1. Introduction
Germany, like many EU nations, faces healthcare challenges due to an aging population and increasing multi-morbidity [
1,
2]. As of 2023, a share of 20% Germans are over 65, a number expected to rise by 2050 [
3,
4]. COVID-19 has intensified the demand for health services and spotlighted the lack of nursing staff [
5]. The nursing sector finds it challenging to fulfill the escalating care demands driven by demographic transformations, esp. in rural areas [
6,
7]. Forecasts [
6,
8] predict that by 2023, the nursing gap in Germany will widen to 500,000 nurses. In addition, there is the need to reduce rising health expenditures, which is addressed by governmental plans to cut support staff funding [
9,
10].
The urgency to implement efficient technological solutions that relieve nurses’ burden, save costs, and augment capacities becomes paramount [
11,
12]. Among technical solutions, robots stand out as a promising option, which can support and free up capacity in routine, repetitive, and administrative clinic processes [
12,
13,
14,
15]. Robots can take over routine transportation tasks, such as lab specimens and patient forms, which ties up medical staff and detracts from time devoted to patient care, treatment, and therapy [
16]. Understanding nurse transportation tasks’ current state, in rural clinics, becomes critical in times of nursing shortage. By examining transport tasks’ complexities, time allocation, and requirements, we aim to provide a foundation for future research and develop user-focused solutions to ease staff from such duties in clinical nursing.
Our paper provides the following contributions: We examine the transportation needs of clinical nursing in a rural clinic and how transports are executed. Therefore, we conducted a participatory observational study first between July 3rd and 9th, 2023, and a follow-up observation in another rural clinic between September 4th and 10th, 2023, answering the central question: "Which transportation needs are undertaken by nurses in clinical settings, and what are their time allocations, requirements, and economical implications?" This includes the following sub-questions:
- RQ1
Which items are transported, how often, and in which direction?
- RQ2
How long does it take to move items, and which requirements exist?
- RQ3
Which specific requirements for certain transportation need to be fulfilled?
- RQ4
Do transportation tasks vary between different days, shifts, and locations?
- RQ5
What is the economic perspective on clinical transportation tasks?
Our paper is structured as follows: In
Section 2, we outline literature according to clinic intra-logistics.
Section 3 presents the methodology, and the results are shown in
Section 4. In addition, in
Section 5, we discuss our findings before concluding in
Section 6.
2. Related Work
Research focuses on overall task assessments and less on nurses’ transportation needs.
2.1. Time and Motion Studies
Time and Motion Studies (TMS) aim to optimize industrial processes, with applications emerging in healthcare [
17] According to Klein et al. [
18], TMS can uncover optimization and assist in efficient work systems. Using the German REFA method, which offers precise work and process measurements, we focused on its application in healthcare tasks [
18,
19]. Despite its growth, TMS research in healthcare is limited, often due to small sample sizes and self-reported data [
20,
21]. Westbrook [
22] highlighted the relevance of nurses’ patient interaction for health outcomes and acknowledged the extensive time nurses, spend on non-direct care tasks. Research shows variability in nursing tasks depending on clinic settings, with a significant portion dedicated to transportation tasks, esp. patient transfers [
23,
24,
25]. Lim et al. [
25] state, that 10.5 % of nursing work time is spent on transportation, like patient transfer to diagnostics and the supply of food as well as medicines.
However, nurses are also burdened with myriad tasks, such as documentation, care organization, and administration, which do not involve direct patient care [
22,
26]. The TMS by Michel et al. [
27] states, that less than one-third of nurses’ work time is spent with patients directly. Hendrich et al. [
28] affirm that administrative tasks, particularly documentation, constitute over 27.5 % of nursing work time. Conversely, Roche et al. [
29] challenge these assumptions, contending that nurses spend most of their time assisting service staff and nursing support workers in direct care tasks [
22,
29]. Notably, some clinics lack support staff, leaving nurses with continued responsibility for non-direct patient care tasks [
30]. TMS may vary based on specific clinic settings [
17]. Furthermore, nursing tasks are multifaceted and often involve intra-clinic transfers, such as moving patients for treatments or diagnoses [
24]. These transportation tasks warrant a deeper look, given that Fiedler et al. report that over 7 % of nursing time is dedicated to patient movement and transfer activities [
23]. Fiedler et al. do not account for transport tasks, suggesting that the proportion of daily nursing work spent on transport is higher.
2.2. Transportation Needs
Studies by Fiedler et al. [
23] and Blay et al. [
31], focus on clinical task assessments, with few results about clinical transportation [
30]. Nevertheless, transporting medical goods and patients, are integral to the efficient execution of clinical nursing practices [
12,
32,
33]. As per the studies by Fiedler et al. [
23], Kriner et al. [
34], Ryoo et al. [
35] and Lim et al. [
25] certain categories of goods—namely medical supplies, non-medical equipment, patients, and medical waste are transported more frequently. Moreover, drug distribution is the most time-consuming good, according to Graf et al. [
36] and Ahtiainen et al. [
15]. Furthermore, Hendrich et al. [
28] identified measuring device transportation and waste handling as time-consuming tasks. Rosenberg et al. [
24], Blay et al. [
31], and Roche et al. [
29] underscore the importance of patient transfers, characterizing them as demanding, vital, and time-intensive aspects of nursing. Ryoo et al. [
35] pointed out that manually handled patient transfers occur frequently and may be a health risk.
In conclusion, as depicted in
Table 1, clinical transportation is multifaceted, marked by diverse requirements that complicate the study of transportation needs in clinics [
35]. Existing studies, non-comparable and small populations, present varying results [
22,
24]. Furthermore, the time required for transports between studies varies [
25] Fiedler et al. [
23] affirm the non-repetitive nature of nursing tasks, underscoring daily variability due to varying patient needs. Concurrent schemes, such as patient communication during transportation or interruptions due to unexpected events, further complicate these tasks [
37]. Therefore, more research is warranted to alleviate transportation tasks’ burden and devise effective technical solutions [
38].
3. Methodology
Addressing the research gap and answering the RQs via participatory observation.
3.1. Setting of the Study
We observed clinical nurses’ transportation tasks in two rural clinics of basic-, regular- and emergency care in Lower Bavaria, Germany. The observation was conducted from July 3rd to 9th, 2023, and September 4th to 10th, 2023. The setting consists of
a geriatric nursing unit for the first observation period (30 mostly immobile patients with an average age of 65 mostly in 17 fully occupied rooms, 30 employees in the nursing staff rotating in a three-shift-system, and additionally one station secretary, three nursing trainees, and two interns),
a surgical unit for the second observation (31 patients in 17 rooms capacity, occupied with 12 patients with an average age of 49 years, 28 employees in the nursing staff rotating in a three-shift system, and one station secretary, four nursing trainees).
Both clinics (Arberlandklinik, Viechtach, shortened as VIE, and Kliniken Am Goldenen Steig, Freyung, abbreviated as FRG were typical rural clinics in Germany, having more than 1,000 employees and caring for approximately 40,000 patients annually. From these clinics, we observed the transportation needs of nurses, and other vocational groups like physicians or supporting staff (e.g., cleaning or service staff) were excluded from our study. Furthermore, Night-shift nurses were excluded because the clinic indicated minimal transport tasks during nighttime in the pre-test. The day-shift nurses, forming our study population, were selected by random drawing.
3.2. Data Collection and Annotation
We conducted a
participatory observation over seven days in each rural clinic during typical weeks in July and September 2023, excluding public holidays. Observations covered the early (06:00-13:30) and late (13:30-21:00) shifts from Monday to Sunday. Daily, our observation focused on two daytime nurses in each clinic, rather than the entire ward. The study authors rotated shifts using an Android app with a standardized protocol, as shown in
Table 2, had pre-set categories and allowed free text, for consistent data collection. Emphasis was on accurate timestamps to track when nurses began and ended transport tasks, ensuring precise measurements.
