Introduction
Endoscopic biliary stenting represents a cornerstone of interventional gastroenterology, playing a pivotal role in the multifaceted realm of biliary tract pathologies [
1]. This therapeutic modality, facilitated primarily through the use of plastic stents, stands as a reliable and effective intervention for a spectrum of conditions afflicting the biliary system, ranging from obstructive jaundice to choledocholithiasis, and from biliary strictures to various ductal aberrations. The traditional choice of plastic materials for these stents has been driven by the need for short-term deployment, a decision grounded in the awareness of potential complications that could ensue from long-term stent use, including the risk of infection, occlusion, migration, and stent fracture [
2,
3].
In the arc of its evolution, the procedure of biliary stenting has witnessed transformative progress. These advancements have been discernible in the refined materials employed in stent manufacturing, as well as the heightened precision and sophistication of the endoscopic equipment utilized. Yet, amid these notable strides, a persistent challenge endures – the inadvertent neglect or prolonged retention of biliary stents, surpassing their originally intended tenure. This oversight, rather than being an inconsequential lapse, often unfurls a labyrinth of complexities that mandate advanced, and at times, invasive interventions to rectify or manage the situation [
4].
Moreover, it is incumbent upon us to acknowledge the substantial influence of healthcare systems’ structural configurations on the management of biliary stenting. Post-procedural follow-up protocols exhibit striking disparities contingent on the healthcare environment and the resources at its disposal. In settings marked by high patient volumes and strained healthcare resources, exemplified by the hustle and bustle of tertiary care institutions, the likelihood of forgotten or retained stents assumes a heightened prevalence [
5,
6].
The emergence of the COVID-19 pandemic added yet another layer of intricacy to this multifaceted issue [
7]. As healthcare systems grappled with the challenges imposed by the pandemic, the routine follow-up procedures for non-urgent conditions, including the imperative removal of biliary stents, were relegated to a lower rung of priority. While empirical data concerning the direct ramifications of the COVID-19 pandemic on the incidence of forgotten biliary stents is still in its infancy, anecdotal accounts and preliminary investigations hint at a discernible upswing in cases that necessitate intervention due to complications that have unfurled as a consequence of forgotten or retained stents [
8,
9,
10].
It is paramount to grasp the urgency of quantifying the scale of this predicament and meticulously assessing the intertwined clinical outcomes. This is pivotal to the judicious allocation of resources and the formulation of effective treatment strategies. Tertiary care institutions, renowned for their prowess in managing intricate medical cases, serve as veritable crucibles for understanding the intricate patterns and multifaceted outcomes associated with forgotten or retained biliary stents. Additionally, the imperative of identifying prevalent complications and ascertaining the most efficacious pathways for their management assumes paramount importance in the endeavour to optimize patient care and mitigate the associated morbidity and, in a worst-case scenario, mortality [
11].
Hence, the overarching objective of this study is to undertake a comprehensive exploration of the incidence and clinical implications of forgotten plastic biliary stents within the precincts of a tertiary care hospital. A specific emphasis is placed on delineating the demographic and clinical profiles of patients grappling with the conundrum of forgotten or retained stents, scrutinizing the corollary complications such as cholangitis and the formation of common bile duct (CBD) stones. The study seeks to gauge the efficacy of endoscopic retrograde cholangiopancreatography (ERCP) in stent retrieval while simultaneously venturing into the realm of alternative interventions, which may encompass cholangioscopy and surgical procedures. Ultimately, this study aspires to offer nuanced recommendations for the fortification of post-stenting follow-up protocols and the enhancement of management strategies, aimed at mitigating the risks inherently associated with this intricate medical dilemma.
Methodology:
Study Design and Setting:
This Case Series unfolds its narrative within the hallowed halls of Andhra Medical College, in conjunction with the esteemed King George Hospital located in Visakhapatnam. The latter, a tertiary care facility renowned for its proficiency in the field of gastroenterology, provides the backdrop for our scholarly inquiry.
Our investigative journey, methodically spanning a noteworthy duration of eight months, commences its voyage on the inaugural day of January 2022, and concludes its odyssey in the month of August of the same year with KGH/IEC/2022/008 institute ethical number. Within this temporal span, we have sought to unravel the intricacies surrounding forgotten plastic biliary stents, a matter of pressing concern that warrants meticulous exploration.
Patient Selection:
Subjects harbouring the circumstance of forgotten or retained plastic biliary stents were discerned by means of the hospital’s sophisticated electronic medical records system, a meticulous and thorough process.
