1. Introduction
The cancellation of surgery has several consequences for employees, employers, patients, the hospital, and people surrounding the local community. An ageing population, urbanization, and the prevalence of anti-health lifestyles worldwide increasingly shape the sustainability of healthcare systems. As a result of significant demographic and disease state changes, healthcare is becoming increasingly complex and costly. Surgery accounts for 40% of hospital expenses and generates about two-thirds of hospital revenues [
1]. It requires about 40% of hospital resource costs, including personnel (surgeons, anesthesiologists, nurses, etc.) and equipment (operating rooms, intensive care beds, etc.) [
2].
Surgery is being performed in a challenging environment, such as high healthcare expenditures [
3], rising healthcare cost ratios [
4], and increasing demand for surgical procedures due to ageing populations and growing patient populations. In addition, technological advances have expanded the scope of surgical interventions [
5]. Against this backdrop, hospital management is under increasing pressure to control the costs of surgical procedures while providing quality health care to surgical patients. An effective cost containment strategy must integrate decision-making at all levels: strategic, tactical, and operational. One of the main issues at the operational level is surgical case scheduling (SCS) [
5]. Continued and disproportionate emphasis on specialized and specific healthcare models undermines the ability of these systems to provide equitable and economically sustainable healthcare.
2. Related works
Over the past two decades, multi-criteria decision-making (MCDM) methods have increased the effectiveness of risk assessment of failure modes [
6]. Risk assessment is applied using appropriate techniques to prevent unexpected failure scenarios. Several publications have already appeared in the literature solving the problem of hospital reorganization, cost reduction or hospital care of patients. [
7] considered current capacity issues in health care and the development of quantitative techniques to facilitate the strategic assessment of high hospital activity levels in a region. Another objective of one of the papers was to conduct a systemic analysis of the resources and performance of public hospitals. A multi-objective optimization (MOO) approach was proposed by [
8]. This approach identifies the theoretical capacity of the entire hospital and facilitates sensitivity analysis, such as patient case mix (PCM). Combining aspects of uncertain scheduling parameters and multi-stakeholder interests and scheduling performance for operating rooms using multi-criteria optimization was described in [
9].
To develop a method, precisely in the era of supporting competition in the market, scientific methods determine the risk and failure of actions [
10]. One of the most well-known risk assessment methods is the FMEA (Failure Mode and Effects Analysis) method [
11]. FMEA is a method known in the healthcare sector since the 1990s to determine the risk of drug production and control errors in hospitals [
12]. Since the application of FMEA in healthcare has been very successful, it has been called failure modes and effects analysis (H-FMEA) [
13]. Recently, several studies had published in which FMEA is used together with fuzzy sets to overcome the weaknesses of the traditional RPN (Risk Priority Number) ranking system [
14]. A general FMEA method based on fuzzy logic has been proposed that simulates the traditional FMEA methodology by reducing the number of rules in the fuzzy RPN modelling process [
15].
Numerous studies [
6,
16,
17] show that the challenges of inappropriate financial allocation, healthcare efficiency, and patient safety make a compelling case for the need for changes in medical systems. New and innovative approaches to care are needed in financing, delivering, and managing health services. At the same time, these approaches should improve the quality of care, ensure financial sustainability and meet the needs and demands of individuals and communities. Patient-centred approaches that engage people and enable self-care are gaining popularity in response to these challenges. Healthcare delivery is a unique process involving real-time decision-making and complex human activity. An integrated care delivery model would effectively coordinate services based on patient and hospital needs.
2.1. Contribution
The study aimed to develop a risk-based approach considering factors contributing to surgery cancellation in classified hip osteoarthritis patients. By accurately identifying the hospital’s risks (e.g., surgery cancellation), one can select an appropriate control solution to eliminate or reduce surgery-related expenses and increase quality, efficiency, and patient safety. The study combines the multi-criteria method and FMEA to introduce a belief structure and describe expert knowledge by integrating the FMEA with FTOPSIS while calculating the criterion weights from the expert questionnaires. FTOPSIS calculate the level of performance, and FMEA calculates the risks of hospital operations in a comprehensive and ranked manner based on potential criteria through their integration. The paper also presents a detailed scheme for combining FMEA and FTOPSIS methods.
