1. Introduction
At a global level, suicide is a complex public health problem, fundamentally affecting the younger population and responding to multiple biological, psychological, and social causes [
1,
2]. It presents a significant global burden of disease for all societies [
3,
4]. It has been estimated that suicides were responsible for over 700,000 deaths worldwide in 2019 [
5]. This represents approximately 1.3% of all deaths globally, making it the 17th leading cause of death in 2019 [
5]. Furthermore, in 2019 the global age-standardized suicide mortality rate was estimated ref to be 9.0/100000 population with a higher rate in men than women (12.6 in males
vs 5.4 in females) [
4]. Decreasing trends in suicide mortality were observed in most countries across the world. Unfortunately, the mortality of suicide shows an increasing trend in many countries and populations [
4]. Specifically, the North, Central and South America experienced a significant increase in suicide mortality over the past 20 years [
4]. Ilic et all reported that between 2000 and 2019 suicide mortality increased from 3.6/100,000 to 6.2/100,000 in Paraguay.
In Paraguay, although cardiovascular diseases and cancer continue to be the leading causes of death in adults, external causes such as traffic accidents and suicide are becoming more frequent every day and represent a significant burden of premature mortality [
6,
7]. In recent years there has been a linear increase in deaths by suicide, especially among young people in Paraguay, but the characteristics of these events are still unknown [
8]. The methods used for suicide vary according to country, culture, time, and demographic characteristics, such as race, sex, age and rural or urban environment [
9]. The most common suicide methods used in Paraguay was intentional self-inflicted injury by hanging, strangulation, or suffocation (all 67.6%) [
8]. Suicide also presents large geographical and temporal variations according to the countries [
10,
11,
12]. Previous studies have suggested a relationship between suicide rates and other factors such as economic, environmental, and temporal factors such as seasonality [
10,
12,
13]. Unfortunately, epidemiological data in years of potential life lost due to suicide, changes in suicide methods and seasonal patterns over time as well as trends of suicide mortality in different states of Paraguay is scant.
Regrettably, there is a paucity of epidemiological data regarding years of potential life lost owing to suicide, shifts in suicide methods across time periods, seasonal fluctuations, and trends in suicide mortality rates between the various states that comprise Paraguay. While understanding the dynamics behind suicide completion at a granular level could help direct preventative efforts, limitations currently exist as to the availability and breadth of relevant statistics. It is hoped that public health authorities may seek to bolster record-keeping and analytical efforts going forward, to build a more comprehensive picture of how this tragic act impacts the population in terms of factors like demographics, geography, and temporality. With a more robust evidence base, stakeholders could potentially devise time- and location-sensitive countermeasures to reduce suicide rates in a targeted manner.
The objective of this study was to describe changes suicide mortality, suicide methods and years of potential life lost during 2005 and 2019 in Paraguay. An understanding of changes over time is important to guide public health professionals in developing, implementing, and monitoring public policies to decrease suicide attempts and suicide mortality.
2. Material and methods
2.1. Study design and data
A descriptive, observational study was conducted using validated records from the General Directorate of Strategic Health Information of the Paraguayan Ministry of Public Health and Social Welfare. This institution is officially responsible for collating national health and disease statistics within Paraguay. The records accessed spanned the period from 2005 to 2019. Data was sourced directly from the validated records held by the General Directorate, being the government body statutorily tasked with the collection and maintenance of healthcare and morbidity data at a nationwide level in Paraguay. To define all cases of death by suicide occurring in Paraguay across the study period, the International Classification of Diseases 10th Revision (ICD-10) codes X60 through X84 were referenced. These numerical codes within the ICD-10 classification system specifically relate to and encompass intentional self-harm, also known as suicide. By limiting the analysis to only those records coded as such, the researchers were able to accurately identify and extract all instances of completed suicide recorded in Paraguay between 2005 and 2019 inclusive.
2.2. Measures of suicide mortality and characteristics
The data collected from death certificates and utilized in this research included several key variables. Demographic information such as the age and sex of the deceased was recorded, with sex categorized as either male or female. Additional details pertaining to the date of death and level of attained education provided important context. The primary cause of mortality was also documented. The state of residence of the individual prior to their passing was noted, as was the location where the suicide took place. Whether this was within the place of residence or elsewhere was distinguished. The geographic area where the person resided was specified. Finally, the specific means by which the victim ended their life, or their suicide method, was identified. This suite of variables from official documentation served to facilitate insightful analysis of trends within the departed population. Age was categorized into the following age groups: (i) <10 years, (ii) 10-14 years-old, (iii) 15-24 years-old, (iv), 25-44 years-old, (v)45-64 years-old) and (vi) ≥ 65 years-old. Educational level was divided into none, primary, high school, College/University and unknown. Suicide method was defined according to ICD-10 codes and were as follows: poisoning (X60-X69), ICD-10 strangulation (X70), ICD-10 drowning (X71), ICD-10 firearm firing (X72-X74) and other ICD-10 (X76-X84). Information on the event site was defined as at home, at health-care institutions, public location/area, and others. The last recorded residence of the suicide victim was dichotomized into rural versus urban. The season of the suicide occurrence was recorded as spring/summer and autumn/winter. Finally, the time between 2005 and 2019 was divided into three intervals (i) 2005-2009, (ii) 2010-2014 and (iii) 2015-2019.