We summarized sub-items, like transportation goods, into functional clusters we identified during pre-tests. In addition, all observers underwent an onboarding, including training, and data collection was supported through a guide and glossary. Furthermore, our app had tooltips as a helping field to explain items to observers.
3.3. Data Pre-Processing and Evaluation
The data was prepared for evaluation, including deleting incomplete values, performing plausibility checks, and transforming, i.e., summarizing necessary variables. To organize the data, we used Python Pandas. The evaluation of times was based on the REFA-Methodology [
39], with some adaptations to our specific needs according to
Table 3. Notably, our measurements began when a nurse initiated a transport action by taking good in the hand and ended once the good was handed over and the transport was completed.
In addition to the descriptive data analysis, we conducted a template analysis of all free-text comments. The free text was filtered and meticulously coded to ensure our findings’ integrity and relevance. After assessing the coded information, it became evident that the comments provided valuable insights, giving us a summarizing overview and a deeper understanding of the data, complementing our quantitative analyses.
4. Results
This section presents the results related to the transportation tasks within the two rural clinics in Germany. These outcomes were derived from a comprehensive participatory observation conducted over two distinct periods within 2023, aiming to shed light on the transportation tasks of clinical nurses during day shifts. Initially, we summarize the transportation needs, the duration, the medium, and the requirements for both clinics.
4.1. Overview of Transported Goods
During each daytime shift, one nurse was observed. 1,830 transports were recorded across both clinics for two weeks. The distribution of transports is shown in
Table 4:
It becomes apparent that clinical nursing involves transporting a diverse range of goods. We’ve grouped these into 10 categories for clarity and ease of interpretation. As illustrated in
Table 4, Non-Medical Supplies emerged as the predominant category, making up nearly a third (27.05 %) of all transported items. Medical Supplies closely trailed this, such as wound dressings, which represented 17.32 % of the overall count. Pharmacotherapy formed another significant portion, amounting to 14.10 %. Further, more specialized categories like medical devices accounted for 12.51 %, and meals or drinks for 12.68 %. Venturing into the less frequent items, which each represented less than 5 % of the total, we observed documents (4.10 %), patient transfer aids (3.99 %), miscellaneous items (4.81 %), patients (2.89 %), and lab samples (0.55 %). It’s worth noting that the distribution of transported goods is inconsistent across rural clinics, Freyung (FRG) and Viechtach (VIE). There are more transportation tasks in the clinic of VIE, esp. since there is more transportation in the category of non-medical supplies, with 338 cases, compared to FRG, with 157 cases. Furthermore, more meals and drinks are transported in FRG as in VIE.
4.2. Frequency of Locations
Table 5 provides insights into the transportation start and endpoints. Six transports were canceled, explaining why the total numbers of start and end locations differ. The primary focus of transport is the corridor, patient rooms, and the station office. With 36.69 % the corridor is the most common starting location. 27.95 % transports started further from the patient room and 25.75 % from the own station office. Other areas, having percentages under 5 %, highlight that transport between places like the kitchen or the storage is less common. When observing the termination points, the patient room dominates with 50.30 % and is followed by the corridor (21.70 %). Furthermore, the station office again emerges as an important location, making up 8.91 % of the end locations. Areas such as the Lounge and various miscellaneous locations, encompassing kiosks, diagnostics areas, and elevators, although constituting smaller percentages, point to specific and specialized transportation needs. In summary, transports focus on the corridor, patient rooms, and the station office.
4.3. Transport Duration Analysis
Another angle of understanding the efficiency and potential bottlenecks in transportation tasks is by assessing the duration taken for transports.
4.3.1. Cumulative Distribution of Total Transport Duration
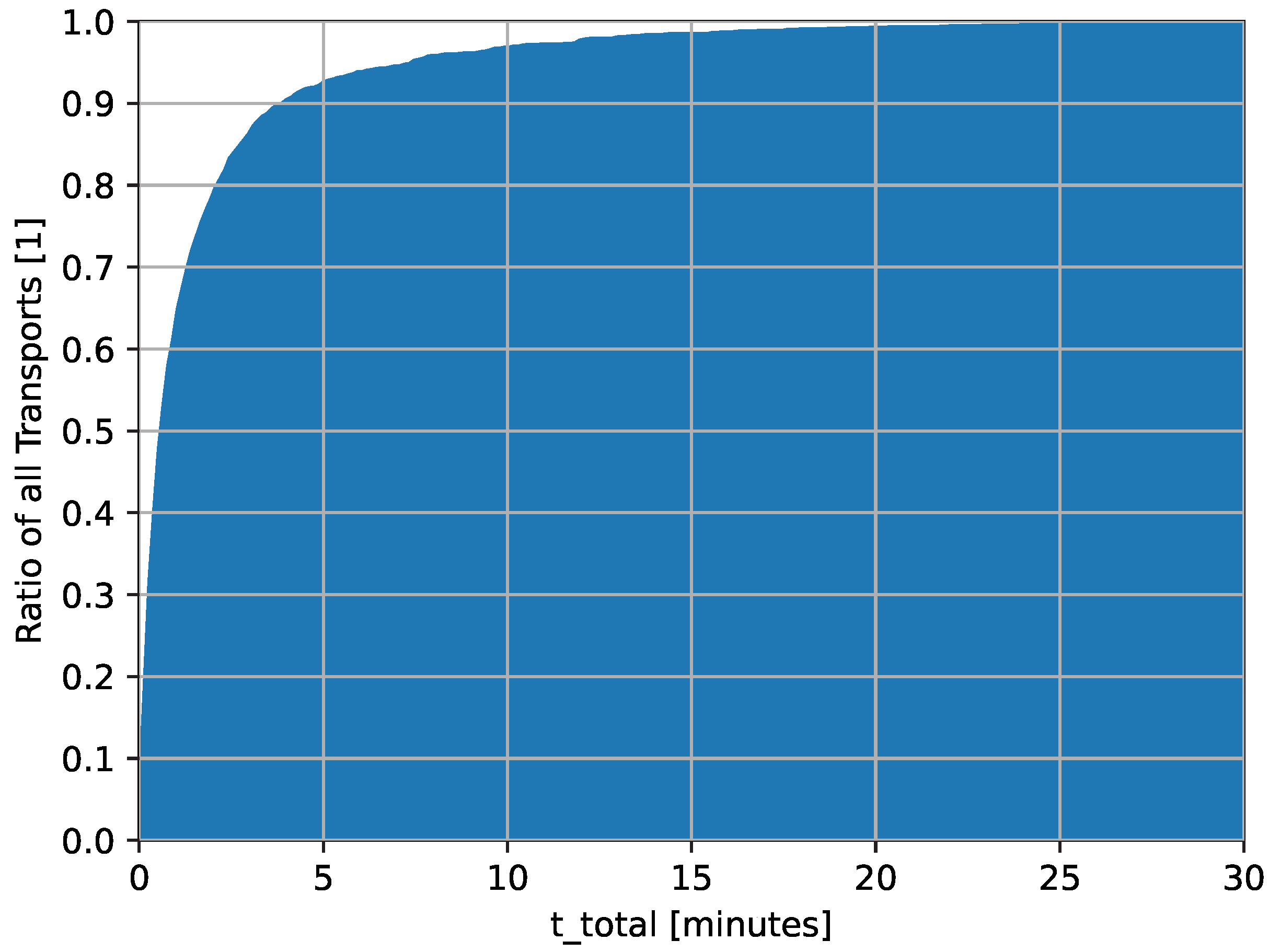
In
Figure 1, the cumulative distribution of total transport duration (
), including all interruptions and needed setup time, is illustrated through a histogram for all transported items. More than 90 % of all transports were completed in under five minutes.