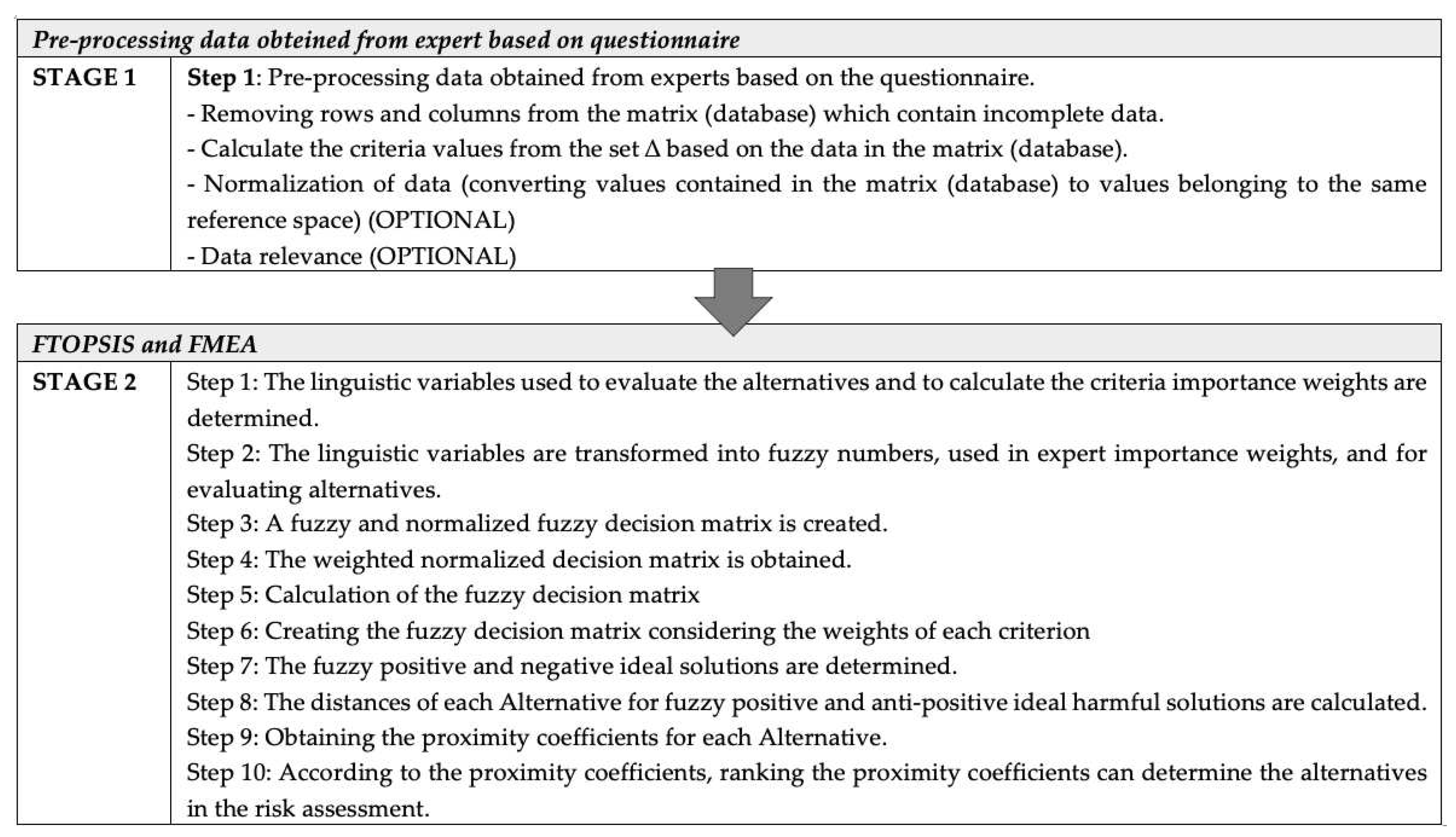
4. Risk assessment based on FTOPSIS and FMEA
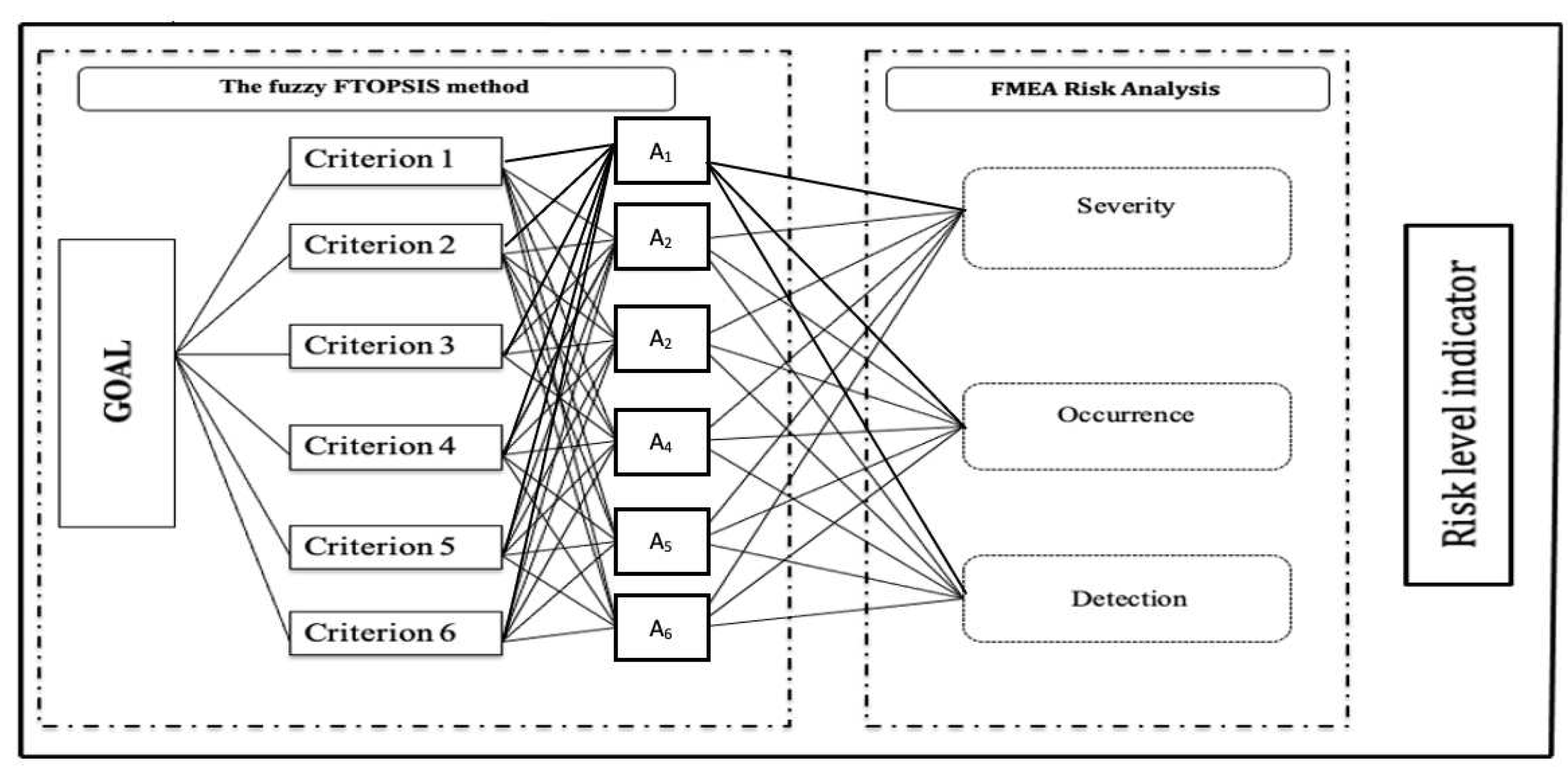
Based on
Figure 1, which shows the risk assessment scheme, the next section of the paper presents solutions for all stages.
Based on Stage 1 in the proposed method risk assessment methodology in determining the abandonment rate is to pre-process the data obtained from the experts based on the questionnaire. This step mainly includes:
Removing rows and columns from a matrix (database) that contain incomplete data.
Calculation the criteria values from the set based on the data in the matrix (database).
Data normalization (replacing the values in the matrix (database) with values belonging to the same reference space).
Pre-process the data from the set
, where the elements of the set
are the expert measures
(where:
denotes the element number in the set
;
d - the number of elements in the set
;
- the i-th element of the set
)
In further considerations, it assumed that matrix is a matrix of dimension where N is the number of rows in the matrix and p is the number of its columns (the number of attributes from the set). Some of the attributes (measures) and opinions of the evaluators (elements of the set ) may be relatively interdependent, relevant, or not for determining the availability of surgical rooms. They may also require calculations (e.g., insufficient medication or tools and materials required). They can also contain the so-called information noise, which results from various errors that may appear in the data derived from the information obtained. Having a matrix , one should use an appropriate method of cleaning, ordering, and validating the data contained in , which will reduce the amount of information noise are called data pre-processing. Regardless of the data pre-treatment, to ensure the credibility of the risk assessment, it is necessary to determine from among the criteria. Those criteria are important for determining the dropout rate. This method is called, in work, the reduction of criteria. Step 1 identifies the language variables used to evaluate alternatives and to calculate the weighting of criteria importance. A formalized multi-criteria information table, will help combine the selected FTOPSIS method with the risk assessment method.