2.3. Data analysis
The data was analyzed using Microsoft Excel® and Epi-Info7 version 7.2.1.1. The data was analyzed according to time interval, age-groups, sex, and state. For the analysis of general trends in suicides, specific rates calculated by the number of deaths in each age group and sex at the national and departmental levels were used, divided by the annual population of the corresponding five-year period for each age group. Direct standardization was used to calculate age-specific mortality rates for the different time intervals. Population estimates were obtained from the Paraguayan General Office of Statistics, Survey and Censuses. National projection of population by sex and disaggregated by age group (2000-2050) based on the 2002 Census were used for the time interval 2006-2014. Population estimates starting from 2015 used data from the 2012 population census and projections for 2000-2025 [
16]. The world population was used as the WHO standard population for rate adjustments (2000-2025). The years potential of life lost (YPLL) were calculated considering 0 years as a lower limit for the cut-off point and 70 years as the upper age limit for both sex per thousand inhabitants. Suicide mortality rates were calculated per hundred thousand inhabitants as denominator. The trend of suicide mortality at the national level during 2005 to 2019 was analyzed with the Joinpoint Trend Analysis Software [
17].
The software took suicide trend data at the national level (increases or decreases) and the rate or rate of annual average change
and fit the simplest joinpoint model that the data allow. The minimum and maximum number of joinpoints were supplied by the investigators. The program started with the minimum number of joinpoints and tests whether more joinpoints were statistically significant and must be added to the model up to that maximum number. This enabled us to test whether an apparent change in trend was statistically significant. The tests of significance used the Monte Carlo Permutation method.
3. Results
3.1. Sociodemographic characteristics of deaths due to suicide
Table 1 shows the sociodemographic characteristics of deaths due to suicide in Paraguay during 2005 and 2019. In total, 4,776 deaths by suicide were recorded corresponding to 1.4% of all deaths recorded. A 62.1% increase between the first-time interval (2005-2009) and the last one (2015-2019) was observed. The percentage of men among all suicides increased from 71.2% (2005-2009) to 75% in 2015-2019. No statistically significant changes were observed in the distribution of age groups according to the three intervals. Most victims of suicide were recorded in the 15- to 24-year-old population followed by the 25 to 44 years-old age group. There was an increase in the percentage of victims with high school or University degrees during 2005 and 2019. Whereas 13.1% of all suicide victims during 2005 and 2010 had high school and 3.9% a university degree, the corresponding percentages of suicide victims with high school degree (16.6%) and university degree (5.3%) was higher in 2015-2019. There seemed to be a change in the site where suicide occurred during 2005 and 2019. The percentage of suicides that occurred in health care service decreased from 23% (2005-2009) to 14% (2010-2014) and 10% in 2015-2019. Suicides at home increased from 63% (2005-2009) to 73% (2015-2019). Whereas during 2005-2009 every second recorded suicide was by strangulation (50%), strangulation already accounted for three out of four suicides in 2015-2019. During the same time interval, the share of suicide by poisoning decreased from 19% to 3.5% and the sue of firearms from 24% to 15%. An increase in the prevalence of suicide in the urban region (from 72% to 77%) was observed between 2005 and 2019. Finally, 56-58% of the suicides occurred the during spring/summer period during 2005-2019.
