Submitted:
04 November 2023
Posted:
06 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Case Report
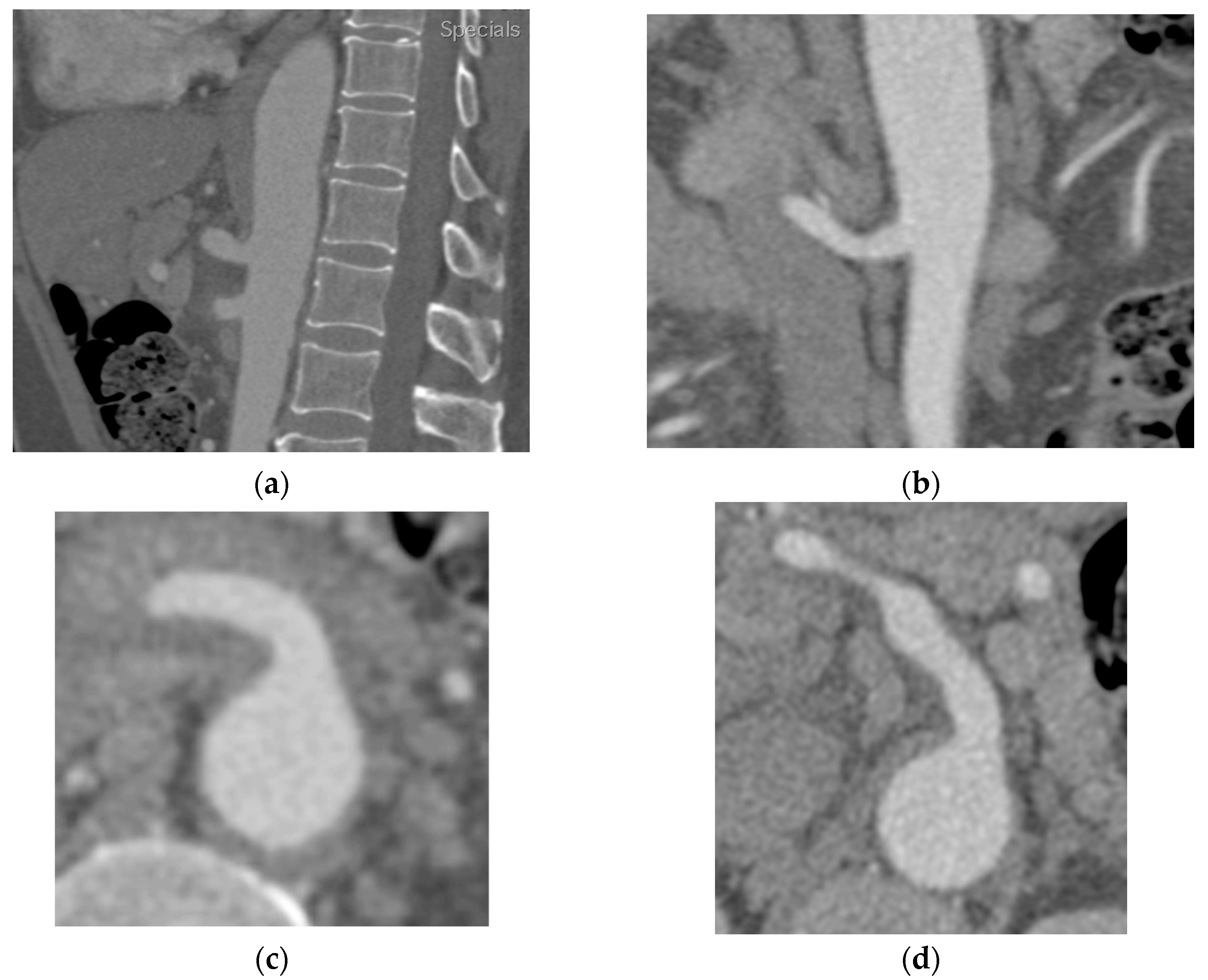
2.1. Case A
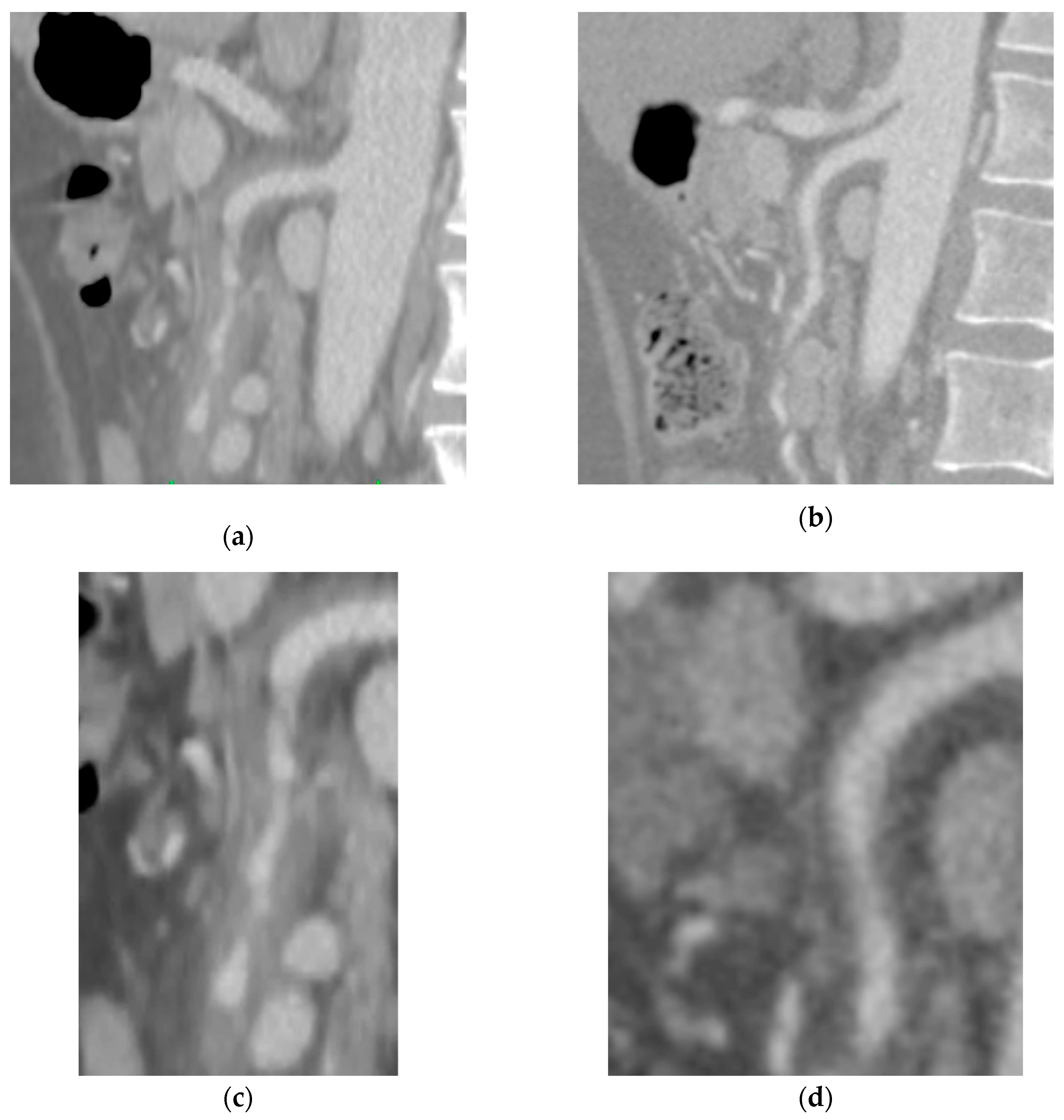
2.2. Case B
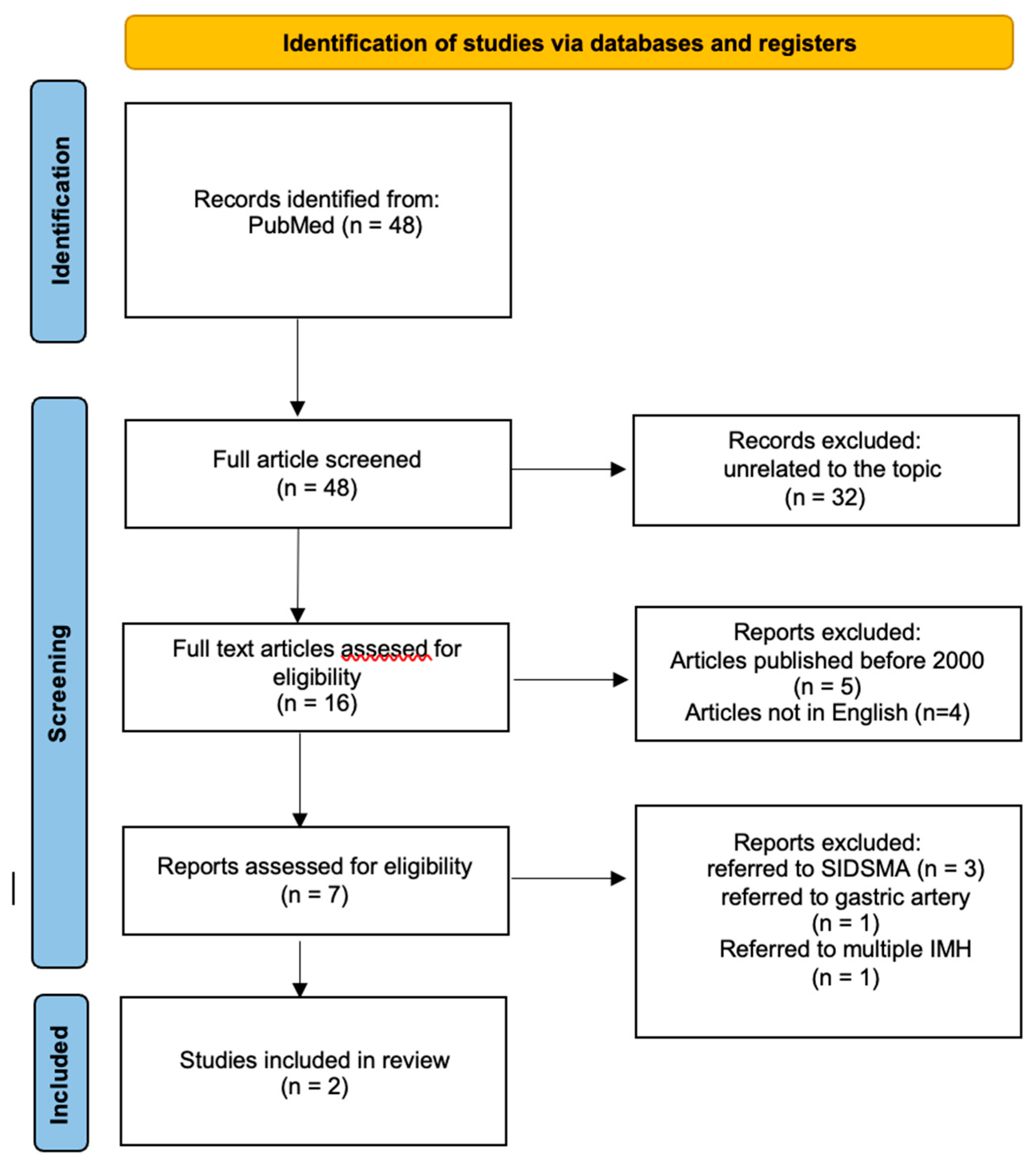
3. Literature Review
3.1. Material and Methods
3.2. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, Y.; Li, T.; Chen, · Yang; Liu, J.; Shi, Q.; Yang, C.; Huang, S.; Chen Zhou, ·; Xiong, · Bin Management of Spontaneous Isolated Intramural Hematoma of the Superior Mesenteric Artery: A Single-Center Experience. 1, 3. [CrossRef]
- Gutschow, S.E.; Walker, C.M.; Martínez-Jiménez, S.; Rosado-de-Christenson, M.L.; Stowell, J.; Kunin, J.R. Emerging Concepts in Intramural Hematoma Imaging. https://doi.org/10.1148/rg.2016150094 2016, 36, 660–674. [CrossRef]
- Nienaber, C.A.; Richartz, B.M.; Rehders, T.; Ince, H.; Petzsch, M. Aortic Intramural Haematoma: Natural History and Predictive Factors for Complications. Heart 2004, 90, 372–374. [CrossRef]
- Kitai, T.; Kaji, S.; Yamamuro, A.; Tani, T.; Kinoshita, M.; Ehara, N.; Kobori, A.; Kim, K.; Kita, T.; Furukawa, Y. Detection of Intimal Defect by 64-Row Multidetector Computed Tomography in Patients with Acute Aortic Intramural Hematoma. Circulation 2011, 124. [CrossRef]
- Nienaber, C.A.; Eagle, K.A. Aortic Dissection: New Frontiers in Diagnosis and Management. Circulation 2003, 108, 628–635. [CrossRef]
- Xiaoq, Z.; Hao, • M; Lin, • L; Jiao, • Y; Zou, • J; Zhang, • X; Hong, • Y Y Clinical and CT Angiographic Follow-Up Outcome of Spontaneous Isolated Intramural Hematoma of the Superior Mesenteric Artery.. [CrossRef]
- Cormier F, L.B.A.A.A.F.JMM. Chirurgie Des Artères Digestives Available online: https://www.em-consulte.com/article/18448/chirurgie-des-arteres-digestives (accessed on 6 May 2023).
