1. Introduction
Atrial fibrillation (AF) stands as the prevailing tachyarrhythmia associated with an increased risk of ischemic stroke and heart failure leading to a mortality rate of 22.3 per 100.000 population aged 35 to 84 years [
1].
The pulmonary veins (PVs) play a pivotal role both in the initiation and persistence of AF. While pulmonary vein isolation (PVI) has been established as an efficacious AF treatment, it is linked to the emergence of PV stenosis, a potentially fatal complication.
Pulmonary vein stenosis defined as a ≥20% narrowing of the pre-ablation pulmonary venous diameter [
2] is a condition often arising as a consequence of radiofrequency ablation (RFA) used to treat atrial fibrillation (AF). At the beginning of the 21
st century, when AF ablation was in its pioneering stage, some degree (mild <50% or moderate 50-70%) of PV stenosis occurred in up to 42% of cases [
3] but severe stenosis (>70%) was infrequent (1.3%) [
4]. Since then, the location of PV isolation moved from the ostium to the antral region and the technique has also evolved with optimization of the radiofrequency energy, emergence of newer methods (e.q. cryoballoon ablation) and usage of 3-dimensional electroanatomical mapping systems based on pre-procedural computed tomography (CT) imaging of the left atrium and PVs thus decreasing the likelihood of PV stenosis. Currently, the prevalence is of less than 0.3% [
5].
Fibrosing mediastinitis on the other hand, is an uncommon life-threatening condition not recognized as a potential complication of RFA for AF but also associated with PV stenosis.
While most patients with PVs stenosis secondary to RFA are asymptomatic, in severe cases, it can lead to a range of symptoms like dyspnea, coughing, and hemoptysis due to the gradual narrowing and occlusion of the veins and the resulting congestion in the lungs with pulmonary hypertension and venous infarction. These symptoms typically manifest gradually over a span of weeks to months following the procedure [
6]. If left untreated, severe forms could prove fatal.
2. Detailed Case Description
We report the case of a 53-year-old male patient with a history of paroxysmal atrial fibrillation diagnosed back in 2021. The patient also suffered from class 1 obesity, type 2 diabetes mellitus treated with oral antihyperglycemic agents and arterial hypertension.
In March 2023, he underwent radiofrequency ablation of the cavotricuspid isthmus (CTI) and pulmonary veins under general anesthesia in another hospital. The discharge letter mentioned a difficult positioning of the decapolar catheter with no other periprocedural accidents or incidents. The procedure was reported as successful with persistent sinus rhythm. No prior fibrosing mediastinitis was indicated in the medical documents provided by the patient.
The patient has consistently taken anticoagulant drugs (apixaban 5 mg twice daily) as prescribed since the procedure together with oral antihyperglycemic agents, antilipidemic and antihypertensive drugs.
The patient reported feeling well after the procedure and an insidious installation of fatigability and dyspnea after 3 months. The symptoms gradually worsened, and he addressed for daycare diagnostic and treatment to our clinic at approximately 6 months after the initial procedure.
Upon admission, the patient was in sinus rhythm with no atrial fibrillation episodes at Holter monitorization. Transthoracic echocardiography showed moderate dilation of right heart cavities, severe pulmonary hypertension, and a turbulent flow in superior pulmonary veins. Pneumological evaluation revealed a mild restrictive dysfunction with a blood oxygen level of 95%. As the patient was under treatment with Eliquis® (apixaban), pulmonary embolism was not suspected. Given his history of radiofrequency ablation for atrial fibrillation, the cardiologist scheduled the patient for a cardiac CT angiography to exclude a post-procedural stenosis of the pulmonary veins.