3.2. Standardized mortality rate for suicides
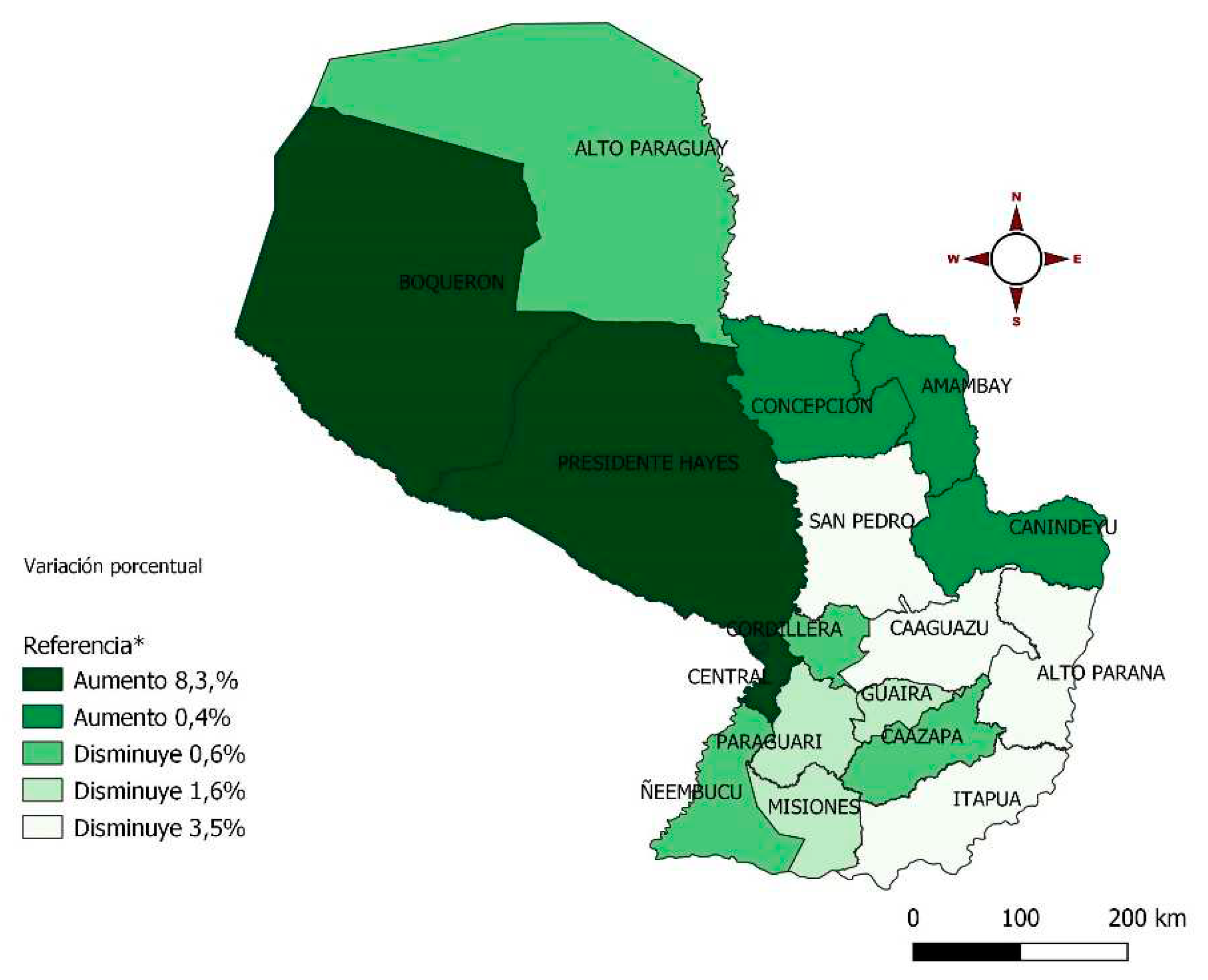
Of the 18 health regions, 12 experienced increases in suicide rates during the 2005-2019 period (
Figure 1). The regions that had increases of suicide rates above the national average were Presidente Hayes, Central, Boquerón, Caazapá, Capital, Amambay, Canindeyú, and Concepción.
The average suicide mortality rate nationwide during 2005 and 2019 was 4.9/100,000 with a gradual increase per five-year period, from 4.3/100,000 (2005-2009) to 5.7/100,000 between 2015 and 2019.
Table 2 presents the standardized mortality rate for suicides according to 5-year time intervals in Paraguay during 2005 and 2019. The age standardized mortality rate for suicides increased in men from 6.1/100,000 (2005-2009) to 8.5/100,00 during 2015-2019. The corresponding increase in women was much lower (from 2.4/100,000 in 2005-2009 to 2.9/100,000 in 20015-2019). Also, the gap in mortality rates for suicide increased between men and women during 2005 and 2019.