The mean transport duration is 1.82 minutes, with a standard deviation of 3.47 minutes. 1 % of transports finish in 4 seconds, while 10 % complete within 11 seconds and a 25 % within 20 seconds. The median is 0.70 minutes, signifying that half of the transports are concluded under that duration. Notably, even including the interruptions and setups, 90 % of all transports are finished in less than 4.05 minutes. While the majority of transports demonstrate efficiency, some extremes stand out. Specifically, the longest 1 % of transports (p99) reach up to 17.72 minutes. The maximum transport duration duration has extended up to 44.58 minutes. These outliers above p99 highlight the complexity of clinical nursing.
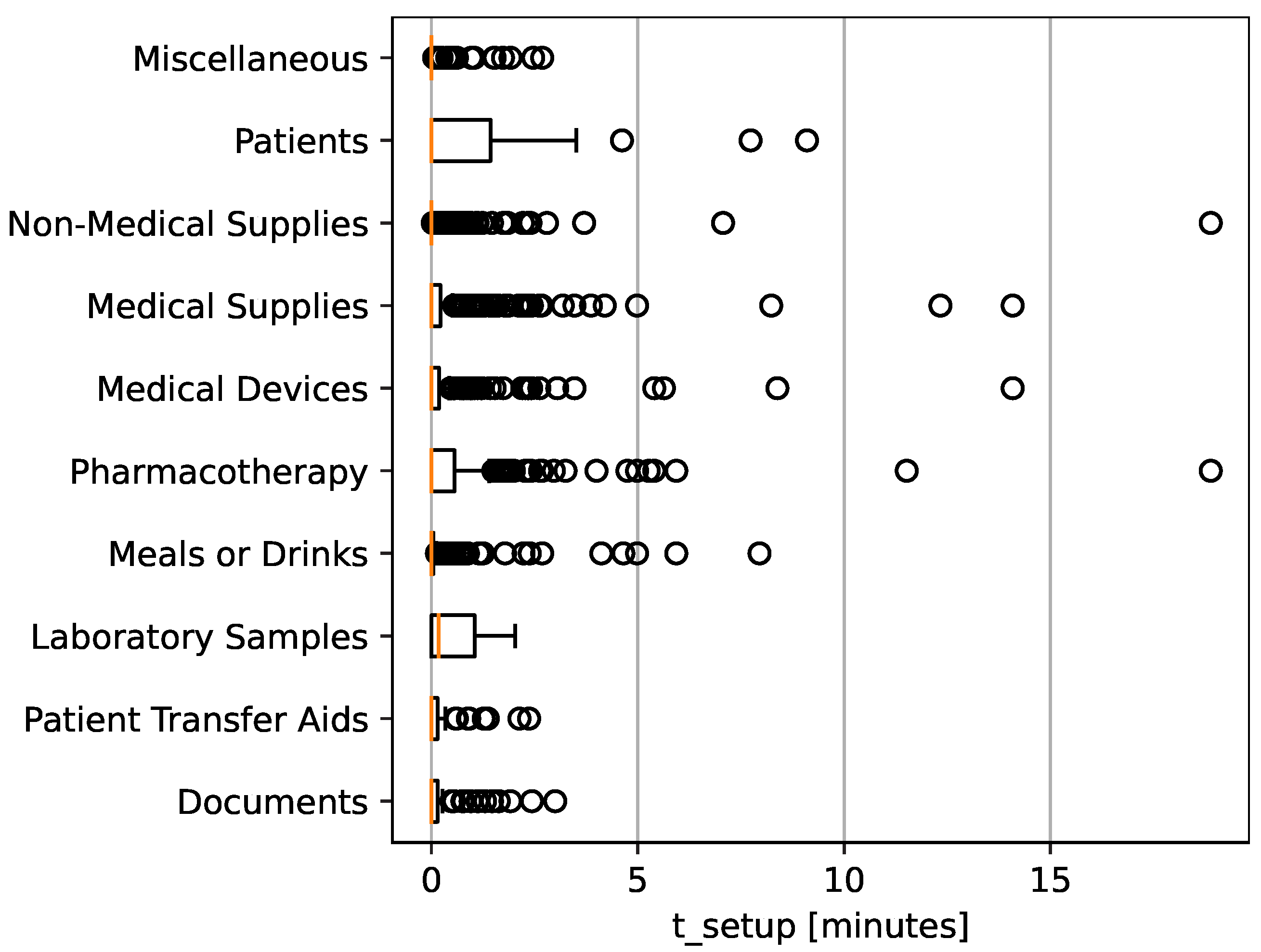
4.3.2. Setup Times
The setup time (
), referring to preparatory steps like disinfecting or turning on a system before and after initiating a transport, averages at 0.31 minutes. While 25 % of the transports (Q1) didn’t require any setup time, 75 % of the transports (Q3) necessitated up to approximately 7 minutes. Many transports require minimal to no setup. The longest observed
was 18.88 minutes. As depicted in
Figure 2, patient transports, pharmacotherapy, and lab sample transports often necessitate preparations.
4.3.3. Interruptions during Transports
Analyzing interruptions () during transportation, we find an average of 0.74 minutes with a standard deviation of 2.49 minutes. Most transports are efficient: up to the median, meaning no interruptions exist. By Q3 (75 %), rises to 0.25 minutes. However, extreme cases exist, with the most extended interruption being 35.17 minutes. Such delays beyond the 99th percentile, highlight challenges in clinical nursing’s transportation, such as emergencies or equipment issues.
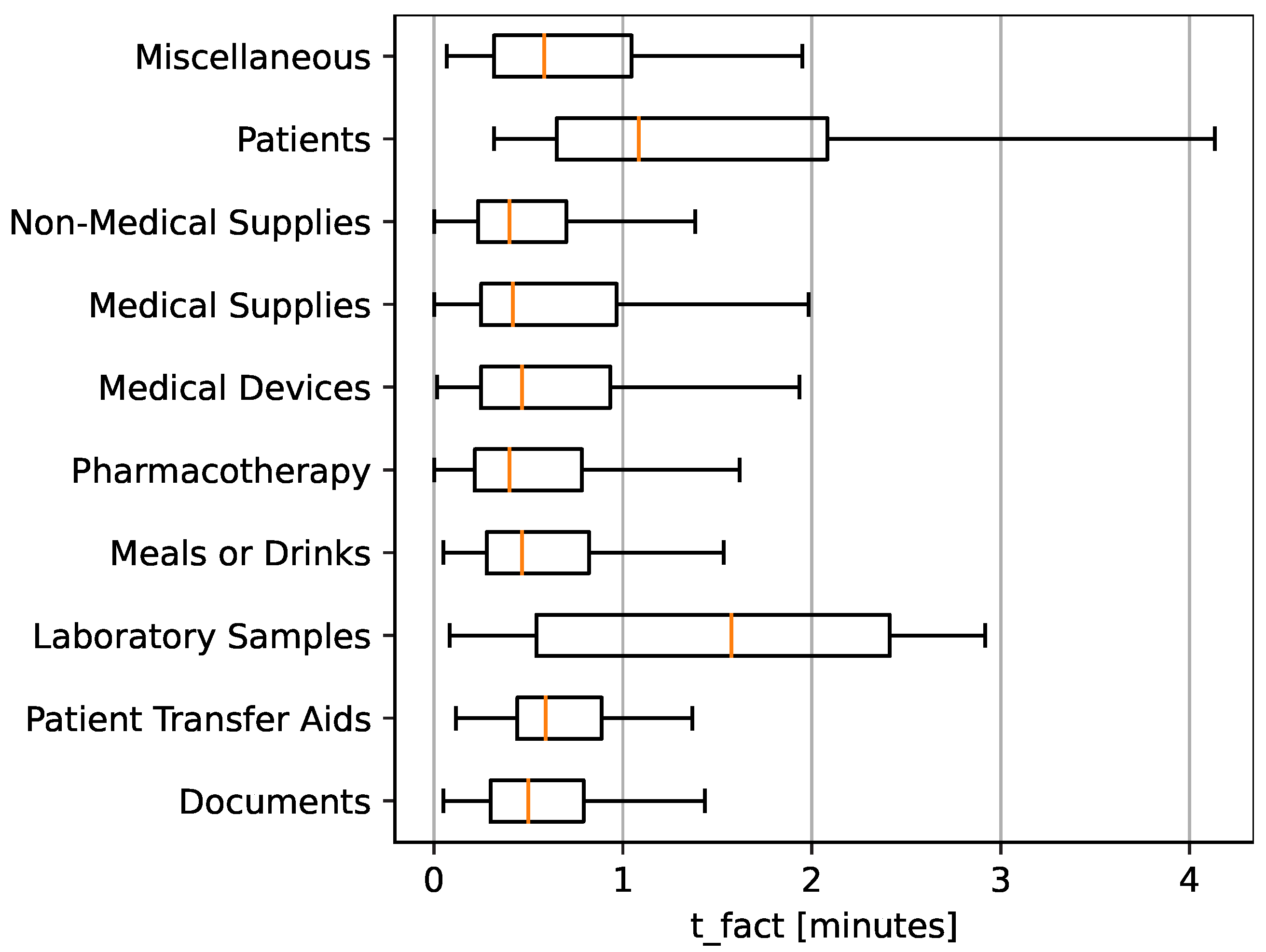
4.3.4. Transported Goods and their Factual Transport Time
The factual transport time (
), the time without any interruptions and set-up, is important for understanding transportation efficiency.
