046. [Google Scholar] [CrossRef]
- Curci, C.; Pisano, F.; Bonacci, E.; Camozzi, D.M.; Ceravolo, C.; Bergonzi, R.; De Franceschi, S.; Moro, P.; Guarnieri, R.; Ferrillo, M.; et al. Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur J Phys Rehabil Med 2020, 56, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Aidalina, M.; Khalsom, S. COVID-19 vaccination: a systematic review of vaccination strategies based on economic evaluation studies. Med J Malaysia 2023, 78, 411–420. [Google Scholar]
- Beccia, F.; Di Pilla, A.; Causio, F.A.; Federico, B.; Specchia, M.L.; Favaretti, C.; Boccia, S.; Damiani, G. Narrative Review of the COVID-19 Pandemic's First Two Years in Italy. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef] [PubMed]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun 2022, 101, 93–135. [Google Scholar] [CrossRef] [PubMed]
- Hope, A.A.; Evering, T.H. Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. Infect Dis Clin North Am 2022, 36, 379–395. [Google Scholar] [CrossRef] [PubMed]
- Ferioli, M.; Prediletto, I.; Bensai, S.; Betti, S.; Daniele, F.; Di Scioscio, V.; Modolon, C.; Rimondi, M.R.; De Molo, C.; Serra, C.; et al. Spontaneous Evolution of COVID-19 Lung Sequelae: Results from a Double-Step Follow-Up. Respiration 2022, 101, 381–393. [Google Scholar] [CrossRef]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Lau, B.; Wentz, E.; Ni, Z.; Yenokyan, K.; Coggiano, C.; Mehta, S.H.; Duggal, P. Physical and mental health disability associated with long-COVID: Baseline results from a US nationwide cohort. medRxiv 2022. [Google Scholar] [CrossRef]
- Pouliopoulou, D.V.; Macdermid, J.C.; Saunders, E.; Peters, S.; Brunton, L.; Miller, E.; Quinn, K.L.; Pereira, T.V.; Bobos, P. Rehabilitation Interventions for Physical Capacity and Quality of Life in Adults With Post-COVID-19 Condition: A Systematic Review and Meta-Analysis. JAMA Netw Open 2023, 6, e2333838. [Google Scholar] [CrossRef]
- Alito, A.; Rodolico, C.; Palco, M.; Portaro, S. Steroid Management in a Patient with Myasthenia Gravis Undergoing COVID-19 Vaccination. Innov Clin Neurosci 2022, 19, 8. [Google Scholar] [PubMed]
- Behl, T.; Kumar, S.; Singh, S.; Bhatia, S.; Albarrati, A.; Albratty, M.; Meraya, A.M.; Najmi, A.; Bungau, S. Reviving the mutual impact of SARS-COV-2 and obesity on patients: From morbidity to mortality. Biomed Pharmacother 2022, 151, 113178. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-Penas, C.; Torres-Macho, J.; Elvira-Martinez, C.M.; Molina-Trigueros, L.J.; Sebastian-Viana, T.; Hernandez-Barrera, V. Obesity is associated with a greater number of long-term post-COVID symptoms and poor sleep quality: A multicentre case-control study. Int J Clin Pract 2021, 75, e14917. [Google Scholar] [CrossRef] [PubMed]
- Shyam, S.; Gomez-Martinez, C.; Paz-Graniel, I.; Gaforio, J.J.; Martinez-Gonzalez, M.A.; Corella, D.; Fito, M.; Martinez, J.A.; Alonso-Gomez, A.M.; Warnberg, J.; et al. Coronavirus disease 2019 is associated with long-term depressive symptoms in Spanish older adults with overweight/obesity and metabolic syndrome. Psychol Med 2023, 1–11. [Google Scholar] [CrossRef]