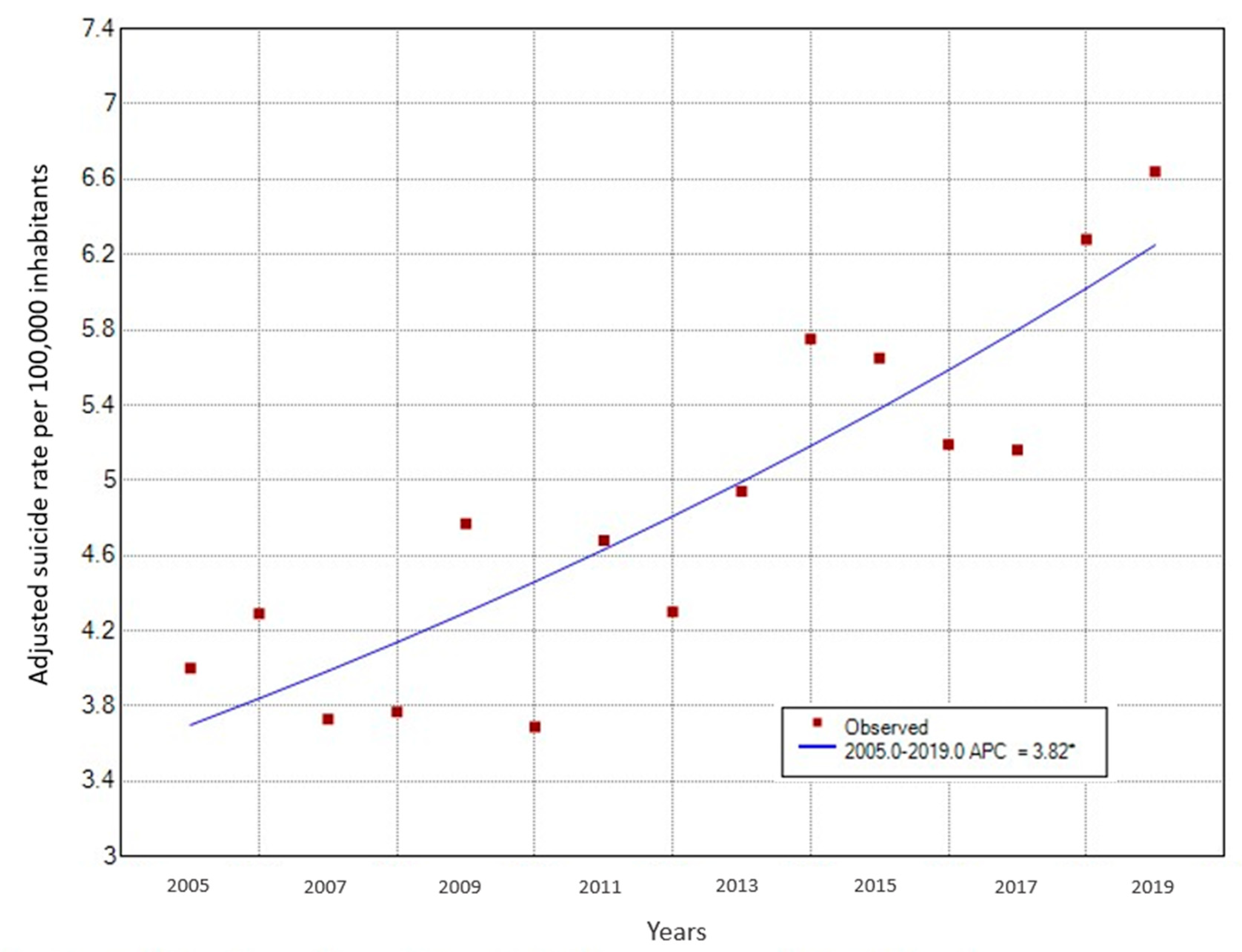
Joinpoint analysis revealed that suicide rates linearly increased by 3.82% per year in Paraguay during 2005 and 2019 (
Figure 2; p-value<0.001).
3.3. Rate of years of potential life lost by suicide
During the 15 years of observation, 172,612 years of potential life were lost due to suicide (
Table 3). The YPLL rate due to suicide increased in the Paraguayan population between the study period. Whereas the YPLL was 1.5/1,000, the corresponding rates for 2010-2014 and 2015-2019 were 1.8/1,000 and 2.1/1,000. Whereas the YPLL rate increased in men from 2.1/1,000 (2005-2009) to 3.02/1,000 during 2015-2019, it remained unchanged in women (1-1.1/1,000) during the three time intervals.
4. Discussion
Our data revealed that there was a linear increase in suicide mortality in Paraguay between 2005 and 2019. The age standardized mortality rate for suicides increased more in men than in women widening the gap in suicide mortality rates between men and women during 2005 and 2019. The YPLL due to suicide increased in men by 50% but remained stable in women. Three out of four suicides occurred by strangulation whereas suicide by poisoning and firearms showed a decreasing trend.
