Submitted:
06 November 2023
Posted:
07 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
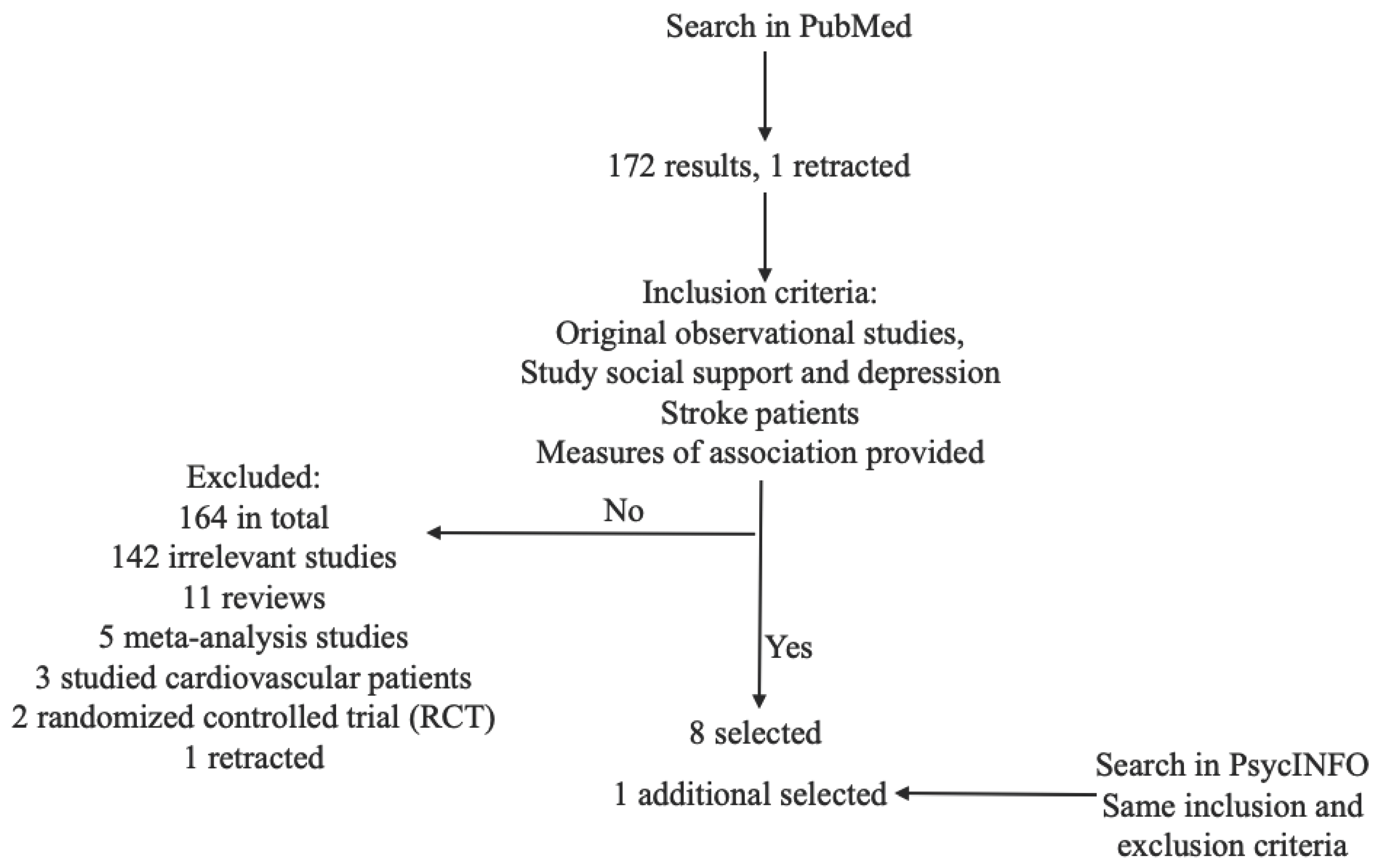
2. Materials and Methods
3. Results
3.1. Samples and Populations
3.2. Social Support and Depression Measurements
3.3. Main Findings
4. Discussion
4.1. Limitations
4.2. Strengths
4.3. Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donkor, E.S. Stroke in the 21(St) Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef]
- American Stroke Association About Stroke. Available online: https://www.stroke.org/en/about-stroke (accessed on 24 May 2023).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P. Heart Disease and Stroke Statistics — 2020 Update: A Report From the American Heart Association. Am. Hear. Assoc. 2020, 141. [Google Scholar] [CrossRef]
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 1–24. [Google Scholar] [CrossRef]
- Unnithan, A.K.A.; Das, J.M.; Mehta, P. Hemorrhagic Stroke. StatPearls 2023. [Google Scholar]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.V.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; et al. An Updated Definition of Stroke for the 21st Century: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef]
- Kumar, S.; Selim, M.H.; Caplan, L.R. Medical Complications after Stroke. Lancet Neurol. 2010, 9, 105–118. [Google Scholar] [CrossRef]
- Medeiros, G.C.; Roy, D.; Kontos, N.; Beach, S.R. Post-Stroke Depression: A 2020 Updated Review. Gen. Hosp. Psychiatry 2020, 66, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, J.; Sun, W.; Liu, X. The Advances of Post-Stroke Depression: 2021 Update. J. Neurol. 2022, 269, 1236–1249. [Google Scholar] [CrossRef] [PubMed]
