1. Introduction
Tendon and ligament injuries account for a large proportion of sport horse’s wastage and early retirement. Most injuries are overstrained injuries as these structures operate near their functional limits in sport horses. Tendons and ligaments are highly organized tissues that depend on the strength and structure of the extracellular matrix to function [
1]. Overloading can lead to physical damage and degeneration [
1,
2]. Although tendons and ligaments can heal spontaneously with time, the fibrous scar tissue formed is biomechanically inferior leading to a decrease in performance, as well as recurrent reinjuries and lameness. Tarsocrural desmitis is an inflammatory event affecting the ligaments of the tarsocrural joint, causing hindlimb lameness in horses. It is often clinically underdiagnosed because it is an uncommon pathology and has a guarded prognosis for athletic soundness [
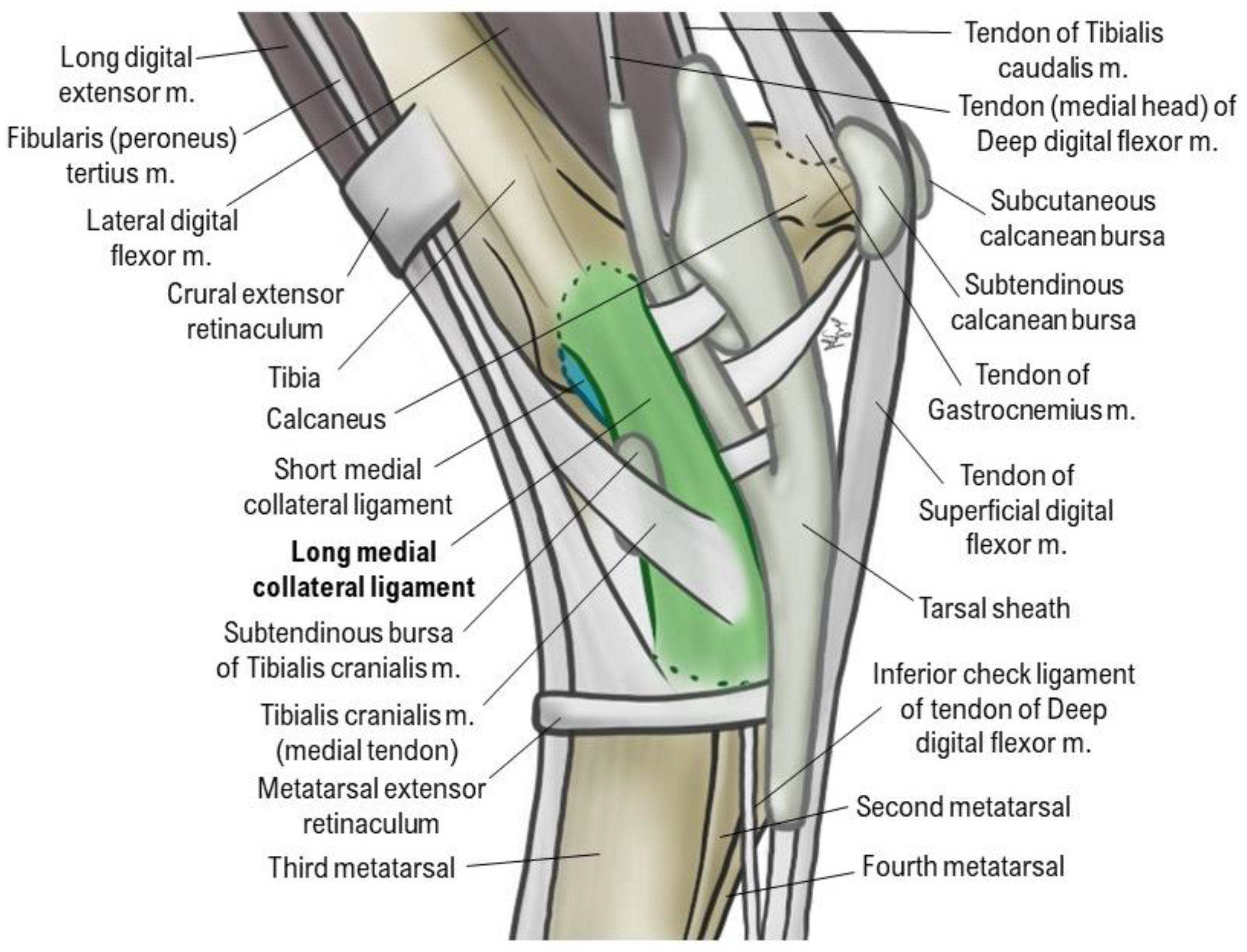
3]. Tarsus pathologies are a complex puzzle to solve because of an intricate relationship between structures: synovial structures, bone, bursae, ligaments, tendons and tendon sheaths, that are all susceptible to a considerable incidence of pathology [
4]. An overview of kinematic and a good knowledge of anatomy are essential for a better understanding of tarsus pathology [
5] (
Figure 1).
