1. Introduction
The observation of persons in the acute phase of ischemic stroke (IS) during the period from the beginning of hospitalization to the moment of standing up to vertical positions allowed to select a group of persons whose spontaneous motor activity stood out from the typical clinical picture of the hemiplegia syndrome. It has been noticed that persons from this group have tendency to shift the body weight toward more affected side (MAS) in sitting which makes it more difficult for them to develop a stable upright position. An additional symptom noticed in these persons, that makes the re-education of postural function difficult, was the tendency to move the less affected upper extremity (LAUE) and/or the less affected lower extremity (LALE) – not covered by the neurological syndrome. These motor behaviors were also observed in the supine at the beginning of the persons' hospitalization. An additional interesting symptom presented by these persons was typical asymmetry in supine. Aims of this study were to describe and characterize the phenomenon of overactivity of less affected side (OLAS) in persons with acute IS and to creative a predictive model for the occurrence of OLAS.
2. Materials and Methods
The study group consists of persons suffered from first-time IS confirmed in MRI or TC. Persons with focal injury in the thalamus or/and cerebellum with another neurological disease in persons’ history and with loss of conscious incident during hospitalization were excluded from the observation.
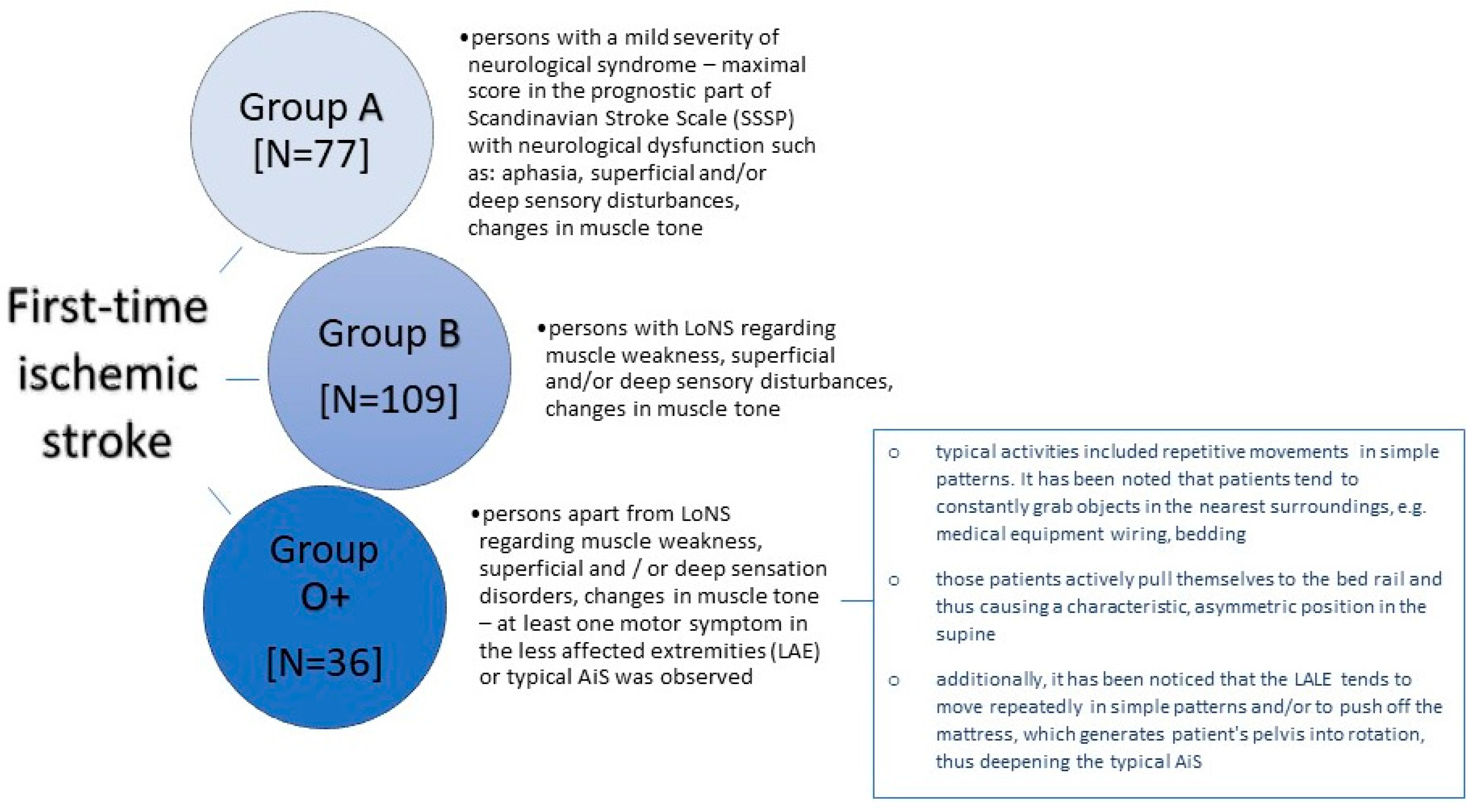
The research was carried out in the years 2020-2021 at the Department of Neurology, Faculty of Medicine and Dentistry, Medical University of Warsaw, located at the Bielański Hospital. The research process collected data from 125 women (56%) and 97 men (44%). The average age of the persons was 71.82 ± 14.27 years and ranged from 29 to 99 years. Persons with first-time IS, on the first day of the physiotherapeutic evaluation were divided into 3 groups depending on their symptoms –
Figure 1.
