Submitted:
23 October 2023
Posted:
02 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
2.3. Data Source and Outcome Definition
2.4. Data Treatment
2.5. Statistical Analyses
2.6. Ethical Approval
3. Results
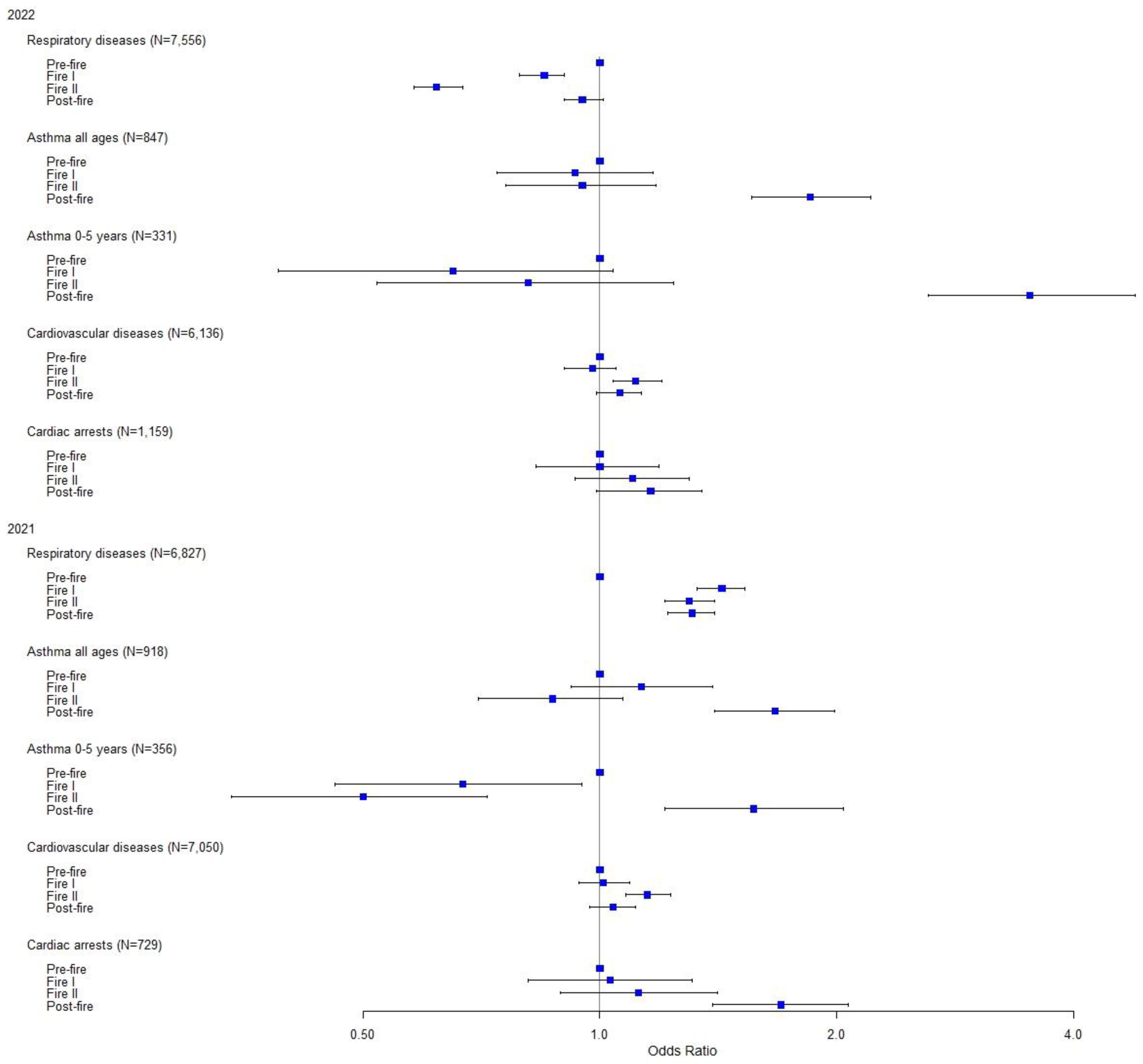
3.1. Outcome-Specific Associations between Time Periods in 2022 and 2021
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications for Research and Practice
5. Conclusions
References
- Organization, WH. Wildfires [Internet]: World Health Organization; [date unknown]. Available online: https://www.who.int/health-topics/wildfires#tab=tab_1.