Inclusion Criteria:
Individuals of 18 years of age and older, A confirmed diagnosis of a retained plastic biliary stent, Diagnosis validation through comprehensive imaging studies, encompassing X-ray, abdominal ultrasound, and MRCP.
Exclusion Criteria:
Patients below the age of 18, Lack of a substantiated diagnosis pertaining to the retention of a plastic biliary stent, Incomplete or insufficient medical records or deficient documentation of imaging, Patients whose imaging studies (including X-ray, ultrasound, and MRCP) are incomplete or unavailable for the verification of retained stent status.
Data Collection:
Data retrieval involved a meticulous examination of electronic medical records, laboratory reports, and in-depth scrutiny of imaging studies for every patient. The variables sought encompassed a spectrum of information, including demographic particulars, the primary indication for stent placement, the temporal interval between stent insertion and patient presentation, the clinical manifestations, and any ensuing complications. To safeguard patient privacy, all data underwent a rigorous anonymization process.
Intervention and Procedures:
The principal approach employed for stent retrieval hinged upon the application of ERCP. Unsuccessful endeavours with ERCP necessitated the recourse to alternative techniques such as the utilization of a cholangioscopy. In instances characterized by heightened complexity, the deliberation extended to options like cholangioscopy or surgical interventions.
Outcome Measures:
Efficacy of ERCP in successfully extracting the stent
Occurrence and nature of complications (e.g., cholangitis, common bile duct stones)
Nature of substitute interventions necessitated (cholangioscopy, surgical procedures)
Duration between the initial stent placement and the identification of complications or the successful stent removal
Statistical Analysis:
In our quest to comprehensively elucidate the demographic and clinical characteristics of the patients under scrutiny, we turned to the judicious application of descriptive statistics. This analytical approach allowed us to distil the essence of continuous variables by articulating them as means and articulating their full range, providing a clear picture of the data’s distribution. On the other hand, categorical variables were eloquently expressed through frequencies and percentages, painting a vivid portrait of their prevalence within our patient cohort. Subsequently, a rigorous logistic regression analysis was conducted, unveiling the variables and factors that bore the potential to prognosticate the likelihood of unsuccessful ERCP attempts. In our pursuit of robust and reliable findings, the threshold for statistical significance was conservatively set at a p-value of less than 0.05.
Ethical Considerations:
At the very core of our study lies an unwavering commitment to the highest ethical standards. Thus, our endeavour was set into motion only after securing the ethical imprimatur of the Institutional Ethics Committee at King George Hospital, Vishakhapatnam, Andhra Pradesh. This ethical oversight not only underscores our dedication to conducting research that upholds the principles of integrity and patient well-being but also ensures that our study aligns with the ethical tenets of medical research. Furthermore, it’s noteworthy that, owing to the retrospective nature of our study and our meticulous measures to protect patient confidentiality through anonymization, the need for individualized informed consent was rightfully waived, affirming that our research adheres to the strictest ethical guidelines while respecting the privacy and autonomy of the patients involved.
Results:
Demographic and Clinical Profile:
Over the span of our meticulously conducted 8-month study, a total of 12 patients came to our attention, individuals grappling with the challenge of forgotten or retained plastic biliary stents. These patients exhibited a median age of 48 years, ranging from 18 to 76 years, casting a broad spectrum. Among them, 7 individuals, constituting 58.3% of the cohort, were female, while the remaining 5, representing 41.7%, were male. The predominant and initial indication for the placement of biliary stents was choledocholithiasis, a prominent feature observed in the majority of cases, encompassing 83.3%, whereas 3 cases, or 25%, were entwined with benign biliary strictures [
Table 1].
Duration and Clinical Presentation:
A temporal chasm, averaging approximately 31.3 months and fluctuating between 13 to 96 months, separated the moment of stent insertion from the subsequent presentation at our institution. Within this temporal dimension, the prevailing clinical tableau unfurled in the form of cholangitis, affecting a notable proportion of the patients, encapsulating 83.3% of the cohort [
Table 2].