Figure 3 showcases a box plot.
Patient transport and lab samples stand out among the items shown in the boxplot. Not only do they have a higher median factual transport time compared to other items, but they also exhibit a broader range in their distribution. This suggests that these two categories face more variability in transportation time. The extended duration for patient transport could be attributed to the inherent complexity and care required in moving patients. Similarly, transporting lab samples might involve specific protocols or detours, leading to longer transportation times. The median factual transport time () for most transported goods, including non-medical supplies, medical supplies, medical devices, pharmaceuticals, meals or drinks, patient transfer aids, and documents, falls under a minute. Moreover, even their interquartile ranges (Q1 to Q3) suggest a tight distribution, mainly concentrated within this under one-minute duration.
Contrastingly, patient transfers and lab samples stand out in the box plot. While predominantly registering under a one-and-a-half minute for their median times, these two categories have a notably wider spread in their box plot. Furthermore, the whiskers are wider, esp. in patient transport, indicating greater variability in . Specifically, up to the Q3, patient and lab transports exhibit times ranging between two and three minutes.
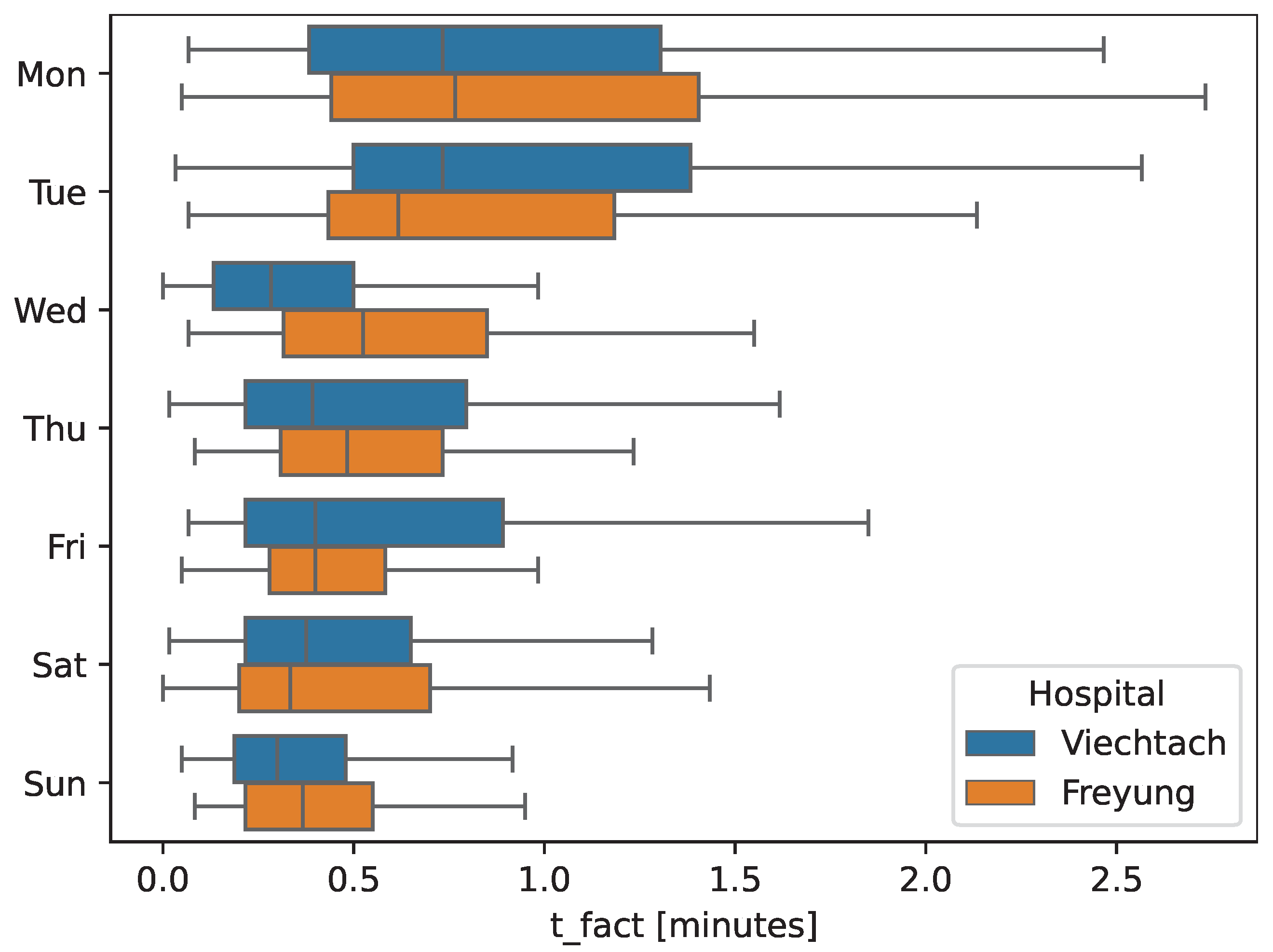
4.4. Transport Duration’s over a Week
As demonstrated in
Figure 4, there’s consistency in the distribution of transports throughout the week. There isn’t any particular day where apparent anomalies occur regarding transport duration or frequency. Whether on weekdays or weekends, the transportation workflow maintains a steady pace throughout the observation period. At the beginning of the week, the duration and outliers in
are more comprehensive.
