2. Results
The patients diagnosed with HAI had an average age of 60.27±21.67 years (mean ± standard deviation), ranging from a minimum of 3 weeks to a maximum of 99 years. Out of the total 4603 cases, 2454 (53.31%) were males, and 46.69% were females. In terms of residence, 54.16% were from urban areas, and the remaining 45.84% were from rural regions.
HAIs were most prevalent in medical sections (48.25%), followed by ICU wards (32.28%), surgical units (17.18%), neonatology (1.39%), and the ED with the fewest cases (0.90%). Regarding the type of HAI reported, enterocolitis with
Clostridioides difficile was the most common at 32.61%, followed by Covid-19 (19.83%), bronchopneumonia (16.90%), sepsis (9.04%), urinary tract infections (9.04%), surgical wound/tissue infections (8.30%), central catheter infections (2.04%), and other types of infections (2.24%). Other infections included meningitis, external ventricular drainage infections, otitis, phlebitis, and influenza-type A/B infections. Among the cases reported, 92.48% originated from the reporting hospital, and HAI was considered a possible cause of death in only 7.06% of 1176 fatal cases (
Table 1).
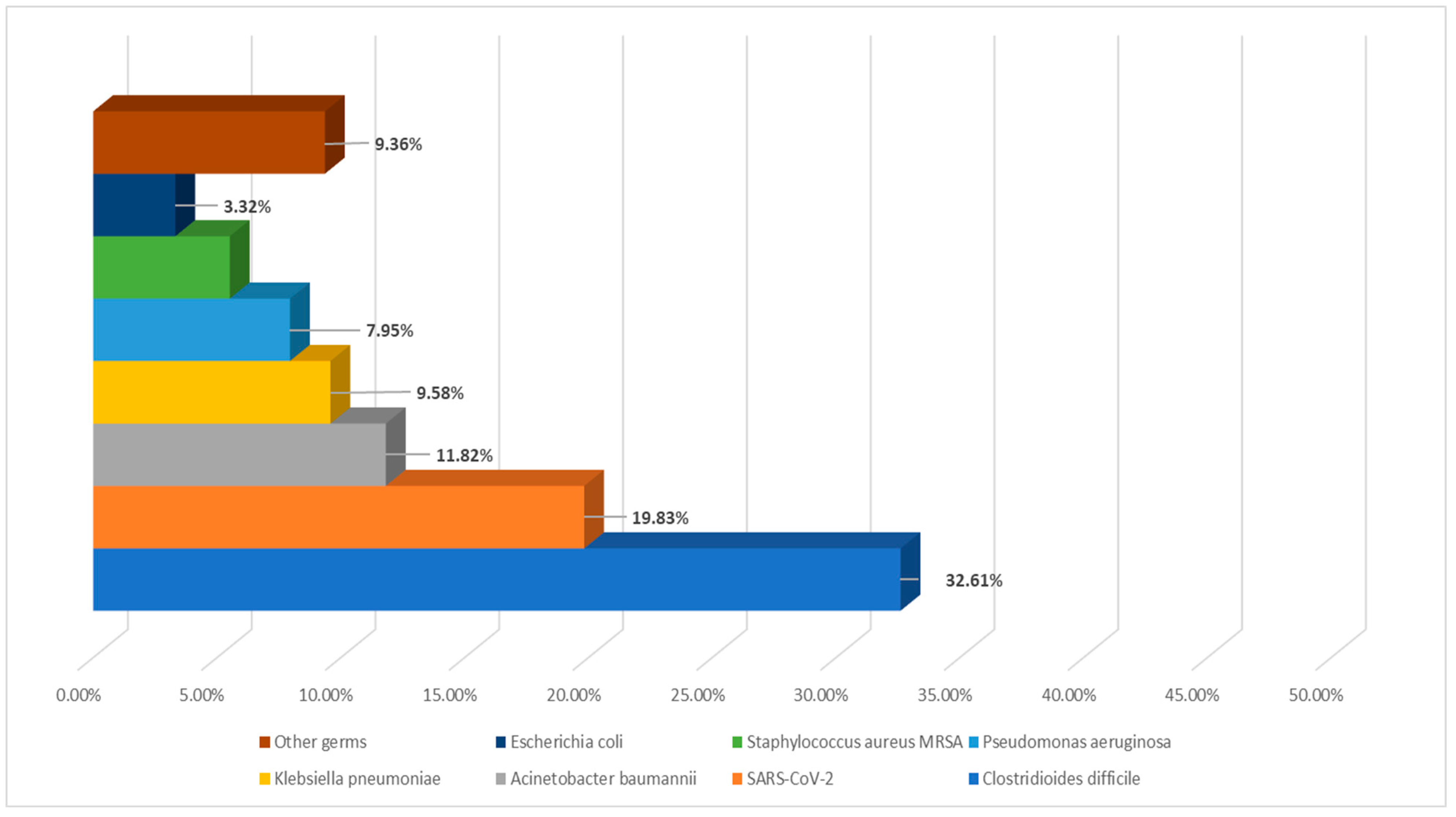
Among all reported cases,
Clostridioides difficile was the most common etiological agent isolated, accounting for 32.61%. SARS-CoV-2, identified as HAI in 2020, emerged as the second most frequent agent in the study group, comprising 19.83%, while
Escherichia coli had the lowest incidence as an HAI etiology, with only 153 cases (
Figure 1).