There are four collateral ligaments in the tarsus. The long lateral collateral ligament (LLCL) arises from the lateral malleolus of the tibia and inserts on the proximal end of metatarsal IV (lateral splint bone). Between these points it attaches to the lateral tarsal bones. The short lateral collateral ligament (SLCL), deep to the long lateral collateral, arises from the lateral malleolus of the tibia and attaches via two branches, one to the calcaneus and one to the talus. The long medial collateral ligament arises from the medial malleolus and inserts on the proximal end of metatarsal II (medial splint bone). Between these points it attaches to the medial tarsal bones. The short medial collateral ligament (SMCL), deep to the long medial collateral, arises from the medial malleolus and attaches via two branches, one on the calcaneus and one on the talus.
From a functional perspective, the long CLs are taut during extension and loose during flexion of the tarsocrural joint. The short CLs show a more complex behavior during the range of motion of the tarsocrural joint but most parts are tense in flexion and loose in extension [
5].
Horses with collateral ligament desmitis typically demonstrate moderate to severe lameness but may present an obscure lameness accompanied by synovial effusion and minimal radiographic change [
6]. Ultrasonographic signs of desmitis are similar to those in any ligament and include increased size, decreased echogenicity, and abnormal fiber pattern [
7].
Medial tarsal collateral desmitis has been few described in veterinary literature, however is one of the most common soft tissue injuries of the tarsus [
7,
8,
9,
10,
11,
12,
13,
14] A study emphasized collateral desmitis was the most common tarsal ligament injury (26/128 horses), being tarsus medial collateral ligament desmitis the most common ultrasonographic diagnosed injury (18/26 horses) [
12].
Intra-articular soft tissue injuries of the tarsus are poorly documented because the clinical signs are very unspecific and may include edema over the injured collateral ligament and/or effusion within the tarsocrural joint and mild to non-weight bearing lameness with positive joint flexion test [
8,
15]. Chronic pain and osteoarthritis (OA) may develop secondary to joint instability leading to cartilage damage in horses with collateral ligament injuries of the tarsocrural joint.
Blaik et al., 2000, reported tarsal pain is responsible for 80% of chronic, low-grade hind limb lameness in horses, with bone spavin, osteochondrosis, tendon and ligament injury and synovial disease being frequently diagnosed [
16]. Hemarthrosis may also develop and is documented as a major factor of pain in both horses and humans [
4,
7,
8,
10,
17,
18,
19,
20]. As a result of nonspecific clinical signs, definitive diagnosis is often difficult to achieve, and implies resorting to diagnostic imaging techniques such as radiology, ultrasonography, computed tomography (CT) or magnetic resonance imaging (MRI) [
9,
16,
21,
22].
Therefore, diagnosis of tarsus collateral ligament desmitis is often made by ruling out other causes of joint injury in combination with diagnostic imaging specific for soft tissue, such as ultrasound and MRI [
9].
Literature, often refers to treatment of this pathology with rest, local and/or systemic anti-inflammatories, local and/or systemic antibiotherapy (in the presence of wound), laser, shock wave, joint lavage, arthroscopy and ligament engraftment [
6,
8,
9,
10,
14,
23]. The outcome of these procedures is not very advantageous, since there is a guarded prognosis to return to same performance level and OA is usually secondarily associated [
8].