- Forecasts ECfM-RW. Air quality, climate change and public health [Internet]: European Centre for Medium-Range Weather Forecasts; [date unknown]. Available online: https://stories.ecmwf.int/air-quality-climate-change-and-public-health/index.html.
- Copernicus. Air quality [Internet]: Copernicus; [date unknown]. Available online: https://atmosphere.copernicus.eu/air-quality.
- ESOTC 2022 Europe Wildfires [Internet] [date unknown]. Available online: https://climate.copernicus.eu/esotc/2022/wildfires.
- Agency USEP. Why Wildfire Smoke is a Health Concern [Internet]: United States Environmental Protection Agency; 2022. Available online: https://www.epa.gov/wildfire-smoke-course/why-wildfire-smoke-health-concern.
- Agency USEP. Health and Environmental Effects of Particulate Matter (PM) [Internet]: United States Environmental Protection Agency; 2022. Available online: https://www.epa.gov/pm-pollution/health-and-environmental-effects-particulate-matter-pm.
- Chen, G.; Guo, Y.; Yue, X.; Tong, S.; Gasparrini, A.; Bell, M.L.; et al. Mortality risk attributable to wildfire-related PM2·5 pollution: a global time series study in 749 locations. Lancet Planet. Health 2021, 5, e579–e87. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Yu, P.; Abramson, M.J.; Johnston, F.H.; Samet, J.M.; Bell, M.L.; et al. Wildfires, Global Climate Change, and Human Health. N. Engl. J. Med. 2020, 383, 2173–2181. [Google Scholar] [CrossRef] [PubMed]
- How the EU is preparing for the 2023 wildfire season [Internet]: European Civil Protection and Humanitarian Aid Operations; 2023. Available online: https://civil-protection-humanitarian-aid.ec.europa.eu/news-stories/stories/how-eu-preparing-2023-wildfire-season_en.
- Service CAM. Euorpe´s summer wildfire emissions highest in 15 years [Internet]: Euorpe´s summer wildfire emissions highest in 15 years [Internet]; 2022. Available online: https://atmosphere.copernicus.eu/europes-summer-wildfire-emissions-highest-15-years.
- Grant, E.; Runkle, J.D. Long-term health effects of wildfire exposure: A scoping review. J. Clim. Chang. Health 2022, 6, 100110. [Google Scholar] [CrossRef]
- Programme UNE. Number of wildfires to rise by 50% by 2100 and governments are not prepared, experts warn [Internet]: United Nations Environment Programme; 2022. Available online: https://www.unep.org/news-and-stories/press-release/number-wildfires-rise-50-2100-and-governments-are-not-prepared.
- EGUsphere. Impact of Landes forest fires on air quality in France during the summer 2022 [Internet]: EGUsphere; 2023. Available online: https://egusphere.copernicus.org/preprints/2023/egusphere-2023-421/egusphere-2023-421.pdf.
- Monde, L. France's unprecedented summer of wildfires, in maps and graphs [Internet]: Le Monde; 2022. Available online: https://www.lemonde.fr/en/les-decodeurs/article/2022/08/25/fires-in-france-maps-and-graphs-to-visualize-an-unprecedented-summer_5994672_8.html.