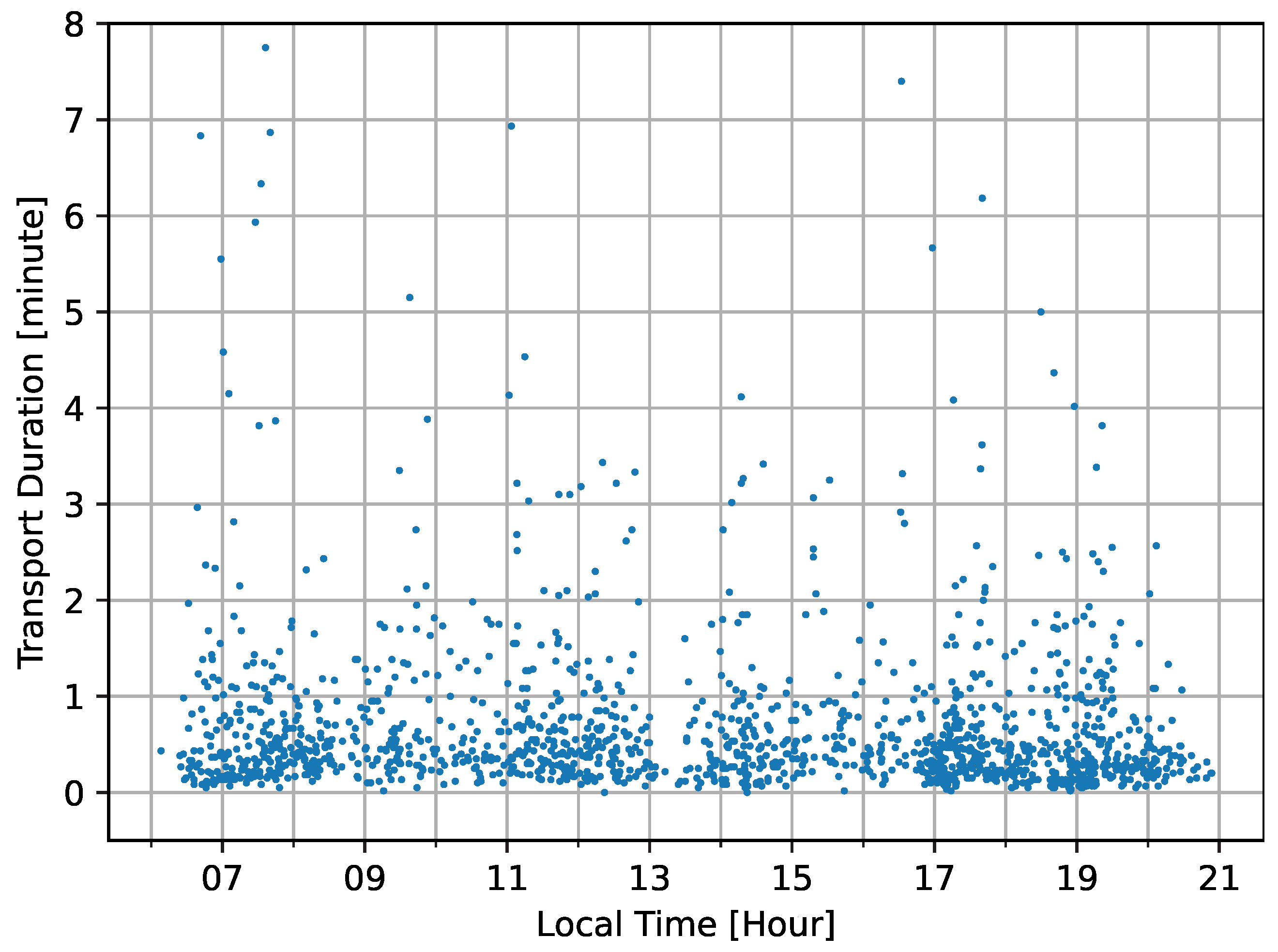
Delving into daily trends,
Figure 5 shows the spread of transports throughout the day. The data doesn’t present any sharp spikes or troughs at specific hours. However, a mild surge in transport can be observed during the early morning hours between seven and eight o’clock and again in the late afternoon, from 6.30 to 8 a.m. These could be times when routine medical activities or shift changes necessitate more movement. Furthermore, another slight surge is in the late afternoon, from 5 to 7 p.m., which can be related to dinner. Apart from these periods, the transports are evenly distributed.
4.5. Share of Transport Mediums
Our analysis shows variations in the transport mediums across the clinics (
Table 6). The most prevalent medium was ’By Hand,’ accounting for 77.15 % of all transports. Other transport mediums followed, including the Nursing Trolley (13.06 %) and Tray (11.73 %). Wheelchairs, beds, cardboard, and others constituted less than 7 % combined.
As most items were transported by hand (77.15 %), a detailed examination of this category sheds light on the nature of items and reasons for this preference. The most frequently hand-carried items were Non-Medical Supplies, with 328 cases (28.32 %), and Medical Supplies at 263 cases (22.71 %). Pharmacotherapy items were also prominently hand-carried, totaling 226 cases (19.52 %). Meals or drinks and medical devices made up 160 (13.82 %) and 156 (13.47 %) cases, respectively. Less frequent hand-carried items included documents with 70 cases (6.05 %), Miscellaneous items at 62 (5.35 %), and patient transfer aids at 35 (3.02 %). In 17 instances (1.47 %), patients were "hand-carried" in the sense of being taken by the hand and led to their destinations. Lab samples were the least transported by hand, tallying at seven cases (0.60 %).
4.6. Transportation Requirements
In 1,291 (79.25 %) of all transports, no specific requirements were noted. Collection was necessary in 4.73 % of cases, while 4.30 % needed nursing supervision during transport. Disinfection and observation of medication intake were required in 2.89 % and 2.82 % of transports, respectively. In 2.15 %, patients needed general help taking drugs, food, or mobilization during transports. Bio-hazard precautions or isolation were needed in 1.41 %. Less than 1 % of the transports had other requirements, such as safety, weight considerations, urgency, labeling, elevator use, and temperature control.
4.7. Differences between the Clinics: Geriatric (VIE) vs. Surgery Unit (FRG)
Table 7 contrasts the top transported goods in each clinic. Viechtach (VIE) features a geriatric unit, whereas Freyung (FRG) operates a surgery unit, impacting transportation and patient mobility. Notably, FRG’s surgical unit sees more patient transports due to more frequent examinations. FRG’s geriatric unit transported fewer non-medical supplies (19.50 %) compared to VIE’s 32.98 %. Conversely, FRG had more meals or drinks transports (20.87 %) versus VIE’s 6.24 %. Patient transports were more frequent in VIE (3.90 %) than in FRG (1.61 %). Moreover, lab transports were exclusive to VIE.
In addition, FRG has prolonged interruptions than VIE, but VIE has extended setup times. Average transport duration is closely matched, but VIE displays a broader duration range. At the median for
, FRG’s transports are 0.47 minutes, slightly longer than VIE’s 0.42 minutes. Detailed time breakdowns are available in the Appendix and
Figure 4.
