Neuromyelitis optica spectrum disorder (NMOSD) is an autoimmune-mediated central nerve system (CNS) disorder characterized by demyelination of the optic nerve and spinal cord, resulting in motor, sensory, and visual symptoms due to antibodies (AQP4–immunoglobulin G [IgG] or
myelin-oligodendrocyte-glycoprotein.[
1] Cervical spondylotic myelopathy (CSM) is caused by spinal cord compression due to degenerative changes in the cervical spine. Both NMO and CSM share similar clinical manifestations, including motor weakness and sensory disturbances.
NMO, characterized by longitudinally extensive transverse myelitis (LETM), typically manifests with spinal cord lesions over three segments. However, reports have suggested that in approximately 14% of cases, NMO can present with short-segment spinal cord lesions involving fewer than three vertebral segments.[
2] Despite distinct diagnostic criteria for NMO and CSM, there have been reported cases where NMO closely mimics the clinical and radiological features of CSM.[
3] The coexistence of disc herniation with spinal cord compression and short-segment transverse myelitis can lead to diagnostic challenges.[
4] This diagnostic challenge can result in delayed or misdiagnosis, potentially leading to inappropriate management and unfavorable patient outcomes. To aid in the differential diagnosis, we present a case report of a patient with recurrent NMOSD who was initially misdiagnosed as having CSM.
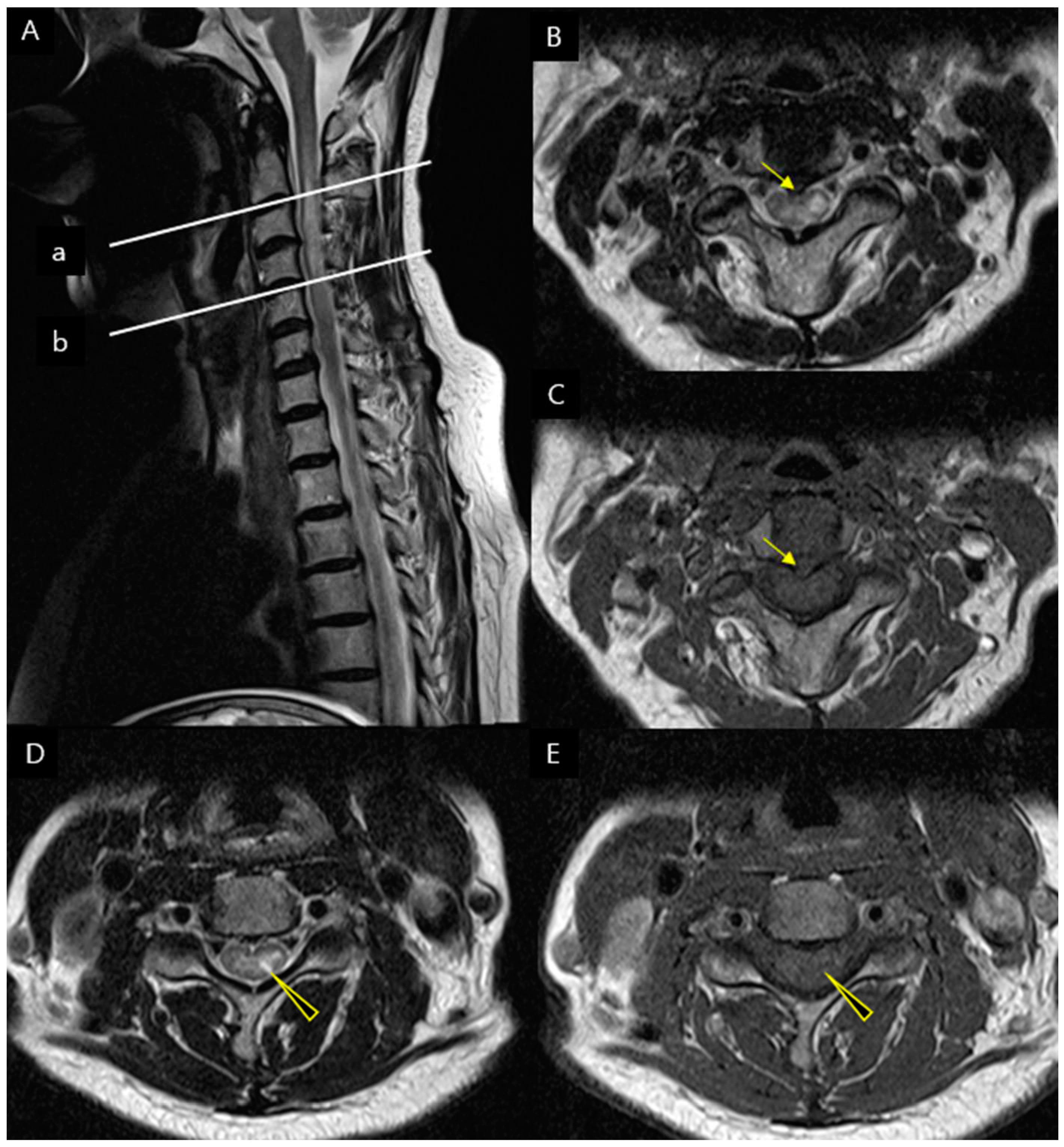
A 66-year-old female patient with a history of hyperlipidemia presented to the hospital three years ago with posterior neck pain, radiating pain on left arm and left upper limb motor weakness. The patient presented with left-sided motor weakness: manual muscle testing (MMT) score of 4 that is nearly normal, and reflexes were intact. The patient also complained of tingling and numbness in the left upper limb, with a Numeric Rating Scale (NRS) score of 3. However, the patient didn't complain of any visual symptoms. At that time, a cervical spine MRI revealed a herniated disc at the C2-3 level, the increased signal intensity of the spinal cord at the C3 to 4 levels (