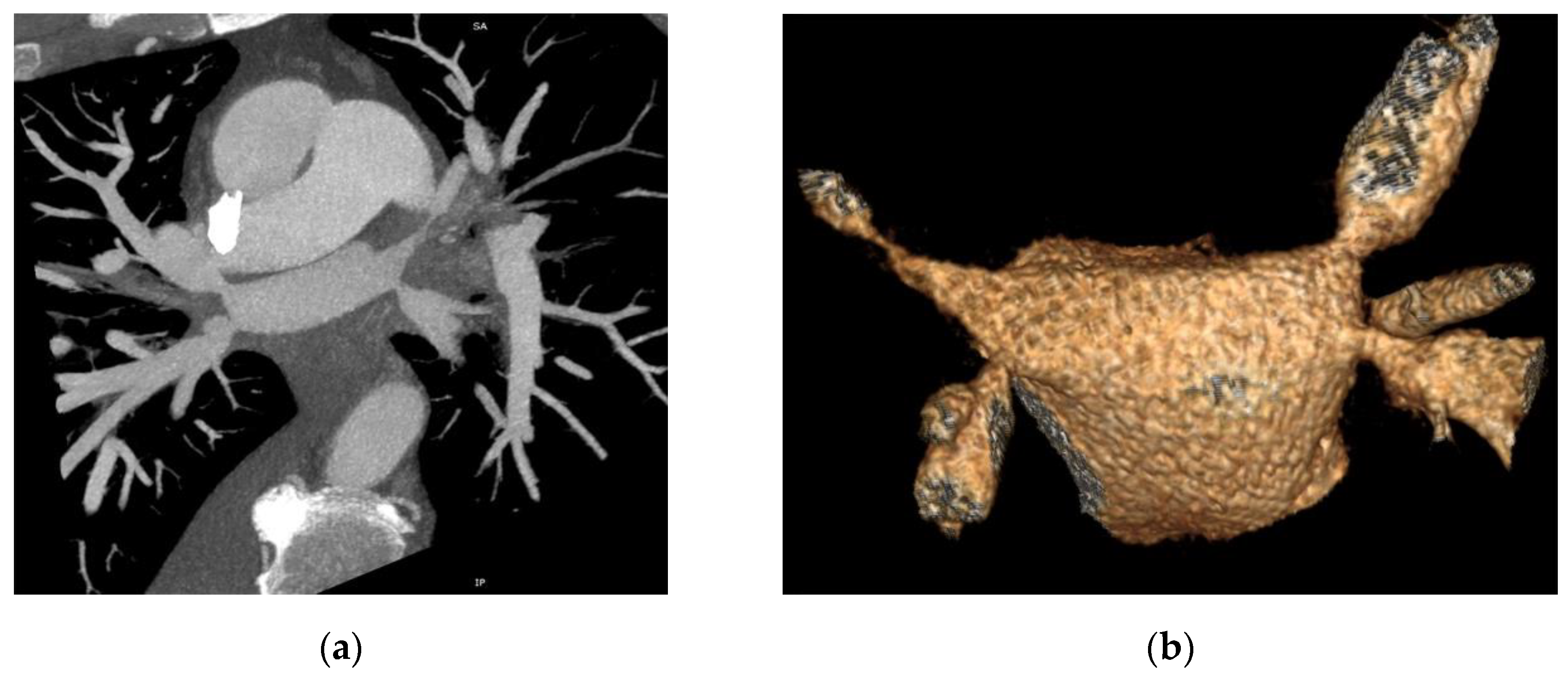
The CT study revealed stenosis of all four pulmonary veins (severe stenosis of the right superior, right inferior and left inferior PVs, near-occlusion of the left superior PV and of the vein draining the apical segment of the right lower lobe) (
Figure 1).
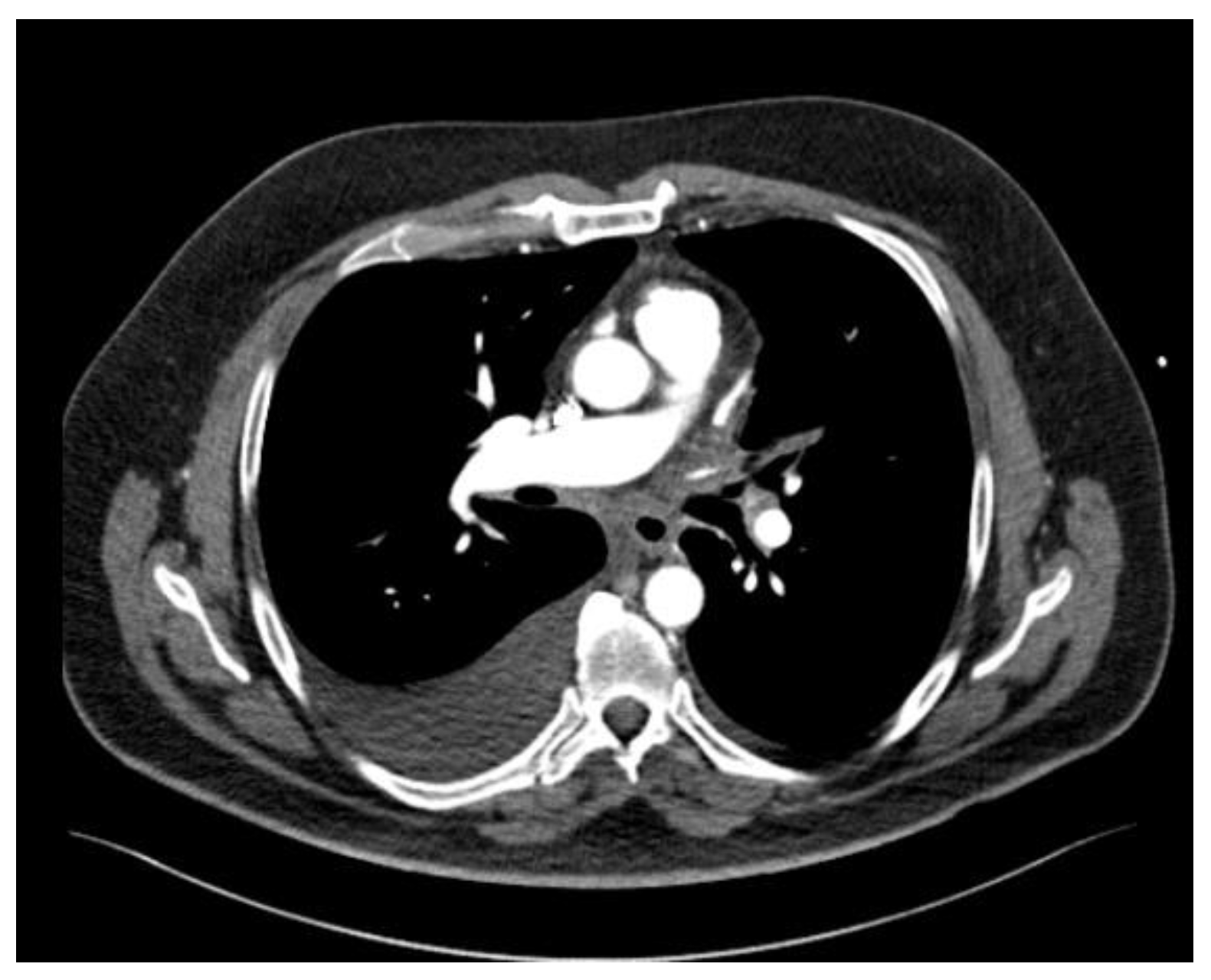
The patient also presented bilateral pleural effusion (40 mm on the right side and 7 mm on the left side) and a soft tissue attenuation obliterating normal mediastinal fat planes and encasing both the PVs and the esophagus posterior to the left atrium, an aspect suggesting fibrosing mediastinitis probably caused by the severe inflammation induced by radiofrequency ablation associated thermal injury (
Figure 2). As for the parenchymal findings, a global mosaic attenuation was present, especially in the right middle lobe, together with a ground-glass opacity in the apical segment of the left lower lobe. The parenchymal findings were mostly consistent with pulmonary venooclusive disease and an area of hemorrhagic infarction.
The case was discussed by the Heart Team including cardiologists, cardiovascular surgeons and interventional cardiologists and the decision to attempt balloon angioplasty and stenting of the PVs was made. Surgical repair was not considered an option because of the severe fibrosing mediastinitis encasing mediastinal structures around the left atrium. Also, the administration of corticosteroid treatment was considered unwarranted due to the pulmonary veins being already completely occluded.