- Hackett, M.L.; Pickles, K. Part I: Frequency of Depression after Stroke: An Updated Systematic Review and Meta-Analysis of Observational Studies. Int. J. stroke Off. J. Int. Stroke Soc. 2014, 9, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Ayerbe, L.; Ayis, S.; Wolfe, C.D.A.; Rudd, A.G. Natural History, Predictors and Outcomes of Depression after Stroke: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2013, 202, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J.; Sheth, B.; Gill, J.; Yadegarfar, M.; Stubbs, B.; Yadegarfar, M.; Meader, N. Prevalence and Predictors of Post-Stroke Mood Disorders: A Meta-Analysis and Meta-Regression of Depression, Anxiety and Adjustment Disorder. Gen. Hosp. Psychiatry 2017, 47, 48–60. [Google Scholar] [CrossRef]
- World Health Organization Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 5 November 2021).
- Thomas, L.H.; Coupe, J.; Cross, L.D.; Tan, A.L.; Watkins, C.L. Interventions for Treating Urinary Incontinence after Stroke in Adults. Cochrane database Syst. Rev. 2019, 2, CD004462. [Google Scholar] [CrossRef]
- Limampai, P.; Wongsrithep, W.; Kuptniratsaikul, V. Depression after Stroke at 12-Month Follow-up: A Multicenter Study. Int. J. Neurosci. 2017, 127, 887–892. [Google Scholar] [CrossRef]
- Srithumsuk, W.; Chaleoykitti, S.; Jaipong, S.; Pattayakorn, P.; Podimuang, K. Association between Depression and Medication Adherence in Stroke Survivor Older Adults. Jpn. J. Nurs. Sci. 2021, 18, e12434. [Google Scholar] [CrossRef]
- Cai, W.; Mueller, C.; Li, Y.-J.; Shen, W.-D.; Stewart, R. Post Stroke Depression and Risk of Stroke Recurrence and Mortality: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2019, 50, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Sibolt, G.; Curtze, S.; Melkas, S.; Pohjasvaara, T.; Kaste, M.; Karhunen, P.J.; Oksala, N.K.J.; Vataja, R.; Erkinjuntti, T. Post-Stroke Depression and Depression-Executive Dysfunction Syndrome Are Associated with Recurrence of Ischaemic Stroke. Cerebrovasc. Dis. 2013, 36, 336–343. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders; Arlington, VA: American Psychiatric Publishing, 2013.
