I. Introduction
In an evolving medical world, remote monitoring and data collection is increasing in popularity. Wearable sensor technologies have been used in medicine for many years. Devices such as heart rate monitors, pulse oximeters on fingertips, or even dry epidermal electrodes have been in constant use to aid medical professionals in diagnosing patients [
1]. The ability to monitor the day while they are on the go provides deeper insight into the average physical load on a patient's cardiovascular system. This allows for a more comfortable and reliable reading, as the stressful location of a hospital is not necessary. Generally, blood pressure monitoring can be used to diagnose several issues, but wearable ultrasonic sensors are one of the technologies that can provide ischemia monitoring to diagnose blood flow issues in diabetics, recent traumatic injuries, or those susceptible to blood clots. By continuously monitoring blood pressure, medical professionals can detect inadequate pressure, the main observable characteristic in an ischemic patient. Treatment of blunt trauma to the limbs must be constantly monitored for ischemic conditions, as the potential damages caused by missed detection can result in serious conditions [
2]. Through continuously monitoring biosensors, these conditions can be under alarm for these patients. Early detection of ischemia symptoms can be lifesaving, and extended use may provide greater insight and data to assist in further cardiovascular research [
3].
The condition of Ischemia can manifest itself in a few ways. Whether it be a slow loss of blood flow through plaque buildup in arteries or a damaged artery during an accident, Ischemia can go unnoticed in patients for a long time before any diagnosis is made. Monitoring for Ischemia is important for this reason, as it can be a preventable issue that is often hard to see without long-term data collection [
3].
Ultrasonic devices emit sound or light waves that reflect off of the intended object, in this case, blood vessels, and echo back into a receiver. The wave's travel time data is then recorded and used to map the vascular system of the patient. The compact, low-noise circuitry of the biosensor transmits data to a software program that can exist on computers or phones and then uses a machine-learning algorithm to model the patient's cardiovascular health. Most of the ultrasonic biosensors that are tested research at the moment are small devices [
4]. Related to the size of a postage stamp, the compact device is powerful enough to reach deep tissues, major blood veins, and even some organs such as the heart. However, there are also studies conducted on larger sensors that, for example, can be inserted as in-soles at the bottom of a patient's foot [
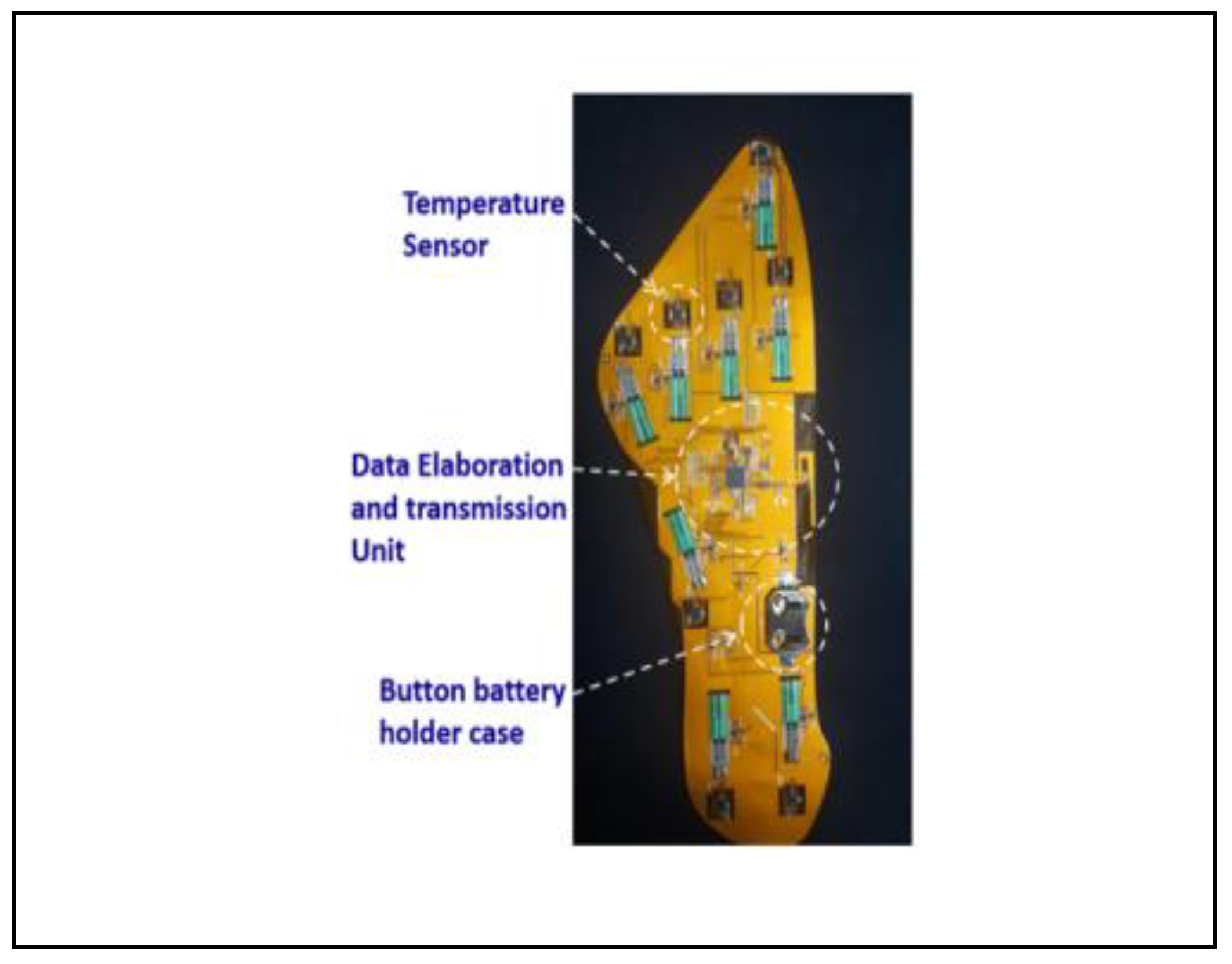