Stent Retrieval and Complications:
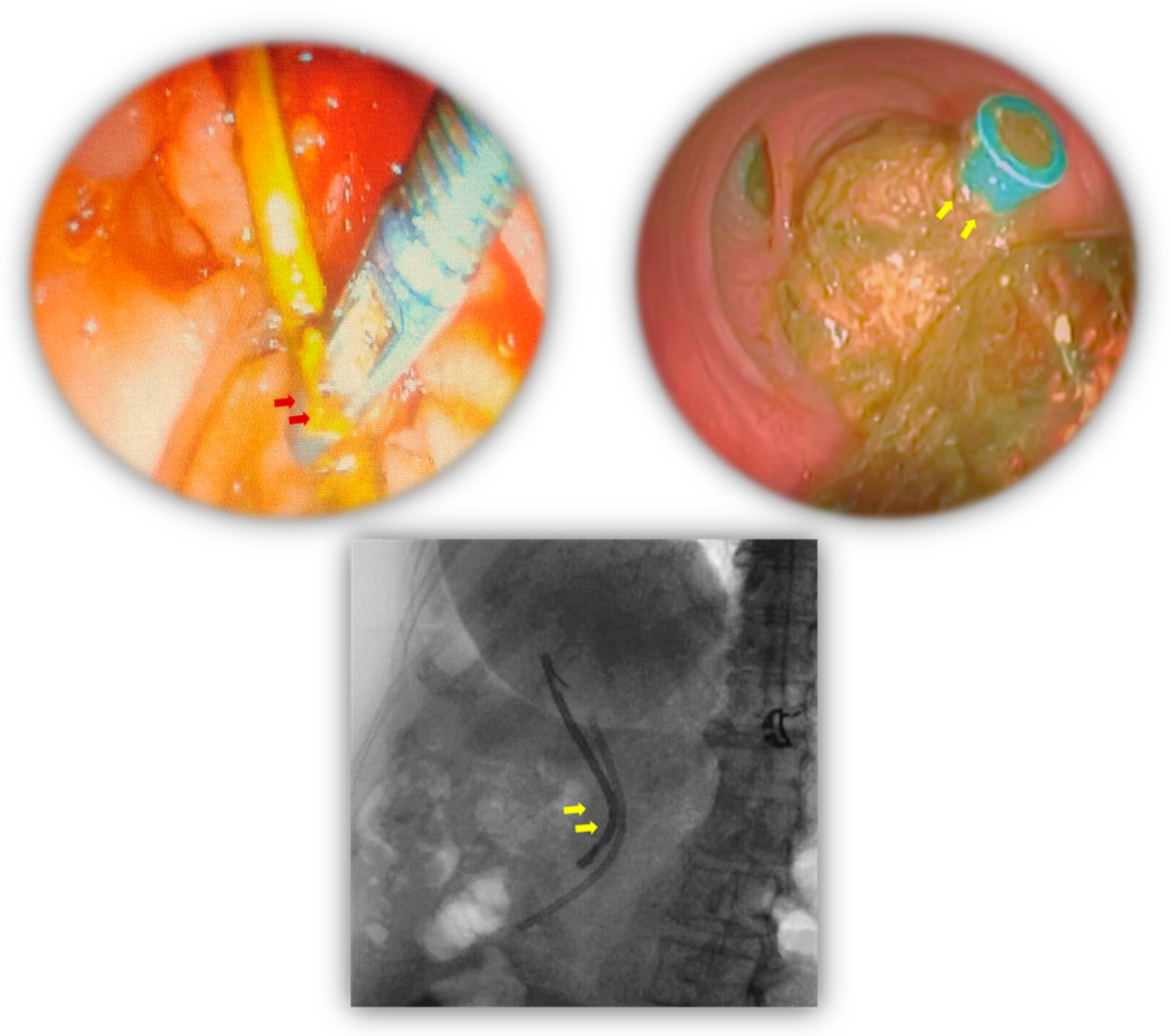
ERCP, initially wielded as the method of choice for the extraction of stents, was successfully executed in 8 patients, heralding an accomplishment rate of 66.6%. However, the path was not devoid of challenges, as complications reared their heads in 4 patients, eventually leading to thwarted ERCP endeavours (
Figure 1). Within this cluster of complications, two patients grappled with fractured distal pigtails, while another faced an obstructed biliary stent, and a fourth patient confronted the perplexing predicament of a fragmented stent that had journeyed into the proximal reaches of the common bile duct (CBD). As a consequence, the management of these four cases demanded the exploration of alternative strategies [
Table 3].
Alternative Intervention Approaches:
Following the encountered complications, diligent efforts were made to retrieve the stents utilizing a cholangioscopy; nevertheless, these endeavours yielded no success. Within this particular subgroup of patients, two individuals achieved resolution through the application of cholangioscopy, a more advanced and intricate procedure. In contrast, the remaining two patients required surgical intervention to ultimately and successfully extract the stents from their biliary tracts [
Table 4].