- Youssouf, H.; Liousse, C.; Roblou, L.; Assamoi, E.M.; Salonen, R.O.; Maesano, C.; et al. Quantifying wildfires exposure for investigating health-related effects. Atmos. Environ. 1994 2014, 97, 239–251. [Google Scholar] [CrossRef]
- Black, C.; Tesfaigzi, Y.; Bassein, J.A.; Miller, L.A. Wildfire smoke exposure and human health: Significant gaps in research for a growing public health issue. Environ. Toxicol. Pharmacol. 2017, 55, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Borchers Arriagada, N.; Horsley, J.A.; Palmer, A.J.; Morgan, G.G.; Tham, R.; Johnston, F.H. Association between fire smoke fine particulate matter and asthma-related outcomes: Systematic review and meta-analysis. Environ. Res. 2019, 179 Pt A, 108777. [Google Scholar] [CrossRef]
- Navarro, K.M.; Kleinman, M.T.; Mackay, C.E.; Reinhardt, T.E.; Balmes, J.R.; Broyles, G.A.; et al. Wildland firefighter smoke exposure and risk of lung cancer and cardiovascular disease mortality. Environ. Res. 2019, 173, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.-S.; Falter, K.; Meyer, P.; Mott, J.; Gwynn, C. Risk factors associated with clinic visits during the 1999 forest fires near the Hoopa Valley Indian Reservation, California, USA. Int. J. Environ. Health Res. 2009, 19, 315–327. [Google Scholar] [CrossRef]
- Delfino, R.J.; Brummel, S.; Wu, J.; Stern, H.; Ostro, B.; Lipsett, M.; et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 2009, 66, 189–197. [Google Scholar] [CrossRef]
- Finlay, S.E.; Moffat, A.; Gazzard, R.; Baker, D.; Murray, V. Health impacts of wildfires. PLoS Curr. 2012, 4, e4f959951cce2c. [Google Scholar] [CrossRef]
- Dohrenwend, P.B.; Le, M.V.; Bush, J.A.; Thomas, C.F. The impact on emergency department visits for respiratory illness during the southern california wildfires. West. J. Emerg. Med. 2013, 14, 79–84. [Google Scholar] [CrossRef]
- Tham, R.; Erbas, B.; Akram, M.; Dennekamp, M.; Abramson, M.J. The impact of smoke on respiratory hospital outcomes during the 2002-2003 bushfire season, Victoria, Australia. Respirology 2009, 14, 69–75. [Google Scholar] [CrossRef]
- Viswanathan, S.; Eria, L.; Diunugala, N.; Johnson, J.; McClean, C. An Analysis of Effects of San Diego Wildfire on Ambient Air Quality. J. Air Waste Manag. Assoc. 1995 2006, 56, 56–67. [Google Scholar] [CrossRef]
- Hutchinson, J.A.; Vargo, J.; Milet, M.; French, N.H.F.; Billmire, M.; Johnson, J.; et al. The San Diego 2007 wildfires and Medi-Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: An observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med. 2018, 15, e1002601. [Google Scholar] [CrossRef]
- Reid, C.E.; Maestas, M.M. Wildfire smoke exposure under climate change: impact on respiratory health of affected communities. Curr. Opin. Pulm. Med. 2019, 25, 179–187. [Google Scholar] [CrossRef]
- Liu, J.C.; Wilson, A.; Mickley, L.J.; Dominici, F.; Ebisu, K.; Wang, Y.; et al. Wildfire-specific Fine Particulate Matter and Risk of Hospital Admissions in Urban and Rural Counties. Epidemiology 2017, 28, 77–85. [Google Scholar] [CrossRef]
- Kunzli, N.; Avol, E.; Wu, J.; Gauderman, W.J.; Rappaport, E.; Millstein, J.; et al. Health Effects of the 2003 Southern California Wildfires on Children. Am. J. Respir. Crit. Care Med. 2006, 174, 1221–1228. [Google Scholar] [CrossRef]
- Rappold, A.G.; Cascio, W.E.; Kilaru, V.J.; Stone, S.L.; Neas, L.M.; Devlin, R.B.; et al. Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ. Health 2012, 11, 71. [Google Scholar] [CrossRef] [PubMed]
- Schranz, C.I.; Castillo, E.M.; Vilke, G.M. The 2007 San Diego Wildfire Impact on the Emergency Department of the University of California, San Diego Hospital System. Prehospital Disaster Med. 2010, 25, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.B.; Brauer, M.; MacNab, Y.C.; Kennedy, S.M. Three Measures of Forest Fire Smoke Exposure and Their Associations with Respiratory and Cardiovascular Health Outcomes in a Population-Based Cohort. Environ. Health Perspect. 2011, 119, 1266–1271. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.; Copes, R.; Fisk, R.; Joy, R.; Chan, K.; Brauer, M. Population Health Effects of Air Quality Changes Due to Forest Fires in British Columbia in 2003: Estimates from Physician-visit Billing Data. Can. J. Public Health 2006, 97, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Elliott, C.T.; Henderson, S.B.; Wan, V. Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires. Environ. Health 2013, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Johnston, F.H.; Kavanagh, A.M.; Bowman, D.M.J.S.; Scott, R.K. Exposure to bushfire smoke and asthma: an ecological study. Med. J. Aust. 2002, 176, 535–538. [Google Scholar] [CrossRef] [PubMed]