Figure 1). Based on the patient's motor weakness, radiating pain, and MRI findings, she was diagnosed with cervical spondylotic myelopathy and underwent C2-3-4 posterior decompression during hospitalization. Following the surgery, the patient showed improvement in left limb motor weakness and radiating pain and was followed up as an outpatient.
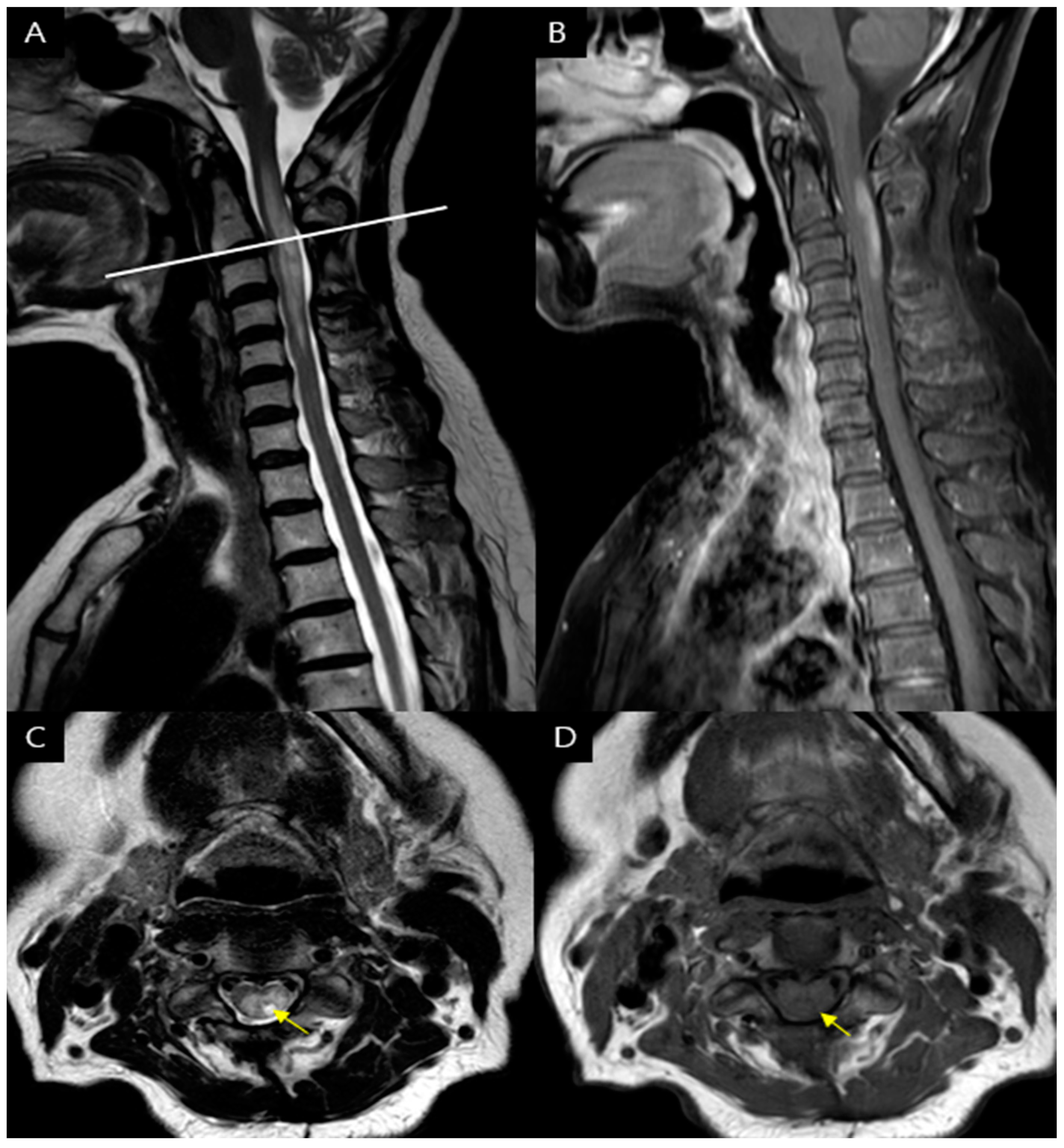
Three years after the initial diagnosis of CSM, the patient presented to the hospital three days ago with sudden onset of left upper extremity motor weakness and mild gait disturbance. On the physical examination, the patient displayed varying degrees of motor weakness on the left side, as assessed by MMT: shoulder flexion scored 2, elbow flexion scored 4, wrist extension scored 4, finger flexion scored 4, finger extension scored 3, hip flexion scored 4, knee extension scored 4, and ankle dorsiflexion scored 4. Sensation to touch and pinprick was normal. The knee-jerk reflex was relatively within the normal range. Hoffmann's sign exhibited equivocality on the left side, while Babinski reflexes and ankle clonus were absent. In addition, the patient reported nonradiating pain with a NRS score of 3, which was accompanied throughout the left upper limb. The cervical spine MRI showed findings consistent with longitudinally extensive transverse myelitis (LETM). In the sagittal view, there was evidence of longitudinally extensive high signal at the C1 to C5. In the axial view, features indicative of transverse myelitis were observed, supporting the diagnosis of LETM. (
Figure 2)