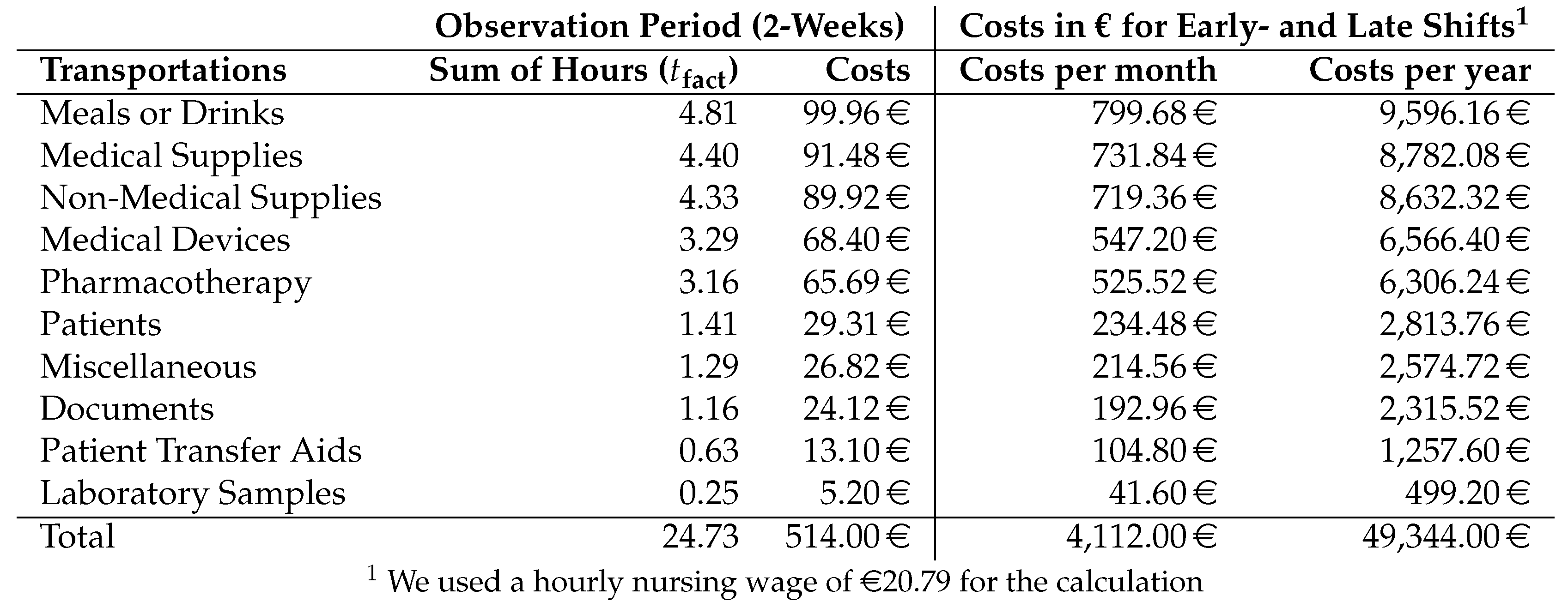
4.8. Transportation Cost Analysis
Using the direct transport time,
, which omits setup and interruption times, we analyzed the costs over a two-week observation period in two clinics, focusing on two nurses per daytime shift. As depicted in
Table 8, these observations revealed a total transportation cost of 514, corresponding to 24.73 hours of work. It’s worth noting that for the calculation, the hourly rate of 20.79 was derived from the German collective agreement TVÖD-P, which sets a nurse’s gross wage at 3,532, inclusive of 600 for additional employer costs such as social insurance. Our data, comprehensive for the day and late shifts with typically four nurses each, doesn’t cover the night shift.
A portion of transport costs is attributed to the transport of ’meals or drinks’, taking up 4.81 hours and accounting for approximately 99.96 during the observation period. Given the clinic’s staffing structure, with an average of four nurses operational during each daytime shift, this translates to a monthly transport cost of 799.68 solely for meals or drinks on the observed stations. When projected over a year, this single task accumulates to an annual expense of around 9,596.16 across both clinics.
5. Discussion
This section situates our methods and results in the context of current nursing TMS.
5.1. Method Discussion:
Our participatory observation method is not without potential bias. While we spotlighted clinical nurses, driven by their higher wages and staffing deficits, our lens did not capture the service support staff, who, in reality, might be significantly involved in transport tasks. Moreover, the inherent risk of observational studies persists: participants might subconsciously modify their behaviors when under observation [
40]. The involvement of several observers can exacerbate this risk. Proactively, we employed random participant selection and harnessed a standardized app-driven data collection approach to counterbalance potential biases. Furthermore, our methodology incorporated the REFA-Methodology [
39], initially designed for production environments. While it sharpened our time measurements, its limitations might not perfectly align with modern healthcare dynamics, given its manufacturing roots and age.
The validity and generalizability of our findings are limited by our study’s specific settings and short duration [
41]. For example, FRG’s unique attributes, such as lower patient occupancy and the notable involvement of interns, affected our results. Although we aimed to capture a typical clinical week, external factors, like student intern presence and clinic-specific processes, played a role. Such factors make it challenging to generalize our findings, suggesting the need for further research in diverse settings.
Still, our study offers cost-effective and tangible insights, addressing our RQs. We examine rural clinical transportation challenges and hint at innovations like transport robots, marking a path for further research in healthcare transportation.
5.2. Result Discussion:
Nursing research underscores the gaps in understanding intra-clinic transports [
20,
30]. Our study contributes to this domain by focusing on the transportation handled by clinical nurses, determining their time allocations, requirements, and economic implications.
5.2.1. Transportation Tasks and Durations
Our findings corroborate with prior research, identifying various clinical transport tasks, including medical supplies, non-medical equipment, patients, and medical waste [
23,
34,
35]. We’ve further identified transport categories, such as distributing food and drinks, which aren’t widely discussed in the existing literature. Transportations like patient transfers, likely due to their inherent complexity, consume more time in our study, aligning with the insights of Rosenberg et al. [
24], Blay et al. [
31], and Roche et al. [
29].
Data from
Table 4 points out a divergent distribution of transports between our two observed clinics attributed to the unique wards. The dementia ward in VIE, for example, could lead to a high percentage (19.50 %) of non-medical goods transports. This suggests a possibility that patients in VIE might have a higher dependency on nursing staff, necessitating more non-medical item transports. Conversely, the lower percentage in FRG could be due to its patients being more independent. These disparities underline the influence of the clinic’s structure and patient demographics on transportation tasks.
During our two-week study, we observed 24.73 hours for transports for two daytime nurses. According to Lim et al. [
25], approximately 10.5 % of nursing work time is dedicated to transportation tasks, such as transferring patients to diagnostics and supplying food and medicines. Our data indicates that nurses working 39 hours per week spend 15.85% of their work time on observed transportation tasks, which is more than Lim et al. [
25] reports. Expanding on durations, our study offers a distinct perspective influenced by the REFA methodology, which differentiates between different time components. We highlight the specific durations but abstain from evaluating their efficiency or wasted potential. In summary, our findings resonate with observations on the time-intensive nature of drug distribution [
15,
36]. Furthermore, Hendrich et al. identified medical device transports and waste management as time-consuming, which we can`t confirm in detail for waste management because of missing subcategorization [
28]. Moreover, our observed time intensities for patient transfers, align with reports of their inherent complexity from Rosenberg et al. [
24], Blay et al. [
31], and Roche et al. [
29]. Additionally, we identified other time-consuming transports, like food and drinks, which haven’t been discussed prior.
Figure 5 exhibit rhythmic patterns in transport activities, possibly tied to daily routines, like the checks and meal times. We found a slight surge in transport between 6:30 and 8 a.m. and 5 to 7 p.m., but apart from these peak hours, the consistent spread of transport events suggests a balanced demand for transport services throughout the day and the week. This might reflect an efficient scheduling and resource allocation mechanism within the clinics.
5.2.2. Mediums and Requirements
Table 6 highlights a reliance on manual transport linked to potential physical strain [
35]. Our data lacks specifics like item weight, which influences transport time [
35]. Moreover, similar to Westbrook et al. and Peter et al.’s findings, under 5 % of all transport tasks involve direct patient interactions, additional care or collection of items [
22,
30]. In summary, using robots for transport might also reduce physical strain for nurses, and also has hardly any special requirements in most cases.
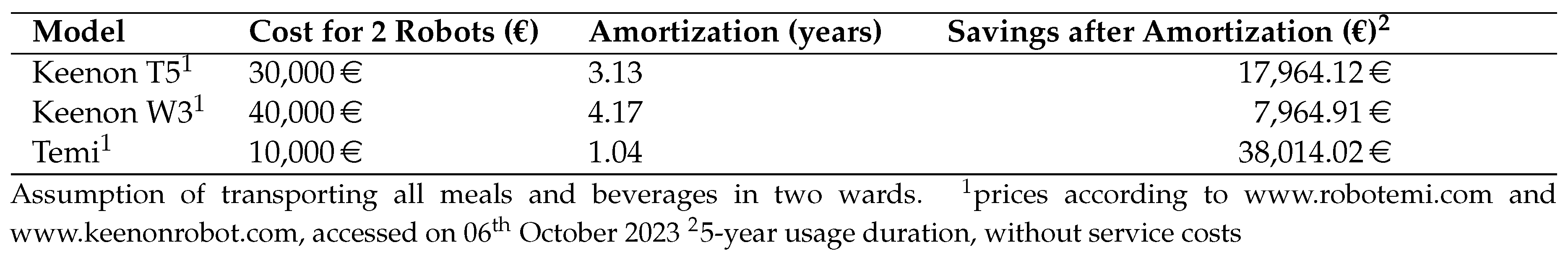
5.2.3. Economical Implications and Robot Potential
Clinic transports impose economic consequences, corroborated by our study and Fiedler et al. [
23]. Our economic analysis is based on actual transport duration, accommodating factors such as disinfection and navigational challenges pertinent to robots.