2.1. Methodology
Persons were assessed on the following baseline parameters: possibility to move against gravity force of the trunk muscles according to Trunk Control Test (TCT) [
1], extremities according to the prognostic part of Scandinavian Stroke Scale (SSSP) [
2], deep sensation, and tactile sensation of the affected limbs, muscle tone in the limbs, hemi neglect (tested by the bedside half-string test). Information about the length of hospitalization, possible death, occurrence of potential predictive for OLAS symptoms – asymmetry in supine (AiS), tendency to move LAUE, tendency do move LALE – were assessed. Moreover, it was marked on which day of hospitalization the patient reached sitting and standing position for the first time. Listed parameters were assessed on the first day of physiotherapeutic assessment – the earliest day when the physiotherapist could examine the patient. If a patient was admitted to the ward on Friday evening, he was assessed on Monday morning. Weeks that included holidays and extended weekends were excluded from follow-up, and no persons were recruited for the study on those days.
2.2. Study design
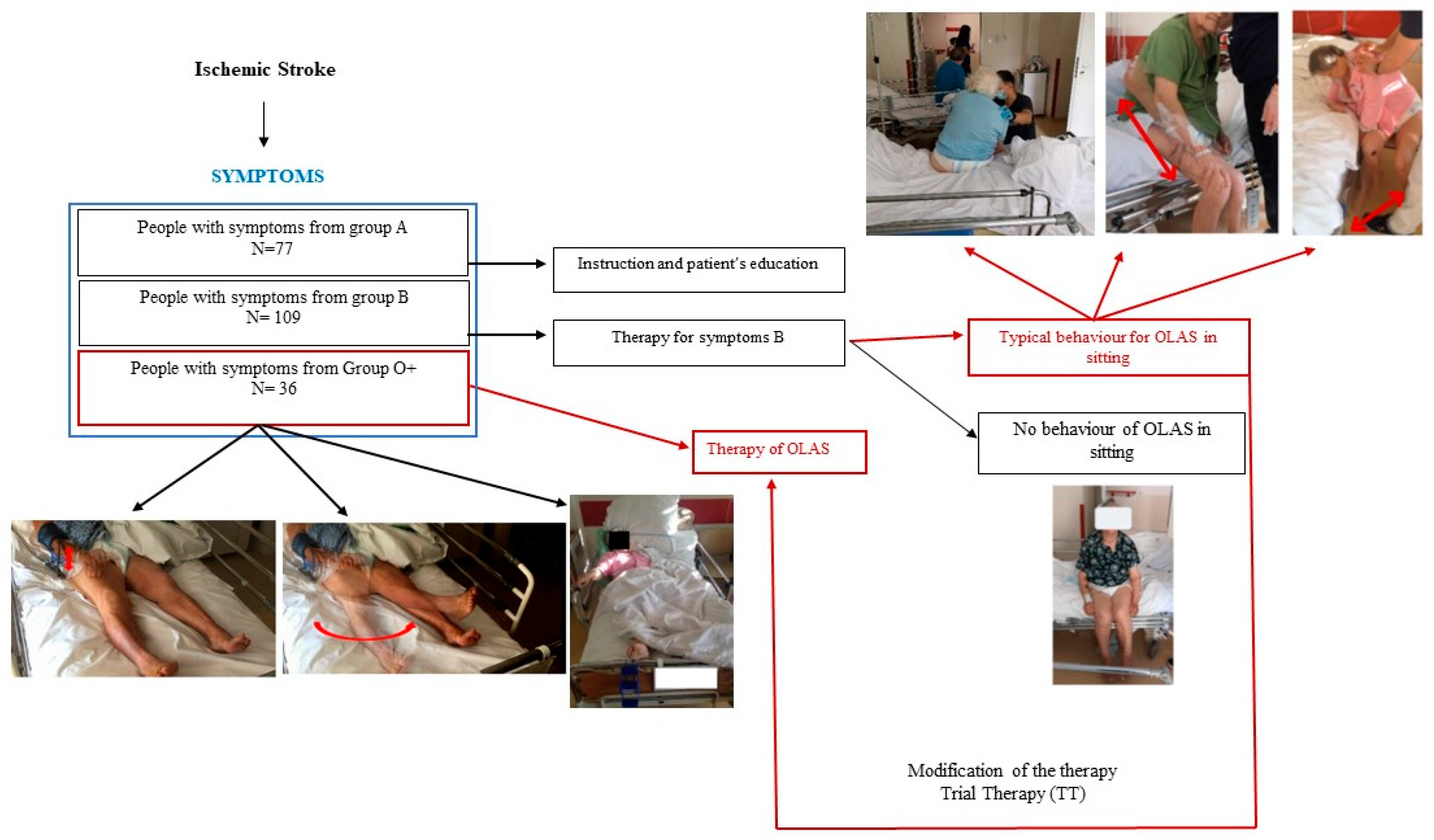
Persons underwent therapy depending on neurological symptoms. The A group underwent health education mainly regarding the possibility of performing physical exercises. The B group underwent standard therapy conducted in accordance with the guidelines of the European Stroke Organization i.e. sensory stimulation in the case of sensory disorders, positioning on the more affected side to prevent shoulder subluxation, strength training in the case of muscle weakness. The therapy was performed once a day apart from Saturday and Sunday. Each session lasted 20-30 minutes. If the patient demonstrated the symptoms of OLAS – weightbearing into MAS and motor activity of the less affected extremities (LAE) – in a higher position than lying in the bed (at least sitting) trial therapy (TT) was performed – described below. TT based on the selected neurophysiological schools techniques was created by the researchers. If such stimulation caused the patient to regain symmetry, he was designated as OLAS and the patient was included in the statistical analysis as such. Described study schema was shown at the
Figure 2.