In equine musculoskeletal medicine, regenerative stem cell therapies and immunomodulatory/paracrine therapies are gaining increased interest due to their anti-inflammatory and immunomodulatory properties, regenerative potential, and high tolerability[
24]. Stem cell therapies consist in injection of mesenchymal stem cells (MSCs) itself or MSC cell free treatments or induced pluripotent stem cells (iPSCs) [
1,
25,
26]. As immunomodulatory or paracrine therapies, we may also consider hemoderivative therapies such as platelet rich plasma (PRP), autologous conditioned medium (ACS), autologous protein solution (APS) and, more recently, receiving more attention from the scientific community - extracellular vesicles (EVs) [
1,
10,
25,
27,
28,
29,
30].
Regenerative medicine aims to replace or regenerate cells and tissues and to restore normal structure and function of injured tissue [
1,
3]. As previously stated, the use of multipotent Mesenchymal Stem/ Stromal Cells (MSCs) therapy is one of the strategies [
4,
5,
6] holding immense promise [
33]. MSCs are adult multipotent progenitor cells, found in many organs and tissue types, that are able to self-renew, to migrate to injury sites (homing), to differentiate into multiple lineages and to secrete bioactive factors, providing immunomodulation, increasing proliferation and migration of tendon stem/progenitor cells via paracrine signaling and increasing the regeneration ability of tissues with poor aptitude [
27,
31].
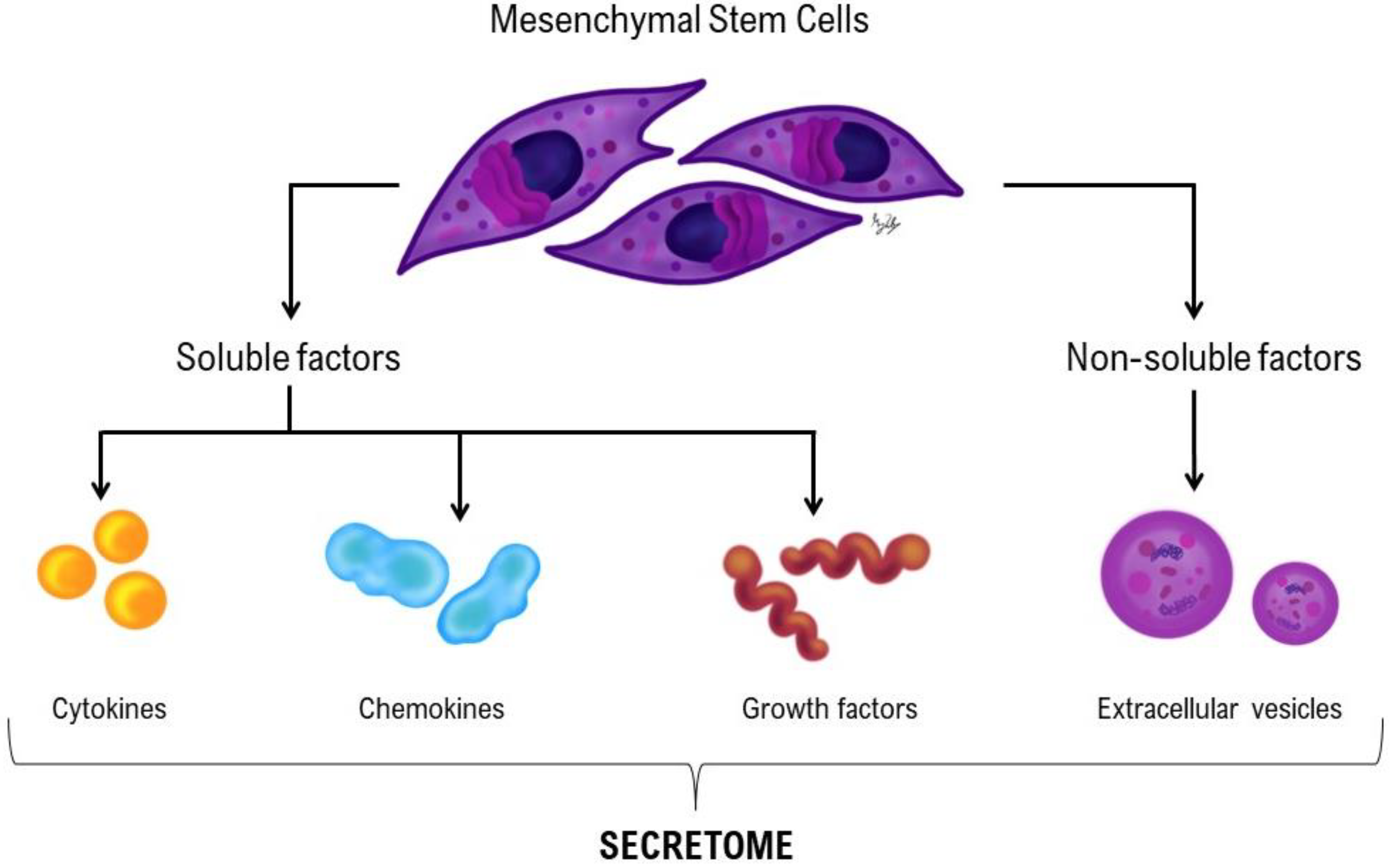
Originally considered as whole-cell therapy, whereby injected MSCs “homed” towards the site of tissue damage and differentiated into the cells needed for repair or regeneration, it is now accepted that transplanted MSCs do not survive for long and that the effects of MSC-based therapies are due to a broad array of secreted bioactive factors, collectively referred to as the secretome [
32,
33].