- Hanigan, I.C.; Johnston, F.H.; Morgan, G.G. Vegetation fire smoke, indigenous status and cardio-respiratory hospital admissions in Darwin, Australia, 1996-2005: a time-series study. Environ. Health 2008, 7, 42. [Google Scholar]
- Johnston, F.H.; Bailie, R.S.; Pilotto, L.S.; Hanigan, I.C. Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health 2007, 7, 240. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.L.; Hanigan, I.C.; Morgan, G.G.; Henderson, S.B.; Johnston, F.H. Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994–2007. Aust. N. Zealand J. Public Health 2013, 37, 238–243. [Google Scholar] [CrossRef]
- Morgan, G.; Sheppeard, V.; Khalaj, B.; Ayyar, A.; Lincoln, D.; Jalaludin, B.; et al. Effects of Bushfire Smoke on Daily Mortality and Hospital Admissions in Sydney, Australia. Epidemiology 2010, 21, 47–55. [Google Scholar] [CrossRef]
- Dennekamp, M.; Straney, L.D.; Erbas, B.; Abramson, M.J.; Keywood, M.; Smith, K.; et al. Forest Fire Smoke Exposures and Out-of-Hospital Cardiac Arrests in Melbourne, Australia: A Case-Crossover Study. Environ. Health Perspect. 2015, 123, 959. [Google Scholar] [CrossRef]
- Haikerwal, A.; Akram, M.; Del Monaco, A.; Smith, K.; Sim, M.R.; Meyer, M.; et al. Impact of Fine Particulate Matter (PM2.5) Exposure During Wildfires on Cardiovascular Health Outcomes. J. Am. Heart Assoc. 2015, 4. [Google Scholar] [CrossRef]
- Johnston, F.; Hanigan, I.; Henderson, S.; Morgan, G.; Bowman, D. Extreme air pollution events from bushfires and dust storms and their association with mortality in Sydney, Australia 1994–2007. Environ. Res. 2011, 111, 811–816. [Google Scholar] [CrossRef]
- Cohen, O.; Shapira, S.; Furman, E. Long-Term Health Impacts of Wildfire Exposure: A Retrospective Study Exploring Hospitalization Dynamics Following the 2016 Wave of Fires in Israel. Int. J. Environ. Res. Public Health 2022, 19, 5012. [Google Scholar] [CrossRef]
- Gao, Y.; Huang, W.; Yu, P.; Xu, R.; Yang, Z.; Gasevic, D.; et al. Long-term impacts of non-occupational wildfire exposure on human health: A systematic review. Environ. Pollut. 2023, 320, 121041. [Google Scholar] [CrossRef] [PubMed]
- Romanello, M.; Di Napoli, C.; Drummond, P.; Green, C.; Kennard, H.; Lampard, P.; et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 2022, 400, 1619–1654. [Google Scholar] [PubMed]
- Chew, F.T.; Ooi, B.C.; Hui, J.K.S.; Saharom, R.; Goh, D.Y.T.; Lee, B.W. Singapore's haze and acute asthma in children. Lancet 1995, 346, 1427. [Google Scholar] [CrossRef]
- Dennekamp, M.; Abramson, M.J. The effects of bushfire smoke on respiratory health. Respirology 2011, 16, 198–209. [Google Scholar] [CrossRef]
- Chen, H.; Samet, J.M.; Bromberg, P.A.; Tong, H. Cardiovascular health impacts of wildfire smoke exposure. Part. Fibre Toxicol. 2021, 18, 2–22. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Kollanus, V.; Prank, M.; Gens, A.; Soares, J.; Vira, J.; Kukkonen, J.; et al. Mortality due to Vegetation Fire-Originated PM2.5 Exposure in Europe-Assessment for the Years 2005 and 2008. Environ. Health Perspect. 2017, 125, 30–37. [Google Scholar] [CrossRef]
- Sastry, N. Forest Fires, Air Pollution, and Mortality in Southeast Asia. Demography 2002, 39, 1–23. [Google Scholar] [CrossRef]
- Hänninen, O.O.; Salonen, R.O.; Koistinen, K.; Lanki, T.; Barregard, L.; Jantunen, M. Population exposure to fine particles and estimated excess mortality in Finland from an East European wildfire episode. J. Expo. Sci. Environ. Epidemiol. 2009, 19, 414–422. [Google Scholar] [CrossRef]
- Wikipedia. Gironde [Internet]: Wikipedia. Available online: https://en.wikipedia.org/wiki/Gironde.