The patient asked to be discharged until the planned procedure and developed fatal hemoptysis 3 days after the presentation during a physical effort. Prehospital cardiopulmonary resuscitation was unsuccessful.
3. Discussion
Atrial fibrillation (AF) is the most common cardiac arrhythmia with an indication for radiofrequency ablation (RFA). While generally considered safe and efficacious when performed by skilled and experienced practitioners, the procedure still carries a significant risk of serious complications, such as the development of PV stenosis, stroke, phrenic nerve palsy, or atrioesophageal fistula [
7]. Among these, PV stenosis is the most frequent, but it’s real incidence is not known as the majority of patients are asymptomatic and routine cardiac CT angiography is not performed during follow-up (not mandated by the Heart Rhythm Society consensus statements) [
7]. A study performed by Teunissen et al. on 1167 patients who benefited from PV radiofrequency isolation between 2005-2016, reported that 36.3% of patients showed a certain degree of PV stenosis. Severe PV stenosis defined as a reduction of >70% in both superoinferior and anteroposterior diameter was noticed in only 0.7% of cases [
8]. The incidence of PV stenosis decreased in the later years because of increased experience and technological progress (cryoballoon ablation, pulsed field ablation, circumferential ablation and antral isolation), Xuan et al. reporting a 2.44% overall incidence in 2020 [
9].
