1. Introduction
Ankle fractures are among the most common skeletal bone injuries, with an estimated prevalence of distal tibiofibular syndesmosis injury of up to 11% of cases [
1]. At least one third of these fractures affect the tibial posterior malleolus (TPM) (Volkmann's fragment), which seems to have a direct impact on worsening clinical outcomes. A recent biomechanical study using a cadaveric model showed that, in a situation of absence of load, neither the injury to the syndesmotic complex nor the fracture TPM significantly influenced the position of the fibula in the fibular notch [
2]. However, this study was based on a designed surgery without additional injuries in a weight-bearing free situation. In addition, the simulated injury during this cadaver study differed in mode from the injuries usually seen after trauma. Thus, considering current knowledge, most ligament injuries of distal tibiofibular syndesmosis and/or TPM fracture will require surgical stabilization [
3].
Despite this, there is still no consensus on the size of the Volkmann fragment that potentially generates instability of the syndesmotic complex, and it remains unclear what is the best approach for this fracture, especially regarding when and how its reduction and fixation. Currently, the most accepted indication is that fractures of the TPM should be operated when they affect at least 20% of the tibiotalar articular surface (TTAS) or present articular diastasis ≥2.0-mm [
4]. In these cases, the reduction is preferably carried out directly with fixation using an anti-glide plate. In another cadaveric study, it was shown that the rigidity of the distal tibiofibular syndesmosis was restored in 70% after fixation of the TPM and in 40% after stabilization of the syndesmosis when compared to intact specimens [
5].
More recently, Mansur et al. [
6] compared the biomechanical behavior of four different methods used for fixation of the TPM using a finite element model (FEM), concluding that the use of two 3.5-mm cannulated screws from posterior to anterior provided better fixation resistance in this type of lesion. Despite these findings, these authors did not investigate the role of TPM fixation in fragments smaller than 30% of the TTAS, nor did they use a comparative model with trans-syndesmotic screw (TSS).
The null hypothesis is that fixation of the TPM with an anti-glide plate, alone or in association with the use of a TSS, regardless of the size of the fragment and the involvement of the TTAS, is superior to stabilization performed with a syndesmotic screw alone. In the herein study, we aimed to biomechanically evaluate the behavior of different fixations of the TPM, simulating distinct situations of involvement of the TTAS through a FEM.
2. Materials and Methods
1. Finite element models of ankle joint.