- Varallo, G.; Suso-Ribera, C.; Ghiggia, A.; Veneruso, M.; Cattivelli, R.; Guerrini Usubini, A.; Franceschini, C.; Musetti, A.; Plazzi, G.; Fontana, J.M.; et al. Catastrophizing, Kinesiophobia, and Acceptance as Mediators of the Relationship Between Perceived Pain Severity, Self-Reported and Performance-Based Physical Function in Women with Fibromyalgia and Obesity. J Pain Res 2022, 15, 3017–3029. [Google Scholar] [CrossRef] [PubMed]
- Aburto, S.; Cisterna, M.; Acuna, J.; Ruiz, C.; Viscardi, S.; Marquez, J.L.; Villano, I.; Letelier, P.; Guzman, N. Obesity as a Risk Factor for Severe COVID-19 in Hospitalized Patients: Epidemiology and Potential Mechanisms. Healthcare (Basel) 2022, 10. [Google Scholar] [CrossRef] [PubMed]
- Raman, B.; Bluemke, D.A.; Luscher, T.F.; Neubauer, S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J 2022, 43, 1157–1172. [Google Scholar] [CrossRef]
- Colas, C.; Le Berre, Y.; Fanget, M.; Savall, A.; Killian, M.; Goujon, I.; Labeix, P.; Bayle, M.; Feasson, L.; Roche, F.; et al. Physical Activity in Long COVID: A Comparative Study of Exercise Rehabilitation Benefits in Patients with Long COVID, Coronary Artery Disease and Fibromyalgia. Int J Environ Res Public Health 2023, 20. [Google Scholar] [CrossRef]
- Zheng, C.; Chen, X.K.; Sit, C.H.; Liang, X.; Ming-Hui, L.I.; Ma, A.C.; Wong, S.H. Effect of Physical Exercise-Based Rehabilitation on Long COVID: A Systematic Review and Meta-analysis. Med Sci Sports Exerc 2023. [Google Scholar] [CrossRef]
- Jimeno-Almazan, A.; Franco-Lopez, F.; Buendia-Romero, A.; Martinez-Cava, A.; Sanchez-Agar, J.A.; Sanchez-Alcaraz Martinez, B.J.; Courel-Ibanez, J.; Pallares, J.G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand J Med Sci Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- McNarry, M.A.; Berg, R.M.G.; Shelley, J.; Hudson, J.; Saynor, Z.L.; Duckers, J.; Lewis, K.; Davies, G.A.; Mackintosh, K.A. Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur Respir J 2022, 60. [Google Scholar] [CrossRef]
- Saha, S.; Sharma, K. Modification of Lifestyle to Recover from Post-COVID Symptoms: A Short Review. J Lifestyle Med 2022, 12, 113–118. [Google Scholar] [CrossRef]
- Gobbi, M.; Bezzoli, E.; Ismelli, F.; Trotti, G.; Cortellezzi, S.; Meneguzzo, F.; Arreghini, M.; Seitanidis, I.; Brunani, A.; Aspesi, V.; et al. Skeletal Muscle Mass, Sarcopenia and Rehabilitation Outcomes in Post-Acute COVID-19 Patients. J Clin Med 2021, 10. [Google Scholar] [CrossRef]
- Araujo, B.T.S.; Barros, A.; Nunes, D.T.X.; Remigio de Aguiar, M.I.; Mastroianni, V.W.; de Souza, J.A.F.; Fernades, J.; Campos, S.L.; Brandao, D.C.; Dornelas de Andrade, A. Effects of continuous aerobic training associated with resistance training on maximal and submaximal exercise tolerance, fatigue, and quality of life of patients post-COVID-19. Physiother Res Int 2023, 28, e1972. [Google Scholar] [CrossRef]
- Cerfoglio, S.; Capodaglio, P.; Rossi, P.; Verme, F.; Boldini, G.; Cvetkova, V.; Ruggeri, G.; Galli, M.; Cimolin, V. Tele-Rehabilitation Interventions for Motor Symptoms in COVID-19 Patients: A Narrative Review. Bioengineering (Basel) 2023, 10. [Google Scholar] [CrossRef]
- Fontana, J.M.; Bozgeyik, S.; Gobbi, M.; Pitera, P.; Giusti, E.M.; Dugue, B.; Lombardi, G.; Capodaglio, P. Whole-body cryostimulation in obesity. A scoping review. J Therm Biol 2022, 106, 103250. [Google Scholar] [CrossRef] [PubMed]
- Fontana, J.M.; Gobbi, M.; Piterà, P.; Giusti, E.M.; Capodaglio, P. Whole-Body Cryostimulation in Fibromyalgia: A Scoping Review. Applied Sciences 2022, 12(9) 4794. [CrossRef]