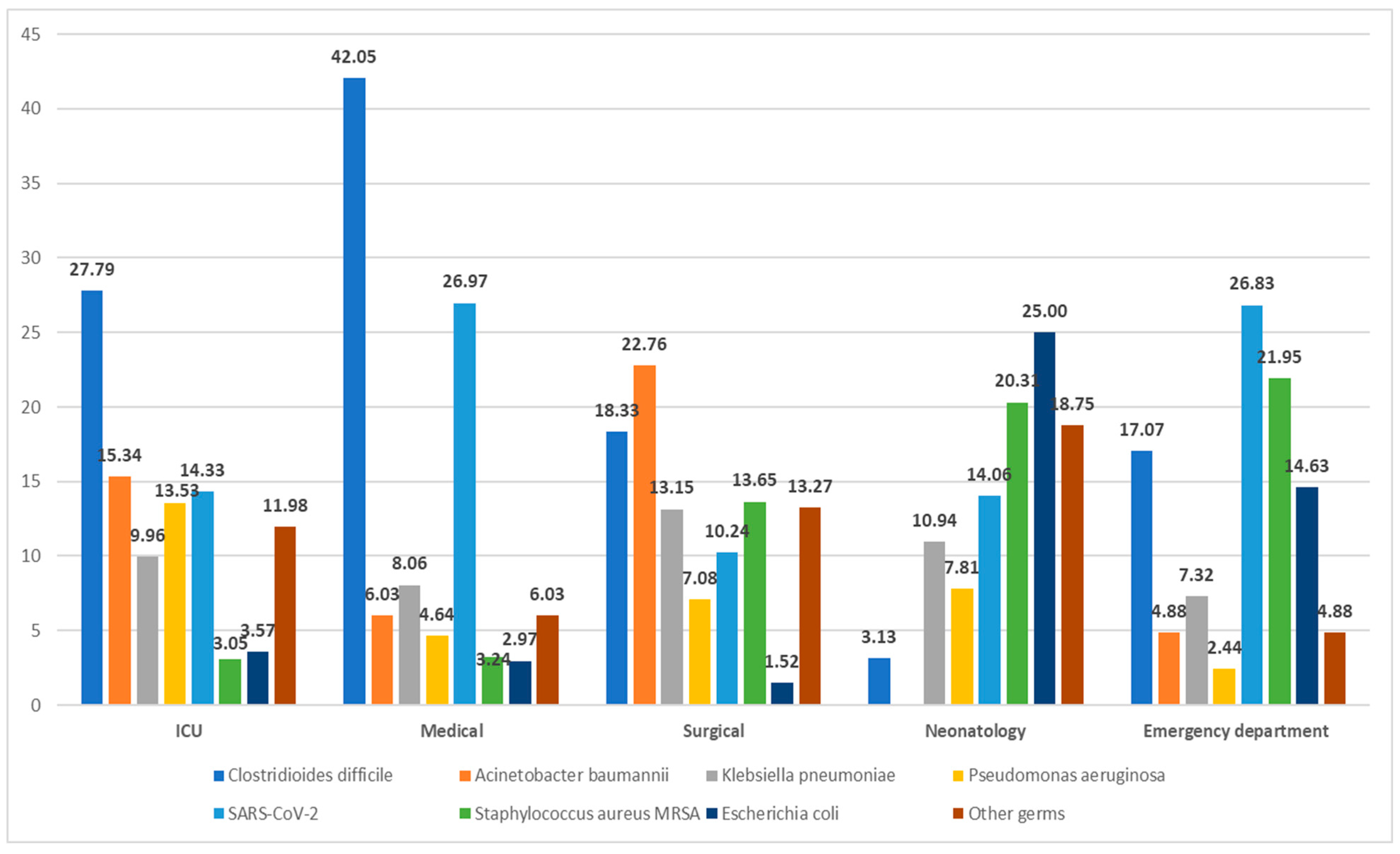
The majority of reported HAIs were observed in medical sections (2221 cases) primarily due to
Clostridioides difficile (42.05%), followed by SARS-CoV-2 (26.97%). In ICU units,
Clostridioides difficile infections were predominant (27.79%), followed by
Acinetobacter baumannii (15.34%),
Pseudomonas aeruginosa (13.53%), and
Klebsiella pneumoniae (9.96%), with
Escherichia coli being the least frequent at 3.57%. Surgical wards reported 791 HAI cases, with
Acinetobacter baumannii being the most common pathogen (22.76%), succeeded by
Clostridioides difficile (18.33%) and
Staphylococcus aureus MRSA (13.65%) among all nosocomial surgical cases. Neonatology departments identified
Escherichia coli as the primary etiological agent (25%), closely followed by
Staphylococcus aureus MRSA (20.31%). The ED reported the fewest HAI cases (0.9%), mainly attributed to SARS-CoV-2 (26.83%) and
Staphylococcus aureus MRSA (21.95%) (
Figure 2).