- Gouëffic, Y.; Costargent, A.; Dupas, B.; Heymann, M.F.; Chaillou, P.; Patra, P. Superior Mesenteric Artery Dissection: Case Report. J Vasc Surg 2002, 35, 1003–1005. [CrossRef]
- Li, D.L.; He, Y.Y.; Alkalei, A.M.; Chen, X.D.; Jin, W.; Li, M.; Zhang, H.K.; Liang, T.B. Management Strategy for Spontaneous Isolated Dissection of the Superior Mesenteric Artery Based on Morphologic Classification. J Vasc Surg 2014, 59, 165–172. [CrossRef]
- Zettervall, S.L.; Karthaus, E.G.; Soden, P.A.; Buck, D.B.; Ultee, K.H.J.; Schermerhorn, M.L.; Wyers, M.C. Clinical Presentation, Management, Follow-up, and Outcomes of Isolated Celiac and Superior Mesenteric Artery Dissections. J Vasc Surg 2017, 65, 91–98. [CrossRef]
- Zhu, Y.; Peng, Y.; Xu, M.; Wei, Y.; Wu, S.; Guo, W.; Wu, Z.; Xiong, J. Treatment Strategies and Outcomes of Symptomatic Spontaneous Isolated Superior Mesenteric Artery Dissection: A Systematic Review and Meta-Analysis. Journal of Endovascular Therapy 2018, 25, 640–648. [CrossRef]
- Sakamoto, I.; Ogawa, Y.; Sueyoshi, E.; Fukui, K.; Murakami, T.; Uetani, M. Imaging Appearances and Management of Isolated Spontaneous Dissection of the Superior Mesenteric Artery. Eur J Radiol 2007, 64, 103–110. [CrossRef]
- Yun, W.S.; Kim, Y.W.; Park, K.B.; Cho, S.K.; Do, Y.S.; Lee, K.B.; Kim, D.I.; Kim, D.K. Clinical and Angiographic Follow-up of Spontaneous Isolated Superior Mesenteric Artery Dissection. European Journal of Vascular and Endovascular Surgery 2009, 37, 572–577. [CrossRef]
- Yoo, J.; Lee, J.B.; Park, H.J.; Lee, E.S.; Park, S. Bin; Kim, Y.S.; Choi, B.I. Classification of Spontaneous Isolated Superior Mesenteric Artery Dissection: Correlation with Multi-Detector CT Features and Clinical Presentation. Abdominal Radiology 2018, 43, 3157–3165. [CrossRef]
- Maslow, A.; Atalay, M.K.; Sodha, N. Intramural Hematoma. J Cardiothorac Vasc Anesth 2018, 32, 1341–1362. [CrossRef]