5]. The extremities of the body, such as the hands and feet, have a higher likelihood of showing ischemia symptoms due to clogged or constricted arteries. This is seen predominantly in diabetes patients; therefore, a larger and more robust sensor is required to be comfortable and effective in shoe wear, as seen in
Figure 1 [
5].
Through many iterations and tests, cardiovascular monitoring has used ultrasound technologies for speckle tracking echocardiography, tissue Doppler imaging, color Doppler flow mapping, coronary flow reserve, and carotid stiffness [
6]. This paper intends to highlight the current and future technologies, studies, and challenges associated with the use of wearable ultrasonic sensors for blood pressure monitoring through a review of academic articles. This review will provide the reader with insight into technologies that will benefit the general population through the goal of widely distributed and affordable cardiovascular monitoring.
II. Technology Review
A. Ease of Use
Although they contain instrumentation, circuit boards, and other various electrical and control components, the wearable ultrasonic sensor is flexible and reliable through a combination of polymer and semiconductive materials [
7]. This information is important to consider if ultrasonic sensors are to be used for stress testing. The allure of wearable sensors is often attributed to the ability to conduct tests on patients from the comfort of their own homes as they go through their day. Yet, those with active lifestyles may see an issue in the rigidity of an electric sensor attached to their leg, arm, chest, etc, as seen in
Figure 2. In a similar fashion, unobtrusive monitoring may be used for testing seniors and children, those groups that require a more comfortable alternative [
8].
Intensive cardiovascular activities can provide medical professionals with an extra layer of certainty and information for diagnoses. Researchers are working to ensure that not only will the sensor remain elastic and unbroken throughout the tests but will stay attached close enough to the patient's skin to provide meaningful data free of outside noise [
9].
B. Controls System
The ultrasonic sensors have very few components that serve as non-invasive and unobtrusive to wear throughout one's day. The ultrasonic sensors in most recent use serve as a primary device, providing data collection for a more robust and powerful primary device to do a deep analysis. The wearable ultrasonic consists of a sensor for blood pressure but can also include other technology, such as temperature probes, to collect even more data to find correlations for a more exact diagnosis. The patch then transmits that data to a microcontroller, such as an ARM Cortex-M3 multiprotocol wireless microcontroller unit, for collection [
5]. This also involves small circuitry and a battery to power and control the unit itself. Outside of these characteristics, many studies have various added components that serve similar purposes but reach that destination differently.
