Submitted:
20 November 2023
Posted:
21 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
- Schroth, Germany
- Lyon, France
- SEAS (Scientific Exercise Approach to Scoliosis), Italy
- BSPTS (Barcelona Scoliosis Physical Therapy School), Spain
- Side Shift, UK
- DoboMed, Poland
- FITS (Functional Individual Therapy of Scoliosis), Poland
2. Materials and Methods
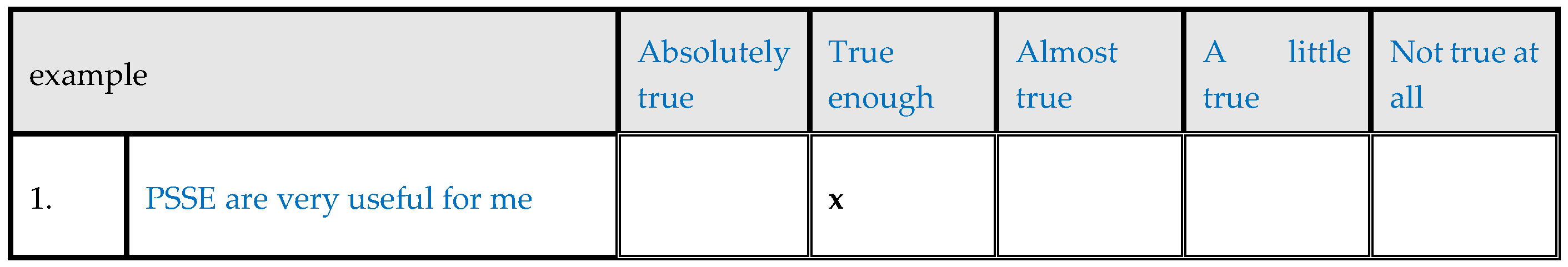
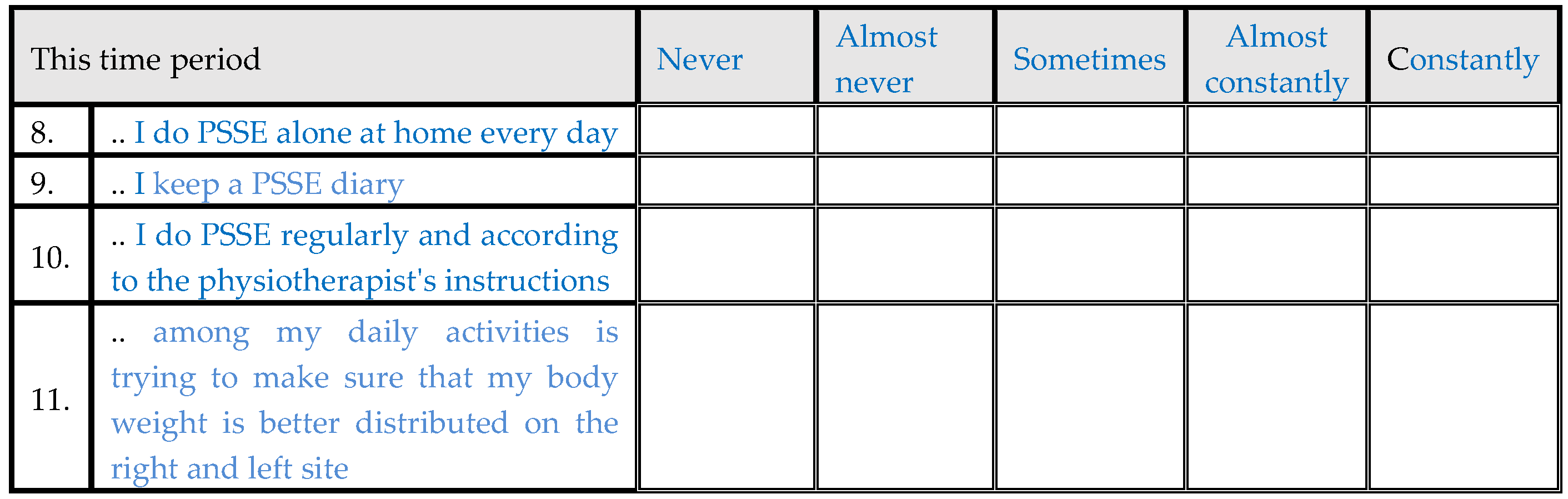
2.1. The questionnaire
2.2. Study Population
2.3. Psychometric evaluation
2.4. Materials
2.4.1. Scoliometer measurement (ATR)
2.4.2. Formetric 4D-DIERS
2.4.3. BMI
2.4.4. Cobb angle
2.4.5. Risser sign
2.4.6. Demographics
3. Results
3.1. Descriptive statistics
| Mean | Standard Deviation | ||
| Age(yrs) | 16.5 | 7.1 | |
| BMI (Kg/m2) | 19.89 | 2.75 | |
| Cobb Angle (degrees) | 36.1 | 4.08 | |
| Risser sign | 4.6 | 1.6 | |
| Age at menarche | 12.1 | 1.1 | |
| Count | Column N % | ||
| Menarche | No | 12 | 18.2% |
| Yes | 54 | 81.8% | |
| Sex | Male | 11 | 13.8% |
| Female | 69 | 86.3% | |
| Brace | No | 19 | 25.0% |
| Yes | 57 | 75.0% | |
| Dominant hand | Right | 67 | 88.2% |
| Left | 9 | 11.8% | |
| In general how would you describe the state of your physical health? | Not good at all | 1 | 1.3% |
| Somewhatgood | 1 | 1.3% | |
| Moderately good | 20 | 25.0% | |
| Quite good | 41 | 51.3% | |
| Very good | 17 | 21.3% | |
| In general how would you rate your appearance? | Not good at all | 0 | 0.0% |
| Somewhatgood | 2 | 2.5% | |
| Moderately good | 17 | 21.3% | |
| Quite good | 39 | 48.8% | |
| Very good | 22 | 27.5% | |
| In general how would you describe your experience with PSSE? | Not good at all | 0 | 0.0% |
| Somewhatgood | 1 | 1.3% | |
| Moderately good | 11 | 13.8% | |
| Quite good | 42 | 52.5% | |
| Very good | 26 | 32.5% | |
| In general how would you describe your mental health? | Not good at all | 0 | 0.0% |
| Somewhatgood | 3 | 3.8% | |
| Moderately good | 11 | 13.8% | |
| Quite good | 40 | 50.0% | |
| Very good | 26 | 32.5% | |
| In general how would you rate your posture during the day? | Not good at all | 2 | 2.5% |
| Somewhatgood | 5 | 6.3% | |
| Moderately good | 29 | 36.3% | |
| Quite good | 36 | 45.0% | |
| Very good | 8 | 10.0% | |
| In general how would you rate your endurance? | Not good at all | 3 | 3.8% |
| Somewhatgood | 6 | 7.5% | |
| Moderately good | 13 | 16.3% | |
| Quite good | 26 | 32.5% | |
| Very good | 32 | 40.0% | |