Outcome Metrics:
The inaugural ERCP-based stent removal success rate was notably etched at 66.6%. The spectrum of complications was dominated by the pervasive presence of cholangitis, a spectre that loomed over 7 cases, closely followed by CBD stones. Among those who grappled with complications, 50% ultimately required advanced interventions that transcended the ambit of ERCP to secure the triumphant removal of the stents.
Complication-Free Survival:
Notably, even in the face of evident complications such as cholangitis and the looming threat of CBD stones, it is striking to observe that the study cohort exhibited a notable absence of mortality. This underscores the remarkable resilience and favourable outcomes observed among the patients, highlighting the resilience and effectiveness of the medical interventions employed [
Table 5].
Discussion
Our study, meticulously conducted at King George Hospital in Visakhapatnam, not only serves as a valuable confirmation of existing research but also ventures to broaden the horizon of knowledge concerning the intricate and often perplexing subject of forgotten or retained plastic biliary stents. Delving into the demographic landscape, our findings paint a vivid portrait of the patient population, revealing a median age of 48 years and a notable preponderance of females at 58.3%. This alignment with prior investigations reinforces the consistency in the demographic patterns observed in this realm [
12,
13].
The consonance between our study and the work of Siiki et al. (2018), who also identified cholangitis as the principal complication associated with retained biliary stents (
Figure 1), underscores the persisting relevance of this issue in diverse medical contexts [
14]. Our findings resonate with and build upon this body of knowledge, contributing to the depth of understanding of this complex subject.
A salient deviation from prior research is notably observed in the context of the success rates of ERCP. Our research documents an ERCP success rate of 66.6%, slightly below the 75% success rate reported by Gadour et al. (2021) [
15]. This variance is a striking observation that invites further scrutiny. It may be attributed to a medley of factors, including variations in surgical techniques, disparities in healthcare resource availability, and distinctions in the expertise of the medical practitioners involved. Indeed, the research by Patel et al. (2023) reinforces the notion that the condition of the stent itself, encompassing factors such as fragmentation and migration, exerts a notable influence on the efficacy of stent retrieval methods [
16].
Adding a novel dimension to the discourse, our study uncovers a heightened prevalence of forgotten biliary stents during the tumultuous period of the COVID-19 pandemic—an aspect that has hitherto evaded exploration (
Figure 1). This discovery is especially noteworthy, as even comprehensive studies like that conducted by Skorupski et al. (2022) did not delve into the potential impact of the pandemic on stent retention. The notable upsurge in instances of forgotten stents can be plausibly attributed to the disruptions in routine healthcare caused by lockdowns and the reallocation of healthcare resources, thus underscoring the urgency of the issue and the need for targeted research [
17].
Expanding on the theme of alternative intervention strategies, our study sheds light on a promising 50% success rate associated with cholangioscopy when ERCP proves ineffective, a rate surpassing the 40% efficacy reported by Oh et al. (2021) [
18]. This divergence prompts contemplation regarding the potential favourability of cholangioscopy as an alternative or supplementary approach to ERCP in specific clinical scenarios. In alignment with the findings of Subhash et al. (2021) [
19], our research reaffirms the effectiveness of surgical intervention as a last-resort strategy for stent retrieval, attaining a flawless 100% success rate.
The implications of our findings resonate far and wide, extending their influence into the realms of clinical practice and future research in the domain of forgotten or retained plastic biliary stents. As we navigate the intricate path of patient care, it becomes essential to assimilate the insights provided by our study into the broader tapestry of existing literature [
20,
21]. Furthermore, the profound impact of the COVID-19 pandemic on healthcare delivery, illuminated by our findings, necessitates continued scrutiny and the adaptive refinement of clinical protocols [
22,
23]. This collective effort will undoubtedly contribute to the amelioration of patient outcomes and the enhancement of management strategies in this specialized domain.
Study Limitations:
While our research undoubtedly constitutes a significant addition to the scholarly discourse, it is paramount to acknowledge the inherent constraints it entails. The rather limited sample size and the conspicuous absence of a control group might encumber the extensiveness of our findings’ applicability. Furthermore, the relatively concise 8-month duration of our study may not fully encompass the exhaustive gamut of enduring ramifications arising from stent retention, a limitation that warrants emphasis as well.