To send the data to the primary device, the sensors can include a wired or wireless transmission device, the latter of the two being the more desired option. The Bluetooth connection provides the ability to connect to an array of devices, such as cellphones, laptops, and computers. In order to see widespread medical use, however, some sensors use an encryption method. For most uses, the ultrasonics do not continuously monitor blood pressure but take sample data randomly throughout the day. This can extend battery lifetime but can also solve the security issue for data transmission in wireless sensors. Between the short burst and encryption of data communication, researchers can ensure the security of the testing [
10]. Wifi and 3G transmission times were tested and shown in alarming monitors for various cardiac transients, measured at less than a minute between alarm communication between devices under 3G networks [
11]. Data collection time and reliability are relatively low for these examples, and as the nationwide coverage for cellular data continues to expand, researchers can lower this transmission time, keeping the data collection reliable. By lowering transmission time, there is a lower chance of data being intercepted.
In control systems, a major concern is noise. Noise is a disturbance in the accuracy of instrumentation equipment and can arise from a number of factors. When dealing with ultrasonic sensors, typically high-frequency sound waves, but occasionally light noise can be an issue with wave interference and scattering [
12]. In a related study, it is noted that no wearable biosensor has successfully eliminated all background noise in sensors used to detect cigarette smoking, and such principles apply here [
13]. One challenge to overcome for researchers is to reduce and account for noise as best as possible. This can be accomplished through heavy analysis of large data sets to account for natural disturbance, as well as ensuring the transducer in the sensor is accurately reading the ultrasonic waves it produces.
The size of the sensors does not allow for a powerful returning wave to be measured. One study found that of the light output from their sensor to muscle tissue, the amplitude of the returning wave was 0.1% of the output. To confidently ignore outside noise and obtain reliable data, many sensors require a pre-amplified signal output to strengthen the reflected waves [
14].
III. Proof of Concept
A. Ischemic Conditions
Ongoing research continues as studies are released detailing the successful monitoring practices. Many studies are documented in a controlled environment, with prototype sensors and volunteers used to test the effectiveness of wearables.
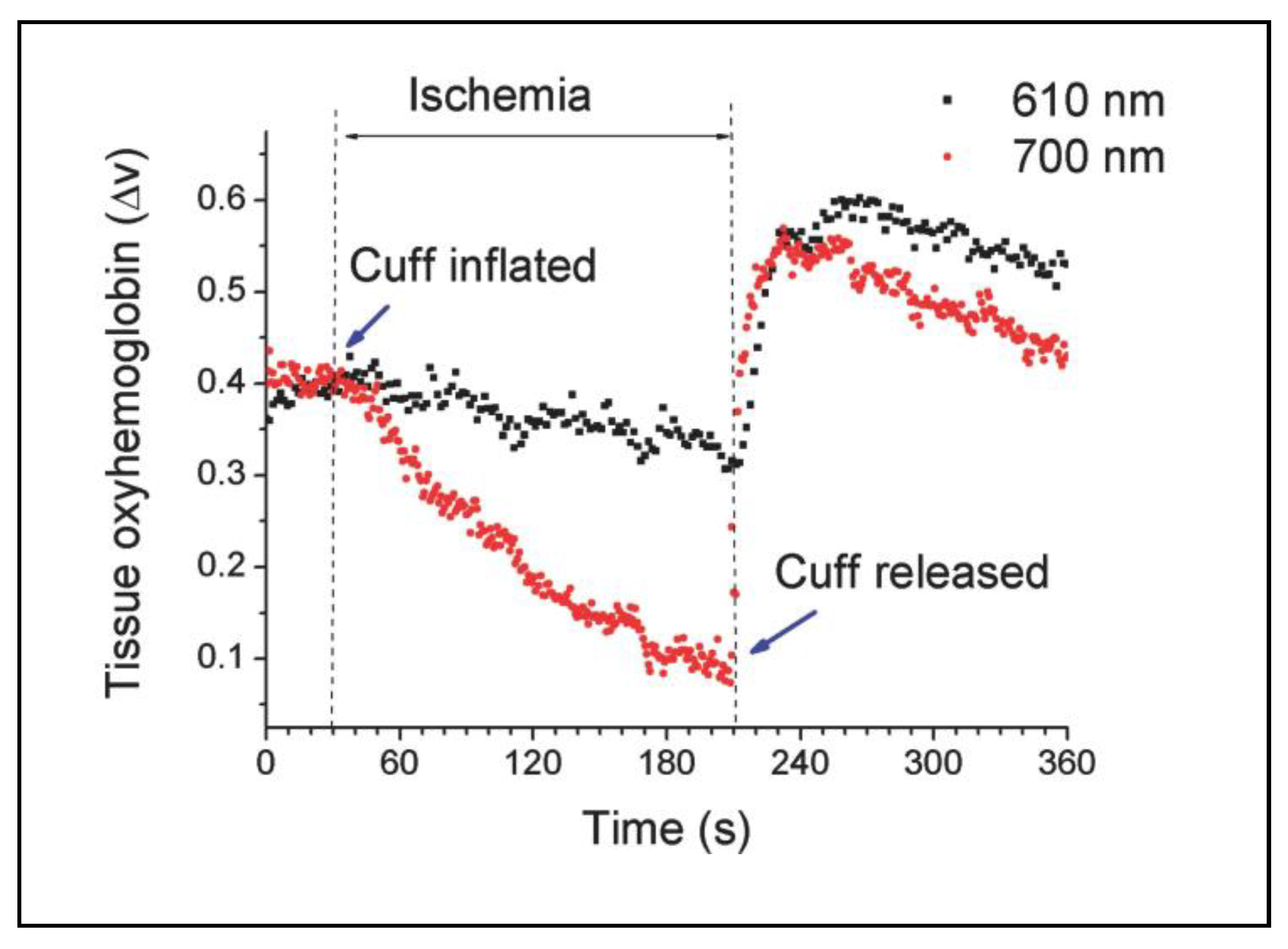