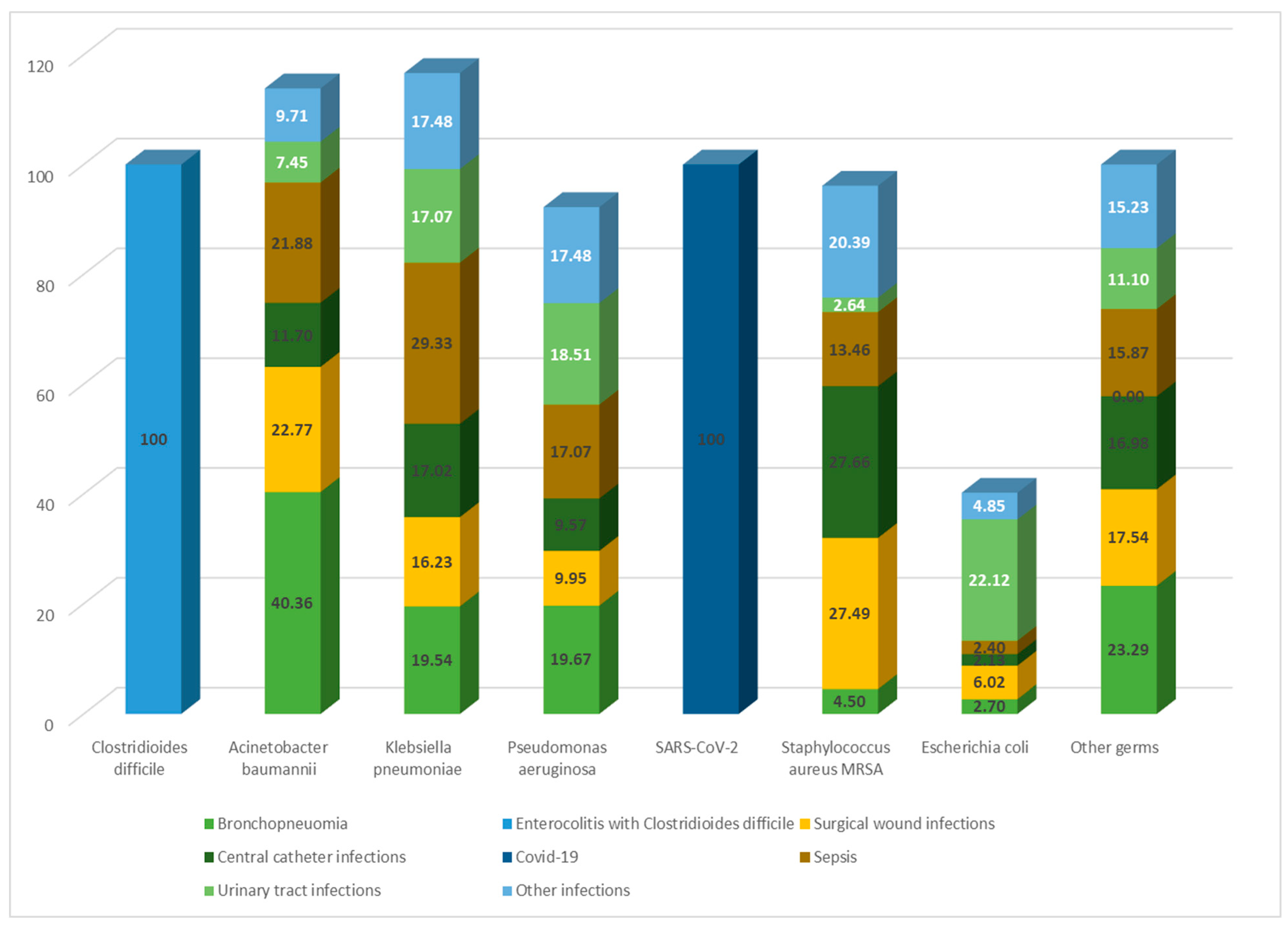
In terms of infection types, enterocolitis was the most common, exclusively caused by
Clostridioides difficile in 100% of cases. Among the 778 cases of bronchopneumonia,
Acinetobacter baumannii was the predominant etiological agent, accounting for 40.36%, followed by
Pseudomonas aeruginosa (19.67%) and
Klebsiella pneumoniae (19.54%).
Escherichia coli was the primary cause of urinary tract infections in 22.12% of cases, with this infection type being most frequently reported in medical wards and ICU units.
Staphylococcus aureus MRSA was predominantly isolated in central catheter infections (27.66%) and surgical wound infections (27.49%). The main sources of infection for sepsis were
Klebsiella pneumoniae (29.33%),
Acinetobacter baumannii (21.88%), and
Pseudomonas aeruginosa (17.07%) (
Figure 3).
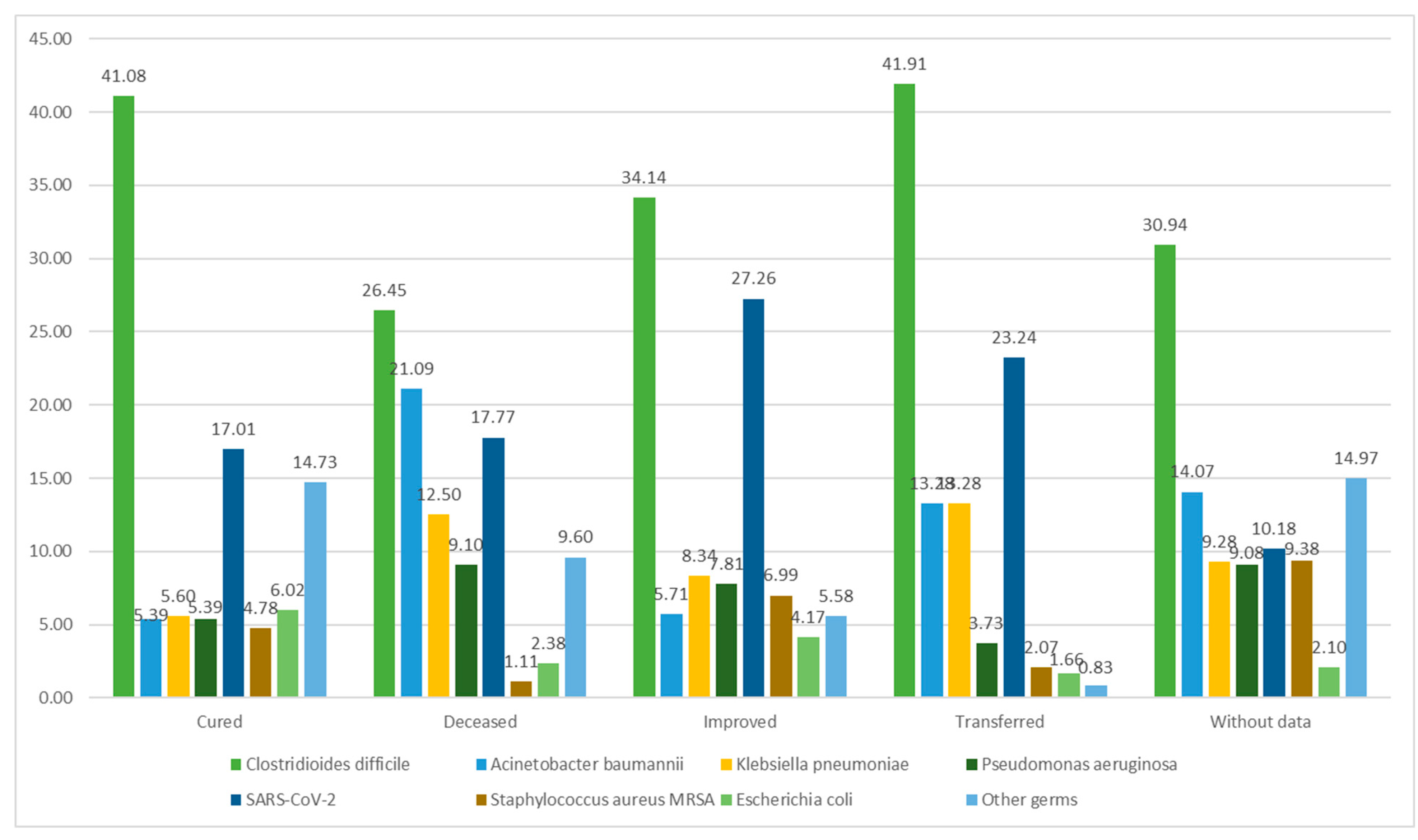