The study was approved by the Institutional Review Board of the hospital and did not involve animals nor humans. A 3D computer-aided design (CAD) model of the left ankle was obtained based on 4th generation composite tibia and fibula models. Tibia model had a length of 405±1 mm, a distal tibial joint width of 58±1 mm, and an inner canal of 10 mm in diameter (#3402, Sawbones, Seattle, USA), whereas fibula model had a length of 384±1 mm, a distal width of 19±1 mm, and an inner canal of 2.5 mm in diameter (#3427-1, Sawbones, Seattle, USA).
The materials used were divided according to their characteristics into ductile (metallic implants) and non-ductile (bone and ligaments). All materials were assumed to be linear elastic, isotropic, and homogenous. The elastic modulus and Poisson’s ratio were obtained from previous studies [
6,
7,
8] (
Table 1).
2. BioCad preparation.
From the synthetic bone models and their syntheses, a computed tomography (CT) scan images of the left ankle in neutral unloaded position were obtained and archived in the communication protocol that includes DICOM (Digital Imaging and Communications in Medicine) files. We used the Emotion CT scan with 16 channels (Siemens™, Munich, Germany), with a resolution of 512x512, and a slice interval of 1.0 mm. The DICOM file was imported to the program InVesalius™, for the three-dimensional (3D) reconstruction of the anatomical structure. Based on a set of two-dimensional images obtained through CT equipment, the program allows the generation of 3D virtual models of the regions of interest. After reconstructing the DICOM images in 3D, the program allows the generation of 3D files in STereo Lithography (STL) format.
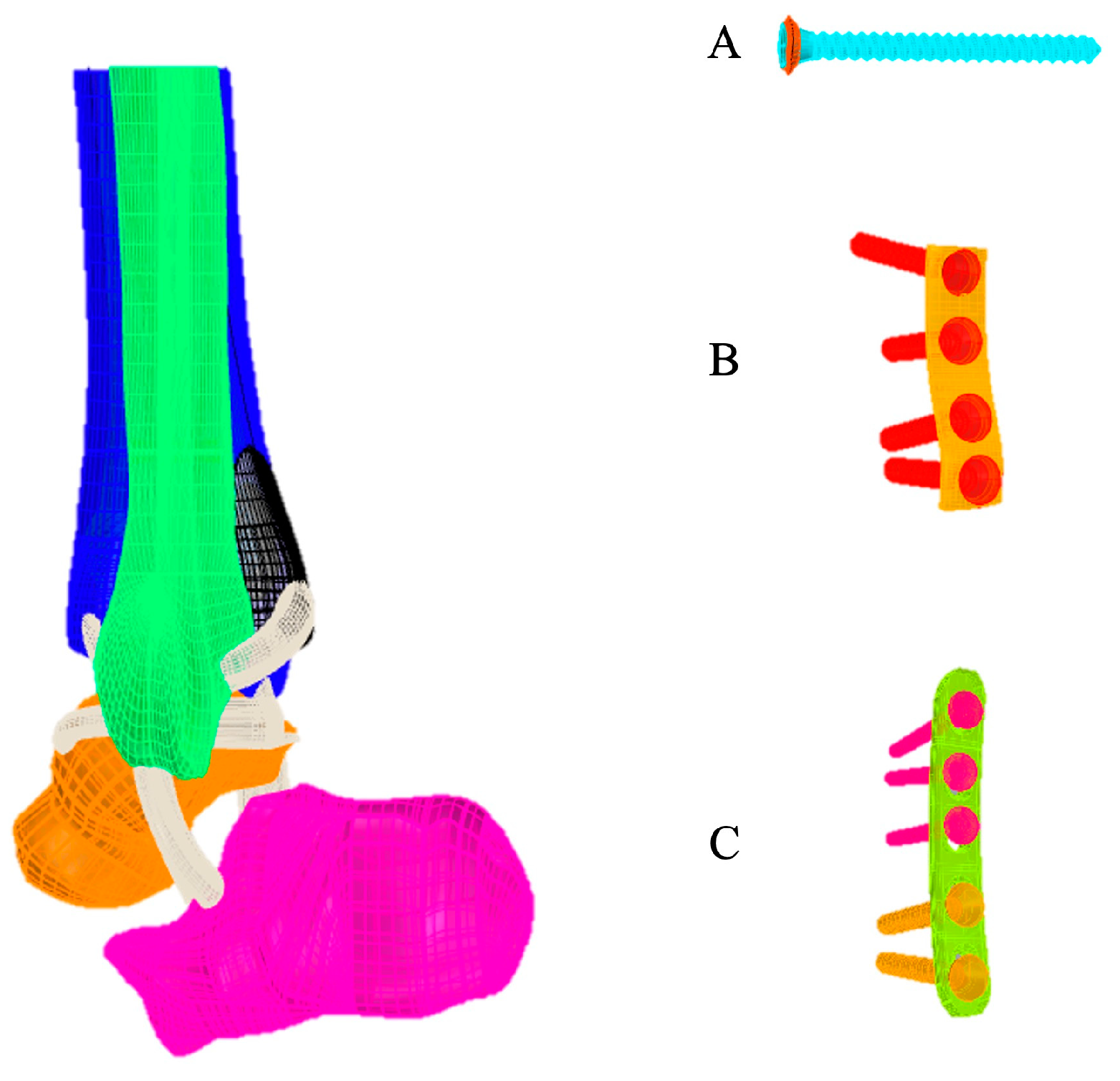
The 3D virtual models of each system (bone and implants) were made by the program Rhinoceros™ 6 (Robert McNeel & Associates, USA). The geometric models of cartilage and ligament were built according to the anatomical relationship between the bones and ligaments following the methodology described by Guan et al. [
9]. Ligaments included anterior tibiofibular ligament, posterior tibiofibular ligament, anterior talofibular ligament, posterior talofibular ligament, deltoid ligament, and calcaneofibular ligament, and the thickness of cartilage was about 1.0 mm (
Figure 1). The analysis by FEM was performed in the program SimLab™ (HyperWorks, United States), using the Optistruct solver, in a computer with Intel Xeon processor (CPU E-3-1240 v3 3.40 GHz, with 32 GB RAM in a 64-bit Windows 7 operating system).
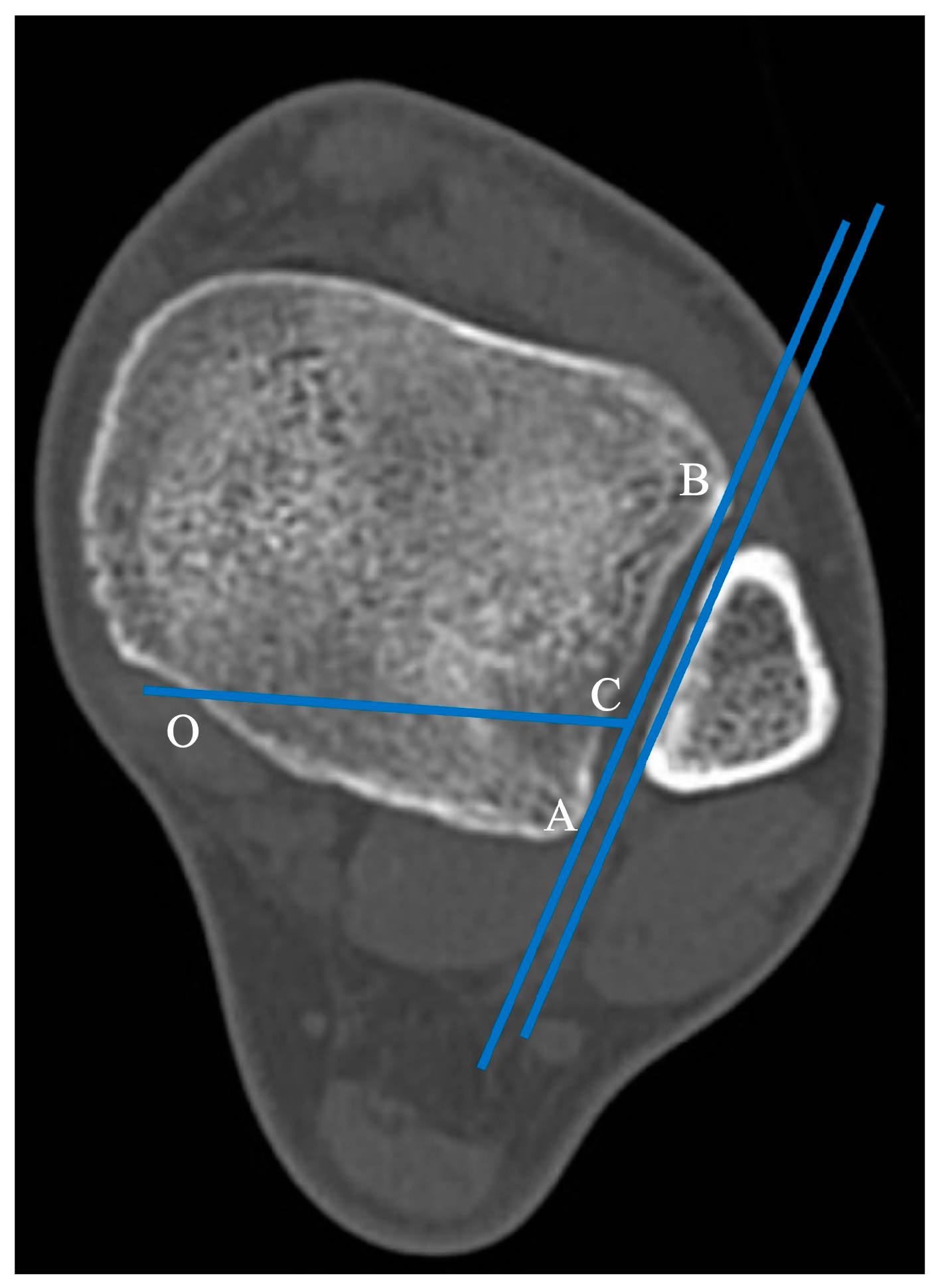
The horizontal projection of the distal articular surface of the tibia was taken as the reference plane. The AB projection line in the plane of the fibular notch and parallel to the medial fibula cortex was taken as a reference line and the point of intersection of the posterior ankle and medial ankle was point “O” [
9]. The 1/4 point of the AB line was taken as point C. The intersection point of the posterior ankle and medial ankle was the “O" point, and the OC line was connected as the horizontal fracture line (
Figure 2).