Even though the suicide mortality rate has increased, it is still lower than the ones reported from Argentine, Brazil, Chile, and Uruguay [
4]. However, a recent study that used preliminary data predicted a further increase of suicide mortality in Paraguay and that that the expected number of suicides in the following years from 2023 to 2027 will range between 462 and 530 per year [
8]. There are several reasons that may explain the increase in suicide mortality rate in Paraguay. First, the increase in suicide mortality may be due to an increase in mood and alcohol use disorders. These disorders are the most important modifiable predictors of suicide and [
18,
19] and both have shown to increase in the region [
20,
21,
22]
. Moreover, recent scientific evidence has suggested that acute alcohol use increases the risk of suicide attempts and that the risk of suicidal ideation, suicidal attempts, and death by suicide are each 2–3 times higher in people with alcohol use disorders compared with the general population [
23,
24]. A small part of the higher mortality rates observed may be explained by improved methods to differentiate suicide mortality from injury and accident-related mortality as some suicide deaths tend to be reported as accidental or underdetermined due to shame, stigma, or lack of evidence [
25]
.
The data that mal had a higher suicide mortality rate than women is consistent with the scientific literature [
26,
27].The gender difference in suicide intention or mortality rates are known as the “Gender Paradox” [
27]. A systematic review and meta-analysis of longitudinal studies revealed that women had a two-fold higher risk of suicide attempt than men, whereas the mortality rate of suicide was 2.5 times higher in men compared with women [
28,
29]. Another study revealed that women had higher rates of suicidal thinking, non-fatal suicidal behavior, and suicide attempts compared with men [
30]. Thus, women seem to exhibit less serious intent to die than men [
31]. Probably, the most important reasons for the observed difference between suicide attempts and suicide mortality between men and women is the method of suicide used. According to scientific evidence, men tend to choose more lethal suicide methods (firearms, hanging, and asphyxiation for instance) while women were more prone to overdose on medications or drugs than men [
32]. Our data regarding higher suicide mortality rates in those with lower levels of education is consistent with previous studies. Several studies in different populations have revealed an inverse association between educational levels and suicide mortality rates in different populations [
33,
34,
35,
36,
37]. It has been suggested that this may be due to better opportunities of being employed for people with higher levels of education resulting in higher level of social integration and lower suicide rates [
33,
37,
38]. While having lower levels of education may increase the chance of unemployment leading to less responsibilities, more narrow networks, and less social ties [
37].
Our data revealed a marked gap in suicide deaths among urban and rural populations, which may be related to several factors ranging from political to anthropological factors. Several epidemiological studies have described these urban–rural variations. However, data on the associations between urban–rural areas and suicide have been contradictory [
39,
40,
41,
42,
43,
44]. While some studies reported statistically significantly higher suicide rates in urban compared with rural areas, some revealed the opposite, and others did not find a difference in suicide between urban and rural areas. It has been proposed that stigma surrounding mental health issues, social isolation, limited social support, socioeconomic conditions, lifestyles, and environmental factors can all play a role in influencing the wellbeing of rural communities [
45]. Finally, a recent literature review in inequalities of suicide mortality across urban and rural areas did not reveal an urban–rural pattern regarding urban–rural changes over time [
46]. Future research may explore the associations between urban -rural areas and suicide mortality and its underlying determinants.
Even though suicide is a serious public health concern in Paraguay, the existing strategies remain limited. Efforts to mitigate the incidence of suicide predominately revolve around restricting access to the means of self-harm for individuals at risk, fostering social and-emotional life skills in adolescents, ensuring the availability of integrated mental health services at the primary care level, and dismantling the stigma surrounding mental health- an obstacle often impeding individuals from seeking help. Recently, the Pan American Health Organization introduced a comprehensive strategy for enhancing mental health and preventing suicide across the Americas focusing on six strategic lines of actions [
47]: (i) fostering mental health leadership, governance, and multisectoral partnerships, and integrate mental health in all policies; (ii) enhancing the availability, accessibility, and quality of community-based services for mental health conditions, and support the advance of deinstitutionalization; (iii) promoting mental health promotion and prevention strategies and activities throughout the life course; (iv) integrating mental health and psychosocial support in emergency contexts; (v) strengthening data, evidence, and research and (vi) prioritizing suicide prevention a national whole-of-government priority and build multisectoral capacity to respond to people affected by suicidal behaviors.
Another proposed community intervention to address suicide in the region is the Engaged Community Action for Preventing Suicide (ECAPS) Model, specifically designed for low-resource settings to confront systemic, societal, and individual level factors [
48]. This model proves to be both feasible and effective in guiding the development of culturally relevant, community-level intervention. ECAPS adopts a community-based participatory approach fostering cross-cultural partnerships, resource sharing and shared decision-making power [
49]. The seven key steps of involve: (1) Identifying the relevant determinants specific to the community associated with suicide risk; (2) Assessing the resources available (and not available) in the community; (3) Prioritizing determinants according to available resources; (4) Developing a change strategy; (5) Implementing the strategy; (6) Evaluating outcomes; and (7) Identifying next steps. Results of the ¡PEDIR! Program revealed that the ECAPS model is a feasible and effective framework for use in low-resource settings to guide the development of a culturally relevant community-level intervention to address the systemic, societal, and individual level factors that serve as barriers to suicide prevention [
49].