In an Advanced Materials study, researchers developed an ultrasonic sensor for monitoring ischemia [
14]. They subjected patients to a routine inflation blood pressure test in the upper arm, using the sensor to read the data from the lower arm near the wrist. The developed sensor uses two wavelengths of light to test the effectiveness of different spectra. The outcome of the study, shown in
Figure 3, measures the oxygen levels in blood under ischemic conditions over a period of time. The outer limit of visible light, 700 nm, seen as humans as red toward the infrared light wave of the electromagnetic spectrum, was highly successful in modeling the changes in the patient's blood oxygen level. By inducing ischemic conditions, the oxyhemoglobin levels dropped dramatically, spiking above normal conditions after the cuff was released. This measurement spike aligns with current medical knowledge of blood pressure tests, as the blood vessels dilate during Ischemia to allow more blood flow before contracting to normal rates after release [
14].
The significance of this test is to prove that ultrasonic sensors are capable of providing adequate data on blood oxygen levels. The crux of ischemia monitoring is this conclusion. Although these conditions and blood pressure monitoring systems have been in medicine, the key advantage of this tested biosensor is the performance, sensitivity, flexibility, and ease of fabrication over other sensing techniques [
14]. The proof of concept from this study confirms the effectiveness of tissue-level biosensors measuring Ischemia in patients.
B. Cardiac Alarming
Reading real-time patient data was tested for a controlled subset of patients. The category of patients tested and a primitive analysis of the data collection is presented. The goal of this study is to detect alarms for cardiac behavior outside of an expected range [
11]. A study of this nature relates to ischemia monitoring through the data points collected. Abnormal activity limits can be set on a per-patient basis set by the medical professionals based on the patient age, cardiovascular system health, etc. This is important to keep in mind as data sets continue to grow and studies continue to be conducted.
To monitor Ischemia, there is nuance on a patient-to-patient basis, so more tests are required to ensure proper analysis of data sets. In blunt traumatic injuries, cardiac abnormality alarms can be particularly helpful. Measuring patient blood pressure in extremities at a near-constant rate can prove helpful to set baselines for alarming. If there is a measured continuously low blood pressure rate, conditions similar to those seen in
Figure 3, medical professionals may be alerted to take precautions related to such conditions.