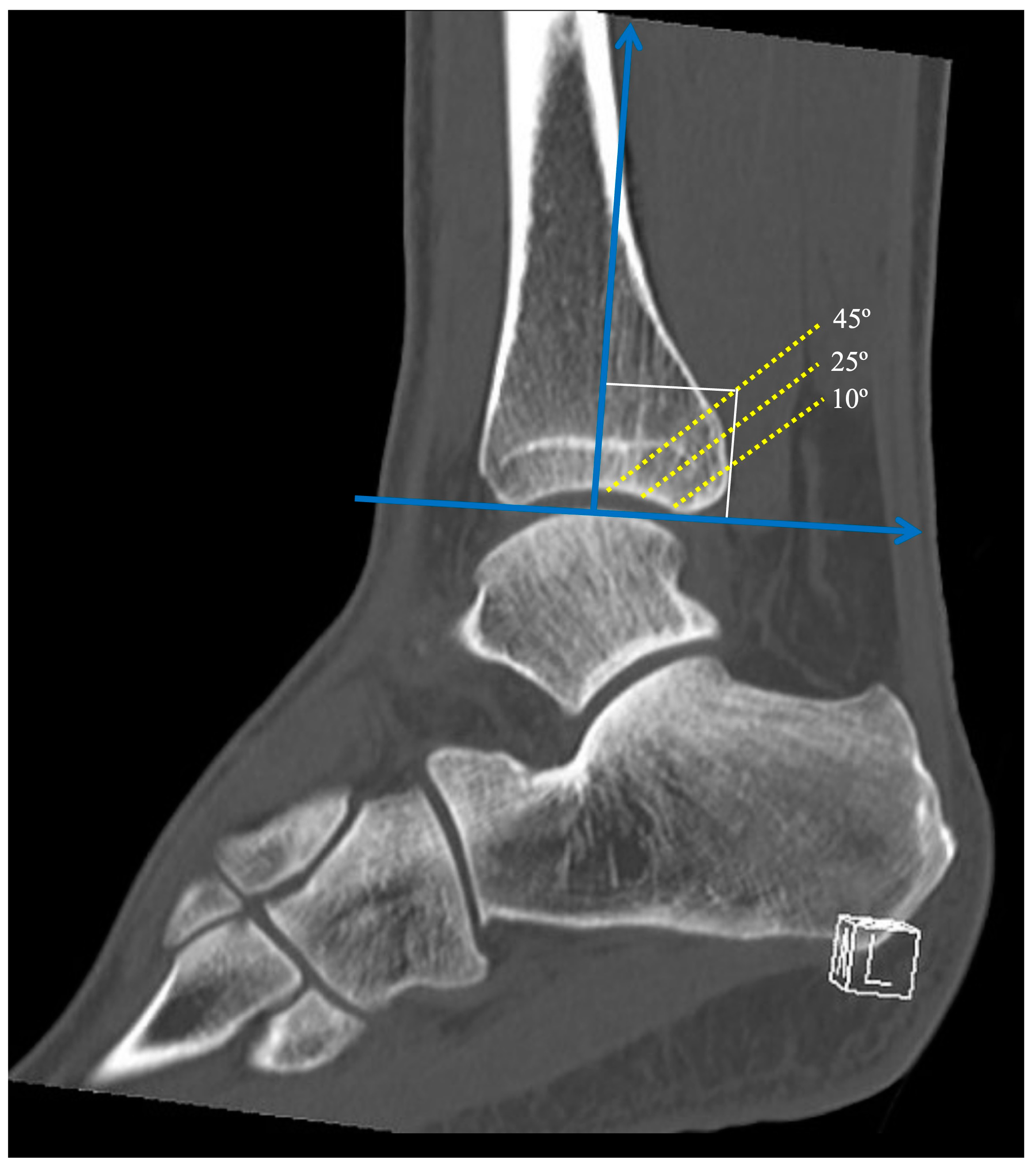
The angle between the fracture line and the Z axis on the sagittal reconstruction images was defined as the sagittal angle of the posterior malleolus fracture (
Figure 3). Taking the Z axis in the sagittal reconstruction images, three different fracture lines of the posterior malleolus were defined, with sagittal angles of 10º, 25º, and 45º. The sagittal angles were defined to simulate a fracture line considered stable (10º), a fracture line that affects the fibular notch (25º), and a fracture line that affects a large part of the tibiotalar loading area (45º), representing a tibial pilon.
The implants used were a 2.7 mm, straight, 5-hole, titanium alloy locked compression plate (X49.681), a 3.5 mm non-locked titanium alloy 1/3 tubular plate, 4 holes (245-401), and a 50 mm 3.5 mm titanium alloy cortical screw. All implants were formatted as indicated by the manufacturer's dimensional characteristics (DePuy Synthes – J&J Company, USA). Two lag-screws were inserted through the distal holes of both plates to apply interfragmentary compression to the posterior malleolus. Three locked screws were used in the proximal holes of the 2.7 mm locked compression plate. The transsyndesmotic screw was inserted as positioning screw to hold the syndesmosis in place.
3. File conversion.
In the InVesalius™ program, all slices were imported to obtain the STL file with the images that would be used in the process of obtaining the 3D solid. This allowed for multiplanar generation, which made it possible to evaluate images in the sagittal, coronal, and axial planes, and volume. From the volume, the creation of the 3D surface was carried out, allowing the selection of the regions of interest using masks and/or filters. This allowed the file to be hidden or portrayed, according to the algorithm in question, generating the 3D surface.