Persons in the O+ group underwent the therapy once a day (apart from Saturday and Sunday) and took lasting 20 to 30 minutes. The main difference between standard therapy and the TT of persons with symptoms of OLAS was, that at the initial phase of the physiotherapeutic stimulation was focused on the less affected side (LAS) – mainly by loading it. TT was shown at the
Figure 3.
3. Results
According to the study design none of the persons from the group A – Table 1. – had finally presented OLAS and they were excluded from the further analysis. These persons have suffered from a mild neurological syndrome, so further analysis comparing persons with and without OLAS could generate overestimated differences between them.
Table 1.
The final number of persons with and without OLAS in each group.
Table 1.
The final number of persons with and without OLAS in each group.
| Group |
n |
% of group |
% of subgroup (A / B / O+) |
| |
77 |
34.7 |
|
| No OLAS |
77 |
34.7 |
100.0 |
| OLAS |
0 |
0.0 |
0.0 |
| B |
109 |
49.1 |
|
| No OLAS |
98 |
44.1 |
89.9 |
| OLAS |
11 |
5.0 |
10.1 |
| O+ |
36 |
16.2 |
|
| No OLAS |
6 |
2.7 |
16.7 |
| OLAS |
30 |
13.5 |
83.3 |
3.1. Baseline data analysis
Baseline neurological and selected symptoms typical for OLAS data have been compared and analysed. The results have been presented in
Table 2. Data are shown as n (% of OLAS group/no OLAS group) unless otherwise noted. Odds ratio (OR) noted for categorical
Table 2.
Comparison of participants’ baseline data between persons with and without OLAS. UE – upper extremity, LE – lower extremity.
Table 2.
Comparison of participants’ baseline data between persons with and without OLAS. UE – upper extremity, LE – lower extremity.