IV. Challenges, Future, and Discussion
There is proven and documented evidence of the successes of wearable sensors, but as more research is conducted, there are always difficulties. In an interview conducted with authors Muyang Lin and Ziyang Zhang from the University of California San Diego after issuing an article on their deep tissue monitors, Zhang was questioned about the greatest difficulties they faced during their testing [
4]. Converting the recorded data into a comprehensible and reliable output was specifically difficult. Accounting for the unpredictable data entries from device misuse on the patient end proved challenging for their machine learning-based model. Each patient will have their own specific differences, issues, and appropriate use, so collecting and modeling reliable data will require a smart and fast learning model. Constantly adapting and improving their data analysis was a technical difficulty, but Zhang was optimistic that through large data collection and studies, the team would be able to continuously improve their models [
4].
Outside of the technological aspects of remote monitoring, there will be difficulties in adopting the sensors on a widespread and affordable scale. The goal of wearable sensors is to provide extensive monitoring in a compact and economically viable way. By reducing hospital visit time and providing patients with a means to measure and self-manage the health of their cardiovascular system, the average consumer can see reductions in medical costs. Off-the-shelf biosensors such as Apple Watches, Zio Patches, and Google Glass devices already provide a deeper insight into the benefits of monitoring and maintaining an active lifestyle [
15].
The connection between medical professionals and their patients can extend beyond the hospital through the Internet-of-Things framework, the system of data collection, analysis, and transmission over the Internet. This can raise concerns about patient privacy, and as new technologies emerge, it is important to provide transparent and accurate information to consumers who are concerned about their medical information being wirelessly transmitted. This difficulty will only continue to cause issues in the field; therefore, there must be regulations and rules carefully imposed upon the real-world use of wearable sensors [
15]. Finding a balance between the strength and integrity of the sensor and the compatibility with human skin is a major concern for regulation. Toxic materials must be avoided, yet the sensors must maintain their effectiveness [
16]. Researchers must maintain a careful balance of safety, cost, and reliability when producing biosensors for real-world use.
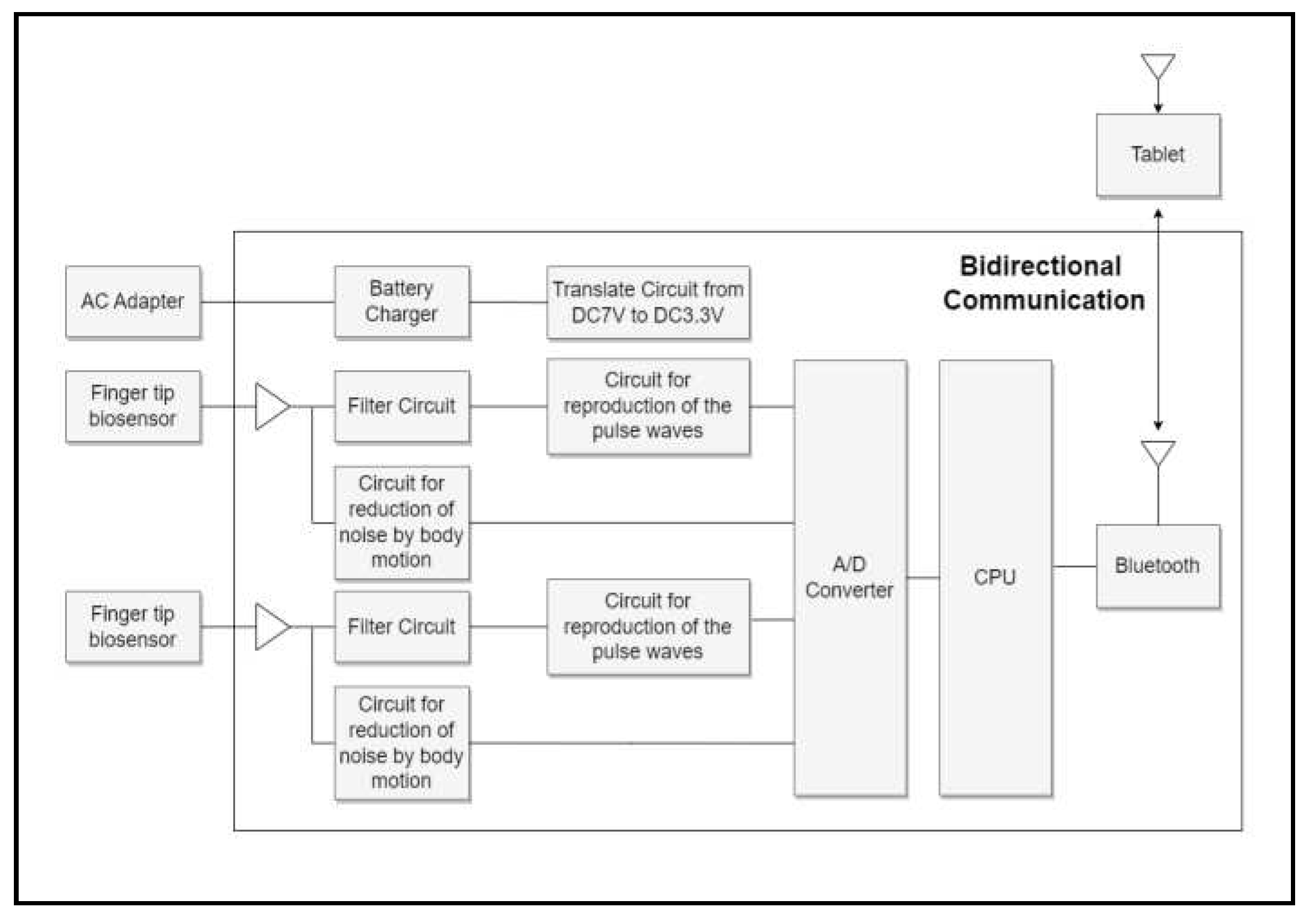
Naturally, the use of ultrasonic sensors has a reach beyond ischemia testing as well, though the same techniques and processes still apply. Researchers are developing blood pressure sensors for integration into steering wheels, for example. Through touch infrared biosensors, researchers have been able to read blood pressures at the fingertips of drivers to monitor the health of professional drivers [