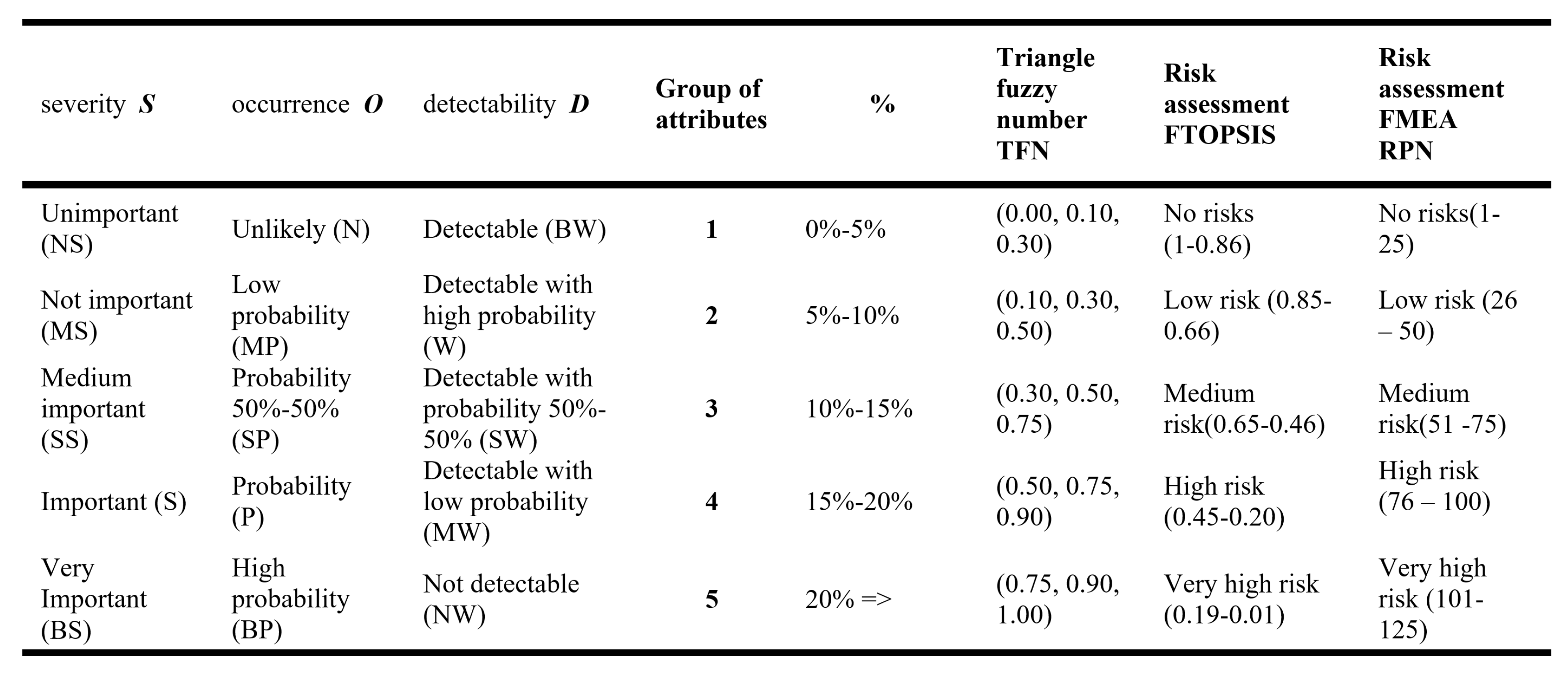
The next stage of the method (
Figure 1) is the risk assessment based on FTOPSIS and FMEA. In traditional FMEA, an indicator called risk priority number (RPN) had used in qualifying failure method by multiplying three parameters, occurrence (O), detectability (D), and severity (S). In FMEA, a value within
had assigned to each parameter O, D, S. After calculating the RPN for the article, the higher the value assigned for a parameter, the more undesirable the effect of that parameter will be on the evaluation.
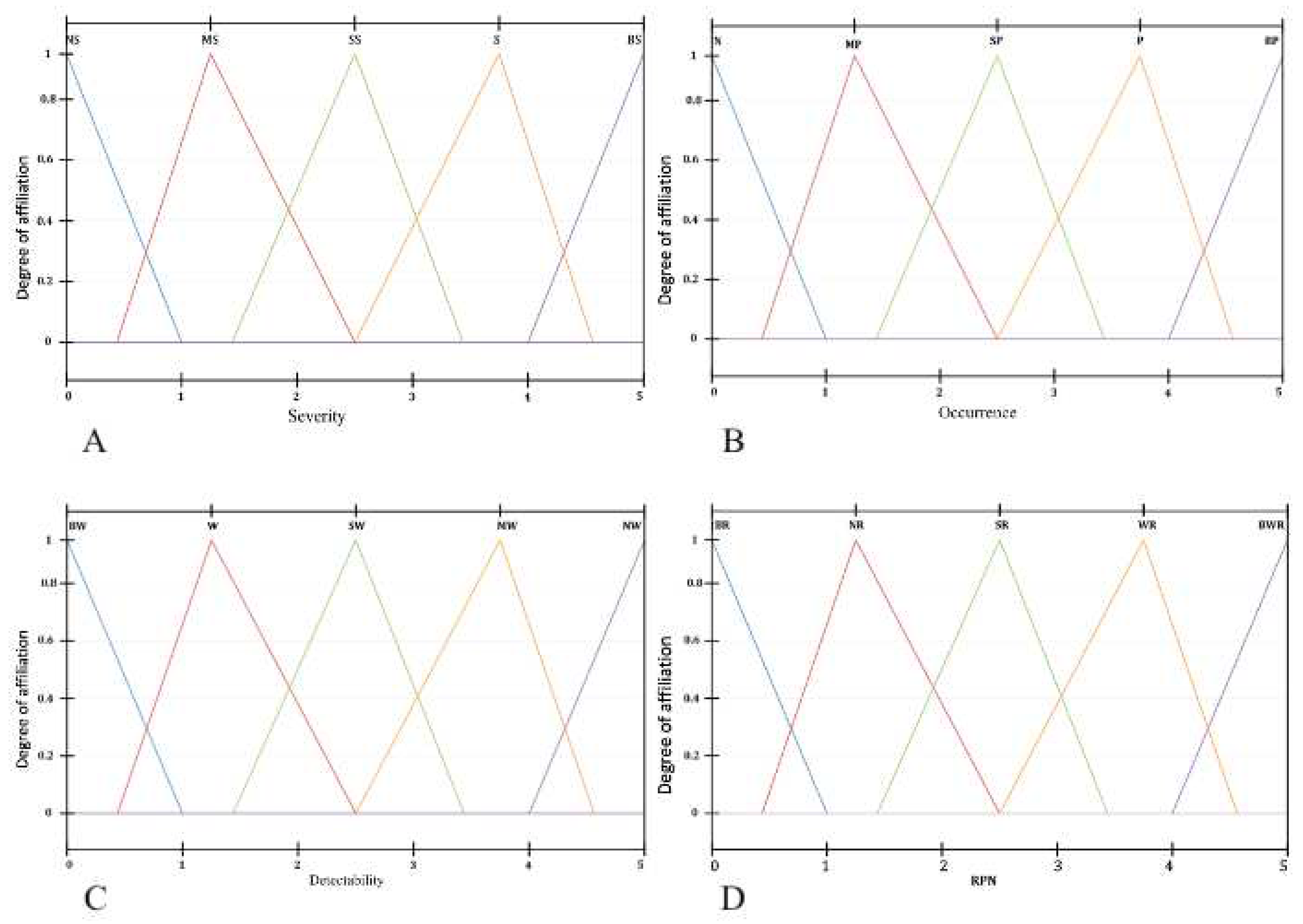
Figure 2 shows the linguistic terms and triangular values for evaluating the alternatives, where the linguistic variables had transformed into fuzzy numbers. Linguistic variables were used in assigning expert importance weights and evaluating alternatives. It contains both fuzzy ratings and degrees of belief. Using linguistic terms allows the decision maker (expert) to assign a more meaningful value to the factors under consideration.
In Step 2 the linguistic variables had transformed into fuzzy numbers, which are used in expert importance weights to evaluate alternatives. Each parameter’s fuzzy function can puts into Triangle Fuzzy Number as a graphical representation of the fuzzy set. To consider the inaccurate data determining the values of alternatives, based on the data contained in the determined information matrix with criteria from the set (Equation (
2)), using the FTOPSIS method, so that its corresponding calculation procedures can have carried out using fuzzy values.
Aggregate the quality values of alternatives
A with weights defined for each criterion after reduction (Step 1)
C from the information matrix
. It had assumed that
denote the alternatives among which the experts will choose the winning solution.
are the criteria against which the performance of each alternative had calculated. The value
is a triangular fuzzy number and denotes the performance of alternatives
against the criterion
. Analytically,
denotes the weight of criterion
and is a normalized triangular fuzzy number.
As well as the fuzzy weight vector W of the form:
Next, Step 3 is computing the fuzzy decision matrix and the normalized fuzzy decision matrix. For each triangular fuzzy value,
the set of
- sections of the form calculate:
Thus, it can transform each fuzzy value into an interval value. Then, the following procedures had used to perform the normalization of the interval values (Step 4):