4. Simulation and boundary conditions.
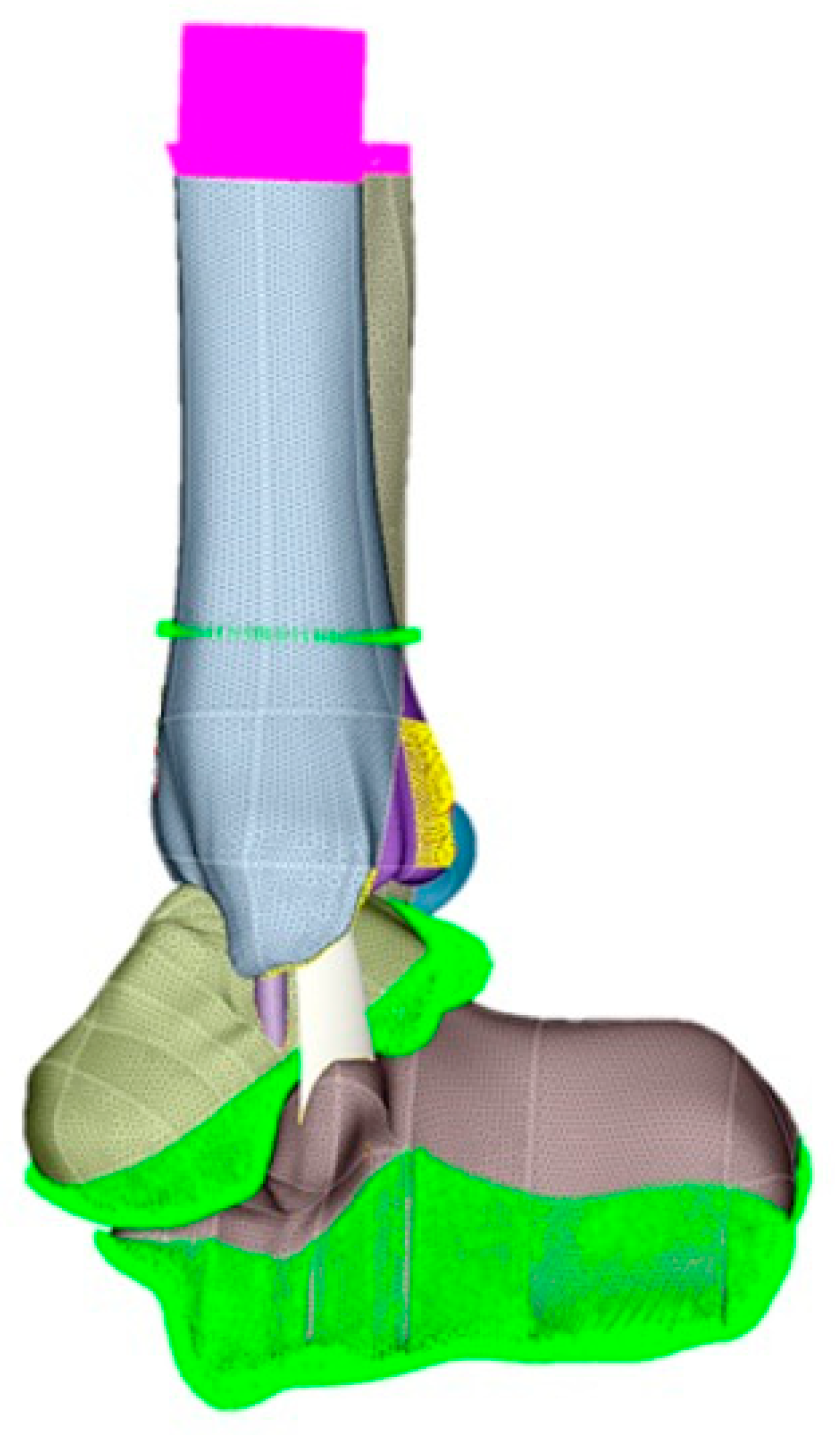
The FEM was used for the stability simulations of the different assemblies. First, the files will be imported into the Simlab™ program, with identification of each part of the digital models. After controlling the meshes of each part, care was taken to always maintain the size of the element, so that there were no contact problems between the different parts in the simulations. A tetrahedral element was adopted to form the meshes.
To define the boundary conditions, load application regions were selected in the direction of the 700N Z axis, 90% on the tibia and 10% on the fibula. On the X and Y axes, no loading was applied. Subsequently, the movement restriction regions (fixed) were delimited, marked in all directions of the displacement and rotation X Y Z axes. These restrictions ensured that the system had perfect alignment without displacement and/or rotation. The friction coefficient of the fracture surface was 0.3. Ligaments were applied to the model as preload by reducing the length of ligaments by 2% with zero load.
5. Load application and fixation site.
After controlling the meshes of each part, care was taken to always maintain the size of the element, so that there are no contact problems between the different parts (ankle and synthesis) in the simulations (
Figure 4).
For biomechanical comparison, each of three different fracture lines of the posterior malleolus (10°, 25°, and 45°) were tested with the following constructions: a transsyndesmotic screw only (Group T), a one-third tubular plate only (Group PS), a one-third tubular plate plus a transsyndesmotic screw (Group PT), locked compression plate only (Group LCPS), and locked compression plate plus a transsyndesmotic screw (Group LCPT). We also tested the models without fixation (Group S) to evaluate the degree of instability generated by the different fracture lines.
Data on the displacement and stress in the FEM were collected, including the total principal maximum (tension, MaxT) and total principal minimum (compression, MinT) for non-ductile materials, total displacement (desT), localized displacement at the fragment (desL), localized displacement at syndesmosis (desS), and Von Mises equivalent stress for ductile materials. Because the mechanical properties, the (-) sign represents the direction of compressive stress (MinT). All results are presented in absolute values and percentiles between the models.
6. Statistical analysis.
Descriptive statistics and percentages were used to determine means and differences. One-way ANOVA and multiple comparison LSD tests were used to determine the mean difference. P-value was considered significant if p < 0.05. The statistical software SPSS 21.0 (SPSS Inc., Chicago IL) was used.
3. Results
The number of nodes was defined as shown in
Table 2. All results are presented for the three different fracture lines of the posterior malleolus (10°, 25°, and 45°) and the tested constructions are summarized in the
Table 3,
Table 4 and
Table 5.