| In general how would you describe your relationship with the people close to you? | Not good at all | 0 | 0.0% |
| Somewhatgood | 0 | 0.0% | |
| Moderately good | 5 | 6.3% | |
| Quite good | 17 | 21.3% | |
| Very good | 58 | 72.5% | |
| This time period I do PSSE alone at home every day | Never | 1 | 1.3% |
| Almost never | 5 | 6.3% | |
| Sometimes | 28 | 35.0% | |
| Almost constantly | 32 | 40.0% | |
| Constantly | 14 | 17.5% | |
| This time period I keep a PSSE diary | Never | 51 | 63.8% |
| Almost never | 10 | 12.5% | |
| Sometimes | 7 | 8.8% | |
| Almost constantly | 5 | 6.3% | |
| Constantly | 7 | 8.8% | |
| This time period I do PSSE regularly and according to the physiotherapist's instructions | Never | 3 | 3.8% |
| Almost never | 1 | 1.3% | |
| Sometimes | 22 | 27.5% | |
| Almost constantly | 26 | 32.5% | |
| Constantly | 28 | 35.0% | |
| This time period among my daily activities is trying to make sure that my body weight is better distributed on the right and left site | Never | 2 | 2.5% |
| Almost never | 6 | 7.5% | |
| Sometimes | 29 | 36.3% | |
| Almost constantly | 39 | 48.8% | |
| Constantly | 4 | 5.0% | |
| I will do PSSE at home even if I’m tired | Not true at all | 6 | 7.5% |
| Somewhat true | 16 | 20.0% | |
| Almost true | 17 | 21.3% | |
| True enough | 31 | 38.8% | |
| Absolutely true | 10 | 12.5% | |
| I will do PSSE at home even if I’m in a bad mood | Not true at all | 10 | 12.5% |
| Somewhat true | 14 | 17.5% | |
| Almost true | 19 | 23.8% | |
| True enough | 22 | 27.5% | |
| Absolutely true | 15 | 18.8% | |
| I will do PSSE at home even if I don’t have time | Not true at all | 12 | 15.0% |
| Somewhat true | 26 | 32.5% | |
| Almost true | 23 | 28.8% | |
| True enough | 14 | 17.5% | |
| Absolutely true | 5 | 6.3% | |
| I will do PSSE at home even if I’m on vacation | Not true at all | 27 | 33.8% |
| Somewhat true | 19 | 23.8% | |
| Almost true | 16 | 20.0% | |
| True enough | 11 | 13.8% | |
| Absolutely true | 7 | 8.8% | |
| I will do PSSE at home even if the physiotherapist is not with me | Not true at all | 6 | 7.5% |
| Somewhat true | 8 | 10.0% | |
| Almost true | 15 | 18.8% | |
| True enough | 18 | 22.5% | |
| Absolutely true | 33 | 41.3% | |
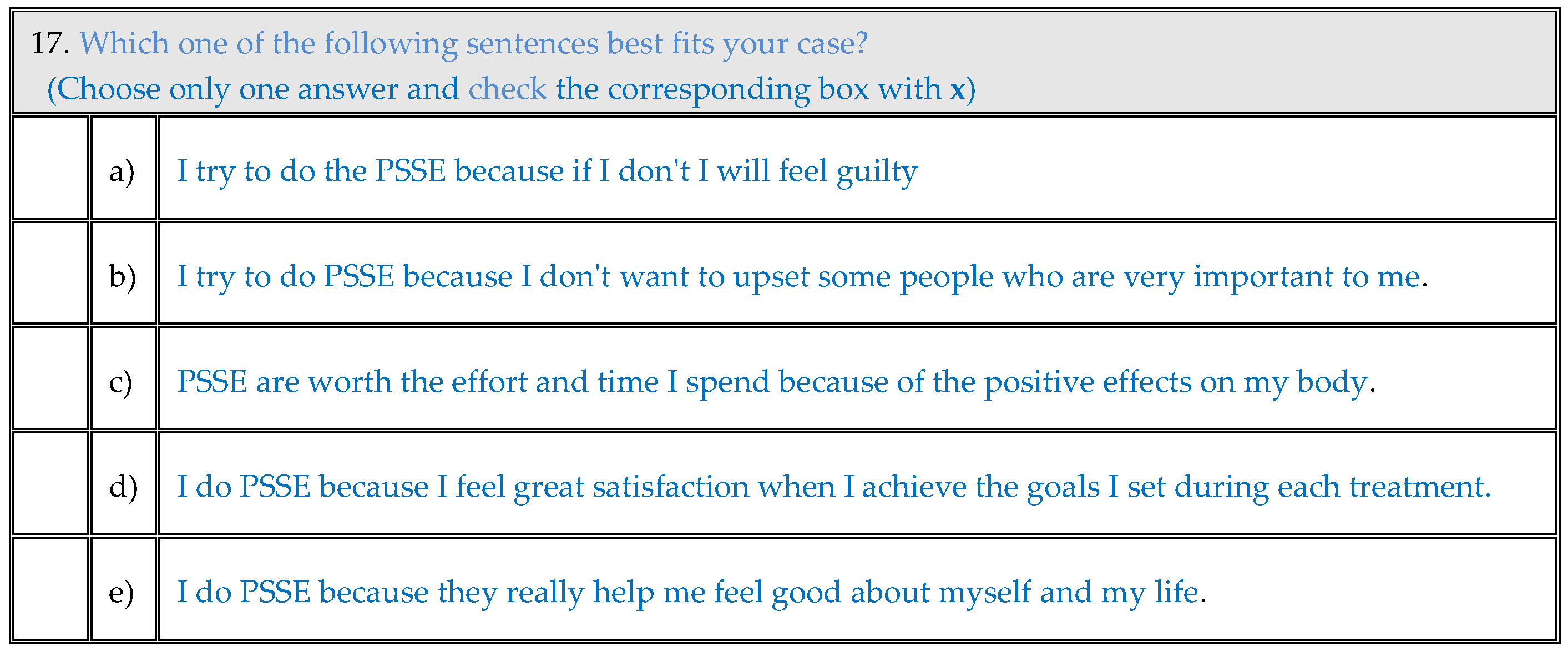
| Motivation | I try to do the PSSE because if I don't I will feel guilty | 4 | 5.0% |
| I try to do PSSE because I don't want to upset some people who are very important to me. | 16 | 20.0% | |
| PSSE are worth the effort and time I spend because of the positive effects on my body. | 37 | 46.3% | |