- Belmaker, R.H.; Agam, G. Major Depressive Disorder. N. Engl. J. Med. 2008, 358, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, M.H. The Link between Depression and Physical Symptoms. Prim. Care Companion J. Clin. Psychiatry 2004, 6, 12–16. [Google Scholar] [PubMed]
- Raič, M. Depression and Heart Diseases: Leading Health Problems. Psychiatr. Danub. 2017, 29 Suppl 4, 770–777. [Google Scholar]
- Simon, G.E.; VonKorff, M.; Piccinelli, M.; Fullerton, C.; Ormel, J. An International Study of the Relation between Somatic Symptoms and Depression. N. Engl. J. Med. 1999, 341, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Dafsari, F.S.; Jessen, F. [Late life depression - Diagnosis, pathophysiology and therapeutic strategies]. Fortschr. Neurol. Psychiatr. 2018, 86, 242–255. [Google Scholar] [CrossRef]
- Bell, R.A.; Franks, P.; Duberstein, P.R.; Epstein, R.M.; Feldman, M.D.; Garcia, E.F.; Kravitz, R.L. Suffering in Silence: Reasons for Not Disclosing Depression in Primary Care. Ann. Fam. Med. 2011, 9, 439–446. [Google Scholar] [CrossRef]
- Halfin, A. Depression: The Benefits of Early and Appropriate Treatment. Am. J. Manag. Care 2007, 13, S92–7. [Google Scholar]
- Cacheda, F.; Fernandez, D.; Novoa, F.J.; Carneiro, V. Early Detection of Depression: Social Network Analysis and Random Forest Techniques. J. Med. Internet Res. 2019, 21, e12554–e12554. [Google Scholar] [CrossRef]
- Khedr, E.M.; Abdelrahman, A.A.; Desoky, T.; Zaki, A.F.; Gamea, A. Post-Stroke Depression: Frequency, Risk Factors, and Impact on Quality of Life among 103 Stroke Patients—Hospital-Based Study. Egypt. J. Neurol. Psychiatry Neurosurg. 2020, 56. [Google Scholar] [CrossRef]
- American Psychological Association Social Support – APA Dictionary of Psychology. Available online: https://dictionary.apa.org/social-support (accessed on 5 November 2021).
- Reblin, M.; Uchino, B.N. Social and Emotional Support and Its Implication for Health. Curr. Opin. Psychiatry 2008, 21, 201–205. [Google Scholar] [CrossRef]
- Rodríguez-Artalejo, F.; Guallar-Castillón, P.; Herrera, M.C.; Otero, C.M.; Chiva, M.O.; Ochoa, C.C.; Banegas, J.R.; Pascual, C.R. Social Network as a Predictor of Hospital Readmission and Mortality among Older Patients with Heart Failure. J. Card. Fail. 2006, 12, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Piferi, R.L.; Lawler, K.A. Social Support and Ambulatory Blood Pressure: An Examination of Both Receiving and Giving. Int. J. Psychophysiol. Off. J. Int. Organ. Psychophysiol. 2006, 62, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Lyyra, T.-M.; Heikkinen, R.-L. Perceived Social Support and Mortality in Older People. J. Gerontol. B. Psychol. Sci. Soc. Sci. 2006, 61, S147–52. [Google Scholar] [CrossRef] [PubMed]
- Usta, Y.Y. Importance of Social Support in Cancer Patients. Asian Pac. J. Cancer Prev. 2012, 13, 3569–3572. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: A Systematic Review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Falak, S.; Safdar, F. ; Nuzhat-Ul-Ain Perceived Discrimination, Social Support, and Psychological Distress in Transgender Individuals. PsyCh J. 2020, 9, 682–690. [Google Scholar] [CrossRef]
- Erler, K.S.; Sullivan, V.; Mckinnon, S.; Inzana, R. Social Support as a Predictor of Community Participation After Stroke. Front. Neurol. 2019, 10, 1013. [Google Scholar] [CrossRef] [PubMed]
- Hartford, W.; Lear, S.; Nimmon, L. Stroke Survivors’ Experiences of Team Support along Their Recovery Continuum. BMC Health Serv. Res. 2019, 19, 723. [Google Scholar] [CrossRef] [PubMed]
- Lehnerer, S.; Hotter, B.; Padberg, I.; Knispel, P.; Remstedt, D.; Liebenau, A.; Grittner, U.; Wellwood, I.; Meisel, A. Social Work Support and Unmet Social Needs in Life after Stroke: A Cross-Sectional Exploratory Study. BMC Neurol. 2019, 19, 220. [Google Scholar] [CrossRef]