- Rymaszewska, J.; Ramsey, D.; Chladzinska-Kiejna, S. Whole-body cryotherapy as adjunct treatment of depressive and anxiety disorders. Arch Immunol Ther Exp (Warsz) 2008, 56, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.; Kostka, J.; Wlodarczyk, T.; Dugue, B. Whole-body cryostimulation (cryotherapy) provides benefits for fatigue and functional status in multiple sclerosis patients. A case-control study. Acta Neurol Scand 2016, 134, 420–426. [Google Scholar] [CrossRef]
- Varallo, G.; Pitera, P.; Fontana, J.M.; Gobbi, M.; Arreghini, M.; Giusti, E.M.; Franceschini, C.; Plazzi, G.; Castelnuovo, G.; Capodaglio, P. Is Whole-Body Cryostimulation an Effective Add-On Treatment in Individuals with Fibromyalgia and Obesity? A Randomized Controlled Clinical Trial. J Clin Med 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Douzi, W.; Dupuy, O.; Tanneau, M.; Boucard, G.; Bouzigon, R.; Dugue, B. 3-min whole body cryotherapy/cryostimulation after training in the evening improves sleep quality in physically active men. Eur J Sport Sci 2019, 19, 860–867. [Google Scholar] [CrossRef] [PubMed]
- White, G.E.; Wells, G.D. Cold-water immersion and other forms of cryotherapy: physiological changes potentially affecting recovery from high-intensity exercise. Extrem Physiol Med 2013, 2, 26. [Google Scholar] [CrossRef]
- Rose, C.; Edwards, K.M.; Siegler, J.; Graham, K.; Caillaud, C. Whole-body Cryotherapy as a Recovery Technique after Exercise: A Review of the Literature. Int J Sports Med 2017, 38, 1049–1060. [Google Scholar] [CrossRef]
- Kujawski, S.; Zalewski, P.; Godlewska, B.R.; Cudnoch-Jedrzejewska, A.; Murovska, M.; Newton, J.L.; Sokolowski, L.; Slomko, J. Effects of whole-body cryotherapy and static stretching are maintained 4 weeks after treatment in most patients with chronic fatigue syndrome. Cryobiology 2023, 112, 104546. [Google Scholar] [CrossRef]
- Poignard, M.; Guilhem, G.; Jubeau, M.; Martin, E.; Giol, T.; Montalvan, B.; Bieuzen, F. Cold-water immersion and whole-body cryotherapy attenuate muscle soreness during 3 days of match-like tennis protocol. Eur J Appl Physiol 2023, 123, 1895–1909. [Google Scholar] [CrossRef] [PubMed]
- Piterà, P.; Gobbi, M.; Fontana, J.M.; Cattaldo, S.; Massucci, M.; Capodaglio, P. Whole-Body Cryostimulation: A Rehabilitation Booster in Post-COVID Patients? A Case Series. Applied Sciences 2022, 12, 4830. [Google Scholar] [CrossRef]
- Gobbi, M.; Trotti, G.; Tanzi, M.; Kasap, F.; Pitera, P.; Capodaglio, P. Post-Covid Symptoms and Whole-Body Cryotheraphy: A Case Report. J Rehabil Med Clin Commun 2022, 5, 1000075. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Lancaster, G.A.; Campbell, M.J.; Thabane, L.; Hopewell, S.; Coleman, C.L.; Bond, C.M. Defining Feasibility and Pilot Studies in Preparation for Randomised Controlled Trials: Development of a Conceptual Framework. PLoS One 2016, 11, e0150205. [Google Scholar] [CrossRef]
- Enright, P.L. The six-minute walk test. Respir Care 2003, 48, 783–785. [Google Scholar] [PubMed]
- Bohannon, R.W. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther 2006, 29, 64–68. [Google Scholar] [CrossRef]
- Gift, A.G. Visual analogue scales: measurement of subjective phenomena. Nurs Res 1989, 38, 286–288. [Google Scholar] [CrossRef]