| I do PSSE because I feel great satisfaction when I achieve the goals I set during each treatment. | 14 | 17.5% | |
| I do PSSE because they really help me feel good about myself and my life. | 9 | 11.3% | |
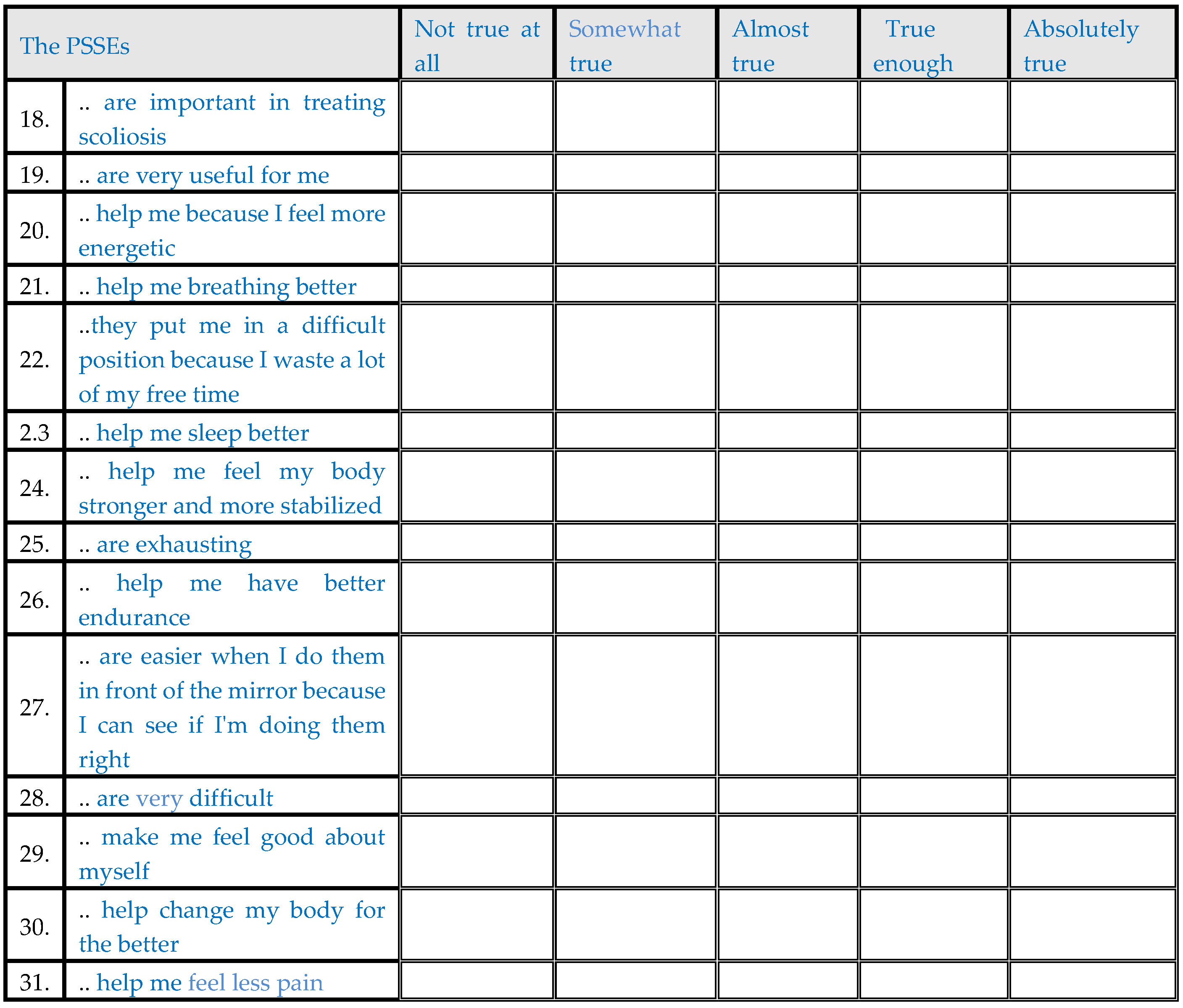
| The PSSEs are important in treating scoliosis | Not true at all | 0 | 0.0% |
| Somewhat true | 0 | 0.0% | |
| Almost true | 6 | 7.5% | |
| True enough | 29 | 36.3% | |
| Absolutely true | 45 | 56.3% | |
| The PSSEs are very useful for me | Not true at all | 0 | 0.0% |
| Somewhat true | 0 | 0.0% | |
| Almost true | 13 | 16.3% | |
| True enough | 33 | 41.3% | |
| Absolutely true | 34 | 42.5% | |
| The PSSEs help me because I feel more energetic | Not true at all | 10 | 12.5% |
| Somewhat true | 10 | 12.5% | |
| Almost true | 26 | 32.5% | |
| True enough | 21 | 26.3% | |
| Absolutely true | 13 | 16.3% | |
| The PSSEs help me breathing better | Not true at all | 10 | 12.5% |
| Somewhat true | 12 | 15.0% | |
| Almost true | 24 | 30.0% | |
| True enough | 23 | 28.8% | |
| Absolutely true | 11 | 13.8% | |
| The PSSEs put me in a difficult position because I waste a lot of my free time | Absolutely true | 12 | 15.0% |
| True enough | 27 | 33.8% | |
| Almost true | 12 | 15.0% | |
| Somewhat true | 16 | 20.0% | |
| Not true at all | 13 | 16.3% | |
| The PSSEs help me sleep better | Not true at all | 18 | 22.5% |
| Somewhat true | 23 | 28.8% | |
| Almost true | 29 | 36.3% | |
| True enough | 7 | 8.8% | |
| Absolutely true | 3 | 3.8% | |
| The PSSEs help me feel my body stronger and more stabilized | Not true at all | 5 | 6.3% |
| Somewhat true | 4 | 5.0% | |
| Almost true | 17 | 21.3% | |
| True enough | 36 | 45.0% | |
| Absolutely true | 18 | 22.5% | |
| The PSSEs are exhausting | Absolutely true | 10 | 12.5% |
| True enough | 9 | 11.3% | |
| Almost true | 21 | 26.3% | |
| Somewhat true | 25 | 31.3% | |
| Not true at all | 15 | 18.8% | |
| The PSSEs help me have better endurance | Not true at all | 5 | 6.3% |
| Somewhat true | 11 | 13.8% | |
| Almost true | 30 | 37.5% | |
| True enough | 26 | 32.5% | |
| Absolutely true | 8 | 10.0% | |
| The PSSEs are easier when I do them in front of the mirror because I can see if I'm doing them right | Not true at all | 0 | 0.0% |
| Somewhat true | 1 | 1.3% | |
| Almost true | 9 | 11.3% | |
| True enough | 29 | 36.3% | |
| Absolutely true | 41 | 51.3% | |
| The PSSEs are very difficult | Absolutely true | 10 | 12.5% |
| True enough | 9 | 11.3% | |
| Almost true | 28 | 35.0% | |