Table 9 shows potential amortization, focusing on automating meal and beverage transports.
Utilizing cost-effective robots like Temi, priced at 5,000, the investment can be recouped within a year. Projecting further, we calculated the costs for 5 years, presuming the robots’ operational lifespan adheres to German depreciation guidelines. However, research should continue to explore the durability of robots in clinics, adjusting calculations as needed for aspects such as repairs and maintenance.
While our calculations provide a directional guideline, we hinge on the assumption of achieving full automation for meal and beverage transports. Our presumption might be overly simplified. Broadening the scope of robot tasks to encompass additional items or span various wards could enhance operational efficiencies but also necessitates comprehensive research. Considering various robots’ unique capabilities, limitations, and applications in clinical contexts leads to further research needs [
13].
6. Conclusions
Transportation is a time-consuming and common task in nursing. Our research reveals that non-medical items, medical supplies, pharmacotherapy, meals, and drinks were the most transported goods. Considering the costs, esp. transporting meals and drinks lead to the main charges, because of the longer duration of these transports. According to the locations, the corridor, patient rooms, and station offices emerged as crucial transportation nodes, which implies that these are areas to support nurses with robotic technologies. In addition, 77.15 % of transport activities were conducted manually, which is a burden for the clinical nurses. Moreover, the transports are short, meaning nurses must run often for short distances. We measured that the factual transport time for most items was under a minute, with patient transport and lab samples showing more variability.
We advocate for the widespread adoption of cost-effective robots to handle routine transportation tasks in healthcare settings, easing nurses’ workload. Through discussions with robot manufacturers, we’ve identified a primary focus on food transportation, representing a significant cost factor in our research. Clinics like LMU Munich already employ service robots for food and beverage delivery [
14]. Rural clinics should also explore the practical use of robots to enhance their operations. However, it is essential to research robots’ feasibility, practicality, longevity, return on investment, and user acceptance to ensure the successful integration of transport robots into healthcare facilities. We recommend initiating intervention studies within clinics to investigate how robots can efficiently transport food and beverages while identifying limitations.
Author Contributions
Conceptualization, D.S., D.J.; Methodology, D.S.; Software, S.F. (android development), K.T. (app testing); Validation, D.S.; Formal Analysis, D.S, J.K. (J.K. esp. for data handling and evaluation); Investigation, D.S., D.J., S.S.; Data Curation, D.S., J.K.; Writing – Original Draft Preparation, D.S.; Writing – Review and Editing, D.S., and F.W.; Visualization, D.S.; Supervision and Resources, F.W.; Administration, S.S.
Funding
The German Federal Ministry for Digital and Transport funded this research under grant number 45FGU120.
Institutional Review Board Statement
Following a self-assessment, in accordance with the Association of the Bavarian Universities of Applied Sciences (UAS) standards, our research design ensured no potential harm to participants, thus waiving the need for further ethical approval.
Informed Consent Statement
Informed consent was obtained from all subjects in the study.
Acknowledgments
We would like to thank the clinics for their support and in-person Tobias Greiler, Stefan Fischer, and Kevin Thaller for their help in programming an executing the data collection.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| UC |
Use-Case |
Q1 |
First Quartile |
| Q3 |
Third Quartile |
TMS |
Time and Motion Studies |
| VIE |
Clinic Viechtach |
FRG |
Clinic Freyung |
| pt. |
part |
esp. |
esp. |
References
- Jacobs, K.; Kuhlmey, A.; Greß, S.; Klauber, J.; Schwinger, A. (Eds.) Pflege-Report 2020 [Nursing Report 2020]; Springer Berlin Heidelberg: Berlin, Heidelberg, 2020. [Google Scholar] [CrossRef]
- Parliament, E. Demographic outlook for the european union 2022: Think Tank, 2022.
- Dudel, C. Demografie [Demography]. In Handbuch Staat [Handbook of the State]; Voigt, R., Ed.; Handbuch [Handbook], Springer VS: Wiesbaden, Germany, 2018; pp. 7–15. [Google Scholar]
- Achter Altersbericht: Ältere Menschen und Digitalisierung: Drucksache 19/21650 [Eighth Aging Report: Older People and Digitalization], 2022.
- Hinterbuchner, K.; Zuschnegg, J.; Lirussi, R.; Windhaber, T.; Archan, T.; Kadric, I. Geringe Attraktivität des Pflegeberufs bei Auszubildenden: COVID 19 hat die Belastungen verschärft [Low Attractiveness of the Nursing Profession Among Apprentices: COVID-19 Has Exacerbated the Challenges]. ProCare 2021, 26, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Isfort, M. Monitoring Pflegepersonalbedarf Bayern 2020 [Monitoring Nursing Staff Demand in Bavaria 2020], 2021.
- Bundesamt, S. Beschäftigte nach Berufsgruppen 2022 [Employees by Occupational Groups 2022], 2023.
- Radtke, R. Fachkräftemangel - Bedarf an Pflegekräften in Deutschland bis 2035: Prognostizierter Bedarf an Stationären und Ambulanten Pflegekräften* in Deutschland bis zum Jahr 2035 [Skilled Labor Shortage - Demand for Nursing Staff in Germany Until 2035: Projected Demand for Inpatient and Outpatient Nursing Staff* in Germany Until the Year 2035], 2020.
- Blachny, M. Pressemitteilung: DKG zum GKV-Finanzstabilisierungsgesetz [Press Release: German Hospital Federation on the Health Insurance Fund Financial Stabilization Act], 2022.
- Health spending, 2017. [CrossRef]
- Gimpel, H.; Schröder, J.; Baier, M.S.; Heger, S.; Hufnagl, C.; Kriner, H.; Wöhl, M. Das Krankenhaus im Wandel – Herausforderungen und Chancen in der Krankenhauslogistik [The Hospital in Transition – Challenges and Opportunities in Hospital Logistics]. In Hospital 4.0; Springer Gabler: Wiesbaden, Germany; pp. 1–19. [CrossRef]
- Köppen, J.; Busse, R. Die Personalsituation im Krankenhaus im internationalen Vergleich [The Staffing Situation in Hospitals in International Comparison]. In Krankenhaus-Report 2023 [Hospital Report 2023]; Klauber, J., Wasem, J., Beivers, A., Mostert, C., Eds.; Springer Berlin Heidelberg: Berlin, Heidelberg, 2023; pp. 19–32. [Google Scholar] [CrossRef]
- Misaros, M.; Stan, O.P.; Donca, I.C.; Miclea, L.C. Autonomous Robots for Services—State of the Art, Challenges, and Research Areas. Sensors 2023, 23, 4962. [Google Scholar] [CrossRef] [PubMed]
- Ohneberg, C.; Stöbich, N.; Warmbein, A.; Rathgeber, I.; Mehler-Klamt, A.C.; Fischer, U.; Eberl, I. Assistive robotic systems in nursing care: a scoping review. BMC Nursing 2023, 22. [Google Scholar] [CrossRef]
- Ahtiainen, H.K.; Kallio, M.M.; Airaksinen, M.; Holmström, A.R. Safety, time and cost evaluation of automated and semi-automated drug distribution systems in hospitals: a systematic review. European journal of hospital pharmacy: Science and practice 2020, 27, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Koczula, G.; Schultz, C.; Gövercin, M. Die Rolle von technologiebasierten Assistenzsystemen bei der ganzheitlichen Versorgung pflegebedürftiger Patienten – Herausforderungen einer flächendeckenden Implementierung [The Role of Technology-Based Assistance Systems in Comprehensive Care for Dependent Patients - Challenges of Widespread Implementation]. In Technologiegestützte Dienstleistungsinnovation in der Gesundheitswirtschaft [Technology-Supported Service Innovation in the Healthcare Industry]; Shire, K.A., Leimeister, J.M., Eds.; Gabler Verlag: Wiesbaden, 2012; pp. 31–55. [Google Scholar] [CrossRef]
- Frey, S.M.; Méan, M.; Garnier, A.; Castioni, J.; Wenger, N.; Egloff, M.; Marques-Vidal, P.; Beer, J.H. Inter-hospital comparison of working time allocation among internal medicine residents using time-motion observations: an innovative benchmarking tool. BMJ Open 2020, 10, e033021. [Google Scholar] [CrossRef] [PubMed]
- Klein, H.H. Arbeitszeitermittlung nach REFA [Work Time Determination According to REFA]. In Fertigung und Betrieb [Production and Operations]; Springer Berlin Heidelberg, 1975; pp. 115–126. [CrossRef]
- REFA-Lexikon: Industrial Engineering und Arbeitsorganisation [REFA Lexicon: Industrial Engineering and Work Organization], 2011.