- Peng, Z.-Y.; Wan, L.-H. Posttraumatic Growth of Stroke Survivors and Its Correlation With Rumination and Social Support. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurses 2018, 50, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Robinson-Smith, G.; Mahoney, C. Coping and Marital Equilibrium after Stroke. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurses 1995, 27, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Recto, P.; Champion, J.D. Social Support and Perinatal Depression: The Perspectives of Mexican-American Adolescent Mothers. Issues Ment. Health Nurs. 2020, 41, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and Depression in the Elderly: The Role of Social Network. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social Support and Protection from Depression: Systematic Review of Current Findings in Western Countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef]
- Nakić Radoš, S.; Tadinac, M.; Herman, R. Anxiety During Pregnancy and Postpartum: Course, Predictors and Comorbidity with Postpartum Depression. Acta Clin. Croat. 2018, 57, 39–51. [Google Scholar] [CrossRef]
- Shih, T.-Y.; Cheng, S.-L.; Chang, S.-H.; Sun, H.-F. Perceived Social Support and Depression Symptoms in Patients with Major Depressive Disorder in Taiwan: An Association Study. Arch. Psychiatr. Nurs. 2020, 34, 384–390. [Google Scholar] [CrossRef]
- Hefner, J.; Eisenberg, D. Social Support and Mental Health among College Students. Am. J. Orthopsychiatry 2009, 79, 491–499. [Google Scholar] [CrossRef]
- Ioannou, M.; Kassianos, A.P.; Symeou, M. Coping with Depressive Symptoms in Young Adults: Perceived Social Support Protects against Depressive Symptoms Only under Moderate Levels of Stress. Front. Psychol. 2019, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Types of Stroke | Cdc.Gov. Available online: https://www.cdc.gov/stroke/types_of_stroke.htm (accessed on 4 November 2021).
- Lin, F.-H.; Yih, D.N.; Shih, F.-M.; Chu, C.-M. Effect of Social Support and Health Education on Depression Scale Scores of Chronic Stroke Patients. Medicine (Baltimore). 2019, 98, e17667. [Google Scholar] [CrossRef] [PubMed]
- Villain, M.; Sibon, I.; Renou, P.; Poli, M.; Swendsen, J. Very Early Social Support Following Mild Stroke Is Associated with Emotional and Behavioral Outcomes Three Months Later. Clin. Rehabil. 2017, 31, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Z.M.; Khalil, M.F.; Kohail, A.M.; Eldesouky, I.F.; Elkady, A.; Shuaib, A. The Prevalence and Predictors of Post-Stroke Depression and Anxiety During COVID-19 Pandemic. J. Stroke Cerebrovasular Dis. 2020, 29. [Google Scholar] [CrossRef]
- Wei, C.; Gao, J.; Chen, L.; Zhang, F.; Ma, X.; Zhang, N.; Zhang, W.; Xue, R.; Luo, L.; Hao, J. Factors Associated with Post-Stroke Depression and Emotional Incontinence: Lesion Location and Coping Styles. Int. J. Neurosci. 2016, 126, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shang, S.; Yang, H.; Ai, H.; Wang, Y.; Chang, S.; Sha, X.; Wang, L.; Jiang, X. Associations of Psychological Distress with Positive Psychological Variables and Activities of Daily Living among Stroke Patients: A Cross-Sectional Study. BMC Psychiatry 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Babkair, L.A.; Chyun, D.; Vaughan, V.; Mohammed, D. The Effect of Psychosocial Factors and Functional Independence on Poststroke Depressive Symptoms : A Cross-Sectional Study. 2021, 00, 1–10. [Google Scholar] [CrossRef]
- Olibamoyo, O.; Adewuya, A.; Ola, B.; Coker, O.; Atilola, O. Prevalence and Correlates of Depression among Nigerian Stroke Survivors. South. African J. Psychiatry 2019, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Volz, M.; Möbus, J.; Letsch, C.; Werheid, K. The Influence of Early Depressive Symptoms, Social Support and Decreasing Self-Efficacy on Depression 6 Months Post-Stroke. J. Affect. Disord. 2016, 206, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Schöttke, H.; Gerke, L.; Düsing, R.; Möllmann, A. Post-Stroke Depression and Functional Impairments – A 3-Year Prospective Study. Compr. Psychiatry 2020, 99, 152171. [Google Scholar] [CrossRef] [PubMed]
- Ladwig, S.; Werheid, K.; Südmeyer, M.; Volz, M. Predictors of Post-Stroke Depression: Validation of Established Risk Factors and Introduction of a Dynamic Perspective in Two Longitudinal Studies. Front. Psychiatry 2023, 14. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Kliem, S.; Mößle, T.; Rehbein, F.; Hellmann, D.F.; Zenger, M.; Brähler, E. A Brief Form of the Perceived Social Support Questionnaire (F-SozU) Was Developed, Validated, and Standardized. J. Clin. Epidemiol. 2015, 68, 551–562. [Google Scholar] [CrossRef]