| variable |
OLAS |
no OLAS |
OR (95% CI) |
p |
| sex, woman |
10 (24.4) |
37 (35.6) |
|
0.069 |
| sex, men |
31 (75.6) |
67 (64.4) |
|
|
| age, median, (Q1;Q3) |
82 (75.00;89.00) |
72 (64.50;82.50) |
|
<0.001 |
| IS right hemisphere |
15 (36.6) |
57 (54.8) |
|
0.208 |
| IS left hemisphere |
24 (63.4) |
47 (45.2) |
|
<0.001 |
| SSSP, median (Q1;Q3) |
10.00 (6.00;14.00) |
20.00 (17.00;22.00) |
|
<0.001 |
| TCT, median (Q1;Q3) |
0.00 (0.00;24.00) |
87.00 (49.00;88.00) |
|
<0.001 |
| Muscle strength UE, median (Q1;Q3) |
0.00 (0.00;2.00) |
5,00 (5.00;6.00) |
|
<0.001 |
| Muscle strength LE, median (Q1;Q3) |
2.00 (0.00;4.00) |
5.00 (4.00;5.00) |
|
<0.001 |
| Hemineglect |
7 (36.8) |
2 (1.9) |
27.13 (5.04;145.9) |
<0.001 |
| Increased muscle tone UE |
8 (20.0) |
21 (20.2) |
0.99 (0.39;2.46) |
0.183 |
| Decreased muscle tone UE |
29 (70.7) |
37 (35.6) |
4.37 (1.99;9.58) |
<0.001 |
| Increased muscle tone LE |
9 (22.0) |
13 (12.5) |
1.97 (0.77;5.043) |
0.158 |
| Increased muscle tone LE |
26 (63.4) |
35 (33.6) |
6.63 (3.04;14.95) |
<0,001 |
| Tactile sensation disturb. UE |
30 (83.3) |
33 (34.02) |
9.69 (3.67;25.63) |
<0.001 |
| Tactile sensation disturb LE |
30 (78.9) |
33 (18.4) |
12.7 (4.78;34.14) |
<0.001 |
| Deep sensation disturb UE |
8 (61.5) |
8 (9.2) |
15.8 (4.17;59.93) |
<0.001 |
| Deep sensation disturb LE |
8 (61.5) |
9 (10.47) |
13.69 (3.68;50.9) |
<0.001 |
| Asymmetry in supine |
26 (63.4) |
7 (6.7) |
24.02 (8.87;65.04) |
<0.001 |
| Tendency to move LAUE |
28 (68.3) |
6 (5.8) |
35.18 (12.25;100.98) |
<0.001 |
| Tendency do move LALE |
17 (41.5) |
3 (2.9) |
23.84 (6.46;87.97) |
<0.001 |
3.2. Length of hospitalization and achievement of a independent sitting position.
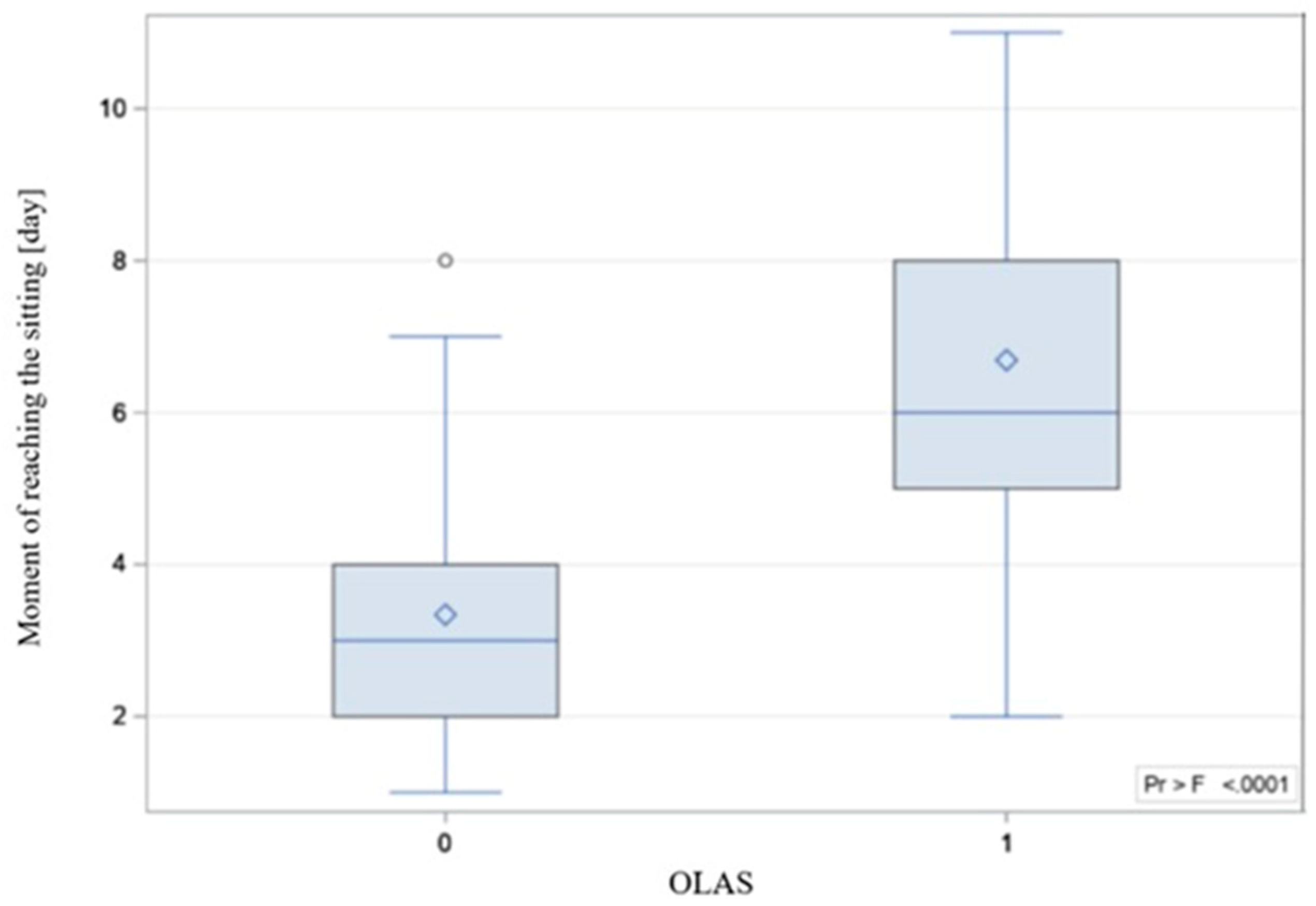
As the another step the differences between the hospitalization time in persons with and without OLAS has been compared. The hospitalization time was significantly longer in persons with OLAS (median = 14 days) compared to persons without OLAS (median = 10 days), p = 0.001. Moreover, it was noticed that some hospitalizations ended with the death. There is significant difference between the compared groups – the rate of deaths was also significantly higher among persons with OLAS (37% vs. 5.8% of persons without OLAS), OR=9.4; p < 0.001. The moment of achieving an active sitting and standing position between persons with OLAS and without OLAS was analyzed. The sitting was achieved by 29 subjects with OLAS (71%) compared to 97 subjects without OLAS (93%), p < 0.001. A visual comparison of the data in the box plot form is shown in
Figure 4.