| Somewhat true | 16 | 20.0% | |
| Not true at all | 17 | 21.3% | |
| The PSSEs make me feel good about myself | Not true at all | 3 | 3.8% |
| Somewhat true | 6 | 7.5% | |
| Almost true | 22 | 27.5% | |
| True enough | 35 | 43.8% | |
| Absolutely true | 14 | 17.5% | |
| The PSSEs help change my body for the better | Not true at all | 0 | 0.0% |
| Somewhat true | 2 | 2.5% | |
| Almost true | 7 | 8.8% | |
| True enough | 29 | 36.3% | |
| Absolutely true | 42 | 52.5% | |
| The PSSEs help me feel less pain | Not true at all | 13 | 16.3% |
| Somewhat true | 19 | 23.8% | |
| Almost true | 15 | 18.8% | |
| True enough | 13 | 16.3% | |
| Absolutely true | 20 | 25.0% | |
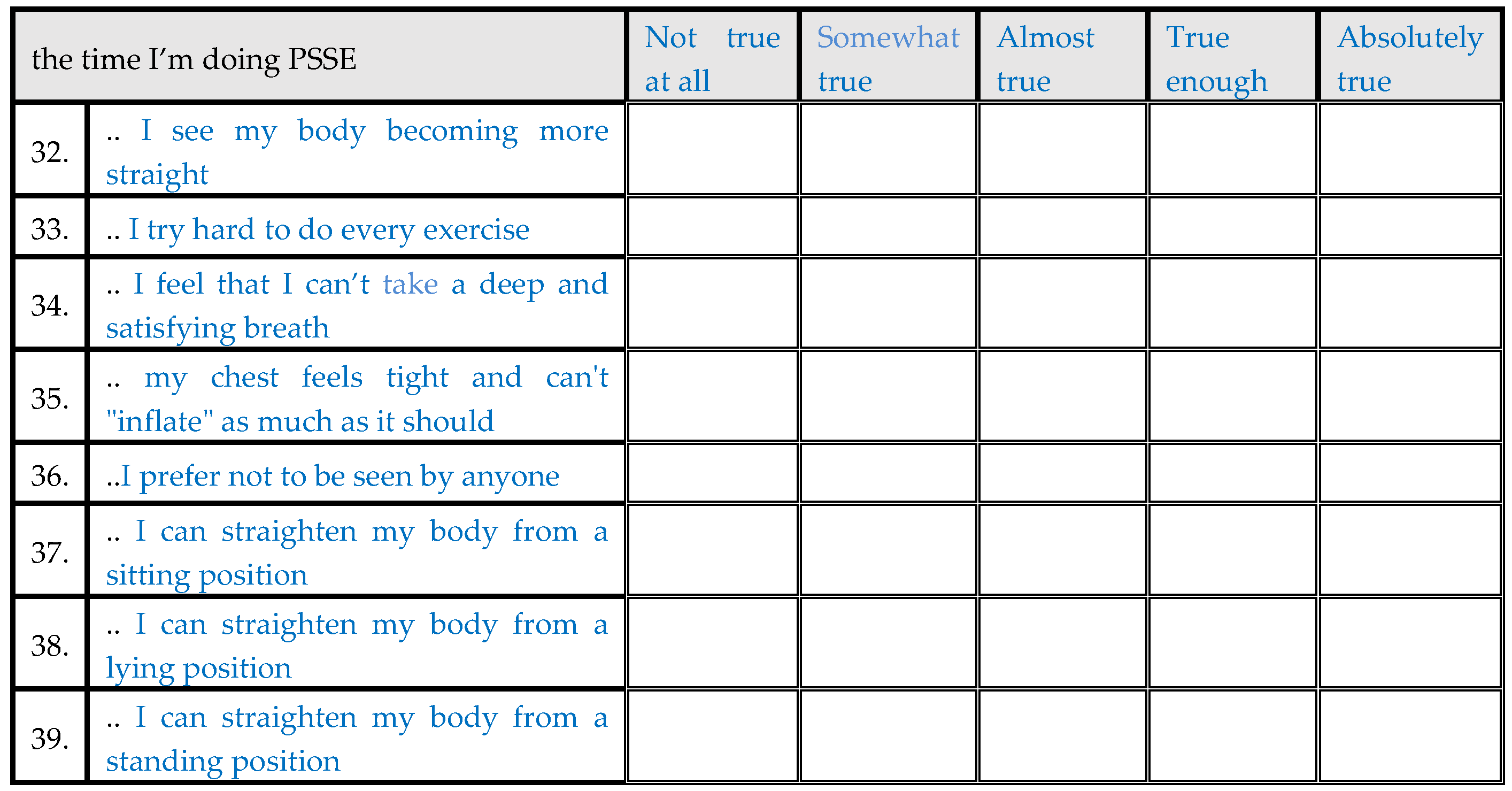
| The time I’m doing PSSEs I see my body becoming more straight | Not true at all | 0 | 0.0% |
| Somewhat true | 0 | 0.0% | |
| Almost true | 12 | 15.0% | |
| True enough | 37 | 46.3% | |
| Absolutely true | 31 | 38.8% | |
| The time I’m doing PSSEs I try hard to do every exercise | Not true at all | 2 | 2.5% |
| Somewhat true | 6 | 7.5% | |
| Almost true | 16 | 20.0% | |
| True enough | 31 | 38.8% | |
| Absolutely true | 25 | 31.3% | |
| The time I’m doing PSSEs I feel that I can’t take a deep and satisfying breath | Absolutely true | 19 | 23.8% |
| True enough | 22 | 27.5% | |
| Almost true | 11 | 13.8% | |
| Somewhat true | 11 | 13.8% | |
| Not true at all | 17 | 21.3% | |
| The time I’m doing PSSE my chest feels tight and can't "inflate" as much as it should | Absolutely true | 25 | 31.3% |
| True enough | 14 | 17.5% | |
| Almost true | 12 | 15.0% | |
| Somewhat true | 13 | 16.3% | |
| Not true at all | 16 | 20.0% | |
| The time I’m doing PSSE I prefer not to be seen by anyone | Absolutely true | 24 | 30.0% |
| True enough | 16 | 20.0% | |
| Almost true | 9 | 11.3% | |
| Somewhat true | 16 | 20.0% | |
| Not true at all | 15 | 18.8% | |
| The time I’m doing PSSE I can straighten my body from a sitting position | Not true at all | 0 | 0.0% |
| Somewhat true | 6 | 7.5% | |
| Almost true | 10 | 12.5% | |
| True enough | 26 | 32.5% | |
| Absolutely true | 38 | 47.5% | |
| The time I’m doing PSSE I can straighten my body from a lying position | Not true at all | 5 | 6.3% |
| Somewhat true | 8 | 10.0% | |
| Almost true | 9 | 11.3% | |
| True enough | 34 | 42.5% | |
| Absolutely true | 24 | 30.0% | |
| The time I’m doing PSSE I can straighten my body from a standing position | Not true at all | 2 | 2.5% |
| Somewhat true | 10 | 12.5% | |