17]. A block diagram shown in
Figure 4 illustrates the data collection system for this example. The reach of ultrasonic cardiac sensors is vast and continuously growing. Ischemic conditions in chronically ill and recently traumatic injured patients are a small subset of those who will benefit from ultrasonic sensor research in the future.
The block diagram, although used for general blood pressure monitoring, is an example of how the biosensors work on a macro scale. The sensor takes the input data and immediately applies a filter circuit to improve the accuracy of the input wave in the junction with a feedback loop. The feedback loop for the steering wheel example must focus on reducing noise resulting from inadequate contact and movement by the user, technologies also seen in use with ischemia sensors, although not as prevalent as this example. The signal then reproduces the photoplethysmography, the technical term for the signal detecting the volume of the blood vessels, wave initially read by the sensor, and converts that incoming analog signal into digital signals via the A/D converter. The final, noise-reduced signal of the blood pressure reading is then collected and analyzed via a combination of CPUs and wireless connection devices [
17]. It may also be beneficial to medical professionals to include other various analog signals to generate a more accurate diagnosis from the subset of data. When looking at data for diabetes patient's blood pressure in the extremities, temperature and pressure readings can help give insight into the parameters that restrict blood flow [
5]. It is important for the future of wearable sensors that researchers design their sensor to include the maximum number of readings that can benefit medical professionals while keeping the sensor's price and footprint as minimal and non-invasive as possible.
This technology for the blood pressure readings is an accurate example of the control circuit for ischemia readings. The signal processing through the filters and analog to digital converters would work the same in a touch sensor as a wearable ultrasonic sensor, with adjustments made for the signal filtering strength.
Wearable ultrasonic biosensors are in continuous testing and development to provide reliable and mass-scale use in the future. The ability to read a patient's blood pressure levels to monitor for ischemic conditions will prove highly beneficial in diagnosing issues before they manifest themselves in major. The ease of use for a patient to be monitored throughout their daily life and the comfort being improved for those wearing them are the initial evidence to warrant increased use. The deep understanding medical professionals will gain from large data sets captured by the sensor can make way for further studies and an improved response time for medical emergencies. The technology and software associated with biosensors continue to evolve, as shown in this review.