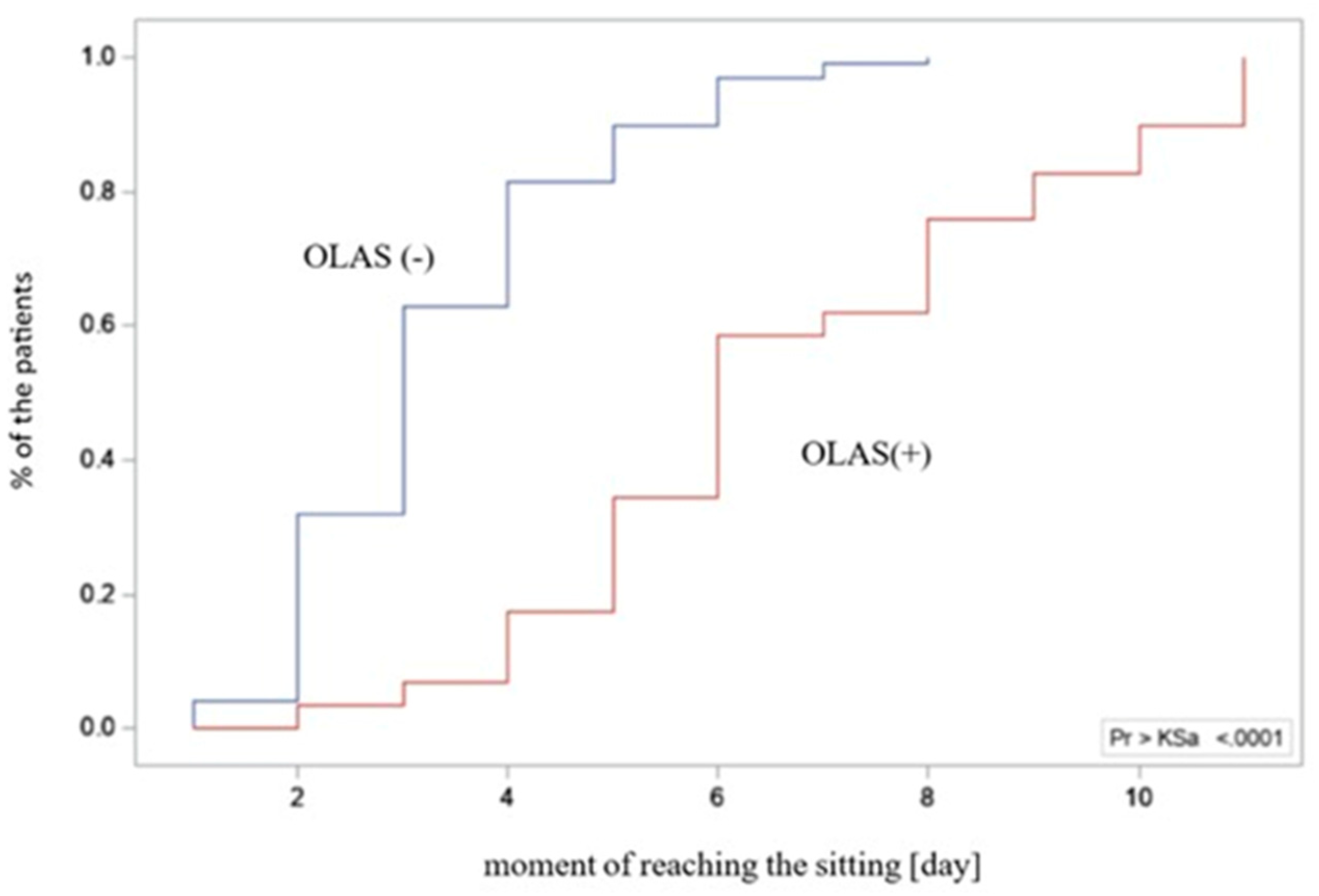
Figure 5 presents an empirical distribution of data showing proportional differences between the groups in the collected data on the time of verticalization to sit on the edge of the bed. The standing position was achieved by 15 subjects with OLAS (37%), compared to 92 subjects without OLAS (88.5%), p < 0.001. Data on the moment of reaching the sitting and standing position have been presented in
Table 3.
Afterwards data regarding the initial attempt of sitting has been analyzed. 35 persons showed a typical asymmetry with a shift of body weight to the MAS. It was checked which variants of symptoms occurred most often, and whether they differed significantly from each other. A summary of all observed combinations of symptoms is presented in
Table 4. It should be noted that in 4 persons typical OLAS behavior (difficulty in weightbearing to the LAS) was observed while standing.