| Almost true | 16 | 20.0% | |
| True enough | 22 | 27.5% | |
| Absolutely true | 30 | 37.5% | |
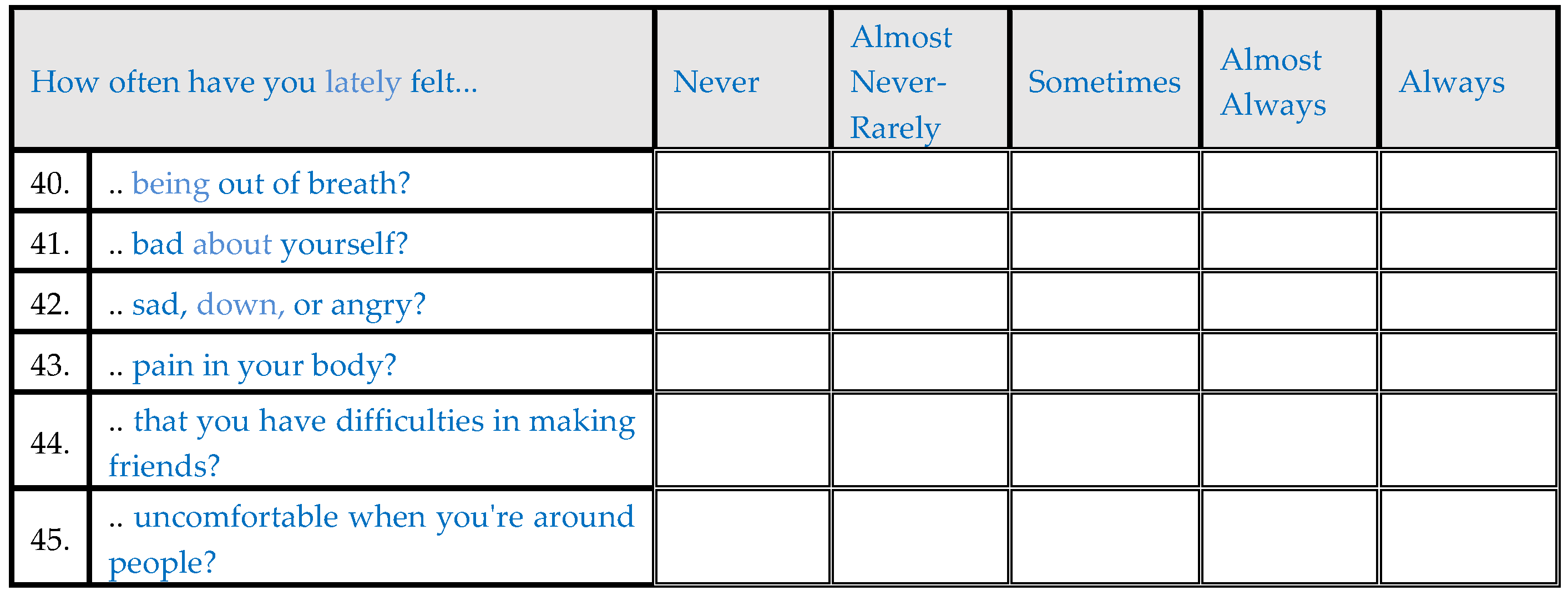
| How often have you felt being out of breath lately ? | Always | 26 | 32.5% |
| Almost always | 22 | 27.5% | |
| Sometimes | 12 | 15.0% | |
| Almost never | 6 | 7.5% | |
| Never | 14 | 17.5% | |
| How often have you lately felt bad about yourself? | Always | 15 | 18.8% |
| Almost always | 22 | 27.5% | |
| Sometimes | 26 | 32.5% | |
| Almost never | 4 | 5.0% | |
| Never | 13 | 16.3% | |
| How often have you lately felt sad, down, or angry? | Always | 5 | 6.3% |
| Almost always | 21 | 26.3% | |
| Sometimes | 41 | 51.3% | |
| Almost never | 7 | 8.8% | |
| Never | 6 | 7.5% | |
| How often have you lately felt pain in your body? | Always | 15 | 18.8% |
| Almost always | 20 | 25.0% | |
| Sometimes | 22 | 27.5% | |
| Almost never | 14 | 17.5% | |
| Never | 9 | 11.3% | |
| How often have you lately felt that you have difficulties in making friends? | Always | 25 | 31.3% |
| Almost always | 19 | 23.8% | |
| Sometimes | 12 | 15.0% | |
| Almost never | 5 | 6.3% | |
| Never | 19 | 23.8% | |
| How often have you lately felt uncomfortable when you're around people? | Always | 15 | 18.8% |
| Almost always | 28 | 35.0% | |
| Sometimes | 13 | 16.3% | |
| Almost never | 13 | 16.3% | |
| Never | 11 | 13.8% | |
| It is true for me that I find it hard to open up to someone, especially as long as I've been dealing with PSSEs | Strongly agree | 25 | 31.3% |
| Agree | 21 | 26.3% | |
| Neutral | 12 | 15.0% | |
| Disagree | 5 | 6.3% | |
| Strongly disagree | 17 | 21.3% | |
| It is true for me that I am not ashamed to do the PSSEs in front of people I consider close to me | Strongly disagree | 3 | 3.8% |
| Disagree | 8 | 10.0% | |
| Neutral | 9 | 11.3% | |
| Agree | 16 | 20.0% | |
| Strongly agree | 44 | 55.0% | |
| It is true for me that my physical therapist is very friendly and supportive | Strongly disagree | 0 | 0.0% |
| Disagree | 1 | 1.3% | |
| Neutral | 2 | 2.5% | |
| Agree | 17 | 21.3% | |
| Strongly agree | 60 | 75.0% | |
| It is true for me that my body’s curve is too obvious to others | Strongly agree | 12 | 15.0% |
| Agree | 9 | 11.3% | |
| Neutral | 27 | 33.8% | |
| Disagree | 20 | 25.0% | |
| Strongly disagree | 12 | 15.0% | |
| It is true that when I meet someone I worry about what they think about my appearance | Strongly agree | 16 | 20.0% |
| Agree | 8 | 10.0% | |
| Neutral | 27 | 33.8% | |
| Disagree | 18 | 22.5% | |