- Lei, Y.; Liu, J.; Lin, Y.; Li, H.; Song, W.; Li, Z.; Huang, W.; Chen, S. Relation between Quantity and Quality of Peri-Coronary Epicardial Adipose Tissue and Its Underlying Hemodynamically Significant Coronary Stenosis. 2020. [CrossRef]
- Asakura, H.; Ogawa, H. COVID-19-Associated Coagulopathy and Disseminated Intravascular Coagulation. Int J Hematol 2021, 113, 45–57. [CrossRef]
- Leentjens, J.; van Haaps, T.F.; Wessels, P.F.; Schutgens, R.E.G.; Middeldorp, S. COVID-19-Associated Coagulopathy and Antithrombotic Agents—Lessons after 1 Year. Lancet Haematol 2021, 8, e524–e533. [CrossRef]
- Beyerstedt, S.; Casaro, E.B.; Rangel, É.B. COVID-19: Angiotensin-Converting Enzyme 2 (ACE2) Expression and Tissue Susceptibility to SARS-CoV-2 Infection. European Journal of Clinical Microbiology and Infectious Diseases 2021, 40, 905–919. [CrossRef]
- Hanff, T.C.; Mohareb, A.M.; Giri, J.; Cohen, J.B.; Chirinos, J.A. Thrombosis in COVID-19. Am J Hematol 2020, 95, 1578–1589. [CrossRef]
- Gómez-Mesa, J.E.; Galindo-Coral, S.; Montes, M.C.; Muñoz Martin, A.J. Thrombosis and Coagulopathy in COVID-19. Curr Probl Cardiol 2021, 46, 100742. [CrossRef]
- Mouawad, N.J.; Cuff, R.F.; Hultgren, R.; Chuen, J.; Galeazzi, E.; Wohlauer, M. The Vascular Surgery COVID-19 Collaborative (VASCC). J Vasc Surg 2020, 72, 379–380. [CrossRef]
- Björck, M.; Koelemay, M.; Acosta, S.; Bastos Goncalves, F.; Kölbel, T.; Kolkman, J.J.; Lees, T.; Lefevre, J.H.; Menyhei, G.; Oderich, G.; et al. Editor’s Choice – Management of the Diseases of Mesenteric Arteries and Veins: Clinical Practice Guidelines of the European Society of Vascular Surgery (ESVS). European Journal of Vascular and Endovascular Surgery 2017, 53, 460–510. [CrossRef]
- Isselbacher, E.M.; Preventza, O.; Black, J.H.; Augoustides, J.G.; Beck, A.W.; Bolen, M.A.; Braverman, A.C.; Bray, B.E.; Brown-Zimmerman, M.M.; Chen, E.P.; et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 2022, 146, E334–E482. [CrossRef]