As a result, the interval
is the normalized equivalent of the interval
. It is then possible to transform the normalized interval back to a triangular fuzzy number of the form
in such a way that the value of
at
will be:
Similarly, establishing the coefficient
, we obtain the remaining values of a triangular fuzzy number:
then
The value is the normalized equivalent of the triangular fuzzy number .
Next, Step 5 creates a fuzzy decision matrix considering the weights of each criterion. Step 6 creates a normalized fuzzy decision matrix considering the weights of each criterion:
These normalized yield values, each of which is in the interval .
Step 7 determines of the ideal with fuzzy nature, both positive and negative. Determining the ideal solution and the inverse of the ideal solution (anti-ideal solution):
Step 8 distances of each alternative for fuzzy positive and anti-positive ideal negative solutions are calculated.
Calculating the distance of each alternative under consideration from the ideal solution and the inverse of the ideal solution (called anti-ideal solution). Calculating the distance of each considered alternative from the ideal solution and the inverse of the ideal solution between two fuzzy numbers of form
and
can have calculated as follows:
The distance of the alternatives from the ideal solution can have calculated as follows:
Similarly, the distance from the inverse of the ideal solution (anti-ideal solution) is calculated:
Step 9 obtains proximity coefficients for each alternative.
Calculating the relative proximity of each alternative to the ideal solution. The relative closeness of alternative
to the ideal solution
defined as:
In Step 10, depending on the result of the proximity coefficients, ranking these coefficients can determine the alternatives in the risk assessment. The result is to rank the alternatives in order from the largest to the smallest relative closeness value to the ideal solution .
Figure 3 shows the graphical solution of the combination of the two methods, TOPSIS and FMEA. Conclusions of the analysis:
The proposed risk assessment approach incorporates fuzzy judgments and belief degrees (expert preferences).
The flexibility of assigning weight to each factor in the proposed approach is consistent with the actual decision situation.
The input factors (S, O, D) are combined according to their weights, enabling a more comprehensive application approach.