The secretome of cells is a commixture of soluble factors (cytokines, chemokines and growth factors) as well as non-soluble factors - molecules associated with extracellular vesicles - lipid bilayer delimited particles of various sizes and complexities containing proteins and nucleic acids released from cells into the extracellular space (
Figure 2). These particles can be found in secretome at various concentrations and their activity levels are determined by cell type and environment [
34,
35]. They activate the resident stem cells and hence mediate the endogenous regeneration [
36].
Interestingly, in light of the many findings regarding their identity and function, the adequate designation or nomenclature of the MSCs acronym has become itself a field of debate. Classically, the “Mesenchymal Stem Cells” designation, as proposed by the International Society for Cellular Therapy (ISCT) while defining the minimal criteria, has been the most widely accepted [
37]. However, other scientific current advocates that these do not represent ‘true’ stem cells, since there is still lacking indisputable evidence of some critical stemness features (such as the asymmetric cell division and complete lineage renewal), and the term “Mesenchymal Stromal Cell” is proposed to better describe the conventionally isolated populations [
38]. More recently, it was proposed that these should be renamed as “Medicinal Signaling Cells” to more accurately reflect the fact that these cells home in on sites of injury or disease and secrete bioactive factors that are immunomodulatory and trophic (regenerative) meaning that these cells make therapeutic drugs
in situ that are medicinal [
39].
The recognition that MSCs secreted factors are responsible for their positive effects on tissue repair is significant, as it spurs the design of MSC-based therapies that do not require administration of the cells, thus avoiding negative side effects that might be correlated with cell administration such as unwanted differentiation of engrafted MSCs, immune reactions or unwanted tumor growth [
31,
40]. MSC-sourced secretome can be immediately available for treatment of acute conditions and could be massively produced from commercially available cell lines avoiding invasive cell collection procedure [
31]. Cell-free products have demonstrated preclinical efficacy without significant safety issue, as they appear to be non-cytotoxicity, non-mutagenicity and have low immunogenicity. They also have the advantage of overcoming the challenge of cell viability maintenance and potency throughout the manufacture, storage, and delivery, maintaining the advantages of therapeutic ability [
36]. Several cell-free preparations have shown encouraging outcomes in early stage clinical trials [
41].
Though MSCs isolated from various tissues display a variety of common appearances, their biological functions, and some markers are dissimilar depending on the their origins [
41].
The present work describes a clinical case of a seven years old male show jumping horse, who sustained an injury of the LMCL of the right hindlimb tarsus, its diagnosis and the treatment with a therapeutic combination of eSM-MSCs + eUC-MSCs CM.
This work also focused on the determination of the therapeutic potential of eSM-MSCs and eUC-MSCs populations and the evaluation of their synergistic effect in the treatment of an equine ligament desmitis case, utilizing the cells themselves plus cell-derived secretome. For such validation, given the pre-established potential of eSM-MSCs, the cytokine content of eUC-MSCs was assessed, through the determination of selected bioactive factors (IL-6 and IL-8), as a prospect of its incremental and synergistic beneficial contributes and therapeutic properties.