- Cho, B.S.; Lee, M.S.; Lee, M.K.; Choi, Y.J.; Kim, C.N.; Kang, Y.J.; Park, J.S.; Ahn, H.Y. Treatment Guidelines for Isolated Dissection of the Superior Mesenteric Artery Based on Follow-up CT Findings. European Journal of Vascular and Endovascular Surgery 2011, 41, 780–785. [CrossRef]
- Yuan, Z.; Sheng, S.; You, Y.; Li, D.; Wei, Q.; Yan, K.; Wang, J. Relationship Between Morphological Remodeling and Angiographic Types of Spontaneous Isolated Superior Mesenteric Artery Dissection After Conservative Management: Determinant Affecting Serial Radiologic Courses. Front Cardiovasc Med 2022, 9, 1838. [CrossRef]
- Yoshioka, Y.; Yoshioka, K.; Ikeyama, S. Large Gastric Intramural Hematoma Mimicking a Visceral Artery Aneurysm: A Case Report. J Med Case Rep 2018, 12, 1–4. [CrossRef]
- Suzuki, S.; Furui, S.; Kohtake, H.; Sakamoto, T.; Yamasaki, M.; Furukawa, A.; Murata, K.; Takei, R. Isolated Dissection of the Superior Mesenteric Artery: CT Findings in Six Cases.. [CrossRef]
- Sakatani, A.; Doi, Y.; Kitayama, T.; Matsuda, T.; Sasai, Y.; Nishida, N.; Sakamoto, M.; Uenoyama, N.; Kinoshita, K. Pancreaticoduodenal Artery Aneurysm Associated with Coeliac Artery Occlusion from an Aortic Intramural Hematoma. World J Gastroenterol 2016, 22, 4259–4263. [CrossRef]
- DeAnda, A.; Kasirajan, V.; Henry, D.; Myers, S.I. Complete Regression of an Intramural Hematoma of the Aorta after Distal Reperfusion. J Vasc Surg 2005, 42, 149–152. [CrossRef]
- Sakata, N.; Takebayashi, S.; Shimizu, K.; Kojima, M.; Masawa, N.; Suzuki, K.; Takatama, M. A Case of Segmental Mediolytic Arteriopathy Involving Both Intracranial and Intraabdominal Arteries. Pathol Res Pract 2002, 198, 493–497. [CrossRef]
- Ghannam, M.; Ghazaleh, D.; Beran, A.; Miller, B.; Berry, B. Arteriopathy of Unknown Etiology: Pathologic, Radiologic, and Cytogenetic Investigations. American Journal of Case Reports 2019, 20, 1235–1240. [CrossRef]