The CSF study revealed a 2+ AQP4-Ab finding. Serum autoimmune markers for rheumatoid factor (4.9IU/ml; normal = 0~15), lupus anticoagulant (0.8; normal = 0.8~1.2), anti-neutrophil cytoplasmic antibody (0.5U/ml; normal ~5), as well as MOG antibody (RPC 0.019; 0.141<Borderline≤0.254, MFIr 1.88; 2.60<Borderline≤3.65) were within normal values. The CSF study revealed negative findings for infections such as viruses and bacteria, TB PCR, and oligoclonal band. A central motor conduction times study of motor evoked potential study in both biceps brachii, abductor pollicis brevis and tibialis anterior were delated (biceps brachii : right 9.5ms, left 11.8ms; normal cutoff value = 9.2ms / abductor pollicis brevis : right 8.5ms, left 8.9ms; normal cutoff value = 8.5ms / tibialis anterior : right 18.1ms, left 18.7ms; normal cutoff value = 18.1ms). Motor and sensory nerve conduction studies showed normal amplitudes and conduction velocities. Additional evaluations for optic neuritis revealed no abnormalities. Finally, the patient was diagnosed with Neuromyelitis Optica Spectrum Disorder (NMOSD). Steroid pulsed therapy (five days of dexamethasone) and immunosuppression therapy (four weeks of azathioprine) were initiated. After 20 days, the patient exhibited significant improvement in shoulder weakness, allowing for overhead activities, and the gait disturbance was resolved, enabling the patient to perform daily activities without difficulty, including using her upper extremities.
The initial diagnosis based on the MRI findings was a cervical herniated disc with cord compression, subsequently led to surgical treatment. However, upon readmission, the patient was ultimately diagnosed with Neuromyelitis Optica Spectrum Disorder (NMOSD). Therefore, in patients with cervical disc herniation and spinal cord compression, careful evaluation of MRI findings may help differentiate between short-segment transverse myelitis and cervical spondylotic myelopathy.