Naturally, our study has some limitations. Under-reporting of suicide may introduce bias in the assessment of suicide mortality. In addition, the quality of mortality statistics (coverage, accuracy, and completeness of data) may have introduced some bias in estimating suicide mortality. For instance, data on suicide mortality in the indigenous population was not available. The department of vital statistics reported that there is an underreporting of deaths that accounts up to 18% in the last available year (2019). Also, the validity of death certification for suicide is a major problem as some of the suicides may be classified as undetermined intent or accident or violent deaths. The vital statistics department revealed that approximately 7% of deaths were incorrectly classified [
50].
5. Conclusions
In conclusion, the increase in suicide mortality in Paraguay is of concern and an important cause of burden of premature death. Future analytical, observational studies should be conducted to identify what the most important predictors of suicide are. Also, more data is needed on the associations between social determinants of health and increasing suicide mortality trends. Moreover, a surveillance system monitoring the characteristics and trends of suicide in Paraguay needs to be implemented to assist political decision makers in developing policies and population-wide interventions to identify people at risk early to offer counseling and support. Finally, to decrease the observed suicide mortality, interdisciplinary collaboration is needed including health professionals, political decision makers, educators, and others.
Author Contributions
Conceptualization, ES, DDZ, GB, GS, DS, NB, FC; methodology, ES, DDZ, GB, GS, FC; software, ES, DDZ, formal analysis, ES, DDZ, BG, GS; investigation, ES, DDZ; resources, DDZ; data curation, ES, GS; writing—original draft preparation, ES, NB; writing—review and editing, ES, DDZ, GB, GS, DS, NB and FC; supervision, GS, FC; project administration, GS. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The three basic principles of ethics in research involving human beings were respected: the principle of respect for persons, the principle of beneficence and the principle of justice. The data gathered for this study was consistently collected by the national surveillance system from the Ministry of Health. The database used ensures that the information is anonymized.
Informed Consent Statement
The information used for the study was derived from data that is regularly collected by the Paraguayan Ministry of Health's mortality surveillance system (SSIEV-
https://ssiev.mspbs.gov.py/). The records analyzed for this study have been anonymized.
Data Availability Statement
The authors do not have permission to share their study data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO Global Tuberculosis Report 2014. Geneva, Switzerland: World Health Organization, 2014.
- Fazel, S.; Runeson, B. Suicide. New England Journal of Medicine 2020, 382, 266–274. [CrossRef]
- Naghavi, M. Global, Regional, and National Burden of Suicide Mortality 1990 to 2016: Systematic Analysis for the Global Burden of Disease Study 2016. BMJ 2019, l94. [CrossRef]
- Ilic, M.; Ilic, I. Worldwide Suicide Mortality Trends (2000-2019): A Joinpoint Regression Analysis. World J Psychiatry 2022, 12, 1044–1060. [CrossRef]
- World Health Organization Mental Health and Substance Use.; Geneva, 2021;
- 6. Directorate for Surveillance of Noncommunicable Diseases Surveillance Bulletin Number 2 Noncommunicable Diseases and Risk Factors (2017); Asuncion, 2017;
- Mansilla Izquierdo F Suicide and Prevention; 1st ed.; Palma de Mallorca, 2010;
- Torales, J.; Barrios, I.; Melgarejo, O.; Tullo-Gómez, J.E.; Díaz, N.R.; O’Higgins, M.; Maggi, C.; Adorno, V.; Medina, A.; Villalba-Arias, J.; et al. Suicides among Adults in Paraguay: An 18-Year National Exploratory Study (2004–2022). International Journal of Social Psychiatry 2023, 002076402311696. [CrossRef]
- World Health Organization Suicide Worldwide in 2019: Global Health Estimates.; Geneva, 2021;
- Phillips, J.A.; Nugent, C.N. Suicide and the Great Recession of 2007-2009: The Role of Economic Factors in the 50 U.S. States. Soc Sci Med 2014, 116, 22–31. [CrossRef]
- Kim, N.; Mickelson, J.B.; Brenner, B.E.; Haws, C.A.; Yurgelun-Todd, D.A.; Renshaw, P.F. Altitude, Gun Ownership, Rural Areas, and Suicide. American Journal of Psychiatry 2011, 168, 49–54. [CrossRef]
- Yip, P.S.F.; Yang, K.C.T.; Qin, P. Seasonality of Suicides with and without Psychiatric Illness in Denmark. J Affect Disord 2006, 96, 117–121. [CrossRef]
- Laanani, M.; Ghosn, W.; Jougla, E.; Rey, G. Impact of Unemployment Variations on Suicide Mortality in Western European Countries (2000–2010). J Epidemiol Community Health (1978) 2015, 69, 103–109. [CrossRef]
- DIGIES Sub-Sistema de Estadisticas Vitales Available online: https://ssiev.mspbs.gov.py/ (accessed on 6 October 2023).