According to El Baba et al. [
10], the pathogenic process of PV stenosis implies a thermal injury induced by the application of energy inside the veins and inappropriate energy delivery leading to intimal proliferation, thrombosis, myocardial necrosis with collagen replacement, endovascular contraction and proliferation of elastic lamina.
Patients with mild (30-50% narrowing) and moderate (50-70% narrowing) PV stenosis are generally asymptomatic, and only a few patients with severe stenosis of one PV develop symptoms (1 in 7 patients according to Teunissen et al.) like cough, dyspnea, chest pain, decreased exercise tolerance, hemoptysis, recurrent lung infections [
8]. The occurrence of symptoms depends on the number of affected PVs, severity of PV stenosis, presence of collateral vessels and clinical setting [
8]. Cardiologists should be aware of this potential complication and exclude it in all patients with a history of radiofrequency ablation presenting with the aforementioned symptoms weeks to months after the initial procedure.
Pulmonary vein stenosis may evolve towards total occlusion, pulmonary hypertension, irreversible parenchymal damage and even prove fatal as in our patient [
11].
The occurrence of both severe PV stenosis and fibrosing mediastinitis following RFA for AF has only been reported once by Makhija et al. in 2009 [
12], RFA not yet being a recognized potential cause of fibrosing mediastinitis [
13]. Fibrosing mediastinitis is generally considered as an atypical immune overactive response within the mediastinum in reaction to specific triggering factors such as infections (histoplasmosis, tuberculosis, aspergillosis, etc.) although most cases are idiopathic.
The presented case is very particular as is the single case reported with a severe stenosis of three PVs, near occlusion of the 4th PV and a collateral branch of the right inferior PV, fibrosing mediastinitis and parenchymal findings consistent with pulmonary venooclusive disease and an area of hemorrhagic infarction diagnosed almost 6 months after RFA of AF. The patient was intensely symptomatic, with pulmonary hypertension and a severely impaired quality of life at presentation, the lesions proving fatal within a 3 days’ time. We plead for the inclusion of fibrosing mediastinitis among the potentially fatal complications of RFA for AF. Further research is mandatory as fibrosing mediastinitis complicates any potential therapeutic management of PV stenosis following RFA.
Treatment of PV stenosis is not stipulated in guidelines, and generally includes balloon angioplasty and stenting with a high restenosis rate of 24% [
14]. Our patient was also scheduled for balloon angioplasty and stenting but succumbed because of fatal hemoptysis. Fender et al. [
9] underline the complexity of PV stenosis treatment and recommend attempting such interventional procedures only in experienced centers. Surgical treatment is generally performed in primary PV stenosis as part of congenital heart disease [
15] and not in iatrogenic induced lesions with severe fibrosis. The most important aspect of the treatment remains prevention by careful technique selection, ablation outside PV ostia and adequate energy application.
4. Conclusions
Severe pulmonary vein stenosis and fibrosing mediastinitis are rare but potentially devastating complications of radiofrequency ablation imposing complex management. Prevention is the key element together with an early diagnosis as these entities could prove life-threatening.
Author Contributions
Conceptualization, V.M.B. and R.O.C.; methodology, F.C.C. and A.C.R.; investigation, V.M.B. and R.O.C.; resources, C.I.S.; writing—original draft preparation, G.D.S.; writing—review and editing, R.O.C. and A.C.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Prof. Dr. George I.M. Georgescu Cardiovascular Diseases Hospital (15/28.09.2023).