2. Materials and Methods
2.1. Ethics and Regulation
This case was carried out in accordance with Organismo Responsável pelo Bem Estar Animal (ORBEA) from ICBAS-UP, project number: P289/ORBEA/2018 recommendations and authorization. Treatments were performed with permission and signature of an informed consent from the patient’s legal tutor, following a thorough explanation on the procedure itself and possible risks and associated effects, in accordance with national regulations and project approval from the competent authorities.
2.2. Patient Identification
In this clinical case report, the patient is a seven-year-old stallion, show jumper with an acute lesion of the right hindlimb tarsus.
2.3. Patient Clinical Evaluation
A seven-year-old stallion was examined for a complaint of a swollen right tarsus. Upon examination, the right tarsus was severely swollen with significant effusion of the tarsocrural joint (
Figure 3).
Patient undergone identification, anamnesis, physical examination (cardiac and respiratory frequency, body temperature, mucous membrane examination, inspection of the whole body and palpation), orthopedic examination (evaluation of the limbs, gait inspection and movements – walk, trot and gallop, and flexion test of the main joints for 60 seconds followed by trot). Lameness was evaluated at walk and trot on hard surface and scored in a scale of 0 to 5, according to American Association of Equine Practitioners (AAEP) parameters –
Table 1.
Palpation and manipulation were not resented and no swelling in the lower limb was observed. The horse was not lame at the walk or trot in a straight line but was a little reluctant to fully bear weight on the right hind leg when turned to the right (grade 2/5 according to AAEP lameness grading scale). Flexion test and pain to pressure were also evaluated and no flexion response and no pain to pressure were identified [
54].
Complementary diagnostic exams included radiographs and ultrasound images, as reported in other studies [
59,
63,
64,
65,
66,
67,
68,
69,
70].
2.4. Complementary Diagnostic Exams
2.4.1. Radiological Examination
Radiological examination (X ray) of the right tarsocrural joint was performed with a digital system – CareRay Cw series®, radiological constants: 72 Kv, 0,8 mA. Four standard views – lateromedial, dorsoplantar, dorsolateral-plantaromedial and dorsomedial-plantarolateral – were obtained.
2.4.2. Ultrasound Examination
Ultrasound examination (U/S) of the right and left tarsocrural joint was performed in longitudinal and transversal scans using a 7,5-MHz linear of a digital portable ultrasound system-Sonoscape A6®.
The contralateral limb was considered normal and used as control. Echogenicity, fiber pattern, and cross-sectional area were evaluated in each collateral ligament. The synovial fluid was evaluated for signs of hemarthrosis (increase in echogenicity and/or a swirling echogenic pattern). The synovial lining was evaluated for thickening and fibrinous loculations in the tarsocrural joint. The medial and lateral long and short collateral ligaments of the tarsus were examined in longitudinal and transverse planes, from proximal to distal.
2.5. Donor Selection and SM Collection
Equine SM-MSCs’ donor was a young and healthy foal (six months old) who died accidentally. Briefly, the tutor authorized synovial membrane collection from hocks, knees and fetlocks. Skin covering the incisional field was surgically cleaned with chlorohexidine and alcohol. Skin and subcutaneous tissue were incised, and debrided, articular capsule was opened, and synovial membrane was isolated and extracted into a Dulbecco′s Phosphate Buffered Saline (DPBS – 14190-144, Gibco
®) container. Samples were transported to the laboratory with ice packs for refrigerated temperatures. These procedures were previously described at
Leal Reis et al, 2023 [
43].
2.6. Equine SM-MSCs Isolation, Culture and Characterization
After collection, equine synovial membrane, was prepared at the Laboratory of Veterinary Cell-based Therapies – ICBAS-UP. The isolation protocol of eSM-MSCs was developed by patented proprietary technology Regenera
® (PCT/IB2019/052006, WO2019175773 – Compositions for use in the treatment of musculoskeletal conditions and methods for producing the same leveraging the synergistic activity of two different types of mesenchymal stromal/ stem cells – Regenera
®), previously described [
43].
Before cryopreservation of the cells batch, the culture medium was subjected to a bacteriological control using the BACT/ALERT® (BioMérieux Portugal®) medium, to rule out the presence of any bacterial or fungal contamination.