- Xiao, S. The Theoretical Basis and Applications of Social Support Rating Scale. J Clin. Psychiatry 1994, 02, 98–100. [Google Scholar]
- Sherbourne, C.D.; Stewart, A.L. The MOS Social Support Survey. Soc. Sci. Med. 1991, 32, 705–714. [Google Scholar] [CrossRef]
- Fydrich, T.; Geyer, M.A.; Hessel, A.; Sommer, G.; Brähler, E. Fragebogen Zur Sozialen Unterstützung (F-SozU): Normierung an Einer Repräsentativen Stichprobe. Diagnostica 1999, 45, 212–216. [Google Scholar] [CrossRef]
- Fydrich, T.; Sommer, G.; Tydecks, S.; Brähler, E. Fragebogen Zur Sozialen Unterstützung (F-SozU): Normierung Der Kurzform (K-14) Social Support Questionnaire (F-SozU): Standardization of Short Form (K-14). Zeitschrift für Medizinische Psychol. 2009, 18, 43–48. [Google Scholar]
- Liu, R.; Yue, Y.; Jiang, H.; Lu, J.; Wu, A.; Geng, D.; Wang, J.; Lu, J.; Li, S.; Tang, H.; et al. A Risk Prediction Model for Post-Stroke Depression in Chinese Stroke Survivors Based on Clinical and Socio-Psychological Features. Oncotarget 2017, 8, 62891–62899. [Google Scholar] [CrossRef] [PubMed]
- Bell, C.C. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA 1994, 272, 828–829. [Google Scholar] [CrossRef]
- Sheehan, D. V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59, 22–33. [Google Scholar] [PubMed]
- Snaith, R.P. The Hospital Anxiety and Depression Scale. Health Qual. Life Outcomes 2003, 1, 6–9. [Google Scholar] [CrossRef]
- Alexopoulos, G.S.; Abrams, R.C.; Young, R.C.; Shamoian, C. . The Cornell Scale for Depression in Dementia : Administration & Scoring Guidelines. Biol. Psychiatry 1988, 23, 271–284. [Google Scholar]
- Hamilton, M. A Rating Scale of Depression. J Neurol Neurosurg Psychiatry 1969, 23, 56–62. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Stone, L.; Granier, K.; Segal, D.L. Geriatric Depression Scale. Encycl. Gerontol. Popul. Aging 2019. [Google Scholar]
- Neff, A.J.; Lee, Y.; Metts, C.L.; Wong, A.W.K. Ecological Momentary Assessment of Social Interactions: Associations With Depression, Anxiety, Pain, and Fatigue in Individuals With Mild Stroke. Physiol. Behav. 2021, 102, 395–405. [Google Scholar] [CrossRef]
- HAMILTON, M. A Rating Scale for Depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Ilut, S.; Stan, A.; Blesneag, A.; Vacaras, V.; Vesa, S.; Fodoreanu, L. Factors That Influence the Severity of Post-Stroke Depression. J. Med. Life 2017, 10, 167–171. [Google Scholar] [PubMed]
- Powers, W.J.; Derdeyn, C.P.; Biller, J.; Coffey, C.S.; Hoh, B.L.; Jauch, E.C.; Johnston, K.C.; Johnston, S.C.; Khalessi, A.A.; Kidwell, C.S.; et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American. Stroke 2015, 46, 3020–3035. [Google Scholar] [CrossRef]
- Ding, P.; VanderWeele, T.J. Sensitivity Analysis without Assumptions. Epidemiology 2016, 27, 368–377. [Google Scholar] [CrossRef]
- Trinquart, L.; Erlinger, A.L.; Petersen, J.M.; Fox, M.; Galea, S. Applying the e Value to Assess the Robustness of Epidemiologic Fields of Inquiry to Unmeasured Confounding. Am. J. Epidemiol. 2019, 188, 1174–1180. [Google Scholar] [CrossRef]
| Citation | Country and setting | Study type (year) & sampling method | Sample Description | Inclusion criteria | Exclusion criteria | Tools measuring exposure variable | Tools measuring outcome variable | Statistics | Main Findings |
|---|---|---|---|---|---|---|---|---|---|
| Olibamoyo et al, 2019 [56] | Nigeria, inpatients, a university teaching hospital | A cross-sectional study Simple random sampling. |
112 adults, age: 18-65 | Clinical history of stroke not less than 6 months prior, confirmed by neuroimaging. | History of any psychotic disorder, history or pre-stroke mood disorder, language impairment severe enough to prevent neuro-psychiatry assessment, history of other central nervous disorders and acute illness preventing proper assessment | Perceived social support, assessed by one question in a demographic questionnaire, categories: good, fair, and poor | Depression, assessed by MINI English Version 5.0 | Poor social support vs. good social support adjusted OR: 92.4 (3.71-22296.83), p = 0.006 | Perceived poor social support, higher number of previous admissions of stroke, younger age, and unemployment are associated with increased risk of depression. |