In 1176 cases, death was reported as an outcome, with
Clostridioides difficile and
Acinetobacter baumannii identified as the etiological agents in nearly half of them. The majority of patients were discharged with improved status, accounting for 36.98%. Among these cases,
Clostridioides difficile was also the most frequently isolated agent (571). A total of 481 patients were successfully treated and discharged as cured, with
Clostridioides difficile responsible for almost half of these cases (41.08%). Data on the discharge status of patients were unavailable in 1002 cases (
Figure 4).
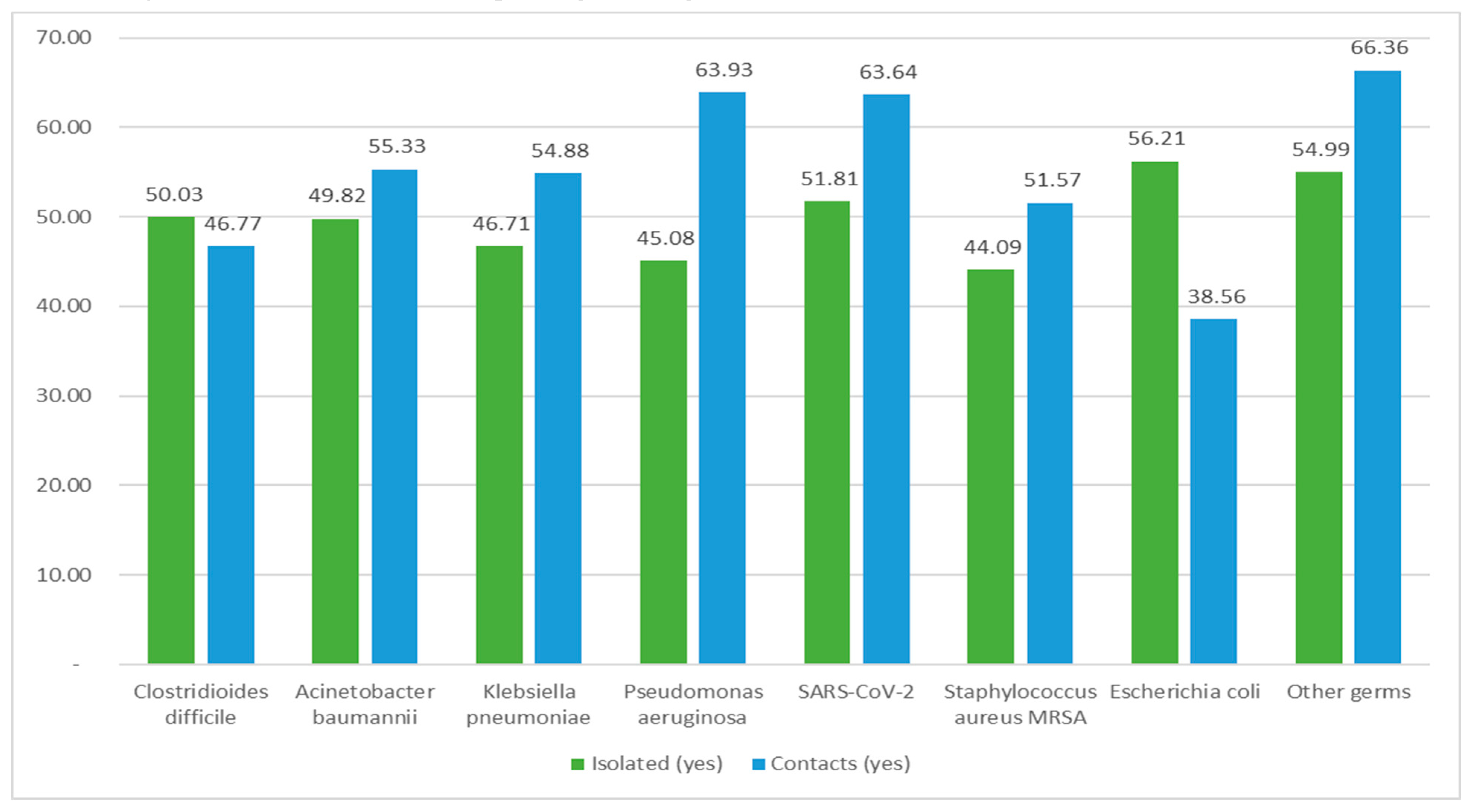
Isolation conditions were implemented in 2301 reported cases, predominantly for patients infected with
Clostridioides difficile. Contacts were documented in 2536 cases, with the majority infected by SARS-CoV-2 and other pathogens (
Figure 5).