| Strongly disagree | 11 | 13.8% | |
| It is true for me that it doesn't matter how someone looks like | Strongly disagree | 5 | 6.3% |
| Disagree | 9 | 11.3% | |
| Neutral | 12 | 15.0% | |
| Agree | 32 | 40.0% | |
| Strongly agree | 22 | 27.5% | |
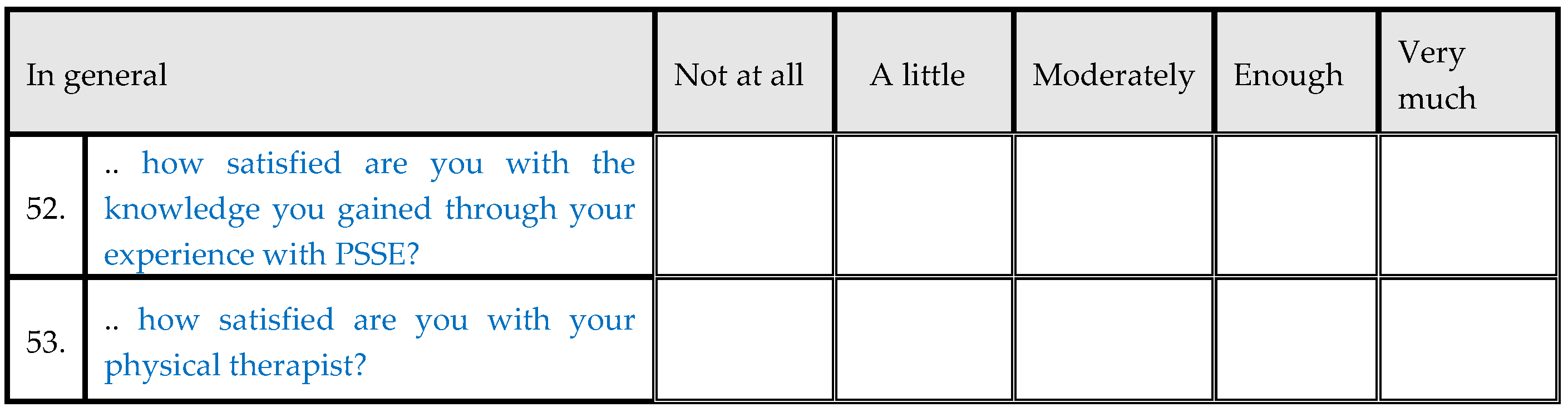
| In general how satisfied are you with the knowledge you gained through your experience with PSSE? | Not at all | 0 | 0.0% |
| A little | 0 | 0.0% | |
| Modarately | 10 | 12.5% | |
| Enough | 46 | 57.5% | |
| Very much | 24 | 30.0% | |
| In general how satisfied are you with your physical therapist? | Not at all | 1 | 1.3% |
| A little | 0 | 0.0% | |
| Modarately | 3 | 3.8% | |
| Enough | 16 | 20.0% | |
| Very much | 60 | 75.0% |
3.1. Statistical analysis
3.2. Factor analysis
3.3. Internal consistency reliability
3.4. Item convergent validity
3.5. Item divergent validity
3.6. Test-Retest Reliability
3.7. Floor and ceiling effects for the overall score
4. Discussion
Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
Appendix A
- Date of filling in the questionnaire: ….. / ….. /2022
- Name: ……………………………………………
- Surname: ………………………………………………………
- Father’s Name: ……………………………….…....
- Sex: ………………………………………………
- Date of Birth: ………………….………………………………………………
- Address:……………………………………………………………….……………………………
- Contact phone number: …………………………………………………….
- Email: ……………………………….……………………………………………………………
- Height in cm: …………………………………..
- Weight in kg: ……………..……..……… BMI: ………….…………..
- Left-handed/Right-handed? ………………………………………………………………
- For girls: Exact date the menstruation cycle started: ………………………………………
- Hair color: …………………………………………………………………………………
- Eye color: ……………………………………………………………….…….………………
- Type of scoliosis: ……………………….…………………………………………
- Standing forward bend test- Scoliometer in degrees- Hump :
- scoliometer right………thoracic…….… thoracolumbar………… lumbar…….…
- scoliometer left …… thoracic…….… thoracolumbar ….… lumbar…......…
- Seated forward bend test - Scoliometer in degrees- Hump :
- scoliometer right:thoracis……… thoracolumbar…………… lumbar …...…
- scoliometer left: thoracic……… thoracolumbar…………… lumbar ….…
- Cobb Angle: ………………………...............................
- Risser Sign : ………………………………………………………….
- Formetric: (if there is any please attach it)
- Treatment (wearing brace?) ………………………………………
- Which method of Physiotherapeutic Specific Scoliosis Exercises is being used:
- …………………………………………………………………………………………………
- TEST-VALIDITY: RETEST: RESPONSIVENESS
- Clinic:



- 54.