Ischemia monitoring is just one example of the medical advancements that can benefit from the widespread use of wearable ultrasonic sensors in cardiovascular systems. The field is expanding into smoking detection, respiratory health, and much more.
V. Conclusion
This review aims to analyze the current technologies used to monitor cardiac behavior in patients through wearable ultrasonic sensors. A study of current research on ischemic conditions and related fields provides insight into the current and future landscape of at-home monitoring systems. The future of wearable ultrasonic sensors is bright as the general population will soon be able to benefit from all of the technologies presented in this review, provided the implementation into medical institutes is handled with the proper care.
References
- J. Heikenfeld, et al, "Wearable sensors: modualities, challenges, and prospects," Lab Chip, Volume 18, 2, pages 209-386, October 2018.
- R. Petre, et al, "Lower limb trauma with injury to the popliteal vessels," The Journal of Trauma: Injury, Infection, and Critical Care 40, pages 595-601, April 1996.
- Institute of Medicine (US) Committee on Social Security Cardiovascular Disability Criteria, "Cardiovascular disability: updating the social security listings," National Academies Press (US) 7, Ischemic Heart Disease, pages 101-132, 2010.
- A. Corselli, "A fully integrated autonomous wearable ultrasonic system on-patch," Tech Briefs, May 2023.
- C. Pascali, L. Francioso, L. Giampetruzzi, G. Rescio, M.A. Signore, A. Leone, P. Sicliano, "Modeling, fabrication and integration of wearable smart sensors in a monitoring platform for diabetic patients," Sensors 21, No. 5, 1847, March 2021.
- A. D'Andrea, et al, "New ultrasound technologies for ischemic heart disease assessment and monitoring in cardiac rehabilitation," J Clin Med, September 2020.
- I. AlMohimeed, Y. Ono, "Ultrasound measurement of skeletal muscle contractile parameters using flexible and wearable sing-element ultrasonic sensor," Sensors 20, 3616, June 2020.
- Y. Guo, et al, "A review of wearable and unobtrusive sensing technologies for chronic disease management," Comput Biol Med, Februrary 2021.
- J.V. Vaghasiya, C.C. Mayorga-Martinez, M. Pumera, "Wearable sensors for telehealth based on emerging materials and nonarchitectonics," npj Flex Electron 7, 26, June 2023.
- P. Ausugstyniak, "Wearable sensor node for cadia ischemia detection" In Proceedings of the 11th Internationall Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) – Volume 4L BIOSIGNALS; ISBN 978-989-758-279-0, ScieTePress, pages 97-104, 2018.
- P. Kakria, N.K. Tripathi, P. Kitipawang, "A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors," International Journal of Telemedicine and Applications Volume 2015, December 2015.
- J. Chen, Y. Shi, S. Shi, "Noise analysis of degitial ultrasonic nondestructive evaluation system," International Journal of Pressure Vessels and Piping, Volume 76, Issue 9, pages 619-630, 1999.
- M. Imitaz, R. Ramos-Garcia, S. Wattal, S. Tiffany, E. Sazonov, "Wearable sensors for monitoring of cigarette somking in free-living: a systematic review," MDPI Volume 19 Issue 21, October 2019.
- A. Bansal, S. Hou, O. Kulyk, E. Bowman, I. Samuel, "Wearable organic optoelectronic sensors for medicine," Advanced Materials Volume 27, Issue 46L Organic Bioelectronic Materials and Devices, December 2015.
- F. Sana, E. Isselbacher, J. Singh, et al, "Wearable devices for abulatory cardiac monitoring," J Am Coll Cardiol, Volume 75, No. 13, pages 1582-1592. April 2020.
- Y. Li, Y. Li, R. Zhang, S. Li, Z. Liu, J. Zhang, Y. Fu, "Progress in wearable acoustical sensors for diagnostic applications," Biosensors and Bioelectronics, Volume 237, 2023.
- T. Arakaw, N. Sakakibara, S. Kondo, "Development of non-invasive steering-type blood pressure sensor for driver state detection," Int. J. Innov. Comput. Inf. Control, 14, pages 1301-1310, 2018.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).