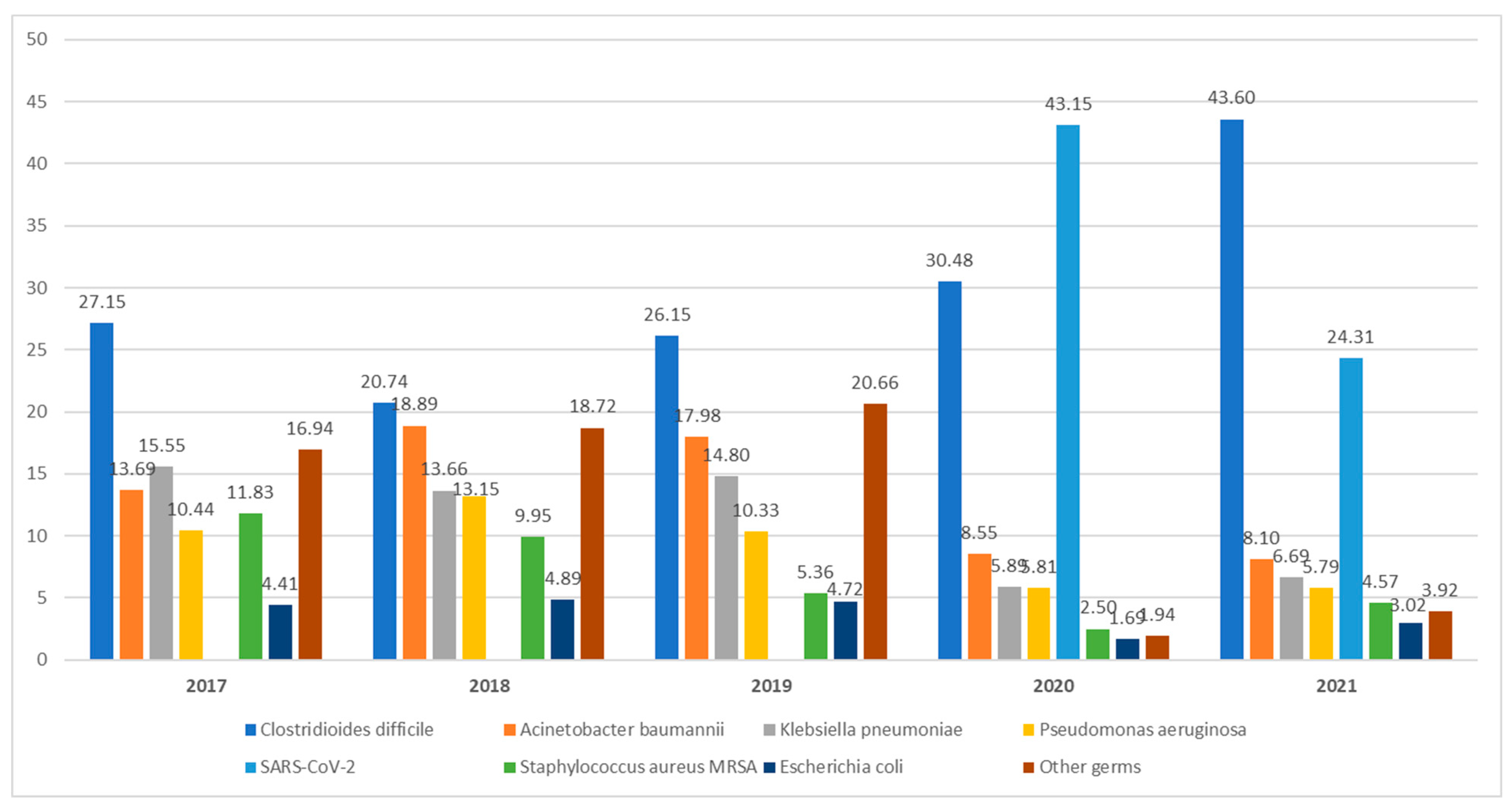
In 2017, HAIs attributed to Clostridioides difficile accounted for 27.15% of cases. During the study period, a significant increase was observed, reaching 43.60% in 2021. In contrast, nosocomial infections involving Klebsiella pneumoniae declined from 15.55% in 2017 to 6.69% in 2021. The peak number of HAI cases linked to Acinetobacter baumannii was recorded in 2018, comprising 18.89% of all 593 reported nosocomial infections. Monitoring HAIs related to SARS-CoV-2 from the pandemic's onset in 2020 until the end of 2021 revealed a decrease in incidence from 43.15% to 24.13%.