- Macari, M.; Chandarana, H.; Balthazar, E.; Babb, J. Intestinal Ischemia versus Intramural Hemorrhage: CT Evaluation. American Journal of Roentgenology 2003, 180, 177–184. [CrossRef]
- Bax, M.; Romanov, V.; Junday, K.; Giannoulatou, E.; Martinac, B.; Kovacic, J.C.; Liu, R.; Iismaa, S.E.; Graham, R.M. Arterial Dissections: Common Features and New Perspectives. Front Cardiovasc Med 2022, 9, 1055862. [CrossRef]
- Martin, Z.; Dorairaj, J.; O’Brien, G.C.; Cloete, N.; Haider, S.N.; Colgan, M.P.; McGovern, E.; Meaney, J.; O’Neill, S.M.; Moore, D.J.; et al. Hybrid Repair of a Symptomatic Thoracic Intra-Mural Haematoma. Ir J Med Sci 2012, 181, 381–383. [CrossRef]
- Reddy, N.; Metwalli, Z.A. Ruptured Pancreaticoduodenal Artery Aneurysm Presenting with Duodenal Obstruction. Radiol Case Rep 2019, 14, 568–571. [CrossRef]
- Li, Y.L.; Ye, J.C.; Yancu, H.; Liu, B.; Wang, Y.Z.; Wang, W.J.; Wang, W.; Li, D.; Chang, H.Y. Thoracic Endovascular Aortic Repair for Type B Aortic Dissection Associated with Retrograde Type A Intramural Hematoma. Journal of Vascular and Interventional Radiology 2020, 31, 1334–1341. [CrossRef]
- Abdu, R.W.; Long, G.W.; Baker, D.; Boudiab, E.; Callahan, R.E.; Studzinski, D.M.; Brown, O.W. Intramural Hematoma of the Thoracic Aorta: A Single-Institution, 12-Year Experience. J Vasc Surg 2022, 75, 1872-1881.e1. [CrossRef]
- Mussa, F.F.; Horton, J.D.; Moridzadeh, R.; Nicholson, J.; Trimarchi, S.; Eagle, K.A. Acute Aortic Dissection and Intramural Hematoma: A Systematic Review. JAMA 2016, 316, 754–763. [CrossRef]
- Evangelista, A.; Mukherjee, D.; Mehta, R.H.; O’Gara, P.T.; Fattori, R.; Cooper, J. V.; Smith, D.E.; Oh, J.K.; Hutchison, S.; Sechtem, U.; et al. Acute Intramural Hematoma of the Aorta: A Mystery in Evolution. Circulation 2005, 111, 1063–1070. [CrossRef]