- DIGIES Indicadores Básicos de Salud Available online: http://portal.mspbs.gov.py/digies/publicaciones/indicadores/ (accessed on 6 October 2023).
- Instituto Nacional de Estadística Proyección de La Población Por Sexo y Edad, Según Distrito, 2000-2025.
- Surveillance Research Program, N.C.Institute. Joinpoint Regression Program Version 4.8.0.1 - April 2020; Statistical Methodology and Applications Branch; 2020;
- Nordentoft, M. Absolute Risk of Suicide After First Hospital Contact in Mental Disorder. Arch Gen Psychiatry 2011, 68, 1058. [CrossRef]
- Nock, M.K. Future Directions for the Study of Suicide and Self-Injury. Journal of Clinical Child & Adolescent Psychology 2012, 41, 255–259. [CrossRef]
- Mental Health and Substance Use Depression and Other Common Mental Disorders: Global Health Estimates.; 2017;
- Manthey, J.; Shield, K.D.; Rylett, M.; Hasan, O.S.M.; Probst, C.; Rehm, J. Global Alcohol Exposure between 1990 and 2017 and Forecasts until 2030: A Modelling Study. The Lancet 2019, 393, 2493–2502. [CrossRef]
- Martinez-Ales, G.; Hernandez-Calle, D.; Khauli, N.; Keyes, K.M. Why Are Suicide Rates Increasing in the United States? Towards a Multilevel Reimagination of Suicide Prevention. In; 2020; pp. 1–23.
- Borges, G.; Bagge, C.L.; Cherpitel, C.J.; Conner, K.R.; Orozco, R.; Rossow, I. A Meta-Analysis of Acute Use of Alcohol and the Risk of Suicide Attempt. Psychol Med 2017, 47, 949–957. [CrossRef]
- Darvishi, N.; Farhadi, M.; Haghtalab, T.; Poorolajal, J. Alcohol-Related Risk of Suicidal Ideation, Suicide Attempt, and Completed Suicide: A Meta-Analysis. PLoS One 2015, 10, e0126870. [CrossRef]
- BEAUTRAIS, A.L.; JOYCE, P.R.; MULDER, R.T. Risk Factors for Serious Suicide Attempts among Youths Aged 13 through 24 Years. J Am Acad Child Adolesc Psychiatry 1996, 35, 1174–1182. [CrossRef]
- Cervantes, C.A.D.; Montaño, A.M.P. Estudio de La Carga de La Mortalidad Por Suicidio En México 1990-2017. Revista Brasileira de Epidemiologia 2020, 23. [CrossRef]
- Canetto, S.S.; Sakinofsky, I. The Gender Paradox in Suicide. Suicide Life Threat Behav 1998, 28, 1–23. [CrossRef]
- Miranda-Mendizabal, A.; Castellví, P.; Parés-Badell, O.; Alayo, I.; Almenara, J.; Alonso, I.; Blasco, M.J.; Cebrià, A.; Gabilondo, A.; Gili, M.; et al. Gender Differences in Suicidal Behavior in Adolescents and Young Adults: Systematic Review and Meta-Analysis of Longitudinal Studies. Int J Public Health 2019, 64, 265–283. [CrossRef]
- Vijayakumar, L. Suicide in Women. Indian J Psychiatry 2015, 57, 233. [CrossRef]
- Crosby, A.E.; Han, B.; Ortega, L.A.G.; Parks, S.E.; Gfroerer, J.; Centers for Disease Control and Prevention (CDC) Suicidal Thoughts and Behaviors among Adults Aged ≥18 Years--United States, 2008-2009. MMWR Surveill Summ 2011, 60, 1–22.