2.7. Equine UC-MSCs Isolation, Culture and Characterization
Equine UC-MSCs were isolated from the equine umbilical cord matrix (Wharton’s jelly), a birth residue, collected during a full-term parturition of a different foal from which the synovial tissues were obtained.
Briefly, tissue samples were collected and placed in transport media [supplemented with penicillin (300 U/mL)-streptomycin (300 μg/mL) (15140-122 - Gibco®), and amphotericin B (5 μg/mL) (15290-026 - Gibco®). Upon arrival, umbilical cord tissues were decontaminated and dissected for the isolation of the stromal tissue, which was digested using Colagenase I (17100-017 - Gibco®) and Dispase II (17105-041 - Gibco®). Single cell suspension of the digested tissues was obtained through a 70 µm cell strainer (CLS431751 – Corning® Falcon®) and cultured in DMEM-HG (11965092 - Gibco®), 20% (v/v) MSC qualified FBS (04-400-1A, Biological Industries Israel Beit-Haemek Ltd), penicillin (150 U/mL)-streptomycin (150 μg/mL), and amphotericin B (3.75 μg/mL) for the first 24 hours. Non-adherent cells were discarded after 24 hours and remaining cells further expanded in DMEM-LG (11885-084 - Gibco®), 10% (v/v) FBS, penicillin (100 U/mL)-streptomycin (100 μg/mL) (Gibco®), and amphotericin B (2.5 μg/mL) (Gibco®) to form culture of adherent cells with fibroblastic morphology. This process was performed and is patented proprietary technology (PCT/IB2019/052006, WO2019175773 – Regenera®).
Before cryopreservation of the cells batch, the culture medium was subjected to a bacteriological control using the BACT/ALERT® (BioMérieux Portugal®) medium, to rule out the presence of any bacterial or fungal contamination.
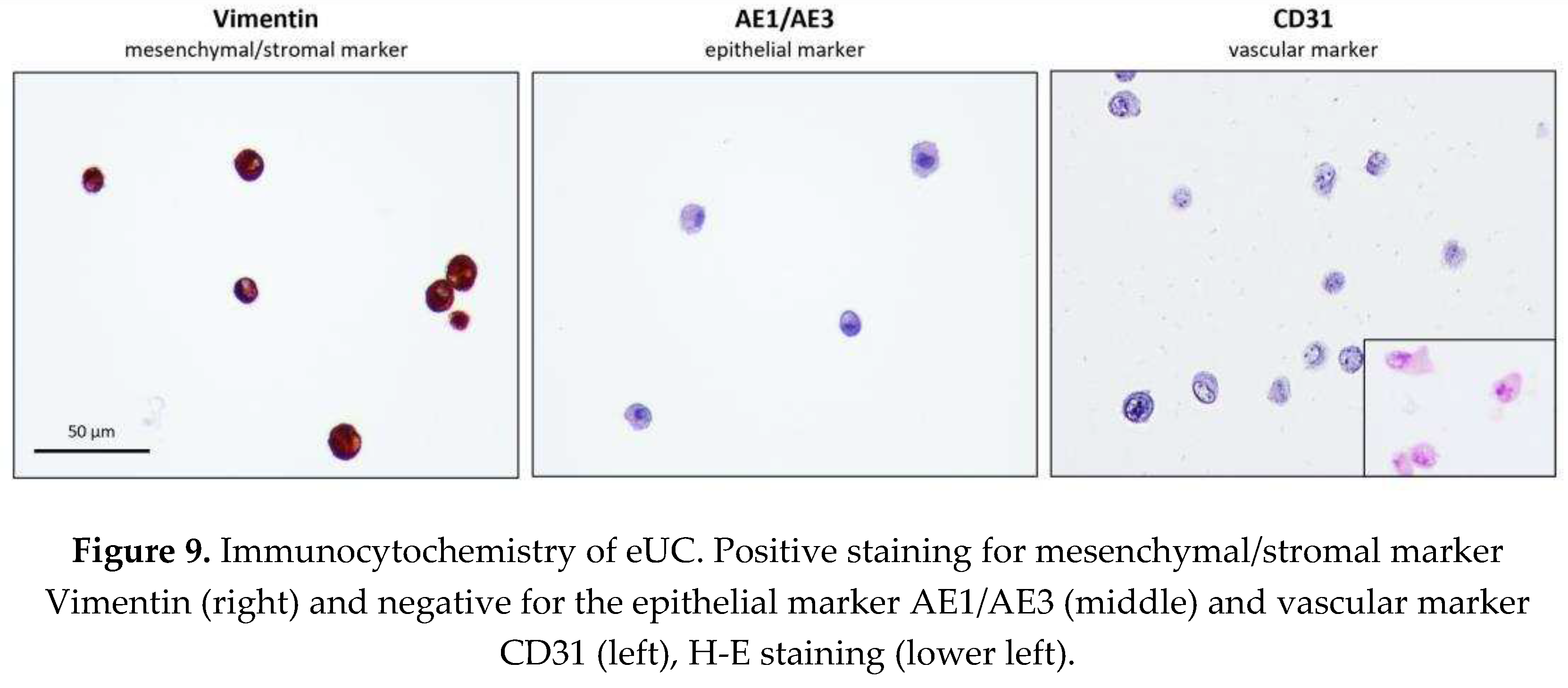