- Kaji, S.; Akasaka, T.; Katayama, M.; Yamamuro, A.; Yamabe, K.; Tamita, K.; Akiyama, M.; Watanabe, N.; Tanemoto, K.; Morioka, S.; et al. Long-Term Prognosis of Patients with Type B Aortic Intramural Hematoma. Circulation 2003, 108 Suppl 1. [CrossRef]
- Sueyoshi, E.; Imada, T.; Sakamoto, I.; Matsuoka, Y.; Hayashi, K. Analysis of Predictive Factors for Progression of Type B Aortic Intramural Hematoma with Computed Tomography. J Vasc Surg 2002, 35, 1179–1183. [CrossRef]
- Vaccari, G.; Caciolli, S.; Calamai, G.; Acquafresca, M.; Montesi, G.; Braconi, L.; Cassai, M.; Perna, A.M. Intramural Hematoma of the Aorta: Diagnosis and Treatment. Eur J Cardiothorac Surg 2001, 19, 170–173. [CrossRef]
- Sundt, T.M. Intramural Hematoma and Penetrating Aortic Ulcer. Curr Opin Cardiol 2007, 22, 504–509. [CrossRef]
- Oderich, G.S.; Kärkkäinen, J.M.; Reed, N.R.; Tenorio, E.R.; Sandri, G.A. Penetrating Aortic Ulcer and Intramural Hematoma. Cardiovasc Intervent Radiol 2019, 42, 321–334. [CrossRef]
- Sundt, T.M. Intramural Hematoma and Penetrating Aortic Ulcer. Curr Opin Cardiol 2007, 22, 504–509. [CrossRef]
| N. (patient) |
Reference | Type of article | Onset symptom | Risk of factors |
|---|---|---|---|---|
| 31 (M/24; F/7) |
Wang, Yingliang et al.[1] | Observational study | -6 (6/31, 19%) asymptomatic with incidental diagnosis -25 (25/31, 81%) gastrointestinal symptoms |
Hypertension 11 (35%) Atherosclerosis, 6 (19%) Diabetes mellitus, 2 (6%) Smoking, 5 (16%) Valvular heart disease, 3 (10%) Coronary arterial disease, 4 (13%) Hyperlipidemia, 2 (6) |
| 24 (M/21; F/3) |
Xiaoq, Z et al. [6] | Retrospective study | -21/24 Gastrointestinal symptoms (abdominal pain) -3/24 asymptomatic (occasional occurrence) |
Hypertension 8 (32%) Coronary artery disease, 1 (4%) History of abdominal surgery, 3 (12%) Current smoker, 3 (12%) |
| Reference | Laboratory data | Instrumental Analysis | Other |
|---|---|---|---|