- Freeman, A.; Mergl, R.; Kohls, E.; Székely, A.; Gusmao, R.; Arensman, E.; Koburger, N.; Hegerl, U.; Rummel-Kluge, C. A Cross-National Study on Gender Differences in Suicide Intent. BMC Psychiatry 2017, 17, 234. [CrossRef]
- Callanan, V.J.; Davis, M.S. Gender Differences in Suicide Methods. Soc Psychiatry Psychiatr Epidemiol 2012, 47, 857–869. [CrossRef]
- Øien-Ødegaard, C.; Hauge, L.J.; Reneflot, A. Marital Status, Educational Attainment, and Suicide Risk: A Norwegian Register-Based Population Study. Popul Health Metr 2021, 19, 33. [CrossRef]
- Bálint, L.; Osváth, P.; Rihmer, Z.; Döme, P. Associations between Marital and Educational Status and Risk of Completed Suicide in Hungary. J Affect Disord 2016, 190, 777–783. [CrossRef]
- Dare, A.J.; Irving, H.; Guerrero-López, C.M.; Watson, L.K.; Kolpak, P.; Reynales Shigematsu, L.M.; Sanches, M.; Gomez, D.; Gelband, H.; Jha, P. Geospatial, Racial, and Educational Variation in Firearm Mortality in the USA, Mexico, Brazil, and Colombia, 1990–2015: A Comparative Analysis of Vital Statistics Data. Lancet Public Health 2019, 4, e281–e290. [CrossRef]
- Næss, E.O.; Mehlum, L.; Qin, P. Marital Status and Suicide Risk: Temporal Effect of Marital Breakdown and Contextual Difference by Socioeconomic Status. SSM Popul Health 2021, 15, 100853. [CrossRef]
- Choi, M.; Sempungu, J.K.; Lee, E.H.; Chang, S.-S.; Lee, Y.H. Single and Combined Effects of Marital Status, Education Attainment, and Employment Status on Suicide among Working-Age Population: A Case-Control Study in South Korea. SSM Popul Health 2022, 19, 101246. [CrossRef]
- Denney, J.T.; Rogers, R.G.; Krueger, P.M.; Wadsworth, T. Adult Suicide Mortality in the United States: Marital Status, Family Size, Socioeconomic Status, and Differences by Sex *. Soc Sci Q 2009, 90, 1167–1185. [CrossRef]
- Fontanella, C.A.; Hiance-Steelesmith, D.L.; Phillips, G.S.; Bridge, J.A.; Lester, N.; Sweeney, H.A.; Campo, J.V. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatr 2015, 169, 466–473. [CrossRef]
- Helbich, M.; Blüml, V.; de Jong, T.; Plener, P.L.; Kwan, M.-P.; Kapusta, N.D. Urban-rural inequalities in suicide mortality: A comparison of urbanicity indicators. Int. J. Health Geogr 2017, 16, 39. [CrossRef]
- Levin, K.A.; Leyland, A.H. Urban/rural inequalities in suicide in Scotland, 1981–1999. Soc. Sci. Med 2005, 60, 2877–2890. [CrossRef]
- Barry, R.; Rehm, J.; de Oliveira, C.; Gozdyra, P.; Kurdyak, P. Rurality and risk of suicide attempts and death by suicide among people living in four English-speaking high-income countries: A systematic review and meta-analysis. Can. J. Psychiatry 2020, 65, 441–447. [CrossRef]
- Li, M.Z.; Katikireddi, S.V. Urban-rural inequalities in suicide among elderly people in China: A systematic review and meta-analysis. Int. J. Equity Health 2019, 18, 2. [CrossRef]
- Hagedoorn, P.; Groenewegen, P.P.; Roberts, H.; Helbich, M. Is suicide mortality associated with neighbourhood social fragmentation and deprivation? A Dutch register-based case-control study using individualised neighbourhoods. J. Epidemiol Community Health 2020, 74, 197–202. [CrossRef]
- Moya-Salazar, J.; Villareal, C.; Cañari, B.; Moya-Salazar, B.; Chicoma-Flores, K.; Contreras-Pulache, H. COVID-19 may lower Quality of Life when infections and deaths increase: a longitudinal study in the Peruvian jungle. Front Psychiatry 2023, 14, 905377. [CrossRef]
- Casant, J.; Helbich, M. Inequalities of Suicide Mortality across Urban and Rural Areas: A Literature Review. Int J Environ Res Public Healt. 2022, 19(5), 2669. [CrossRef]
- Pan American health organization. CD60/9 – Strategy for Improving Mental Health and Suicide Prevention in the Region of the Americas. Available online at: https://www.paho.org/en/documents/cd609-strategy-improving-mental-health-and-suicide-prevention-region-americas (accessed on 15 December 2023).
- Alonzo, D.; Zapata Prato, D. Mental health services for individuals at risk of suicide in Peru: attitudes and perspectives of mental health professionals. Intern J Soc Psychiat 2020, 67(3), 209. [CrossRef]
- Alonzo, D. The engaged community action for preventing suicide (ECAPS) model in Latin America: development of the ¡PEDIR! program. Soc Psychiatry Psychiatr Epidemiol 2023, 58(6), 861-870,. [CrossRef]
- Ministerio de Salud Pública y Bienestar Social Indicadores Básicos de Salud, Paraguay; Asunción, 2019;
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).