| Ahmed et al, 2020 [52] | Saudi Arabia, Inpatients, two tertiary stroke centers | A prospective cohort study (90-day follow-up). Convenient sampling. |
68 adults, mean age: 56.72, age range: 29-75 |
Acute ischemic stroke, confirmed clinical and radiological evidence/ | Fever, cough or any acute respiratory symptoms, any chronic psychiatric or neurocognitive disorder, pre-existing chronic neurological disorders, chronic debilitating medical disorders | Perceived social support assessed by (MSPSS). | Post-stroke depression (PSD) & post-stroke (PSA) assessed by HADS | MSPSS score unadjusted OR: 0.44 (0.26-0.75), p = 0.003; adjusted OR: 0.66 (0.47-0.94), p = 0.002 |
Lower social support score, worse stroke severity at admission, and worse disability status are associated with an increased risk of post-stroke depression. |
| Schöttke et al, 2020 [58] | German, inpatients, three rehabilitation clinics | A prospective cohort study (3-year follow-up). Sampling method not introduced. |
174 patients, mean age: 67.51 | Either acute cerebral infarction or intracerebral hemorrhage, neurological symptoms over 24 hours prior. | The need for intensive medical treatment, artificial respiration, intensive treatment of body injuries and heightened intracranial pressure, and severe aphasia. | Perceived social support assessed by F-SozU at acute phase | PSD assessed by structured clinical interview & Functional impairment assessed by BI | Without the interaction term, F-SozU adjusted OR: 1.355 (0.516, 3.560), p = 0.537. With the interaction term, F-SozU adjusted OR: 1.825 (0.593, 5.617), p = 0.295. | Perceived social support is not found to have a statistically significant association with poststroke depression 3 years from stroke, adjusting for age, sex, functional impairment, and depression at acute phase with or without the interaction between functional impairment and social support at acute phase. |
| Citation | Country and setting | Study type (year) & sampling method | Sample description | Inclusion criteria | Exclusion criteria | Tools measuring exposure variable | Tools measuring outcome variable | Statistics | Main Findings |
| Villain et al, 2017 [51] | France, stroke patients, setting not specified | A prospective cohort study (3-month follow-up). Convenient sampling. |
44 adults enrolled, 33 followed up | First mild ischemic stroke diagnosed by a neurologist, confirmed with clinical evidence and MRI, NIHSS score ≤ 6. | A history of dementia (Mini-Mental State Examination < 24), severe aphasia, visual or motor handicap, or a history of major depression prior to stroke. | Perceived social support assessed by Ecological Momentary Assessments immediately after stroke | Depression assessed by HDRS-17 at follow-up | Medical attention γ: -0.019, SE: 0.055, t ratio: -0.357; Moral support (medical staff) γ: -0.051, SE: 0.043, t ratio: -1.191; Moral support (family, friends) γ: -0.097, SE: 0.046, t ratio: -2.141; Material support (family, friends) γ: 0.008, SE: 0.055, t ratio: 0.161 |
Lower perceived moral support from family and friends are associated with an increased risk of depression, conditional on medical attention, adjusting for age, sex, anxiety, and depression levels at hospital admission. |
| Volz et al, 2016 [57] | German, inpatients, two inpatient rehabilitation centers | A prospective cohort study (6.1-month follow-up) Sampling methods not introduced. |
88 adults, mean age: 66.35, age SD: 10.70, age range: 44-90 | First ischemic stroke ≥4 weeks prior, education ≥ 8 years, comprehension Token test > 12, age over 40, less than 12 weeks deviation from follow-up interval | social support assessed by F-SozU | Depression diagnosed by DSM-IV | F-SozU adjusted OR = 0.95, p = 0.03 | Lower social support is associated with increases in later depression, adjusting for physical disability status, pre-stroke mental illness, stroke severity, cognitive status, and general self-efficacy and early depressiveness. | |