In the initial three years analyzed, Pseudomonas aeruginosa was found in more than 10% of cases each year, followed by a decrease to 5.81% in 2020 and 5.79% in 2021, Escherichia coli showed a relatively steady incidence during the first three years (4.41%, 4.89%, and 4.42%), with a slight decrease to 3.02% in 2021.
3. Discussion
This research monitored HAI cases over a span of 5 years, during which 4603 cases were documented. The average age of the participants ranged from 60 to 65 years, with ages spanning from 3 weeks to 99 years. Older individuals constituted the majority of patients requiring medical services. They form a vulnerable demographic due to their diminished immune system, influenced by both age-related factors and underlying chronic illnesses [
8]. Typically, patients diagnosed with HAIs exhibit multiple concurrent health conditions, making them susceptible to a general decline in immune competence. Prolonged or repeated hospital stays increase the likelihood of HAI, occurring not only in ICUs but also in various medical and surgical services.[
9].
All instances were documented from seven public hospitals, establishments inherently more susceptible to the proliferation of pathogens causing HAIs when compared to private institutions. Firstly, state-run hospitals accommodate a significantly larger number of patients than private medical facilities. They have a higher quantity of medical departments and limited space, making it challenging to create isolation rooms [
10]. Secondly, financially, public hospitals lack the resources of their private counterparts. Consequently, ensuring an equivalent level of cutting-edge equipment or a continuous supply of cleaning agents and disinfectants remains unfeasible. [
11]. Conversely, private hospitals might report fewer HAI cases due to potential underreporting. This omission could stem from their desire to avoid negative publicity, subsequently reducing patient attendance [
12].
In this study, it was noted that the majority of HAI cases occurred in medical departments. Before 2020, the studied hospitals primarily reported nosocomial infections in the ICU. However, during the onset of the COVID-19 pandemic, a significant shift was observed, with most HAIs being recorded in medical wards, followed closely by the ICU. In 2020, due to the surge in SARS-CoV-2 cases and the rise in critical cases, Romanian hospitals faced limited space in their ICUs. Consequently, medical departments, particularly those specializing in infectious diseases and pneumology, had to accommodate a substantial number of patients. The overcrowding in these departments, coupled with the prolonged hospital stays of COVID-19 patients, increased the risk of nosocomial infections in these areas.
Additionally, there was a shift in the predominant type of HAI infection. While bronchopneumonia caused by Acinetobacter baumannii was the most common type between 2017 and 2019, starting from 2020, enterocolitis associated with Clostridioides difficile became the most frequently reported infection. Consequently, over the five-year period, enterocolitis stood out as the most prevalent infection, documented in a total of 1,501 cases, with 62.23% of them within medical wards.
Clostridioides difficile emerged as the most frequently detected pathogen responsible for HAIs, constituting 1501 out of 4603 cases. Notably, compared to the pre-pandemic years when Acinetobacter baumannii was predominant,
Clostridioides difficile exhibited a significant surge in its incidence rate. Particularly striking was the rise coinciding with the emergence of the SARS-CoV-2 virus, accounting for nearly half of all HAI cases in 2021. Indeed, the occurrences of
Clostridioides difficile infections in the period 2020-2021 surpassed those reported between 2017-2019. Several factors could explain this trend. Firstly, during the pandemic, healthcare facilities faced overcrowding, making it challenging to isolate potential community cases effectively. Consequently, bacterial transmission among patients became inevitable. Similar limitations in isolation protocols were observed concerning HAI with
Clostridioides difficile, where strict isolation measures would have been necessary. Secondly, recent research indicates that
SARS-CoV-2 can persist and replicate in the intestinal environment for extended periods. Moreover, the findings from Lin et al. study [
13] revealed that a portion of patients (27.3%) exhibited no lung imaging characteristics of COVID-19. Instead, they presented gastrointestinal symptoms, underscoring the susceptibility of gastrointestinal tissues to
SARS-CoV-2. The interaction between
SARS-CoV-2 and the renin-angiotensin-aldosterone system leads to reduced local anti-inflammatory responses. This viral cycle triggers an excessive imbalance in immune responses and cytokine release. Post-viral infection, the downregulation of angiotensin-converting enzyme 2 causes gastrointestinal dysfunctions. Consequently,
SARS-CoV-2 infection might heighten susceptibility to
Clostridioides difficile infections, given the opportunistic nature of this bacterium. [
14].
Furthermore, managing antibiotic treatment for COVID-19 patients presents challenges due to similarities between bacterial pneumonia and moderate to severe COVID-19 cases. Although current guidelines suggest using empiric antibiotics only when bacterial infections are suspected in moderate COVID-19, they are routinely recommended for severe COVID-19 cases. Distinguishing between advancing COVID-19 illness and bacterial co-infection or superinfection is challenging. The decision for empiric antibiotic treatment might be influenced by experiences from Influenza cases, where bacterial co-infection rates range from 11% to 35%. [
15]. Despite this, hospitals commonly utilize prophylactic antibiotic therapy. Studies indicate that antibiotic treatment for bacterial infections in hospitalized COVID-19 patients leads to the depletion of beneficial commensals and the proliferation of opportunistic pathogens, including
Clostridioides difficile [
16].
A crucial issue to address concerning
Clostridioides difficile infections is the management and treatment of this condition.