- FIRE-RES. 2022 Summer fires in the Living Lab in Nouvelle Aquitaine, France 2022: FIRE-RES; 2022. Available online: https://fire-res.eu/2022-summer-fires-in-the-living-lab-in-nouvelle-aquitaine-france/.
- Gironde, France Climate [Internet]: Weather and Climate; [date unknown]. Available online: https://tcktcktck.org/france/gironde.
- Méheut, C. Scenes of Devastation Emerge From a Fire-Ravaged Southwestern France [Internet] 2022. Available online: https://www.nytimes.com/2022/07/19/world/europe/france-wildfires-europe-heat-wave.html.
- Watch, G.F. France, Nouvelle-Aquitaine, Gironde [Internet]: Global Forest Watch; [date unknown]. Available online: https://www.globalforestwatch.org/dashboards/country/FRA/10/7/?category=fires&dashboardPrompts=eyJzaG93UHJvbXB0cyI6dHJ1ZSwicHJvbXB0c1ZpZXdlZCI6WyJkb3dubG9hZERhc2hib2FyZFN0YXRzIiwid2lkZ2V0U2V0dGluZ3MiXSwic2V0dGluZ3MiOnsic2hvd1Byb21wdHMiOnRydWUsInByb21wdHNWaWV3ZWQiOlsiZG93bmxvYWREYXNoYm9hcmRTdGF0cyJdLCJzZXR0aW5ncyI6eyJzaG93UHJvbXB0cyI6dHJ1ZSwicHJvbXB0c1ZpZXdlZCI6W10sInNldHRpbmdzIjp7Im9wZW4iOmZhbHNlLCJzdGVwSW5kZXgiOjAsInN0ZXBzS2V5IjoiIn0sIm9wZW4iOnRydWUsInN0ZXBJbmRleCI6MCwic3RlcHNLZXkiOiJkb3dubG9hZERhc2hib2FyZFN0YXRzIn0sIm9wZW4iOnRydWUsInN0ZXBJbmRleCI6MCwic3RlcHNLZXkiOiJ3aWRnZXRTZXR0aW5ncyJ9LCJzdGVwc0tleSI6IndpZGdldFNldHRpbmdzIiwiZm9yY2UiOnRydWV9&location=WyJjb3VudHJ5IiwiRlJBIiwiMTAiLCI3Il0%3D&map=eyJjZW50ZXIiOnsibGF0Ijo0NC44ODc0NTc1MDQzMjE4MywibG5nIjotMC40NzMwOTc2MTk5OTc5OTQ4fSwiem9vbSI6Ni45NDUwNzk5ODE0OTgzMzcsImNhbkJvdW5kIjpmYWxzZSwiZGF0YXNldHMiOlt7ImRhdGFzZXQiOiJwb2xpdGljYWwtYm91bmRhcmllcyIsImxheWVycyI6WyJkaXNwdXRlZC1wb2xpdGljYWwtYm91bmRhcmllcyIsInBvbGl0aWNhbC1ib3VuZGFyaWVzIl0sImJvdW5kYXJ5Ijp0cnVlLCJvcGFjaXR5IjoxLCJ2aXNpYmlsaXR5Ijp0cnVlfSx7ImRhdGFzZXQiOiJmaXJlLWFsZXJ0cy12aWlycyIsImxheWVycyI6WyJmaXJlLWFsZXJ0cy12aWlycyJdLCJvcGFjaXR5IjoxLCJ2aXNpYmlsaXR5Ijp0cnVlLCJwYXJhbXMiOnsidmlzaWJpbGl0eSI6dHJ1ZSwiYWRtX2xldmVsIjoiYWRtMiJ9LCJ0aW1lbGluZVBhcmFtcyI6eyJzdGFydERhdGVBYnNvbHV0ZSI6IjIwMjMtMDItMjUiLCJlbmREYXRlQWJzb2x1dGUiOiIyMDIzLTA1LTI1Iiwic3RhcnREYXRlIjoiMjAyMy0wMi0yNSIsImVuZERhdGUiOiIyMDIzLTA1LTI1IiwidHJpbUVuZERhdGUiOiIyMDIzLTA1LTI1In19XX0%3D&showMap=true.