| Citation | Country and setting | Study design & sampling method | Sample description | Inclusion criteria | Exclusion criteria | Tools measuring exposure variable | Tools measuring outcome variable | Statistics | Main Findings |
| Wang et al, 2019 [54] | China, inpatients from community hospitals in five major cities in a province | A cross-sectional study. Convenient sampling. |
800 stroke patients enrolled, 710 responded, age: 30-90 | Stroke patients, able to read. | Missing items in questionnaires | Perceived social support assessed by the Chinese version of MSPSS | Depressive symptoms assessed by CES-D | MSPSS adjusted β: -0.111, p < 0.01 in linear regression | Lower social support is associated with increases depressive symptoms, adjusting for age, gender, marital status, education, residence types, chronic disease, monthly income, medical payment types, activities of daily living, hope, resilience and self-efficacy. |
| Babkair et al, 2021 [55] | Saudi Arabia, inpatients from three hospitals | A cross-sectional study Convenient sampling. |
135 adults, history of stroke, age ≥ 18 | Stroke patients, age≥ 18 years, able to comprehend and communicate in Arabic | Conditions that limit ability to complete a survey (cognitive impairment, dementia, aphasia, and chronic psychiatric diagnoses except previous depression) | Social support assessed by MOS-SSS | Poststroke depressive symptoms assessed by PHQ-9 | MOS-SSS adjusted β: -0.31, p <0.001 | Lower perceived social support is associated with increased depressive symptom level, adjusting for sex, marital status, employment, income, perceived stress, and functional independence. |
| Wei et al, 2016 [53] | China, inpatients from a university hospital | A prospective cohort study (3-month follow-up) |
368 adult stroke patients, overall age statistics not provided | Diagnosis of acute stroke confirmed based on CT or MRI findings within 7 days after stroke onset | Hemorrhagic stroke, unusual causes such as dissections, venous infarction or moyamoya disease, transient ischemic attack (TIA) without progression to stroke, communication problems, severe neurologic or medical conditions, score ≤23 on the Mini-Mental State Examination (MMSE) | Social support assessed by SSRS | Poststroke depression assessed by BDI | The degree of social utilization section of SSRS adjusted β: -0.558, p = 0.001. Converted to adjusted odds ratio: 0.57 | Higher degree of social utilization, a dimension of social support, is associated with decreased poststroke depression, adjusting for sensory dysfunction and motor dysfunction at admission, and coping strategies including avoidance level and acceptance vs. resignation. |
| TCitation | Country and setting | Study design & sampling method | Sample description | Inclusion criteria | Exclusion criteria | Tools measuring exposure variable | Tools measuring outcome variable | Statistics | Main Findings |
| Ladwig et al, 2023 [59] | Study A: German, inpatients from two rehabilitation clinics; Study B: German, inpatients from the stroke unit of an acute hospital |
Secondary data analysis based on two cohort studies (denoted studies A and B, 6month-follow-up in) Sampling methods not introduced. |
273 (Study A) and 226 (Study B). Study A mean age: 63.9, age SD: 10.9, age range: 42-92. Study B mean age: 64.2, age SD: 10.2, age range: 42-90. |
Both studies: ischemic stroke patients with sufficient language comprehension. Study B further required sufficient cognition. |
Both studies: terminal or impairing disease other than stroke. | Social support assessed by F-SozU K22 (Study A) and F-SozU K14 (Study B); |
Depressive symptoms assessed by GDS_15 (Study A) and PHQ-9 (Study B) | Study A: F-SozU adjusted β = -1.91, 95% CI: (-2.71, -1.11). Study B: F-SozU K-14 adjusted β = - 2.69, 95% CI: (-3.92, -1.47). Difference of social support adjusted β = -0.14 (-0.22, 0.05). |
Social support is negatively associated with the risk of post-stroke depression, adjusting for history of mental disorder, stroke severity, physical. The change of social support (follow-up minus baseline) is also a protective factor against depression. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