- What would you like to have been different in the whole experience you have had so far with PSSE?
- 55.
- How would you feel if you been told that you must continue PSSE until you reach adulthood?
- 56.
- What changes do you think would improve this questionnaire?
- 57.
- Have you felt this questionnaire was tiresome? (Please explain)
- 58.
- Would you rather not answer some of the questions? which ones? (Please write down the numbers of the questions)
- 59.
- Would you like to comment on anything else?
References
- Kikanloo SR, Tarpada SP, Cho W. Etiology of Adolescent Idiopathic Scoliosis: A Literature Review. Asian Spine Journal [Internet]. 2019 Jun 1;13(3):519–26. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6547389/.
- Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of Bracing in Adolescents with Idiopathic Scoliosis. New England Journal of Medicine. 2013 Oct 17;369(16):1512–21.
- Hawes MC, O’Brien JP. The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis. 2006 Mar 31;1(1).
- Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and Spinal Disorders. 2018 Jan 10;13(1).
- Grossman TW, Mazur JM, Cummings RJ. An Evaluation of the Adams Forward Bend Test and the Scoliometer in a Scoliosis School Screening Setting. Journal of Pediatric Orthopaedics. 1995 Jul;15(4):535–8.
- Fabio Galbusera, Bassani T, Panico M, Luca Maria Sconfienza, Cina A. A fresh look at spinal alignment and deformities: Automated analysis of a large database of 9832 biplanar radiographs. Frontiers in Bioengineering and Biotechnology [Internet]. 2022 Jul 15 [cited 2023 Nov 16];10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9335010/.
- Choudhry MN, Ahmad Z, Verma R. Adolescent Idiopathic Scoliosis. The Open Orthopaedics Journal. 2016 May 30;10(1):143–54.
- Peng Y, Wang SR, Qiu GX, Zhang JG, Zhuang QY. Research progress on the etiology and pathogenesis of adolescent idiopathic scoliosis. Chinese Medical Journal [Internet]. 2020 Feb 20;133(4):483–93. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9335010/. 7046.
- Balagué F, Pellisé F. Adolescent idiopathic scoliosis and back pain. Scoliosis and Spinal Disorders. 2016 Sep 9;11(1).
- Théroux J, Le May S, Hebert JJ, Labelle H. Back Pain Prevalence Is Associated With Curve-type and Severity in Adolescents With Idiopathic Scoliosis. SPINE. 2017 Aug;42(15):E914–9.
- Kobayashi K, Ando K, Machino M, Tanaka S, Morozumi M, Kanbara S, et al. Trends in Medical Costs for Adolescent Idiopathic Scoliosis Surgery in Japan. Global Spine Journal. 2019 Oct 29;10(8):1040–5.
- Boylan MR, Riesgo AM, Chu A, Paulino CB, Feldman DS. Costs and complications of increased length of stay following adolescent idiopathic scoliosis surgery. Journal of Pediatric Orthopaedics B. 2019 Jan;28(1):27–31.
- Bettany-Saltikov J, Parent E, Romano M, Villagrasa M, Negrini S. Physiotherapeutic scoliosis-specific exercises for adolescents with idiopathic scoliosis. European Journal of Physical and Rehabilitation Medicine [Internet]. 2014 Feb 1;50(1):111–21. Available from: https://pubmed.ncbi.nlm.nih.gov/24525556/. 2452.
- Berdishevsky H, Lebel VA, Bettany-Saltikov J, Rigo M, Lebel A, Hennes A, et al. Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Scoliosis and Spinal Disorders. 2016 Aug 4;11(1).
- Côté P, Kreitz BG, Cassidy JD, Dzus AK, Martel J. A study of the diagnostic accuracy and reliability of the Scoliometer and Adam’s forward bend test. Spine [Internet]. 1998;23(7):796–802; discussion 803. Available from: https://pubmed.ncbi.nlm.nih.gov/24525556/. 9563.
- Diers H, Mooshake S, Heitmann K. Dynamic 3D (4D) in objective classification of severe back deformities. Scoliosis. 2009 Dec;4(S2).
- Seleviciene V, Cesnaviciute A, Strukcinskiene B, Marcinowicz L, Strazdiene N, Genowska A. Physiotherapeutic Scoliosis-Specific Exercise Methodologies Used for Conservative Treatment of Adolescent Idiopathic Scoliosis, and Their Effectiveness: An Extended Literature Review of Current Research and Practice. International Journal of Environmental Research and Public Health. 2022 Jul 28;19(15):9240.
- Jenn, NC. Designing A Questionnaire. Malaysian family physician: the official journal of the Academy of Family Physicians of Malaysia [Internet]. 2006 Apr 30;1(1):32–5. Available from: https://www.ncbi.nlm.nih. 4797. [Google Scholar]
- Weir CB, Jan A. BMI Classification Percentile And Cut Off Points [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://pubmed.ncbi.nlm.nih. 3108.
- Wang J, Zhang J, Xu R, Chen TG, Zhou KS, Zhang HH. Measurement of scoliosis Cobb angle by end vertebra tilt angle method. Journal of Orthopaedic Surgery and Research. 2018 Sep 4;13(1).
- Subramanian S, Viswanathan VK. Bone Age [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih. 5370.
- Asher M, Min Lai S, Burton D, Manna B. The Reliability and Concurrent Validity of the Scoliosis Research Society-22 Patient Questionnaire for Idiopathic Scoliosis. Spine. 2003 Jan;28(1):63–9.
- Vasiliadis E, Grivas TB, Gkoltsiou K. Development and preliminary validation of Brace Questionnaire (BrQ): a new instrument for measuring quality of life of brace treated scoliotics. Scoliosis. 2006 May 20 ;1(1).
- Ware JE, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. Journal of Clinical Epidemiology. 1998 Nov;51(11):903–12.
- Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care [Internet]. 1996;34(3):220–33. Available from: https://www.ncbi.nlm.nih.gov/pubmed/8628042. 8628.
- Sanders JO, Harrast JJ, Kuklo TR, Polly DW, Bridwell KH, Diab M, et al. The Spinal Appearance Questionnaire: Results of Reliability, Validity, and Responsiveness Testing in Patients With Idiopathic Scoliosis. Spine [Internet]. 2007 Nov 15 [cited 2021 May 2];32(24):2719–22. Available from: https://journals.lww.com/spinejournal/Abstract/2007/11150/The_Spinal_Appearance_Questionnaire__Results_of.15.aspx#:~:text=This%20study%20tested%20the%20instrument. 2 May.