Conclusions
Our study serves as a valuable conduit to gain profound insights into the intricate realm of retrieving forgotten plastic biliary stents and unravelling the associated complications, thus significantly augmenting the corpus of medical knowledge. It bolsters our understanding by corroborating well-established demographic trends and common complications, most notably the spectre of cholangitis.
Of particular note are the discernible disparities in the success rates of ERCP, shining a spotlight on the intricacies involved in stent removal. What emerges as a significant revelation is the sharp upsurge in the prevalence of forgotten stents during the relentless tide of the COVID-19 pandemic. This unearths concerns about healthcare delays and the potential exacerbation of patients’ conditions, underscoring the critical importance of implementing vigilant and efficient management strategies, especially during times of crisis.
Moreover, our study accentuates the efficacy of alternative interventions such as cholangioscopy, which have a pronounced role in enhancing the landscape of medical practices. In sum, our research adeptly addresses critical gaps in knowledge and highlights the intricate interplay between healthcare delivery and external factors. These findings beckon healthcare practitioners to adopt proactive measures, ensuring optimal outcomes for patients grappling with the challenges of plastic biliary stents, a pressing matter in the realm of modern medicine.
Author Contributions
SS and MKK were the architects of the study’s conceptual framework, responsible for its inception and data conception. PRKM and NHR undertook the tasks of data analysis, curation, and comprehensive literature review. SBS and SRK played pivotal roles in the study’s design, execution, drafting, editing, statistical analysis, and data validation. It’s worth noting that NHR also contributed to the study’s design.
Acknowledgments
The authors expressed their gratitude for the individuals who participated in the study, as well as for the affiliations of Andhra Medical College and King George Hospital, Vishakhapatnam.
Conflicts of Interest
None.
References
- Baron TH. Best endoscopic stents for the biliary tree and pancreas. Curr Opin Gastroenterol. 2014 Sep;30(5):453-6. [CrossRef]
- Vozzo CF, Sanaka MR. Endoscopic Management of Pancreaticobiliary Disease. Surg Clin North Am. 2020 Dec;100(6):1151-1168. [CrossRef]
- Scheers I, Ergun M, Aouattah T, Piessevaux H, Borbath I, Stephenne X, De Magnée C, Reding R, Sokal E, Veyckemans F, Weynand B, Deprez PH. Diagnostic and Therapeutic Roles of Endoscopic Ultrasound in Pediatric Pancreaticobiliary Disorders. J Pediatr Gastroenterol Nutr. 2015 Aug;61(2):238-47. [CrossRef]
- Mangiavillano B, Pagano N, Baron TH, Arena M, Iabichino G, Consolo P, Opocher E, Luigiano C. Biliary and pancreatic stenting: Devices and insertion techniques in therapeutic endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography. World J Gastrointest Endosc. 2016 Feb 10;8(3):143-56. [CrossRef]
- Siiki A, Vaalavuo Y, Antila A, Ukkonen M, Rinta-Kiikka I, Sand J, Laukkarinen J. Biodegradable biliary stents preferable to plastic stent therapy in post-cholecystectomy bile leak and avoid second endoscopy. Scand J Gastroenterol. 2018 Oct-Nov;53(10-11):1376-1380. [CrossRef]
- Padmanaban V, Jalloh S, Barrie U, Livingston D, Sifri ZC. Expanding post-operative follow-up in rural Sierra Leone: A community-based protocol. Am J Surg. 2021 May;221(5):895-899. [CrossRef]
- Contini C, Caselli E, Martini F, Maritati M, Torreggiani E, Seraceni S, Vesce F, Perri P, Rizzo L, Tognon M. COVID-19 Is a Multifaceted Challenging Pandemic Which Needs Urgent Public Health Interventions. Microorganisms. 2020 Aug 12;8(8):1228. [CrossRef]
- Sbeit W, Khoury T, Kadah A, M Livovsky D, Nubani A, Mari A, Goldin E, Mahamid M. Long-Term Safety of Endoscopic Biliary Stents for Cholangitis Complicating Choledocholithiasis: A Multi-Center Study. J Clin Med. 2020 Sep 12;9(9):2953.