- Lundgren-Nilsson, A.; Jonsdottir, I.H.; Ahlborg, G., Jr.; Tennant, A. Construct validity of the Psychological General Well Being Index (PGWBI) in a sample of patients undergoing treatment for stress-related exhaustion: a Rasch analysis. Health Qual Life Outcomes 2013, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- Hoeg, T.B.; Ladhani, S.; Prasad, V. How methodological pitfalls have created widespread misunderstanding about long COVID. BMJ Evid Based Med 2023. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.M.; Brigham, E.; Connolly, B.; McPeake, J.; Agranovich, A.V.; Kenes, M.T.; Casey, K.; Reynolds, C.; Schmidt, K.F.R.; Kim, S.Y.; et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. Lancet Respir Med 2021, 9, 1328–1341. [Google Scholar] [CrossRef] [PubMed]
- Sardella, A.; Chiara, E.; Alibrandi, A.; Bellone, F.; Catalano, A.; Lenzo, V.; Quattropani, M.C.; Basile, G. Changes in Cognitive and Functional Status and in Quality of Life of Older Outpatients during the COVID-19 Pandemic. Gerontology 2022, 68, 1285–1290. [Google Scholar] [CrossRef] [PubMed]
- Munblit, D.; Nicholson, T.; Akrami, A.; Apfelbacher, C.; Chen, J.; De Groote, W.; Diaz, J.V.; Gorst, S.L.; Harman, N.; Kokorina, A.; et al. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respir Med 2022, 10, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Leisman, D.E.; Ronner, L.; Pinotti, R.; Taylor, M.D.; Sinha, P.; Calfee, C.S.; Hirayama, A.V.; Mastroiani, F.; Turtle, C.J.; Harhay, M.O.; et al. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med 2020, 8, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Vimercati, L.; De Maria, L.; Quarato, M.; Caputi, A.; Gesualdo, L.; Migliore, G.; Cavone, D.; Sponselli, S.; Pipoli, A.; Inchingolo, F.; et al. Association between Long COVID and Overweight/Obesity. J Clin Med 2021, 10. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Sivan, M.; Delaney, B.; Evans, R.; Milne, R. Long covid-an update for primary care. BMJ 2022, 378, e072117. [Google Scholar] [CrossRef]
- Wahlgren, C.; Divanoglou, A.; Larsson, M.; Nilsson, E.; Ostholm Balkhed, A.; Niward, K.; Birberg Thornberg, U.; Lilliecreutz Gudmundsson, E.; Levi, R. Rehabilitation needs following COVID-19: Five-month post-discharge clinical follow-up of individuals with concerning self-reported symptoms. EClinicalMedicine 2022, 43, 101219. [Google Scholar] [CrossRef]
- Decary, S.; Gaboury, I.; Poirier, S.; Garcia, C.; Simpson, S.; Bull, M.; Brown, D.; Daigle, F. Humility and Acceptance: Working Within Our Limits With Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J Orthop Sports Phys Ther 2021, 51, 197–200. [Google Scholar] [CrossRef]
- De Maria, B.; Lucini, D.; Gois, M.O.; Catai, A.M.; Perego, F.; Malacarne, M.; Pagani, M.; Porta, A.; Dalla Vecchia, L.A. Improvement of Sympathovagal Balance by Regular Exercise May Counteract the Ageing Process. A Study by the Analysis of QT Variability. Front Physiol 2022, 13, 880250. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Andrenelli, E.; Negrini, F.; Lazzarini, S.G.; Cordani, C.; Ceravolo, M.G.; International Multiprofessional Steering Committee of Cochrane Rehabilitation, R. E.H.C.A. Rehabilitation and COVID-19: update of the rapid living systematic review by Cochrane Rehabilitation Field as of February 28th, 2022. Eur J Phys Rehabil Med 2022, 58, 498–501. [Google Scholar] [CrossRef]