Isolated populations immunophenotype was validated in Passage 5, protocol was previously described [
43]. The antibodies were selected to confirm the mesenchymal/ stromal origin - non-epithelial origin histogenesis – Vimentin [Clone V9 – M0725 Dako Denmark; 1/500 dilution RS/WB antigen unmasking; Canine mammary gland pos. control] and discard vascular/endothelial – CD31 [Clone JC70A – M0823 :Dako Denmark 1/50 dilution Pepsine antigen unmasking; Canine spleen pos. Control] and epithelial – Pancytokeratin [Cocktail AE1/AE3 – M3-343-P1 Thermo Scientific 1/300 ON RS/WB Canine mammary gland pos. Contorl] origin of eUC-MSCs. For each antibody, appropriate negative and positive controls were included, all primary antibodies were incubated overnight.
Trilineage differentiation was also validated in Passage 5: Adipogenic, Chondrogenic and Osteogenic differentiation (StemPro® Differentiation kits: A1007201 – Osteogenesis; A1007001 – Adipogenesis; A1007101 – Chondrogenesis, Gibco®), assessed through Oil Red-O, Alcian Blue and Von Kossa stainings, respectively). All protocols followed as described in [
43], except for Von Kosa staining employed to visualize mineral extracellular deposition: cells were fixated and dehydrated with increasing ethanol concentrations. Then, cells were rehydrated and incubated with 2% Silver Nitrate (7761-88-8, Sigma-Aldirch) solution, under Ultra-violet light and sodium thiosulfate (1091471000, Merk
TM) 5% for 3 minutes. Wells were rinsed, and photographic record obtained.
2.8. Secretome – Conditioned Medium Preparation and Analysis