3.3. The predictive model creation
In the next step, it was checked how many of the 35 persons who presented typical symptoms in sitting reacted positively to the TT. 29 persons (83%) who presented asymmetry in sitting or asymmetry in sitting with coexisting LAUE or/and LALE motor activity underwent TT. From this group, 23 persons (79%) reacted positively to the TT, the remaining 6 persons (21%) did not achieve positive effect, p = 0.005.
In the last step, in order to check whether baseline AiS or a tendency to repetitive movements of LAUE and/or LALE are a significant predictors of occurrence OLAS in sitting, a logistic regression analysis was performed. Only persons who achieved sitting position were included in this analysis. Univariate analysis indicated that each of the considered predictors, analyzed separately, was statistically significant. Effect sizes was shown in the
Table 5.
Then, an attempt was made to create a multidimensional model using the stepwise method and two baseline predictors were included in the final model. The quality of the final multivariate model was assessed using the chi-square likelihood ratio test (p < 0.001) and the Hoshmer-Lemeshow (goodness-of-fit) test (p > 0.999). The results indicate a good fit of the model. Negelkerke's pseudo R2 of 44% was adequate. There was no significant co-correlation between the predictors (VIF values - variance inflation factor was 1.18). The data presented above are summarized in
Table 6.
4. Discussion
Observation of persons in the acute IS in the period from the beginning of hospitalization to the moment of sitting and standing, allowed to select a group of persons whose spontaneous motor activity stood out in comparison to people presenting a typical clinical picture of hemiplegia. Based on the results of this research inspired by the observation of the clinical condition of people in the acute phase of IS, the concept of OLAS was defined. In addition, the most typical symptoms of OLAS were characterized, and it was determined which neurological symptoms coexist with it. It was considered whether, in view of the above, the characteristic motor behaviors observed in persons on the first day of physiotherapeutic assessment could be predictive symptoms for later therapeutic problems in higher positions? To the best of the researchers' knowledge, no work has yet been published with such an approach to the problem of persons in the acute phase of IS.
It was hypothesized that the group of persons presenting baseline symptoms of OLAS (additional movements of the LAE and/or AiS) would be the group that would also be characterized by asymmetry in high positions, and thus – based on observation of the supine position only will allow the diagnosis of OLAS to be made. The results on the motor symptoms of OLAS collected from the analysis at the beginning of hospitalization showed that each symptom typical of OLAS from the index day, analyzed separately, was a significant predictor of the occurrence of OLAS in sitting. An attempt was also made to create a predictive model from more than one typical symptom of OLAS from the index day to check whether adding one significant symptom to another would improve the ability to predict that OLAS would actually occur in the sitting position. The conducted analysis gave the results that the coexistence of LAUE and LALE activity on the first day of physiotherapeutic assessment allows, with a certain probability, to predict the occurrence of OLAS in sitting. A review of the literature on the treatment of people with IS did not provide data with which the obtained result could be compared.
One of the hypotheses was the occurrence of characteristic, reproducible differences in the sitting between persons with OLAS and people with a typical clinical picture of post-stroke hemiplegia. It was noticed that persons from OLAS group have tendency to shift the body weight to MAS, which makes it more difficult for them to develop a stable sitting position, and then - standing. In addition, in the sitting, persons also tended to move their LAE. To check the validity of this hypothesis, the way persons with OLAS presented themselves in a sitting position was examined. It was checked which behaviors in this position appear most often and whether the selected variants of motor behaviors are significantly different from others. Such action was needed to create the definition of OLAS. Of all the symptoms of OLAS in sitting presented by persons, three variants of motor behavior stand out from the statistical point of view. OLAS in the sitting position may be manifested not only by asymmetry of the trunk with a deviation towards MAS. The coexistence of a tendency to move the LAE is also important. Information has been found in the literature on the existence of other possible causes of sitting instability. These include, for example, antigravity muscles weakness, changes in muscle tone, hemineglect, or Pusher Syndrome – PS which, apart from extension and abduction activity of the limbs on the LAS and passive resistance during posture correction, is characterized by tilting to the MAS. However, this is due to a specific reason – such persons incorrectly perceive the position of their body in the frontal plane, defining their position as correct (symmetrical) when it is tilted by 18-20 degrees to the MAS. PS persons (similar to OLAS persons) demonstrate abnormal activity of the LAS, and limited ability to change movement patterns. The clinical Scale for contraversive pushing, in which the occurrence of the mentioned symptoms is evaluated (in contrast to OLAS) solely in the sitting and standing positions, as well as the presence of a lesion in the thalamus as a structural cause of PS mentioned in some sources, indicate the necessity to differentiate between OLAS and PS [
3,
4]. In this study, to ensure that PS was not the cause of sitting asymmetry, persons with a thalamic stroke were excluded from the research. Both OLAS and PS persons tend to shift body weight to the MAS. In persons with PS, pushing activity of LAE typically leads to a fall on the MAS. In PS, the purpose of this behavior is to align the body relative to the vertical midline incorrectly perceived by patient. On the other hand, in OLAS it is probably (as researchers conclude from their clinical practice) due to the patient's feelings – it is more comfortable for the patient to take the weight off the LAS, which is indicated by protesting motor behavior in the situation of hypercorrection and support on the LAE, e.g. in sitting. It should be emphasized, however, that persons with OLAS will allow for positioning to the support on the LAS during therapy, which is much more difficult to achieve in the case of persons with PS. Persons with PS, when trying to hypercorrect to the LAS, react with strong resistance. In the treatment of a patient with the PS, many vertical reference points are needed, while in the case of OLAS, therapeutic activities focus on its extinction by stimulating weighting on the LAS.