For posterior malleolus fractures with a sagittal angle of 10º, there was no statistical significance between groups T, PT, and LCPT for desT and desS (p <0.005), however desL was significantly lower in the PT and LCPT groups, although there was no statistically significant difference between them. There was statistically significant reduction for the Von Mises stress in Group LCPT (p <0.00001), which denotes less demand on implants in this construction (
Table 3).
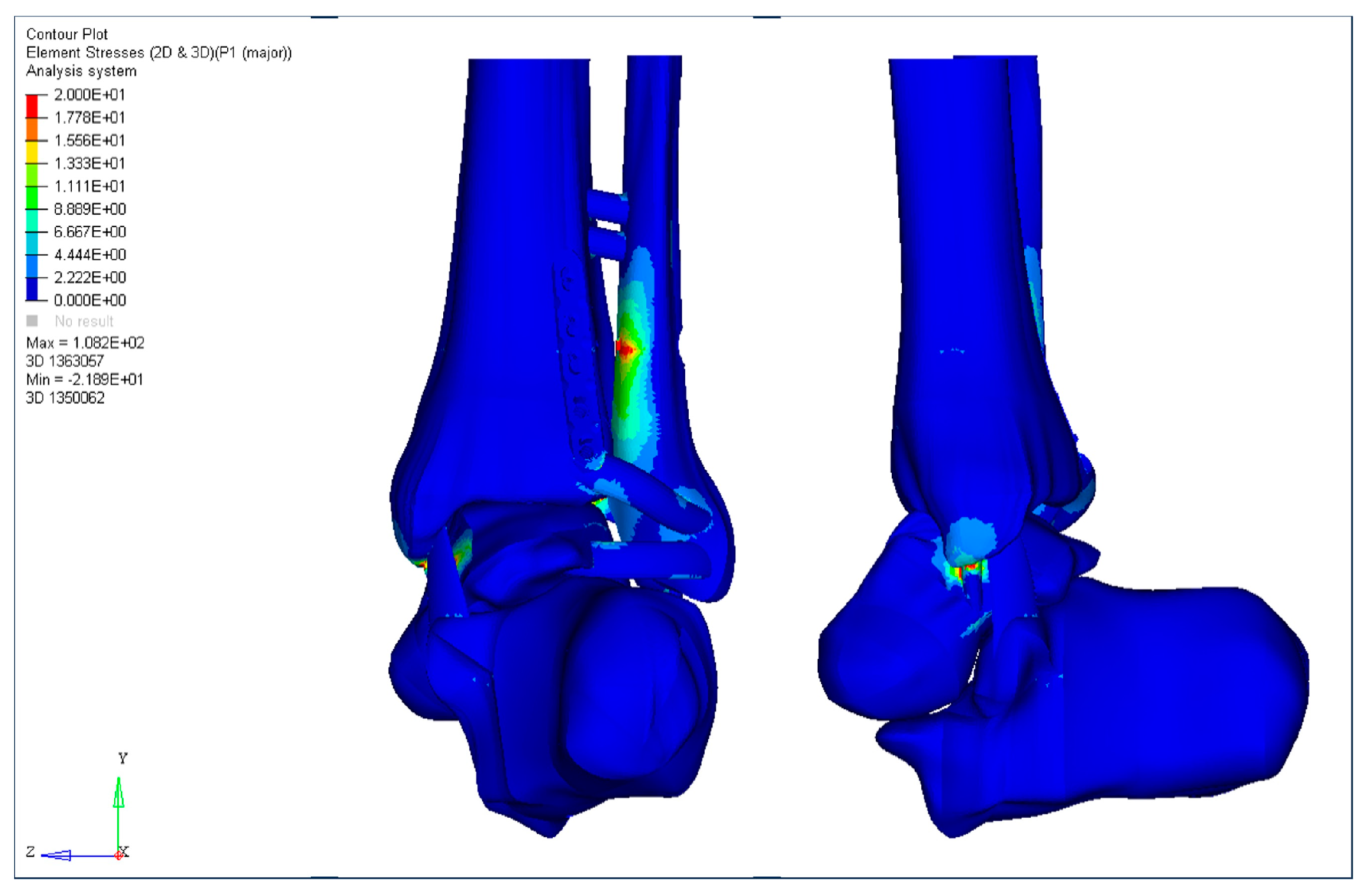
Figure 5 illustrates the MaxT for Group LCPS.
Table 3.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 10º.
Table 3.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 10º.
| |
Group S |
Group T |
Group PS |
Group PT |
Group LCPS |
Group LCPT |
| MaxT |
138.9 |
158.9 |
84.4 |
171.6 |
108.2 |
107.6 |
| MinT |
-111.5 |
-221.5 |
-78.74 |
-153.2 |
-71.03 |
-138.4 |
| desT |
18.34 |
13.34 |
13.73 |
13.15 |
13.67 |
13.63 |
| desL |
4.7 |
3.1 |
1.3 |
1.1 |
0.8 |
0.6 |
| desS |
6.4 |
4.1 |
7.1 |
3.6 |
7.0 |
3.4 |
| Von Mises |
n/a |
2533 |
1296 |
1290 |
1056 |
654.6 |
For posterior malleolus fractures with a sagittal angle of 25º, there was no statistical significance between groups T, PT, and LCPT for desT and desS (p.0.005), however desL was significantly lower in the PT and LCPT groups, although there was no statistically significant difference between them. There was a statistically significant reduction in Von Mises stress in the PT (p <0.00001) and LCPT (p <0.00001) groups, which denotes a lower requirement for implants in these constructions (
Table 4).
Table 4.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 25º.