- A-M S, S S, Wagemann, F F. Summer 2022: exceptional wildfire season in Europe [Internet]: European Organisation for the Exploitation of Meteorological Satellites; 2022. Available online: https://www.eumetsat.int/summer-2022-exceptional-wildfire-season-europe.
- 2022 European and Mediterranean wildfires [Internet]: Wikipedia; 2022. Available online: https://en.wikipedia.org/wiki/2022_European_and_Mediterranean_wildfires#cite_note-13.
- France: Emergency crews responding to wildfires in Gironde Department as of [Internet]: Crisis24; 2022. 13 July. Available online: https://crisis24.garda.com/alerts/2022/07/france-emergency-crews-responding-to-wildfires-in-gironde-department-as-of-july-13.
- Nouvelle-Aquitaine, A. Communiqué de presse - Feux de forêt en Gironde : recommandations sanitaires aux populations du 22 juillet 2022 2022. Available online: https://www.nouvelle-aquitaine.ars.sante.fr/communique-de-presse-feux-de-foret-en-gironde-recommandations-sanitaires-aux-populations-du-22.
- Nouvelle-Aquitaine, A. Feux de forêts - Impact sanitaire et recommandations 2023. Available online: https://www.nouvelle-aquitaine.ars.sante.fr/feux-de-forets-impact-sanitaire-et-recommandations.
- Gil-Jardine, C.; Chenais, G.; Pradeau, C.; Tentillier, E.; Revel, P.; Combes, X.; et al. Trends in reasons for emergency calls during the COVID-19 crisis in the department of Gironde, France using artificial neural network for natural language classification. Scandinavian journal of trauma, resuscitation and emergency medicine. 2021, 29, 55. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Health effects of wildfire smoke in children and public health tools: a narrative review. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Wildland Fire Research: Health Effects Research [Internet]: United States Environmental Protection Agency; 2023. Available online: https://www.epa.gov/air-research/wildland-fire-research-health-effects-research.
| EMCC Calls | Pre-Fire Period 1/6 - 11/7 |
Fire Period I 12/7 - 9/8 |
Fire Period II 10/8 - 15/9 |
Post-fire Period 16/9 - 31/10 |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| 2022 | ||||||||
| Respiratory diseases | 2,457 | 5.1 | 1,453 | 4.3 | 1,233 | 3.2 | 2,413 | 4.9 |
| Asthma all ages (0-5 yrs) | 197 (58) | 0.4 (0.1) | 127 (26) | 0.4 (0.08) | 148 (37) | 0.4 (0.1) | 375 (210) | 0.8 (0.4) |
| Cardiovascular diseases | 1,684 | 3.5 | 1,141 | 3.4 | 1,478 | 3.9 | 1,833 | 3.7 |
| Cardiac arrests | 309 | 0.6 | 214 | 0.6 | 268 | 0.7 | 368 | 0.7 |
| Other | 43,598 | 90.4 | 30,517 | 91.2 | 35,015 | 91.8 | 44,728 | 89.9 |
| Total | 48,245 | 100.0 | 33,452 | 100.0 | 38,142 | 100.0 | 49,717 | 100.0 |
| 2021 | ||||||||
| Respiratory diseases | 1,484 | 3.0 | 1,599 | 4.2 | 1,675 | 3.8 | 2,069 | 3.9 |
| Asthma all ages (0-5 yrs) | 208 (98) | 0.4 (0.2) | 180 (50) | 0.5 (0.1) | 158 (43) | 0.4 (0.1) | 372 (165) | 0.7 (0.3) |
| Cardiovascular diseases | 1,814 | 3.7 | 1,401 | 3.7 | 1,820 | 4.2 | 2,015 | 3.8 |
| Cardiac arrests | 159 | 0.3 | 125 | 0.3 | 156 | 0.4 | 289 | 0.5 |
| Other | 45,860 | 92.6 | 34,562 | 91.3 | 39,619 | 91.2 | 48,455 | 91.1 |
| Total | 49,525 | 100.0 | 37,867 | 100.0 | 43,428 | 100.0 | 53,200 | 100.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