- Lopetegui, M.; Yen, P.Y.; Lai, A.; Jeffries, J.; Embi, P.; Payne, P. Time motion studies in healthcare: What are we talking about? Journal of Biomedical Informatics 2014, 49, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Kalne, P.S.; Mehendale, A.M. The Purpose of Time-Motion Studies (TMSs) in Healthcare: A Literature Review. Cureus 2022. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Duffield, C.; Li, L.; Creswick, N.J. How much time do nurses have for patients? a longitudinal study quantifying hospital nurses’ patterns of task time distribution and interactions with health professionals. BMC Health Services Research 2011, 11. [Google Scholar] [CrossRef]
- Fiedler, K.M.; Weir, P.L.; van Wyk, P.M.; Andrews, D.M. Analyzing what nurses do during work in a hospital setting: a feasibility study using video. Work (Reading, Mass.) 2012, 43, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.; Britton, M.C.; Feder, S.; Minges, K.; Hodshon, B.; Chaudhry, S.I.; Jenq, G.Y.; Emerson, B.L. A taxonomy and cultural analysis of intra-hospital patient transfers. Research in Nursing & Health 2018, 41, 378–388. [Google Scholar] [CrossRef]
- Lim, M.L.; Ang, S.Y. A time–motion observation study to measure and analyse clinical nursing workload in an acute care hospital in Singapore. Proceedings of Singapore Healthcare 2019, 28, 124–128. [Google Scholar] [CrossRef]
- Al-Moteri, M.; Alzahrani, A.A.; Althobiti, E.S.; Plummer, V.; Sahrah, A.Z.; Alkhaldi, M.J.; Rajab, E.F.; Alsalmi, A.R.; Abdullah, M.E.; Abduelazeez, A.E.A.; zel M. Caslangen, M.; Ismail, M.G.; Alqurashi, T.A. The Road to Developing Standard Time for Efficient Nursing Care: A Time and Motion Analysis. Healthcare 2023, 11, 2216. [Google Scholar] [CrossRef] [PubMed]
- Michel, O.; Manjon, A.J.G.; Pasquier, J.; Bucher, C.O. How do nurses spend their time? A time and motion analysis of nursing activities in an internal medicine unit. Journal of Advanced Nursing 2021, 77, 4459–4470. [Google Scholar] [CrossRef] [PubMed]
- Hendrich, A.; Chow, M.P.; Skierczynski, B.A.; Lu, Z. A 36-Hospital Time and Motion Study: How Do Medical-Surgical Nurses Spend Their Time? The Permanente Journal 2008, 12, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Roche, M.A.; Friedman, S.; Duffield, C.; Twigg, D.E.; Cook, R. A comparison of nursing tasks undertaken by regulated nurses and nursing support workers: a work sampling study. Journal of advanced nursing 2017, 73, 1421–1432. [Google Scholar] [CrossRef] [PubMed]
- Abbey, M.P. Understanding the Work of Intensive Care Nurses: a Time and Motion Study. Theses - Higher Degree by Research 2009. [CrossRef]
- Blay, N.; Roche, M.A.; Duffield, C.; Gallagher, R. Intrahospital transfers and the impact on nursing workload. Journal of clinical nursing 2017, 26, 4822–4829. [Google Scholar] [CrossRef] [PubMed]
- Heuer, T.; Schiering, I. Einsatz von Robotik als Assistive Technologie [The Use of Robotics as Assistive Technology]. In Assistive Technologien im Sozial- und Gesundheitssektor [Assistive Technologies in the Social and Healthcare Sector]; Luthe, E.W., Müller, S.V., Schiering, I., Eds.; Gesundheit. Politik - Gesellschaft - Wirtschaft [Health. Politics - Society - Economy], Springer Fachmedien Wiesbaden: Wiesbaden, 2022; pp. 29–49. [Google Scholar] [CrossRef]
- Fragapane, G.; Hvolby, H.H.; Sgarbossa, F.; Strandhagen, J.O. Autonomous Mobile Robots in Hospital Logistics. In Advances in Production Management Systems. The Path to Digital Transformation and Innovation of Production Management Systems; Lalic, B., Majstorovic, V., Marjanovic, U., von Cieminski, G., Romero, D., Eds.; Springer International Publishing and Imprint Springer: Cham, 2020. [Google Scholar] [CrossRef]
- Kriner, H.; Heger, S. Referenzmodell schlanke, digital-unterstützte Materiallogistik in Krankenhäusern [Reference Model for Lean, Digitally Supported Material Logistics in Hospitals]. In Hospital 4.0; Springer Gabler, Wiesbaden, 2021; pp. 99–161. [CrossRef]
- Ryoo, J.J.; Lee, K.S.; Koo, J.W. A Taxonomy of the Common Tasks and the Development of a Risk Index for Physical Load Assessment in Nursing Job. Safety and health at work 2020, 11, 335–346. [CrossRef]
- Graf, B.; Klein, B. Robotik im Krankenhaus [Robotic in Hospitals]. In Krankenhaus-Report 2023 [Hospital Report 2023]; Springer, Berlin, Heidelberg, 2023; pp. 179–195. [CrossRef]
- Kalisch, B.J.; Aebersold, M. Interruptions and Multitasking in Nursing Care. The Joint Commission Journal on Quality and Patient Safety 2010, 36, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Holland, J.; Kingston, L.; McCarthy, C.; Armstrong, E.; O’Dwyer, P.; Merz, F.; McConnell, M. Service Robots in the Healthcare Sector. Robotics 2021, 10, 47. [Google Scholar] [CrossRef]
- Zimmermann, W. Bewährte Arbeits- und Zeitstudienverfahren im Dienste der Betriebsrationalisierung (Bedaux-System und Refa) [Proven Work and Time Study Procedures in the Service of Operational Rationalization (Bedaux System and Refa).]. Die Unternehmung [The Enterprise] 1959, 13, 14–23. [Google Scholar]
- Döring, N. Datenerhebung [Data Collection]. In Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften [Research Methods and Evaluation in the Social and Human Sciences]; Springer Berlin Heidelberg, 2023; pp. 321–570. [CrossRef]
- Hess, A.S.; Abd-Elsayed, A. Observational Studies: Uses and Limitations. In Pain; Springer International Publishing, 2019; pp. 123–125. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).