Table 4.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 25º.
| |
Group S |
Group T |
Group PS |
Group PT |
Group LCPS |
Group LCPT |
| MaxT |
122.3 |
149.0 |
101.2 |
143.5 |
113.6 |
117.6 |
| MinT |
-97.34 |
-186.0 |
-87.47 |
-112.2 |
-128.4 |
-108.4 |
| desT |
20.18 |
13.67 |
13.72 |
13.40 |
10.60 |
14.63 |
| desL |
5.1 |
3.4 |
1.7 |
1.3 |
1.0 |
0.7 |
| desS |
6.7 |
4.3 |
7.2 |
3.5 |
7.1 |
3.5 |
| Von Mises |
n/a |
2445 |
831.2 |
739.3 |
1248 |
694.8 |
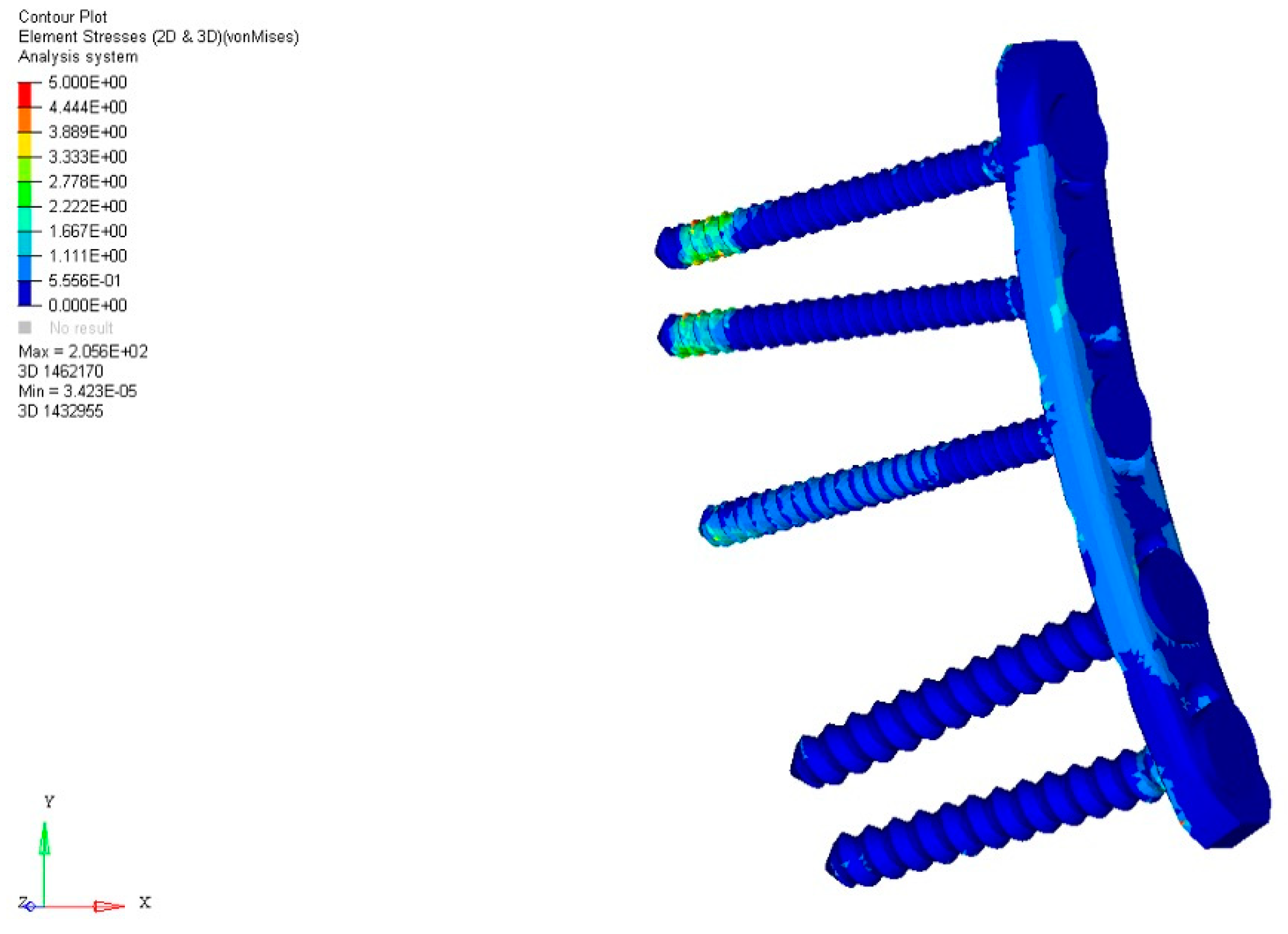
For posterior malleolus fractures with a sagittal angle of 45º, there was no statistical significance between groups T, PT, and LCPT for desT and desS (p.0.005), however desL was significantly lower in Group LCPT. There was a statistically significant reduction in Von Mises stress in group LCPS (p <0.05) and LCPT (p <0.05), although there was no statistically significant difference between them, which denotes a lower requirement for implants in these constructions (
Table 5 and
Figure 6).
Table 5.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 45º.
Table 5.
Data on the displacement and stress in the FEM for posterior malleolus fractures with a sagittal angle of 45º.
| |
Group S |
Group T |
Group PS |
Group PT |
Group LCPS |
Group LCPT |
| MaxT |
90.04 |
103.3 |
112.8 |
127.9 |
122.0 |
127.8 |
| MinT |
-78.87 |
-142.3 |
-78.87 |
-126.1 |
-82.57 |
-100.4 |
| desT |
24.17 |
15.34 |
15.55 |
15.23 |
20.81 |
19.88 |
| desL |
5.4 |
3.6 |
2.9 |
2.2 |
1.2 |
0.7 |
| desS |
7.0 |
4.6 |
7.3 |
3.8 |
7.2 |
3.6 |
| Von Mises |
n/a |
1145 |
1256 |
1119 |
594.8 |
794.8 |
4. Discussion
Although recent studies have raised the question of the role of the posterior malleolus in ankle stability, there is still a great debate as to whether, when, and how posterior malleolus fractures should be repaired [
4,
5,
6,
10,
11]. It has been reported that fractures of the posterior malleolus occur in approximately 46% of Weber type B or C ankle fracture-dislocations and have a close relationship to injury or instability of the distal tibiofibular syndesmosis, especially the posterior inferior tibiofibular ligament (PITFL). Of relevance, it was shown that the PITFL is the most resistant in syndesmosis stability, with the majority of LTFPI injuries occurring in the form of delamination of the posterior malleolus [
12,
13].
In a large cohort of rotationally unstable ankle fractures without posterior malleolus fractures, Warner et al. [
13] observed that accurate and stable syndesmotic reduction is a significant component of restoring the ankle mortise after unstable ankle fractures. They found that in 122 ankle fractures, the PITFL was delaminated from the posterior malleolus in 97% (119/122) of cases, with a smaller proportion (3%; 3/122) having an intrasubstance PITFL rupture. Despite this, until recently the classic indications for surgical treatment were the presence of a fragment >25% and posterior instability of the ankle [
4].