5. Results
Surgical scheduling involves allocating hospital resources to individual cases and deciding when to perform surgeries. This task is critical in efficiently using hospital resources while providing quality patient care. The following are the study results in the treatment process based on actual data. Research in the [Name of Institute] usually consists of three stages: patient classification, reference to treatment (therapeutic care), and elective surgery.
Patients entering the orthopedics department are first classified according to their level of urgency, using appropriate indicators.
If the patient is qualified for elective surgery, he/she is given a date for hip replacement surgery (endoprosthesis).
A patient referred to the surgery department undergoes a medical consultation by: nurses, residents, doctors performing the surgery, orthopedic doctors, and anesthesiologists.
After a screening - essential examination. The patient has surgery the next day.
To confirm the validity of the risk assessment model, three experts (a nurse, an anesthesiologist, and a physician, the so-called "operator" - who performs surgery) participated in the research. The assessment was made the day before the elective surgery [
20]. The study looked at indicators affecting the cancellation of hip replacement surgery (6 variants of the cancellation process). Finally, compare the obtained grades with those of experts in the [Name of Institute].
General hospital characteristics:
3 operating rooms
Inpatient surgery room,
Operating room for patients with infections,
Operating room for trauma patients,
1 post-operative room,
42 patient bed.
Additional factors:
Hip replacement surgery is performed on Mondays, Wednesdays, or Fridays (optional).
There are 3 or 4 scheduled surgeries per day.
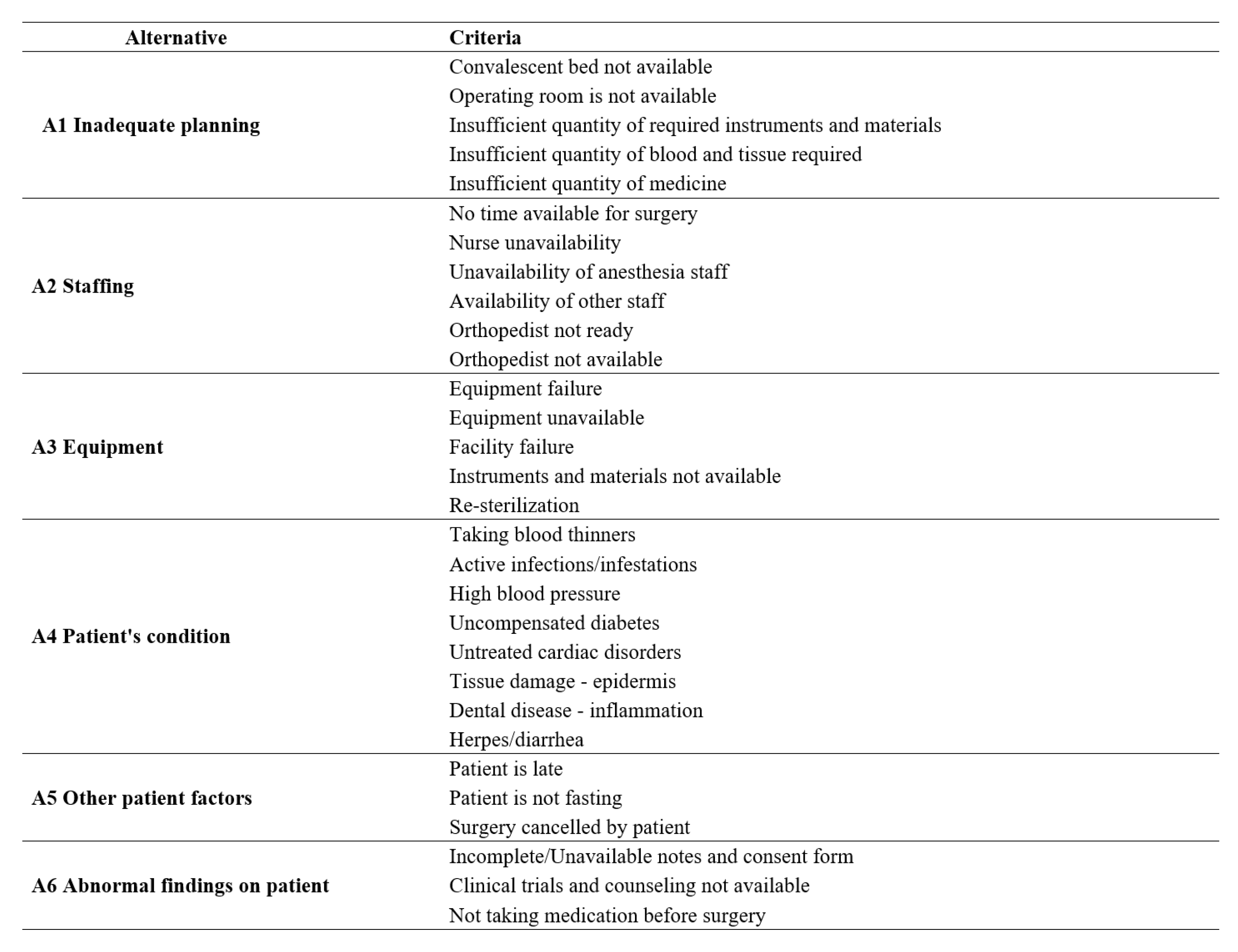
The questionnaire, evaluated by experts, obtained six alternatives based on 30 criteria.