Apart from the already mentioned PS, asymmetry in the sitting position may also be caused by weakening of the muscular strength of the limbs and trunk, decreased muscle tone, disorders of superficial and deep sensation, cerebellar syndrome and hemineglect [
5,
6,
7,
8,
9]. Among the assessed neurological symptoms in persons qualified for this study, there were many missing data caused by the lack of the verbal-logical contact with the patient which is necessary to conduct a full neurological examination. For this reason, superficial and deep sensation, or the presence of hemineglect, was impossible to assess in some cases. It is noteworthy that the group of persons diagnosed with OLAS consisted of persons with a significant severity of the neurological syndrome, similar to PS. Statistical analysis of data collected from persons in the second measurement period confirmed that persons with OLAS significantly more often suffered from decreased muscle tone in more affected lower and upper extremity severe paresis or paralysis of the limbs, sensory disturbances, and hemineglect. Therefore, it was considered whether the asymmetry occurring in OLAS may be caused by the above-mentioned disorders, or is even the result of several of them. A similar asymmetry to that observed in OLAS may be presented by persons with deficits in superficial and deep sensation, hemineglect and more severe hemiparesis. Exactly the same symptoms appear to be significantly associated with the behavior of persons with OLAS. However from the available literature, it can be learned that with such disorders, typical asymmetry (with a greater load on the MAS) is possible, however, it occurs less frequently than the opposite pattern - with the body weight shifted the LAS. This would suggest that OLAS is a separate cause of sitting asymmetry. However, it cannot be ruled out that mentioned disorders underlie the behavior of persons in OLAS.
At the stage of study designing, it was hypothesized that persons with OLAS symptoms from the first and second measurement time would also present symptoms of overactivity in the standing. In the standing data were collected from 37% of persons with OLAS. An interesting observation is that 4 persons (9.8%) showed signs of OLAS (strong transfer of body weight to the MAS and inability to weight more affected lower extremity) only in the standing. The data collected from the persons did not show a significant relationship between the occurrence of OLAS in the sitting and the pattern of weighting more affected lower extremity in the standing. This result indicates that persons diagnosed with OLAS in the sitting do not necessarily have problems in the standing. On the other hand, it cannot be said that persons with or without OLAS in sitting will not show the symptoms of OLAS in standing. An issue that requires comment is also the time when it was decided to facilitate the patient to standing position. From the physiotherapy’s point of view persons in the acute IS, before facilitating the standing position, should first regain stability in the sitting. As mentioned earlier, OLAS persons present the problem of trunk instability in sitting. It has been shown that persons with OLAS needed more time to be able to stand correctly and independently.
In purely theoretical terms, it is unclear whether the observed motor activities of the LAE in subjects with OLAS correspond with the hemispheric activity visible on fMRI. According to literature, moving the more affected upper extremity during the acute phase of stroke triggers pathological stimulation in both hemispheres of the brain, while moving the less affected extremity does not have the same effect [
10]. Could the continuous, repetitive movement of LAE, which patients exhibited during their initial physiotherapy assessments, be directed towards "protecting" the damaged hemisphere in the event of significant damage? This study does not provide the researchers with the means to answer this question. However, the mechanism of activation of the brain hemispheres after an ischemic stroke was considered when reflecting on physiotherapy methods. It was noted that movement of the more affected limbs induces pathological stimulation of both brain hemispheres, whereas movement of the less affected extremities (LAE) does not. Scientific reports provide information on physiotherapeutic interventions aimed at determining the impact of such activities on interhemispheric balance. In 2021, N. Salehi et al. published research attempting to answer whether increasing resistance exercises performed by LAUE could restore balance of interhemispheric activity visible in fMRI. Additionally, the study aimed to determine if patients undergoing this therapy would experience greater improvements in the motor functions of their more affected upper extremities compared to patients undergoing standard therapy. The study group exhibited a markedly greater enhancement in muscle strength and efficiency in comparison to the control group. The researchers identified improved interhemispheric balance as the mechanism responsible for enhancing strength in the more affected upper extremity [
11]. It is remarkable that the use of the LAS does not induce any pathological pattern of interhemispheric activity and promotes proper activation, which is encouraging.