Here we report the biomechanical behavior of different fixations of the posterior tibial malleolus, simulating different situations of involvement of the tibiotalar articular surface through a finite element model. In addition to presenting our results, we aimed to define the role of combined osteosynthesis of the Volkmann fragment using a posterior buttress plate and transsyndesmotic screw. Our findings showed that there is no need for direct reduction of a posterior malleolar fracture involving less than 10% of the articular surface, but it is necessary to stabilize the distal tibiofibular joint with a transsyndesmotic screw. When the posterior fragment of the tibia involves 25% of the articular joint, we find that it is necessary to use a buttress plate, but there is no difference if a locked or non-locked plate is used. The addition of a transsyndesmotic screw to the posterior plate does not significantly reduce the total maximum displacement or Von Mises stress. Finally, for the posterior malleolus involving 45% of the articular surface, the use of a locking plate significantly reduced the maximum total displacement and Von Mises stress, with or without the addition of a transsyndesmotic screw.
Our findings reinforce what was demonstrated by Bartoníček et al. [
14] that involvement of the fibular notch due to a posterior malleolus joint fracture potentially generates distal tibiofibular joint incongruity, leading to instability and post-traumatic osteoarthritis of the ankle. Although the magnitude of syndesmotic malreduction that can lead to inferior patient-reported outcomes remains unclear, theoretically both rotational and sagittal translation of the fibula may occur after posterior malleolus non-reduction, malreduction, or insufficient fixation, and may go undetected using traditional imaging methods [
15,
16].
In a retrospective cohort study of 87 patients with complete syndesmosis injury evaluated with radiographs and CT scan, Andersen et al. [
17] observed a syndesmosis malreduction rate of 32%. These authors noted that a difference of 2.0 mm in the anterior distal tibiofibular relationship predicts unsatisfactory clinical results, with 79% specificity and 61% sensitivity. In another study, Sagi et al. [
18] found a similar malreduction rate, as high as 44%, in patients in whom the syndesmosis underwent closed reduction.
Indeed, it has been reported that the overall functional outcome of ankle fractures with posterior malleolar involvement are significantly worse compared to uni or bimalleolar fractures [
4], which is probably due to the unrecognized or occult injury to the PITFL. Biomechanical studies have shown a significant decrease in the tibiotalar contact area as the size of the posterior malleolar fragment exceeds 33%, a significant increase in posterior subluxation between 25% and 40%, and an increase in stress on the remainder of the tibiotalar joint [
19,
20,
21,
22,
23]. In this context, adequate stabilization of the distal tibiofibular syndesmosis is essential for the normal movement of the ankle joint, necessary for weight transmission and walking, and the posterior malleolus is of great importance for this.
Mason et al. [
11,
23] recommended the use of one transsyndesmotic screw for extra-articular posterior malleolar fractures, sustained by avulsion from the distal posterior tibial cortex by the pull of the PITFL, and open reduction and internal fixation for posterolateral fractures of the tibia extending into the incisura fibularis, regardless of the size of the posterior malleolar fragment. Our findings indicate the same, however based on FEM results we suggest the use of a locked plate with or without a transsyndesmotic screw for posterior malleolar fragments greater than 45% of the tibiotalar articular joint.
This study has some limitations. As this is an experimental biomechanical study using FEM, limitations inherent to the project include the lack of correlation of mechanical findings with the expected biological response during tissue healing in a malleolar fracture of the ankle. In addition, we used normal-density 4th generation composite tibia and fibula models, therefore, our findings cannot be extrapolated to situations in which bone stock is not adequate, such as elderly patients with osteoporotic or insufficiency fracture. Also, the load application was performed in a single positioning of the ankle joint. Since this joint can undergo several load changes in the most varied gait cycles, it seems necessary to validate our findings simulating other ankle positions. Finally, our study evaluated a transsyndesmotic screw versus buttress plate constructs. We didn't evaluate the mechanical behavior of other implants currently used for the treatment of distal tibiofibular syndesmosis injury, such as elastic fixation devices and suture tape.
However, our study has strengths. First, the use of synthetic bone models in biomechanical experiments has been shown to increase the potential for high biomechanical fidelity, low variability across specimens, decreased financial burden, and ease of use compared to human cadaveric bones [
24,25]. Second, FEM may be applied to almost any orthopedic problem which is related to a biomechanical issue, representing the most used computational technique in orthopedic research [
24]. Third, we used highly controlled and reproducible testing conditions, simulating three different situations of posterior malleolus fracture, in which there continues to be controversy about the need to stabilize the distal tibiofibular syndesmosis and how to do it. Finally, in addition to the bone structures, in our model the ligamentous structures of the distal tibiofibular syndesmosis were considered in the computational model, which almost perfectly replicate the physiological condition of this joint. It has been suggested that the creation of an anatomical 3-D FEM of the ankle joint is necessary for realistic prediction of load transfer and stress distribution for preclinical analysis of numerous constructs and implants [26].
5. Conclusion
In conclusion, any fracture occurring in the posterior malleolus of the ankle can be indicative of potential instability within the distal tibiofibular syndesmosis, even when the fragment is relatively small in size. Our research findings have demonstrated that when the fracture involves approximately 10% of the tibiotalar articular surface, employing a transsyndesmotic screw is generally effective. However, in cases where the involvement exceeds 25% of the articular surface, it becomes necessary to consider the utilization of either a non-locked or locked plate to provide reinforcement to the posterior malleolus. For posterior fragments that impact 45% or more of the articular surface, it is strongly recommended to apply a locking plate as the preferred method of treatment.
Author Contributions
Conceptualization, V.G. and A.F.; methodology, V.G. and A.F.; software, V.G.; validation, V.G., M.A.B., A.F., R.P.E., F.S.S., L.P.G.F., P.J.L and A.G.S.; formal analysis, V.G. and A.F.; investigation, V.G.; resources, V.G.; data curation, V.G.; writing—original draft preparation, V.G.; writing—review and editing, V.G., M.A.B., A.F., R.P.E., F.S.S., L.P.G.F., P.J.L and A.G.S; visualization, V.G., M.A.B., A.F., R.P.E., F.S.S., L.P.G.F., P.J.L and A.G.S; supervision, V.G., M.A.B. and A.F.; project administration, V.G.; funding acquisition, V.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study did not require ethical approval – biomechanical investigation.