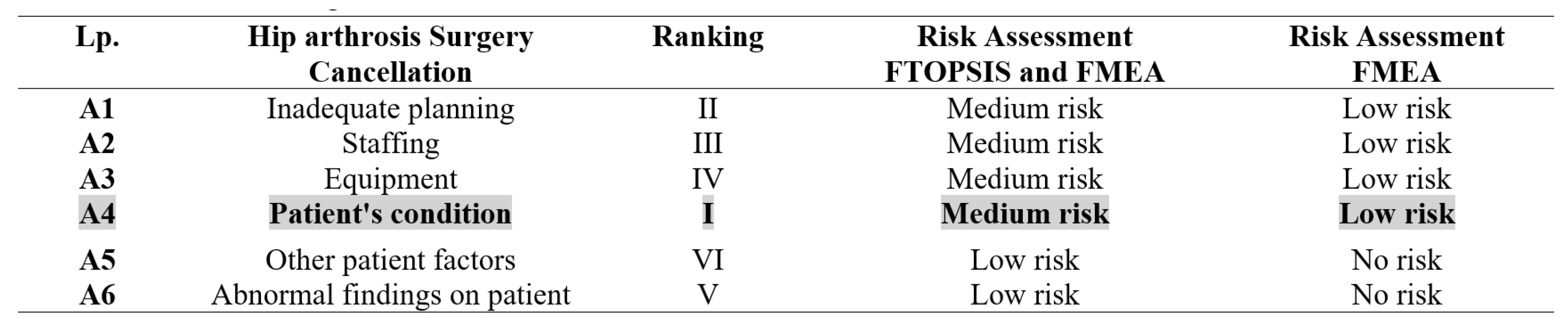
Figure 4 shows the obtained alternatives from the decision matrix for risk assessment based on the questionnaire.
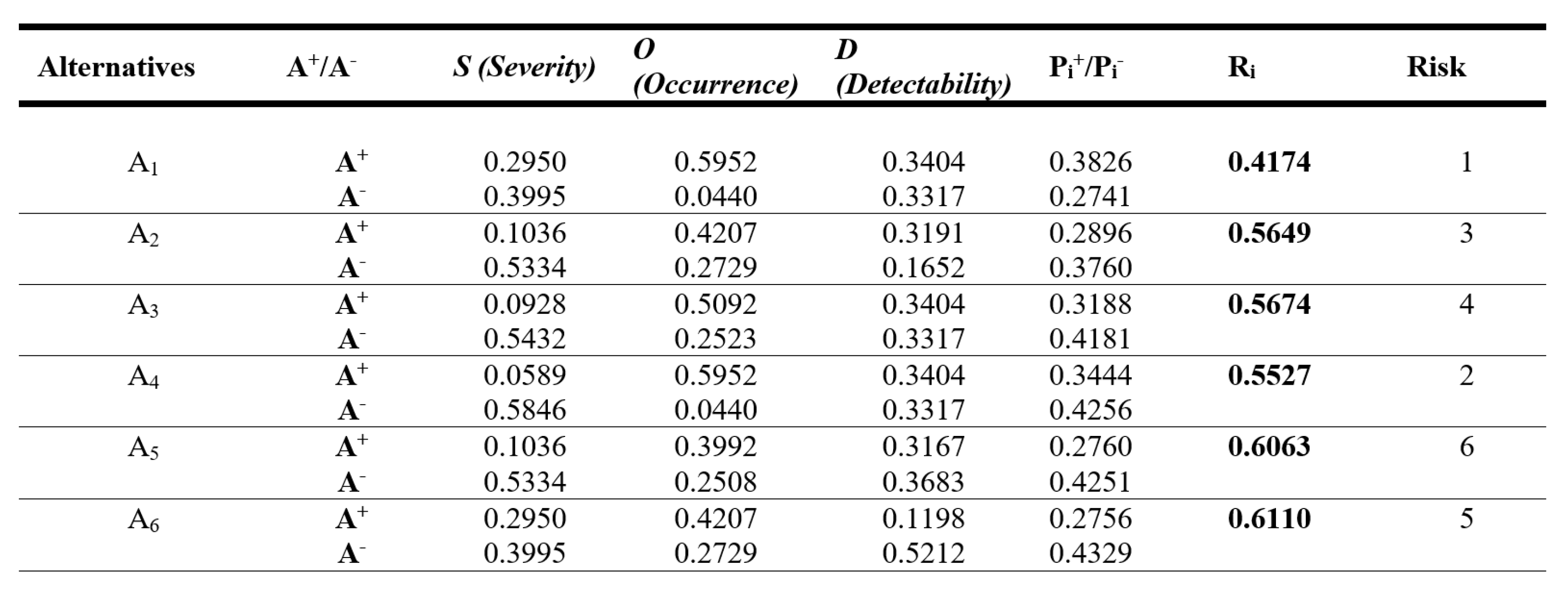
The following research presents the results from the steps based on the previous methodology. To fit the data from the questionnaires into the information matrix, determined the following factors to give us the evaluation attributes with the determination of alternatives from the decision matrix for risk assessment. These are: A1-Inadequate planning; A2 – Staffing; A3 - Equipment; A4 - Patient’s condition; A5 - Other patient factors; A6 - Abnormal findings on a patient. After obtaining the results from Stage 1 and Stage 2 obtained the belief distance measurement along (
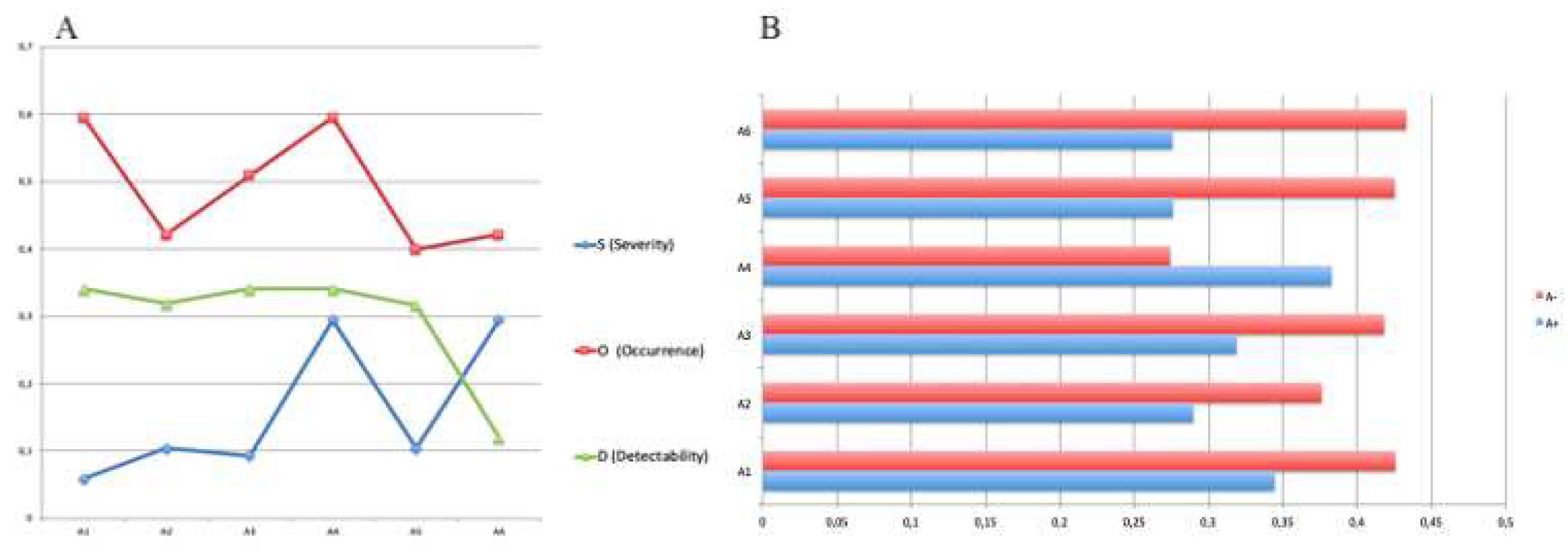
Figure 5) with a graphical representation of the fuzzy function of each parameter (
Figure 6).
The results from the presented method from the measurement of belief distance are presented below, along with a graphical representation of the fuzzy function of each parameter.
Based on the proposed method, the results show that the expert’s opinion compared with the results of FMEA and FTOPSIS showed the potential of the framework in the correct prioritization of abandonment rates. Figure 8 shows the ideal solution for the designated alternatives in the risk assessment.
Figure 7 shows the distance of each alternative to the ideal solution in the risk assessment
Figure 7.
Designated alternatives from the decision matrix for risk assessment.
Figure 7.
Designated alternatives from the decision matrix for risk assessment.
From among the six factors, tree of them: patient condition, inadequate scheduling, and personnel were identified as having the most significant impact on the surgical cancellation of elective surgery, as shown in
Figure 7 and
Figure 9.
Figure 8.
A: The ideal solution for the alternatives in the risk assessment; B:Distance of each of the considered alternatives to the ideal solution in the risk assessment.
Figure 8.
A: The ideal solution for the alternatives in the risk assessment; B:Distance of each of the considered alternatives to the ideal solution in the risk assessment.
Figure 9.
Relative proximity for each Alternative in the risk assessment.
Figure 9.
Relative proximity for each Alternative in the risk assessment.
The results show that the patient’s condition is the main risk of canceling surgery. Of course, it can reduce the financial risk by examining the patient before admission to the ward, but only if schedule surgery. The patient can then perform the necessary tests with health funds. During urgent operations, the risk increases, as do the hospital’s finances. What is needed is a strategy that will ultimately reduce the additional cost to the hospital. The research presented in the case study combined two methods and showed the problem in Polish hospitals. The decision to operate on patients is a daily one. The method demonstrated the validity of the procedure carried out and its importance for the future of the hospital.