- Isayama H, Ishii S, Tomishima K, Fujisawa T. Recent Advances in Pancreato-Biliary Endoscopic Intervention: How to Resolve Unmet Needs in Pancreato-Biliary Diseases Endoscopically. J Clin Med. 2022 Jun 23;11(13):3637. [CrossRef]
- Kitagawa K, Mitoro A, Ozutsumi T, Furukawa M, Fujinaga Y, Nishimura N, Sawada Y, Namisaki T, Akahane T, Yoshiji H. Comparison of the efficacy and safety between palliative biliary stent placement and duct clearance among elderly patients with choledocholithiasis: a propensity score-matched analysis. BMC Gastroenterol. 2021 Oct 10;21(1):369. [CrossRef]
- Kumar S, Chandra A, Kulkarni R, Maurya AP, Gupta V. Forgotten biliary stents: ignorance is not bliss. Surg Endosc. 2018 Jan;32(1):191-195. [CrossRef]
- Pan G, Yang K, Gong B, Deng Z. Analysis of the Efficacy and Safety of Endoscopic Retrograde Cholangiopancreatography in Children With Symptomatic Pancreas Divisum. Front Pediatr. 2021 Nov 2;9:761331. [CrossRef]
- Odabasi M, Arslan C, Akbulut S, Abuoglu HH, Ozkan E, Yildiz MK, Eris C, Gunay E, Tekesin K, Muftuoglu T. Long-term effects of forgotten biliary stents: a case series and literature review. Int J Clin Exp Med. 2014 Aug 15;7(8):2045-52.
- Siiki A, Rinta-Kiikka I, Sand J, Laukkarinen J. A pilot study of endoscopically inserted biodegradable biliary stents in the treatment of benign biliary strictures and cystic duct leaks. Gastrointest Endosc. 2018 Apr;87(4):1132-1137. [CrossRef]
- Gadour E, Agu O, Musharaf M, Dixon M, Askar A, Hafeez S, Shafiq Y, Arabiyat A, Moradi J. Success Rate of Wire Control-Assisted ERCP Sphincterotomy Versus Non-assisted ERCP Cannulation of Common Bile Duct in a Secondary Care Unit During the First COVID-19 Peak: A Retrospective Observational Study of 281 Patients. Cureus. 2021 Sep 9;13(9):e17861. [CrossRef]
- Patel S, Patel KB, Patel Z, Konat A, Patel A, Doshi JS, Chokshi P, Patel D, Sharma K, Amdani MM, Shah DB, Dholu U, Patel M. Evolving Coronary Stent Technologies - A Glimpse Into the Future. Cureus. 2023 Mar 1;15(3):e35651. [CrossRef]
- Skorupski WJ, Grygier M, Lesiak M, Kałużna-Oleksy M. Coronary Stent Thrombosis in COVID-19 Patients: A Systematic Review of Cases Reported Worldwide. Viruses. 2022 Jan 27;14(2):260. [CrossRef]
- Oh CH, Dong SH. Recent advances in the management of difficult bile-duct stones: a focus on single-operator cholangioscopy-guided lithotripsy. Korean J Intern Med. 2021 Mar;36(2):235-246. [CrossRef]
- Subhash A, Abadir A, Iskander JM, Tabibian JH. Applications, Limitations, and Expansion of Cholangioscopy in Clinical Practice. Gastroenterol Hepatol (N Y). 2021 Mar;17(3):110-120.
- Hwang JJ, Jeong YS, Park YS, Yoon H, Shin CM, Kim N, Lee DH. Comparison of Endoscopic Vacuum Therapy and Endoscopic Stent Implantation With Self-Expandable Metal Stent in Treating Postsurgical Gastroesophageal Leakage. Medicine (Baltimore). 2016 Apr;95(16):e3416. [CrossRef]
- Moss AC, Morris E, Leyden J, MacMathuna P. Do the benefits of metal stents justify the costs? A systematic review and meta-analysis of trials comparing endoscopic stents for malignant biliary obstruction. Eur J Gastroenterol Hepatol. 2007 Dec;19(12):1119-24. [CrossRef]
- Anjum MR, Chalmers J, Hamid R, Rajoriya N. COVID-19: Effect on gastroenterology and hepatology service provision and training: Lessons learnt and planning for the future. World J Gastroenterol. 2021 Nov 28;27(44):7625-7648. [CrossRef]
- Alboraie M, Piscoya A, Tran QT, Mendelsohn RB, Butt AS, Lenz L, Alavinejad P, Emara MH, Samlani Z, Altonbary A, Monged A, Lemmers A, Sudovykh I, Ho DQD, Ghazanfar S, Kamau E, Iqbal S, Tan DMY, Liao WC, Vignesh S; “The Global Endo-COVID working group”. The global impact of COVID-19 on gastrointestinal endoscopy units: An international survey of endoscopists. Arab J Gastroenterol. 2020 Sep;21(3):156-161. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).