Informed Consent Statement
The study did not involve humans.
Acknowledgments
The authors would like to acknowledge the Research Office of AO Trauma Latin America.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Grass, R.; Herzmann, K.; Biewener, A.; Zwipp, H. Verletzungen der unteren tibiofibularen Syndesmose. Unfallchirurg 2000, 103, 520-532. [CrossRef]
- Vetter, S.Y.; Palesche, N.; Beisemann, N.; Schnetzke, M.; Keil, H.; Kirsch, J.; Grützner, P.A.; Franke, J. Influence of syndesmotic injuries and posterior malleolar ankle fractures on fibula position in the ankle joint: a cadaveric study. Eur J Trauma Emerg Surg 2021, 47, 905-912. [CrossRef]
- Hunt, K.J. Syndesmosis injuries. Curr Rev Musculoskelet Med 2013, 6, 304–312.
- Odak, S.; Ahluwalia, R.; Unnikrishnan, P.; Hennessy, M.; Platt, S. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg 2016, 55, 140-145. [CrossRef]
- Gardner, M.J.; Brodsky, A.; Briggs, S.M.; Nielson, J.H.; Lorich, D.G. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006, 447, 165-171. [CrossRef]
- Mansur, H.; Lucas, P.P.A.; Vitorino, R.C.; Barin, F.R.; Freitas, A.; Battaglion, L.R.; Ramos, L.S. Biomechanical comparison of four different posterior malleolus fixation techniques: a finite element analysis. Foot Ankle Surg 2022, 28, 570-577. [CrossRef]
- Kang, K.S.; Tien, T.N.; Lee, M.C.; Lee, K.Y.; Kim, B.; Lim, D. Suitability of metal block augmentation for large uncontained bone defect in revision Total knee arthroplasty (TKA). J Clin Med 2019, 8, 384. [CrossRef]
- Liu, Y.; Zhang, A.; Wang, C.; Yin, W.; Wu, N.; Chen, H.; Chen, B.; Han, Q.; Wang, J. Biomechanical comparison between metal block and cement-screw techniques for the treatment of tibial bone defects in total knee arthroplasty based on finite element analysis. Comput Biol Med 2020, 125, 104006. [CrossRef]
- Guan, M.; Zhao, J.; Kuang, Y.; Li, G.; Tan, J. Finite element analysis of the effect of sagittal angle on ankle joint stability in posterior malleolus fracture: a cohort study. Int J Surg 2019, 70, 53-59. [CrossRef]
- De Vries, J.S.; Wijgman, A.J.; Sierevelt, I.N.; Schaap, G.R. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 2005, 44, 211-217. [CrossRef]
- Mason, L.W.; Kaye, A.; Widnall, J.; Redfern, J.; Molloy, A. Posterior malleolar ankle fractures: an effort at improving outcomes. JBJS Open Access 2019, 4, e0058.
- Jayatilaka, M.L.T.; Philpott, M.D.G.; Fisher, A.; Fisher, L.; Molloy, A.; Mason, L. Anatomy of the insertion of the posterior inferior tibiofibular ligament and the posterior malleolar fracture. Foot Ankle Int 2019, 40, 1319-1324. [CrossRef]
- Warner, S.J.; Garner, M.R.; Schottel, P.C.; Hinds, R.M.; Loftus, M.L.; Lorich, D.G. Analysis of PITFL injuries in rotationally unstable ankle fractures. Foot Ankle Int 2015, 36, 377-382. [CrossRef]
- Bartoníček, J.; Rammelt, S.; Tuček, M. Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin 2017, 22, 125-145.
- Gardner, M.J.; Demetrakopoulos, D.; Briggs, S.M.; Helfet, D.L.; Lorich, D.G. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int 2006, 27, 788-792. [CrossRef]
- Warner, S.J.; Fabricant, P.D.; Garner, M.R.; Schottel, P.C.; Helfet, D.L.; Lorich, D.G. The measurement and clinical importance of syndesmotic reduction after operative fixation of rotational ankle fractures. J Bone Joint Surg Am 2015, 97, 1935-1944. [CrossRef]
- Andersen, M.R.; Diep, L.M.; Frihagen, F.; Castberg Hellund, J.; Madsen, J.E.; Figved, W. Importance of syndesmotic reduction on clinical outcome after syndesmosis injuries. J Orthop Trauma 2019, 33, 397-403. [CrossRef]
- Sagi, H.C.; Shah, A.R.; Sanders, R.W. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma 2012, 26, 439-443. [CrossRef]
- Fitzpatrick, D.C.; Otto, J.K.; McKinley, T.O.; Marsh, J.L.; Brown, T.D. Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma 2004, 18, 271-278. [CrossRef]
- Hartford, J.M.; Gorczyca, J.T.; McNamara, J.L.; Mayor, M.B. Tibiotalar contact area. Contribution of posterior malleolus and deltoid ligament. Clin Orthop Relat Res 1995, (320), 182-187.
- Irwin, T.A.; Lien, J.; Kadakia, A.R. Posterior malleolus fracture. J Am Acad Orthop Surg, 2013, 21, 32-40.
- Macko, V.W.; Matthews, L.S.; Zwirkoski, P.; Goldstein, S.A. The joint-contact area of the ankle. The contribution of the posterior malleolus. J Bone Joint Surg Am 1991, 73, 347-351. [CrossRef]
- Mason, L.W.; Marlow, W.J.; Widnall, J.; Molloy, A.P. Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int 2017, 38, 1229-1235. [CrossRef]
- Augat, P.; Hast, M.W.; Schemitsch, G.; Heyland, M.; Trepczynski, A.; Borgiani, E.; Russow, G.; Märdian, S.; Duda, G.N.; Hollensteiner, M.; Bottlang, M.; Schemitsch, E.H. Biomechanical models: key considerations in study design. OTA Int 2021, 4, e099(1-6). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).