- Antonarakos PD, Katranitsa L, Angelis L, Paganas A, Koen EM, Christodoulou EA, et al. Reliability and validity of the adapted Greek version of scoliosis research society – 22 (SRS-22) questionnaire. Scoliosis. 2009 Jul 16;4(1).
- Yapar A, Yapar D, Ergisi Y, Kaptan AY, Tokgoz MA, Senkoylu A. Reliability and validity of the adapted Turkish version of the Spinal Appearance Questionnaire. Spine Deformity. 2020 Aug 17;9(1):57–66.
- Pappa E, Kontodimopoulos N, Niakas D. Validating and norming of the Greek SF-36 Health Survey. Quality of Life Research. 2005 Jun;14(5):1433–8.
- Carreon LY, Sanders JO, Polly DW, Sucato DJ, Parent S, Roy-Beaudry M, et al. Spinal Appearance Questionnaire. Spine. 2011 Aug;36(18):E1240–4.
- Roy-Beaudry M, Beauséjour M, Joncas J, Forcier M, Bekhiche S, Labelle H, et al. Validation and Clinical Relevance of a French-Canadian Version of the Spinal Appearance Questionnaire in Adolescent Patients. Spine. 2011 Apr;36(9):746–51.
- Wei X, Zhu X, Bai Y, Wu D, Chen J, Wang C, et al. Development of the Simplified Chinese Version of the Spinal Appearance Questionnaire. Spine. 2012 Aug;37(17):1497–504.
- Guo J, Lau AHY, Chau J, Ng BKW, Lee KM, Qiu Y, et al. A validation study on the traditional Chinese version of Spinal Appearance Questionnaire for adolescent idiopathic scoliosis. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society [Internet]. 2016 Oct 1 [cited 2023 Nov 16];25(10):3186–93. Available from: https://pubmed.ncbi.nlm.nih.gov/27167743/.
| Domain | Number of items | Cronbach's alpha | Item convergent validity* | Floor effects | Ceiling effects |
|---|---|---|---|---|---|
| Physical functioning | 12 | 0.452 | 75.0% | 0(0%) | 0(0%) |
| Self Image | 4 | 0.16 | 100.0% | 0(0%) | 0(0%) |
| PSSEs | 8 | 0.514 | 87.5% | 0(0%) | 0(0%) |
| Psychosocial Functioning | 12 | 0.75 | 75.0% | 0(0%) | 0(0%) |
| Cognitive functioning | 5 | 0.641 | 100.0% | 0(0%) | 0(0%) |
| Compliance | 8 | 0.822 | 100.0% | 0(0%) | 1(1.25%) |
| Motivation | 2 | 0.156 | 100.0% | 0(0%) | 3(3.8%) |
| Pain | 2 | 0.313 | 50.0% | 4(5%) | 2(2.5%) |
| Total | 53 | 0.836 | 79.2% | 0(0%) | 0(0%) |
| No of Item | Floor effect | Ceiling effect |
|---|---|---|
| 1 | 1 (1.3%) | 17 (21.3%) |
| 2 | 0 (0%) | 22 (27.5%) |
| 3 | 0 (0%) | 26 (32.5%) |
| 4 | 0 (0%) | 26 (32.5%) |
| 5 | 2 (2.5%) | 8 (10%) |
| 6 | 3 (3.8%) | 32 (40%) |
| 7 | 0 (0%) | 58 (72.5%) |
| 8 | 1 (1.3%) | 14 (17.5%) |
| 9 | 51 (63.8%) | 7 (8.8%) |
| 10 | 3 (3.8%) | 28 (35%) |
| 11 | 2 (2.5%) | 4 (5%) |
| 12 | 6 (7.5%) | 10 (12.5%) |
| 13 | 10 (12.5%) | 15 (18.8%) |
| 14 | 12 (15%) | 5 (6.3%) |
| 15 | 27 (33.8%) | 7 (8.8%) |
| 16 | 6 (7.5%) | 33 (41.3%) |
| 17 | 4 (5%) | 9 (11.3%) |
| 18 | 0 (0%) | 45 (56.3%) |
| 19 | 0 (0%) | 34 (42.5%) |
| 20 | 10 (12.5%) | 13 (16.3%) |
| 21 | 10 (12.5%) | 11 (13.8%) |
| 22 | 12 (15%) | 13 (16.3%) |
| 23 | 18 (22.5%) | 3 (3.8%) |
| 24 | 5 (6.3%) | 18 (22.5%) |
| 25 | 10 (12.5%) | 15 (18.8%) |
| 26 | 5 (6.3%) | 8 (10%) |
| 27 | 0 (0%) | 41 (51.3%) |
| 28 | 10 (12.5%) | 17 (21.3%) |
| 29 | 3 (3.8%) | 14 (17.5%) |
| 30 | 0 (0%) | 42 (52.5%) |
| 31 | 13 (16.3%) | 20 (25%) |
| 32 | 0 (0%) | 31 (38.8%) |
| 33 | 2 (2.5%) | 25 (31.3%) |
| 34 | 19 (23.8%) | 17 (21.3%) |
| 35 | 25 (31.3%) | 16 (20%) |
| 36 | 24 (30%) | 15 (18.8%) |
| 37 | 0 (0%) | 38 (47.5%) |
| 38 | 5 (6.3%) | 24 (30%) |
| 39 | 2 (2.5%) | 30 (37.5%) |
| 40 | 26 (32.5%) | 14 (17.5%) |
| 41 | 15 (18.8%) | 13 (16.3%) |
| 42 | 5 (6.3%) | 6 (7.5%) |
| 43 | 15 (18.8%) | 9 (11.3%) |
| 44 | 25 (31.3%) | 19 (23.8%) |
| 45 | 15 (18.8%) | 11 (13.8%) |
| 46 | 25 (31.3%) | 17 (21.3%) |
| 47 | 3 (3.8%) | 44 (55%) |
| 48 | 0 (0%) | 60 (75%) |
| 49 | 12 (15%) | 12 (15%) |
| 50 | 16 (20%) | 11 (13.8%) |
| 51 | 5 (6.3%) | 22 (27.5%) |
| 52 | 0 (0%) | 24 (30%) |
| 53 | 1 (1.3%) | 60 (75%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