Clostridioides difficile, being a widespread organism, has developed unique survival mechanisms that enable its successful proliferation in the competitive gut environment. This pathogen's remarkable adaptability is largely attributed to the diversity of its genome. When
Clostridioides difficile encounters cellular stress, it employs two survival strategies: producing a toxin and forming a protective coat through sporulation. Sporulation aids its persistence in the gut or facilitates an escape. Considering the rising number of cases and the bacterium's exposure to various treatments, there has been an increase in its resistance to antibiotics. Metronidazole exhibits low bioavailability in the colon, leading to fecal concentrations ranging from 0.8 to 24.2 µg/g stool [
17]. This phenomenon may account for metronidazole nonsusceptibility, as exposure to subinhibitory concentrations might have played a role in the selection of resistance. Oral vancomycin is increasingly being utilized as the primary treatment option, driven by recent updates in treatment guidelines as well as concerns related to costs and availability. A study conducted by Darkoh and colleagues [
18] identified
Clostridioides difficile isolates with reduced susceptibility to vancomycin in patient populations from two distinct geographic locations on different continents – Houston and Nairobi. The results revealed that 26% of patients in Houston and 67% of patients in Nairobi, suffering from enterocolitis with
Clostridioides difficile, carried bacterium isolates that were not susceptible to vancomycin. Fidaxomicin has demonstrated superiority over vancomycin in preventing recurrent enterocolitis with
Clostridioides difficile. This superiority might be attributed to its narrow spectrum of activity, which allows the gut to restore a normal microbiome. Additionally, fidaxomicin inhibits
Clostridioides difficile sporulation and the production of toxins. The inhibition of sporulation by fidaxomicin could potentially reduce the transmission of the infection to others by decreasing the shedding of spores and subsequent environmental contamination [
19]. While some studies indicate that fidaxomicin, as opposed to vancomycin, decreases the risk of recurrent enterocolitis caused by
Clostridioides difficile [
20], the use of fidaxomicin comes with substantial costs that surpass the financial constraints of state hospitals. Consequently, Fidaxomicin remains an impractical treatment option for most state-funded medical facilities. Modern medicine requires further research to explore innovative solutions for managing this infection, focusing on both prevention and treatment of the infection and its recurrence.
Apart from enterocolitis, the leading types of nosocomial infections included COVID-19, bronchopneumonia, urinary tract infections, sepsis, and surgical wound infections. Bronchopneumonia was notably frequent in ICU cases, with
Acinetobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumoniae, and
Staphylococcus aureus MRSA being the primary causative agents, especially prevalent in ICU sections. The extensive use of tracheal intubation and mechanical ventilation for critically ill patients further heightens the risk for this condition among patients already susceptible [
21]. In line with our findings, a cohort study conducted by Trivedi et al. [
22] revealed that the most common isolates in ICU nosocomial pneumonia were
Pseudomonas aeruginosa (55%),
Acinetobacter baumannii (20%),
Staphylococcus aureus (14.5%), and
Klebsiella pneumoniae (7.5%). A limited number of nosocomial lower respiratory tract infections were linked to
Escherichia coli. Aspiration and mechanical ventilation were identified as risk factors for this condition. In recent years,
Escherichia coli with extraintestinal pathogenicity has attracted attention and is believed to cause a range of infections, including bacteremia, urinary tract infections, prostate infections, pneumonia, liver abscesses, meningitis, and brain abscesses [
23].
Urinary tract infections accounted for 416 cases, predominantly caused by
Escherichia coli. More than half of these cases were reported in the ICU and medical departments. In a comprehensive retrospective study, Machado et al. [
24] analyzed the prevalence of HAIs caused by extended-spectrum beta-lactamase - or carbapenemase-producing
Escherichia coli. Their findings indicated alarming prevalence rates, possibly underestimated due to clinically diagnosed HAIs, highlighting the persistence and spread of these bacteria in healthcare institutions in Portugal. Similar epidemiological trends have been reported in other countries as well.
We discovered that among the HAIs, 416 were identified as sepsis, with
Klebsiella pneumoniae infections being the most common culprit, accounting for 122 cases. The majority of systemic infections were detected in ICU wards.
Klebsiella pneumoniae was also isolated in 62 cases of surgical wound infections and 16 cases of urinary tract infections. The significant challenge in dealing with
Klebsiella pneumoniae infections lies in limited treatment options due to extensive antibiotic resistance, leading to heightened morbidity and mortality rates. The widespread and inappropriate use of carbapenems can result in challenging-to-control epidemics, particularly in intensive care units, owing to the acquired resistance to this group of antibiotics. Outbreaks and isolated cases caused by carbapenem-resistant
Klebsiella pneumoniae species have been increasingly reported worldwide in recent years [
25].
Surgical wound infections and central catheter infections are frequently identified in both ICU and surgical wards. It's essential to consider that some ICU patients were initially in surgical wards. Additionally, patients reported with HAIs in surgical wards might have had ICU exposure during postoperative care, indicating potential infections originating from the ICU.
In the case of neonates, although they accounted for only 1.39% of reported HAI cases, it's crucial to highlight the prevalence of Escherichia coli and
Staphylococcus aureus MRSA infections in this group. Newborns in neonatal ICUs, especially preterm infants, face elevated infection risks due to factors such as immature immune systems, extended hospital stays, and frequent use of invasive devices and antibiotics.
Staphylococcus aureus MRSA infections are particularly common in neonatal ICUs, leading to severe conditions like pneumonia, osteomyelitis, and bacteremia. [
26]. Neonatal bloodstream infections often result in
Staphylococcus aureus MRSA-related sepsis, associated with high mortality rates. Studies have revealed the endemic presence of
Staphylococcus aureus MRSA in numerous neonatal ICUs, causing invasive diseases and death [
27,
28].