| Wang, Yingliang et al.[1] | N/A | Computed tomography angiography (CTA): -21 (21/31, 68%) cases with the IMH involving the branches of the SMA (Ileocolic or distal ileal arteries) -10 (10/31, 32%) cases with the IMH limiting to the trunk of SMA. |
CTA or ultrasound images as follow-up at 1 month, 3 months, 6 months and 12 months and every year thereafter |
| Xiaoq, Z et al.[6] | N/A | Computed tomography angiography (CTA): arteries were measured and classified according to anatomic descriptors |
CTA control: 7 days after the initial diagnosis, 1 month, and 6 months after admission. |
| Reference | Treatment Managmment | Outcomes | Use of corticosteroid |
|---|---|---|---|
| Wang, Yingliang et al.[1] | -28 patients (26/31, 87%) of patients were treated conservatively (fasting, pain management, blood pressure control, vasodilator drugs, anticoagulation drugs, anti-aggregant drugs). -3 patients (3/31, 9.67%) underwent endovascular stenting for persistent abdominal pain symptoms |
-1/31 progression of intramural haematoma to penetrating ulcer at CT and underwent stent implantation and coils embolization 1.5 months later due to -1/31 progression from haematoma to dissection 7 months later but remained stable. -27/31 no progression of haematoma -All the patients who had stents implantation (n = 3) maintained a patent vascular lumen and complete absorption of IMH. |
NO |
| Xiaoq, Z et al.[6] | -20\24 Conservative treatment using fasting, pressure control, vasodilators, antiaggregants, anticoagulants (LMWH - enoxaparin; warfarin; rivaroxaban)* -1\24: Exploratory laparotomy + embolectomy + arteriotomy. - 3\24: visceral vessel stenting** |
-15/24 (62.5%) Complete remodeling -4/24 (16.67%) Partial remodeling -2/24 (8.33%) No change -3/24 (12.5%) Dissection remodeling or aneurysm change -22 patients (91.6%) showed angiographic improvement to complete remodelling. |
NO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