- Udina, C.; Ars, J.; Morandi, A.; Vilaro, J.; Caceres, C.; Inzitari, M. Rehabilitation in adult post-COVID-19 patients in post-acute care with Therapeutic Exercise. J Frailty Aging 2021, 10, 297–300. [Google Scholar] [CrossRef] [PubMed]
- Cattadori, G.; Di Marco, S.; Baravelli, M.; Picozzi, A.; Ambrosio, G. Exercise Training in Post-COVID-19 Patients: The Need for a Multifactorial Protocol for a Multifactorial Pathophysiology. J Clin Med 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Lemos, M.M.; Cavalini, G.R.; Pugliese Henrique, C.R.; Perli, V.A.S.; de Moraes Marchiori, G.; Marchiori, L.L.M.; Sordi, A.F.; Franzoi de Moraes, S.M.; de Paula Ramos, S.; Valdes-Badilla, P.; et al. Body composition and cardiorespiratory fitness in overweight or obese people post COVID-19: A comparative study. Front Physiol 2022, 13, 949351. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Wu, X.; Jing, H.; Novakovic, V.A.; Shi, J. The intersection of obesity and (long) COVID-19: Hypoxia, thrombotic inflammation, and vascular endothelial injury. Front Cardiovasc Med 2023, 10, 1062491. [Google Scholar] [CrossRef]
- Zakynthinos, G.E.; Stavrou, V.T.; Malli, F.; Papathanasiou, I.V.; Zakynthinos, E.; Gourgoulianis, K.I.; Kalabakas, K.; Karagiannis, D.; Basdekis, G. The Effect of Whole-Body Cryostimulation in Healthy Adults : Whole-Body Cryostimulation According to Gender and Smoking Status. Adv Exp Med Biol 2021, 1337, 315–321. [Google Scholar] [CrossRef]
- Cerfoglio, S.; Capodaglio, P.; Rossi, P.; Verme, F.; Boldini, G.; Cvetkova, V.; Galli, M.; Cimolin, V. Inertialbased Six-Minute Walking Test Assessment in Post-Covid Patients: Preliminary Results. In Proceedings of the EUROCON 2023 - 20th International Conference on Smart Technologies, Proceedings, Torino, 6 July 2023through 8 July 2023, 2023; pp. 520 - 524.
- Tabisz, H.; Modlinska, A.; Kujawski, S.; Slomko, J.; Zalewski, P. Whole-body cryotherapy as a treatment for chronic medical conditions? Br Med Bull 2023, 146, 43–72. [Google Scholar] [CrossRef]
- Pilch, W.; Piotrowska, A.; Wyrostek, J.; Czerwinska-Ledwig, O.; Ziemann, E.; Antosiewicz, J.; Zasada, M.; Kulesa-Mrowiecka, M.; Zychowska, M. Different Changes in Adipokines, Lipid Profile, and TNF-Alpha Levels between 10 and 20 Whole Body Cryostimulation Sessions in Individuals with I and II Degrees of Obesity. Biomedicines 2022, 10. [Google Scholar] [CrossRef]
- Alito, A.; Quartarone, A.; Leonardi, G.; Tisano, A.; Bruschetta, A.; Cucinotta, F.; Milardi, D.; Portaro, S. Brown adipose tissue human biomarkers: Which one fits best? A narrative review. Medicine (Baltimore) 2022, 101, e32181. [Google Scholar] [CrossRef]
- Hanssen, M.J.; van der Lans, A.A.; Brans, B.; Hoeks, J.; Jardon, K.M.; Schaart, G.; Mottaghy, F.M.; Schrauwen, P.; van Marken Lichtenbelt, W.D. Short-term Cold Acclimation Recruits Brown Adipose Tissue in Obese Humans. Diabetes 2016, 65, 1179–1189. [Google Scholar] [CrossRef]
- Wiecek, M.; Szymura, J.; Sproull, J.; Szygula, Z. Whole-Body Cryotherapy Is an Effective Method of Reducing Abdominal Obesity in Menopausal Women with Metabolic Syndrome. J Clin Med 2020, 9. [Google Scholar] [CrossRef]