Escherichia coli stands out as a major pathogen causing neonatal infections, particularly meningitis and sepsis in developing countries. Recent increases in its incidence and drug resistance pose significant threats to neonatal health. Plasmid-borne extended-spectrum beta-lactamase (ESBL) genes lead to
Escherichia coli resistance against β-lactam antibiotics like cephalosporin, resulting in treatment challenges worldwide. A study published by Xiao et al. [
29] found that some
Escherichia coli strains were resistant to carbapenem antibiotics, including ertapenem, doripenem, meropenem, and imipenem. Carbapenem resistance can occur through various mechanisms, severely limiting treatment options for multidrug-resistant
Escherichia coli, particularly ESBL and carbapenem-resistant
Enterobacterales (CRE) infections in neonates. Consequently, there is an urgent need to focus on surveillance, prevention, and management of ESBL and CRE to enhance the accuracy of neonatal infection diagnosis and the rational use of antibiotics.
Considering our study, which highlighted a gradual decrease in reported cases of HAIs caused by
Acinetobacter baumanii, Pseudomonas aeruginosa, and Klebsiella pneumoniae strains, particularly in the last two years, 2020 and 2021, we attribute this trend to potential underreporting. Numerous recent scientific articles have demonstrated a significant rise in HAIs with these strains since the onset of the COVID-19 pandemic [
30,
31]. A review study published in June 2023 has shown an overall increase in drug-resistant bacterial infections involving
Streptococcus pneumoniae, Klebsiella pneumoniae, Haemophilus influenzae, Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, and Acinetobacter baumannii, correlating with the heightened use of antibiotics in COVID-19 admissions [
32]. Contrary to the literature findings, the lower incidence of infections with these agents observed in our study during the pandemic period (2020-2021) could be attributed to underreporting. The medical staff's exclusive focus on diagnosing and treating
SARS-CoV-2 infections, along with laboratories being burdened by COVID-19 testing, likely resulted in a partial interruption in detecting these bacteria.
In the post-pandemic era, it becomes crucial to resume accurate reporting of HAI cases in hospitals.
Additional comprehensive studies are essential to assess the current antibiotic resistance of reported germs causing HAIs. Implementing preventive measures to safeguard patients against these infections and adopting appropriate therapeutic interventions for confirmed nosocomial infections is imperative.
Limitations of the study
The research was conducted solely at the county level, making it insufficient to draw valid comparisons with other regions in Romania. The data utilized were incomplete regarding patients' risk factors and comorbidities. Additionally, the discharge status of a significant number of cases remained unknown.
4. Materials and Methods
We conducted a cross-sectional study analyzing cases reported by public hospitals in Mures County (Romania) to the Mures Public Health Directorate. This included county clinical hospitals, a cardiovascular disease institute, municipal hospitals, and a city hospital. No cases were reported from private hospitals. The study focused on HAIs reported between 2017-2021, totaling 4603 cases. Data analysis considered patient demographics, hospital departments, diagnoses, surgical procedures, HAI diagnoses, isolation protocols, pathogens involved, antibiotic resistance, treatment details, patient status upon discharge, and potential links between HAI and patient deaths. The study encompassed various medical and surgical departments, which were later categorized into ICU, surgical units (general surgery, plastic surgery, obstetrics and gynecology, orthopedics, neurosurgery, urology), medical units (infectious diseases, cardiology, diabetes, hematology, gastroenterology, palliative care, internal medicine, neurology, nephrology, oncology, pediatrics), neonatology units, and emergency departments (ED) for statistical analysis. For processing the data, we received the consent of the Mures Public Health Directorate, and confidentiality and anonymity were maintained.
HAI identification and diagnosis in Romania
On September 30, 2016, the Romanian Minister of Health issued Order No. 1101/2016 [
5], approving the regulations for the supervision, prevention, and containment of infections associated with medical care in healthcare facilities. According to this document, an HAI is defined as an infection acquired in healthcare settings (both public and private) and encompasses any infectious disease identifiable clinically and/or microbiologically. It must have epidemiological evidence indicating contraction during hospitalization or medical/surgical procedures. The incubation period of these infections is linked to the duration of medical care received by the patient in these facilities, regardless of whether symptoms appear during the hospitalization period. To diagnose HAIs, it is crucial to establish that the infection resulted from hospitalization or medical care in healthcare settings and was not present during the incubation/initial phase of the disease at the time of hospitalization or medical procedure.
When a physician suspects an HAI, they promptly notify the hospital's HAI prevention department, following the European Union's specified case definitions. The microbiology lab investigates suspected cases within 24 hours. Upon germ identification, bacteriology notifies the Public Health Directorate and relevant medical departments, especially when multidrug-resistant germs are isolated. The attending physician collaborates with an epidemiologist to assess the case clinically and classify it as confirmed, denied, or colonization based on definitions. The attending physician completes signs and files the HAI case statement, including the diagnosis in clinical records. The HAI diagnosis (coded Y95) is recorded in the general clinical observation sheet and computer system at the patient's discharge or transfer. The responsible physician ensures data accuracy. Suspected cases trigger daily electronic reports, while confirmed cases are reported weekly to the HAI prevention department. At the hospital level, the department maintains centralized records and prepares epidemiological investigations, implementing measures to prevent pathogen transmission. Monthly, quarterly, and annual reports on HAI incidence, categorized by sections and infection types, are submitted to the hospital's Steering Committee and the county's Public Health Directorate.
Statistical analysis
We utilized Statistical Package for Social Sciences (SPSS) for statistical analysis. Normally distributed quantitative data, such as age, were expressed as mean and standard deviation. Qualitative data were represented as counts and percentages.