Informed Consent Statement
Informed consent was obtained from the patient upon admission.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tanaka, Y.; Shah, N.S.; Passman, R.; Greenland, P.; Lloyd-Jones, D.M.; Khan, S.S. Trends in Cardiovascular Mortality Related to Atrial Fibrillation in the United States, 2011 to 2018. J. Am. Heart Assoc. 2021, 10, e020163. [Google Scholar] [CrossRef] [PubMed]
- De Greef, Y.; Tavernier, R.; Raeymaeckers, S.; Schwagten, B.; Desurgeloose, D.; De Keulenaer, G.; Stockman, D.; De Buyzere, M.; Duytschaever, M. Prevalence, Characteristics, and Predictors of Pulmonary Vein Narrowing After Isolation Using the Pulmonary Vein Ablation Catheter. Circ Arrhythmia Electrophysiol. 2012, 5, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.C.; Hsu, T.L.; Tai, C.T.; Tsai, C.F.; Hsieh, M.H.; Lin, W.S.; Lin, Y.K.; Tsao, H.M.; Ding, Y.A.; Chang, M.S.; Chen, S.A. A. Acquired pulmonary vein stenosis after radiofrequency catheter ablation of paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2001, 12, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Almendral, J.; Barrio-López, M.T. Pulmonary Vein Stenosis After Ablation: The Difference Between Clinical Symptoms and Imaging Findings, and the Importance of Definitions in This Context. Rev. Esp. Cardiol. (Engl. Ed.) 2015, 68, 1056–1058. [Google Scholar] [CrossRef] [PubMed]
- Cappato, R.; Calkins, H.; Chen, S.-A.; Davies, W.; Iesaka, Y.; Kalman, J.; Kim, Y.-H.; Klein, G.; Natale, A.; Packer, D.; Skanes, A.; Ambrogi, F.; Biganzoli, E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. Arrhythmia Electrophysiol. 2010, 3, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Shroff, N.; Choi, W.; Villanueva-Meyer, J.; Palacio, D.M.; Bhargava, P. Pulmonary Vein Occlusion: A Delayed Complication Following Radiofrequency Ablation for Atrial Fibrillation. Radiol. Case Rep. 2021, 16, 3666–3671. [Google Scholar] [CrossRef] [PubMed]
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.-H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation. Heart Rhythm 2017, 14, e275–e444. [Google Scholar] [CrossRef] [PubMed]
- Teunissen, C.; Velthuis, B.K.; Hassink, R.J.; van der Heijden, J.F.; Vonken, E.-J.P.A.; Clappers, N.; Doevendans, P.A.; Loh, P. Incidence of Pulmonary Vein Stenosis After Radiofrequency Catheter Ablation of Atrial Fibrillation. JACC Clin. Electrophysiol. 2017, 3, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Xuan, Z.; Liu, B.; Ci, M.; Wang, Z.; Fan, Y. Hemoptysis Secondary to Pulmonary Vein Stenosis after Radiofrequency Ablation for Atrial Fibrillation: A Case Report and Literature Review. J. Interv. Med. 2020, 3, 98–100. [Google Scholar] [CrossRef] [PubMed]
- El Baba, M.; Sabayon, D.; Refaat, M.M. Radiofrequency Catheter Ablation: How to Manage and Prevent Collateral Damage? J. Innov. Card. Rhythm. Manag. 2020, 11, 4234–4240. [Google Scholar] [CrossRef]
- Yang, H.-M.; Lai, C.K.; Patel, J.; Moore, J.; Chen, P.-S.; Shivkumar, K.; Fishbein, M.C. Irreversible Intrapulmonary Vascular Changes after Pulmonary Vein Stenosis Complicating Catheter Ablation for Atrial Fibrillation. Cardiovasc. Pathol. 2007, 16, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Makhija, Z.; Murgatroyd, F.; Gall, N.; Marrinan, M.T.; Deshpande, R.; Desai, S.R. Fibrosing mediastinitis and occlusion of pulmonary veins after radiofrequency ablation. Ann. Thorac. Surg. 2009, 88, 1674–1676. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Su, H.; Duan, Y.; Jiang, K.; Li, Y.; Deng, M.; Long, X.; Wang, H.; Zhang, M.; Zhang, Y.; Cao, Y. Pulmonary Hypertension Caused by Fibrosing Mediastinitis. JACC. Asia 2022, 2, 218–234. [Google Scholar] [CrossRef]
- Fender, E.A.; Widmer, R.J.; Hodge, D.O.; Cooper, G.M.; Monahan, K.H.; Peterson, L.A.; Holmes, D.R.J.; Packer, D.L. Severe Pulmonary Vein Stenosis Resulting From Ablation for Atrial Fibrillation: Presentation, Management, and Clinical Outcomes. Circulation 2016, 134, 1812–1821. [Google Scholar] [CrossRef] [PubMed]
- Feins, E.N.; Ireland, C.; Gauvreau, K.; Chávez, M.; Callahan, R.; Jenkins, K.J.; Baird, C.W. Pulmonary Vein Stenosis: Anatomic Considerations, Surgical Management, and Outcomes. J. Thorac. Cardiovasc. Surg. 2022, 163, 2198–2207. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).