In this research it has been assumed that TT is a useful tool in the process of diagnosing OLAS. Persons reacting positively to this therapeutic intervention were diagnosed as OLAS. In everyday physiotherapeutic practice and in the functional diagnostics of each patient – also a patient after a stroke – trial therapy should be used as a tool for programming an individual rehabilitation process. It allows to assess whether the given techniques are acceptable by the patient, constitute a movement challenge at an appropriate level of difficulty for him. Trial therapy is also a valuable element of the rehabilitation program evaluation. The main therapeutic rule based on neurophysiological schools is to reduce asymmetry by shifting weight on the LAS. For the purposes of this study, the TT could be performed when the patient was able to actively, with little help, maintain a sitting position. The therapy was conducted on the patient's bed. In this study, the TT was constructed on the theoretical knowledge, own observations and experience of working with persons. It has not been evaluated for effectiveness. Further analysis is required for a better understanding of OLAS. One of the stages of expanding knowledge about OLAS may be an attempt to modify the trial therapy, also in terms of its impact on overactivity observed in the supine.
5. Conclusions
The study results allows to present the OLAS definition as instability of the trunk in the sitting position with associated characteristic motor activities of less affected limbs. Moreover, predictive symptoms of OLAS were distinguished.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Video S1: Activity of the less affected extremities on the first day of physiotherapeutic evaluation
Author Contributions
Conceptualization, A. Zdrowowicz-Doroz. and J. Stolarski.; methodology, A. Zdrowowicz-Doroz and J. Stolarski.; software: A. Zdrowowicz-Doroz; validation: I. Domitrz and J. Kochanowski; formal analysis, A. Zdrowowicz-Doroz and J. Stolarski and K. Krzysztoń; investigation: A. Zdrowowicz-Doroz, J. Stolarski; resources, A. Zdrowowicz-Doroz.; data curation: A. Zdrowowicz-Doroz and J. Stolarski; writing—original draft preparation, A. Zdrowowicz-Doroz and K.Krzysztoń; writing—review and editing, J. Stolarski K. Krzysztoń, I. Domitrz; visualization, A. Zdrowowicz-Doroz and K. Krzysztoń and J. Stolarski; supervision, I. Domitrz, J. Kochanowski; project administration, A. Zdrowowicz-Doroz and J. Stolarski; funding acquisition, - . All authors have read and agreed to the published version of the manuscript.”
Funding
this research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee – protocol code: AKBE / 99/2020, date of approval 11 of May 2020.
Informed Consent Statement
not applicable.
Data Availability Statement
The data are not publicly available due to lots of sensitive data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Duarte E, Marco E, Muniesa JM, et al. Trunk control test as a functional predictor in stroke patients. J Rehabil Med. Nov 2002;34(6):267-72. [CrossRef]
- Stubbs PW, Mortensen J. Clinimetrics: The Scandinavian Stroke Scale. J Physiother. Apr 2020;66(2):132. [CrossRef]
- Paci M, Macchioni G, Ferrarello F. Treatment approaches for pusher behaviour: a scoping review. Top Stroke Rehabil. Feb 14 2022:1-18. [CrossRef]
- Ticini LF, Klose U, Nägele T, Karnath HO. Perfusion imaging in Pusher syndrome to investigate the neural substrates involved in controlling upright body position. PLoS One. May 29 2009;4(5):e5737. [CrossRef]
- Chen P, Motisi SE, Cording C, Ward I, Jasey NN. Impact of eliminating visual input on sitting posture and head position in a patient with spatial neglect following cerebral hemorrhage: a case report. Physiother Theory Pract. Jul 2021;37(7):852-861. [CrossRef]
- Roelofs JMB, van Heugten K, de Kam D, Weerdesteyn V, Geurts ACH. Relationships Between Affected-Leg Motor Impairment, Postural Asymmetry, and Impaired Body Sway Control After Unilateral Supratentorial Stroke. Neurorehabil Neural Repair. Nov 2018;32(11):953-960. [CrossRef]
- Tasseel-Ponche S, Yelnik AP, Bonan IV. Motor strategies of postural control after hemispheric stroke. Neurophysiol Clin. Nov 2015;45(4-5):327-33. [CrossRef]
- Ting DS, Pollock A, Dutton GN, et al. Visual neglect following stroke: current concepts and future focus. Surv Ophthalmol. Mar-Apr 2011;56(2):114-34. [CrossRef]
- Ramaswamy S, Rosso M, Levine SR. Body Lateropulsion in Stroke: Case Report and Systematic Review of Stroke Topography and Outcome. Journal of Stroke and Cerebrovascular Diseases. 2021;30(5):105680.
- Grefkes C., Nowak D. A., Eickhoff S. B., Dafotakis M., Küst J., Karbe H Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Ann Neurol 2008 Vol. 63 Issue 2 Pages 236-46. [CrossRef]
- Salehi Dehno N., Kamali F., Shariat A. and Jaberzadeh S. Unilateral Strength Training of the Less Affected Hand Improves Cortical Excitability and Clinical Outcomes in Patients With Subacute Stroke: A Randomized Controlled Trial. Arch Phys Med Rehabil 2021 Vol. 102 Issue 5 Pages 914-924. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).