The initial C-spine MRI revealed disc herniation with cord compression at the C2-3 . In cases of cord compression caused by disc herniation, it is common to observe spinal cord signal changes primarily in proximity to the site of compression.[
5] However, in this case, despite the compression being located at C2-3, there were signal intensity change observed at C3-4, suggesting that the observed signal alteration may not be solely attributable to compression. While autoimmune diseases are commonly observed in individuals in their 50s, they have also been reported to occur in individuals in their 90s.[
6] Considering that spondylosis represents a degenerative change associated with aging, it is reasonable to assume that the likelihood of developing disc herniation or spondylotic myelopathy increases, especially in older individuals.[
7] It is crucial to be aware of the potential occurrence of transverse myelitis in elderly patients with spondylosis. Therefore, when the spinal cord MRI findings do not align with the degenerative structural changes typically associated with spondylosis, it is essential to consider alternative differential diagnoses apart from spondylotic myelopathy.
Furthermore, at the C4-5 level, where no cord compression was observed, there is a high signal change within the spinal cord that appears brighter than the cerebrospinal fluid signal. These findings correspond to bright spotty lesions (BSLs), which are defined as hyperintense intramedullary lesions on axial T2-weighted images usually associated with T1 low signal. BSLs are considered a characteristic feature of NMOSD, distinguishing it from conditions such as multiple sclerosis (MS) and other disorder that revealed LETM. [
5,
8] if BSLs do not correlate with the level of compression, additional investigations should be conducted to consider the possibility of NMOSD.
This case emphasizes the significance of a thorough evaluation of characteristic MRI findings, including the location of disc herniation and associated signal changes in cases of cord compression. It also highlights the importance of paying close attention to specific MRI features, such as Bright Spinal Lesion (BSL), as it plays a crucial role in making an accurate differential diagnosis.
Author Contributions
Conceptualization, J.P. and D.L.; methodology, D.L.; formal analysis, D.L.; investigation, J,P. and D.L.; writing—original draft preparation, J.P.; writing—review and editing, D.L.; visualization, J.P.; funding acquisition, D.L.. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Basic Science Research Program though the National Research Funding of Korea (NRF) and funded by the Ministry of Education (2022R1I1A3071887).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Yeungnam University (YUMC 2023-09-028 and date of approval; 25 SEP 2023 ).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Data are available on a reasonable request from the authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wingerchuk, D.M.; Banwell, B.; Bennett, J.L.; Cabre, P.; Carroll, W.; Chitnis, T.; De Seze, J.; Fujihara, K.; Greenberg, B.; Jacob, A. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015, 85, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.P.; Weinshenker, B.G.; Krecke, K.N.; Lennon, V.A.; Lucchinetti, C.F.; McKeon, A.; Wingerchuk, D.M.; Shuster, E.A.; Jiao, Y.; Horta, E.S. Short myelitis lesions in aquaporin-4-IgG–positive neuromyelitis optica spectrum disorders. JAMA neurology 2015, 72, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Newsome, S.D. Cervical spondylotic myelopathy mimicking transverse myelitis. Multiple Sclerosis and Related Disorders 2019, 31, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Fang*, W.; Zheng*, Y.; Yang, F.; Cai, M.-T.; Shen, C.-H.; Liu, Z.-R.; Zhang, Y.-X.; Ding, M.-P. Short segment myelitis as the initial and only manifestation of aquaporin-4 immunoglobulin G-positive neuromyelitis optica spectrum disorders. Therapeutic Advances in Neurological Disorders 2020, 13, 1756286419898594. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.; Feizi, P.; Pasham, S.R.; Sharma, K.; Srivastava, S.; Elkhooly, M.; Nirwan, L.; Jaiswal, S.; Sriwastava, S. Relevance of bright spotty lesions in neuromyelitis optica spectrum disorders (NMOSD): a case series. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery 2022, 58, 165. [Google Scholar] [CrossRef]
- Ohe, Y.; Fukuoka, T.; Deguchi, I.; Hayashi, T.; Tanahashi, N. Case of elderly-onset neuromyelitis optica spectrum disorder mimicking cervical spondylotic myelopathy. Neurology and Clinical Neuroscience 2014, 2, 18–19. [Google Scholar] [CrossRef]
- Wang, C.; Tian, F.; Zhou, Y.; He, W.; Cai, Z. The incidence of cervical spondylosis decreases with aging in the elderly, and increases with aging in the young and adult population: a hospital-based clinical analysis. Clinical interventions in aging 2016, 47–53. [Google Scholar]
- Woo, P.Y.-M.; Chiu, J.H.-F.; Leung, K.-M.; Chan, K.-Y. Seropositive neuromyelitis optica imitating an intramedullary cervical spinal cord tumor: Case report and brief review of the literature. Asian spine journal 2014, 8, 684. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).