- Capodaglio, P.; Cremascoli, R.; Pitera, P.; Fontana, J.M. Whole-Body Cryostimulation: A Rehabilitation Booster. J Rehabil Med Clin Commun 2022, 5, 2810. [Google Scholar] [CrossRef]
- Verme, F.; Scarpa, A.; Varallo, G.; Pitera, P.; Capodaglio, P.; Fontana, J.M. Effects of Whole-Body Cryostimulation on Pain Management and Disease Activity in Active Rheumatic Polymyalgia: A Case-Report. Biomedicines 2023, 11. [Google Scholar] [CrossRef]
- Allendes, F.J.; Diaz, H.S.; Ortiz, F.C.; Marcus, N.J.; Quintanilla, R.; Inestrosa, N.C.; Del Rio, R. Cardiovascular and autonomic dysfunction in long-COVID syndrome and the potential role of non-invasive therapeutic strategies on cardiovascular outcomes. Front Med (Lausanne) 2022, 9, 1095249. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med (Lond) 2021, 21, e63–e67. [Google Scholar] [CrossRef]
- Hausswirth, C.; Schaal, K.; Le Meur, Y.; Bieuzen, F.; Filliard, J.R.; Volondat, M.; Louis, J. Parasympathetic activity and blood catecholamine responses following a single partial-body cryostimulation and a whole-body cryostimulation. PLoS One 2013, 8, e72658. [Google Scholar] [CrossRef]
- Louis, J.; Theurot, D.; Filliard, J.R.; Volondat, M.; Dugue, B.; Dupuy, O. The use of whole-body cryotherapy: time- and dose-response investigation on circulating blood catecholamines and heart rate variability. Eur J Appl Physiol 2020, 120, 1733–1743. [Google Scholar] [CrossRef]
- Zalewski, P.; Bitner, A.; Slomko, J.; Szrajda, J.; Klawe, J.J.; Tafil-Klawe, M.; Newton, J.L. Whole-body cryostimulation increases parasympathetic outflow and decreases core body temperature. J Therm Biol 2014, 45, 75–80. [Google Scholar] [CrossRef]
| Mean | SD | Mean | SD | ||
|---|---|---|---|---|---|
| Age (y) | 55.94 | ±7.50 | CRP (mg/L) | 0.57 | ±0.54 |
| Weight (kg) | 99.83 | ±29.19 | HDL (mg/dL) | 49.37 | ±11.41 |
| BMI (kg/m2) | 37.99 | ±8.44 | LDL (mg/dL) | 130.50 | ±40.94 |
| WC (cm) | 114.40 | ±13.99 | Tot. Col. (mg/dL) | 196.96 | ±49.06 |
| LOS (d) | 30.6 | ±7.69 | TG (mg/dL) | 156.62 | ±51.38 |
| 6MWT (m) | 381.80 | ±145.05 | Glu (mg/dL) | 112.25 | ±40.70 |
| TUG (s) | 12.65 | ±11.65 | SBP (mmHg) | 135.0 | ±19.0 |
| VAS pain | 53.06 | ±26.64 | DBP (mmHg) | 81.3 | ±11.9 |
| PGWBI | 63.50 | ±16.92 | HR (bpm) | 80.0 | ±10.4 |
| T0 | T10 | p-Value | |||
|---|---|---|---|---|---|
| Weight (kg) | 99.83 | ±29.19 | 95.819 | ±27.10 | < .001ᵃ |
| BMI (kg/m2) | 37.99 | ±8.44 | 36.491 | ±7.81 | < .001ᵇ |
| WC (cm) | 114.40 | ±13.99 | 108.800 | ±13.73 | 0.002ᵃ |
| 6MWT (m) | 381.80 | ±145.05 | 446.200 | ±84.56 | 0.093ᵃ |
| TUG (s) | 12.65 | ±11.65 | 9.373 | ±4.67 | 0.009ᵃ |
| VAS pain | 53.06 | ±26.64 | 33.938 | ±18.71 | < .001ᵇ |
| PGWBI | 63.50 | ±16.92 | 76.188 | ±16.59 | 0.002ᵃ |
| CRP (mg/L) | 0.57 | ±0.54 | 0.459 | ±0.41 | 0.013ᵃ |
| HDL (mg/dL) | 49.37 | ±11.41 | 43.688 | ±9.90 | < .001ᵇ |
| LDL (mg/dL) | 130.50 | ±40.94 | 107.563 | ±47.00 | 0.005ᵇ |
| Tot. Col. (mg/dL) | 196.96 | ±49.06 | 176.838 | ±56.51 | 0.013ᵇ |
| TG (mg/dL) | 156.62 | ±51.38 | 147.438 | ±49.77 | 0.473ᵇ |
| Glu (mg/dL) | 112.25 | ±40.70 | 97.563 | ±17.94 | 0.003ᵃ |
| SBP (mmHg) | 135.0 | ±19.0 | 125.625 | ±14.59 | 0.046ᵃ |
| DBP (mmHg) | 81.3 | ±11.9 | 76.250 | ±5.00 | 0.084ᵇ |
| HR (bpm) | 80.0 | ±10.4 | 73.188 | ±5.50 | 0.014ᵇ |
| SpO2 * | 91.5 | ±1.47 | 94.0 | ±2.05 | 0.047ᵇ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