Conditioned Medium of eSM-MSCs and eUC-MSCs in Passage 4 and 6, respectively, was analyzed to identify cytokines and chemokines secreted after conditioning. When in culture, after reaching a confluence of around 70–80%, the culture medium was removed, and the culture flasks were gently washed with DPBS two to three times. Then, the culture flasks were further washed two to three times with the basal culture medium of each cell type, without any supplementation. To begin the conditioning, non-supplemented DMEM/F12 GlutaMAX™ (31331-093 - Gibco
®) culture medium was added to the culture flasks, which were then incubated under standard conditions. The culture medium rich in factors secreted by the cells (CM) was collected after 48 h. The collected CM was then concentrated five times (5×). After collection, it was centrifuged for 10 min at 3000 x
g and the supernatant was collected and filtered with a 0.2 μm syringe filter (Filtropur S, PES, Sarstedt
®). For the concentration procedure, Pierce™ Protein Concentrator, 3k MWCO, 5–20 mL tubes (88525, Thermo Scientific
®) were used. Initially, the concentrators were sterilized following the manufacturer’s instructions. Briefly, the upper compartment of each concentrator tube was filled with 70% ethanol (v/v) and centrifuged at 3000 ×g for 10 min. Then, the ethanol was discarded, and the same procedure was carried out with DPBS. Each concentrator tube was subjected to two such centrifugation cycles, followed by a 10-min period in the laminar flow hood for complete drying. Finally, the upper compartment of the concentrator tubes was filled with plain CM (1× concentration) and subjected to new centrifugation cycle, under the conditions described above, for the number of cycles necessary to obtain the desired CM concentration (5×). Equine SM-MSCs secretome has been previously described [
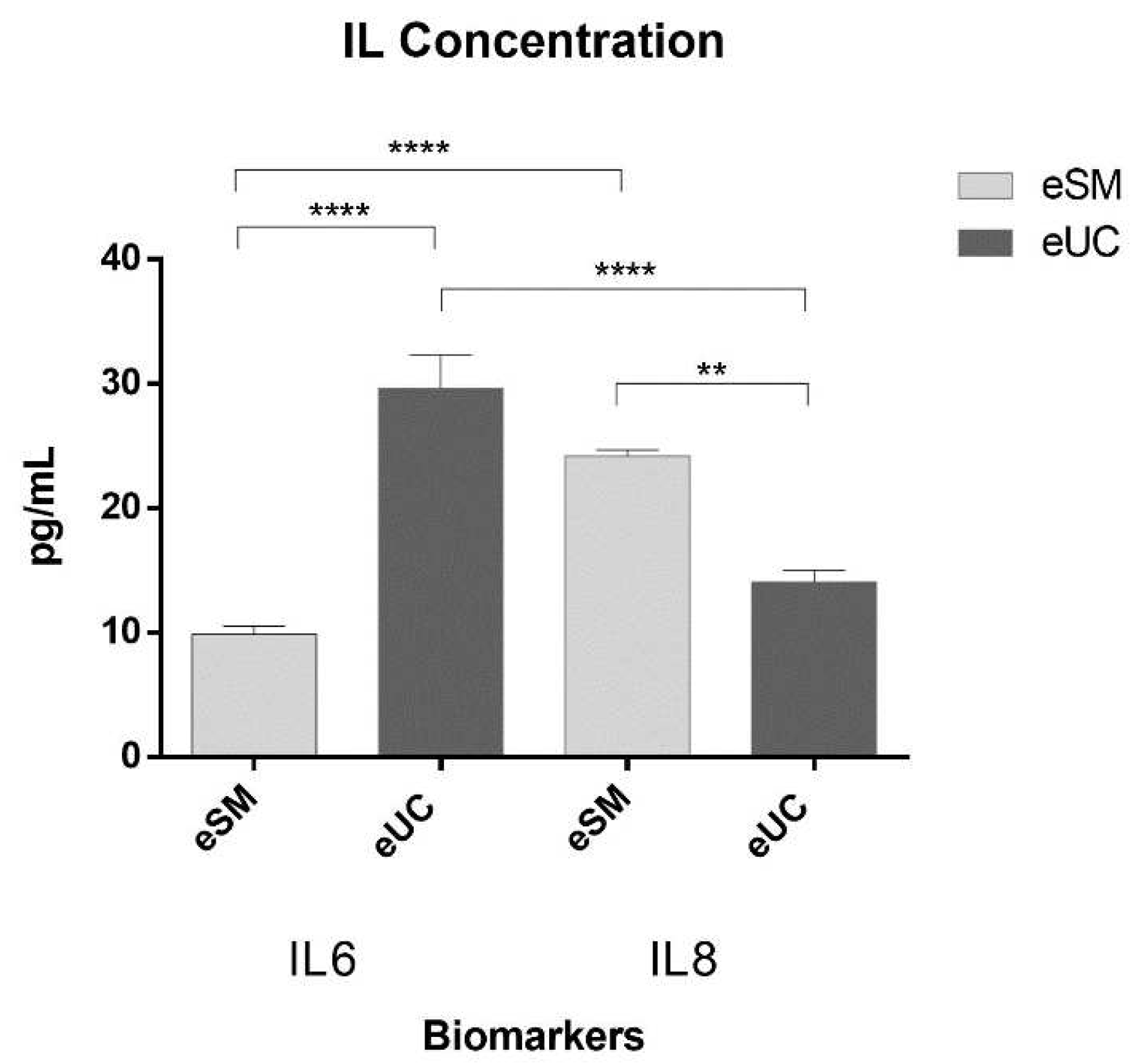
43]. For the eUC-MSCs, the concentrated CM was stored at -20°C and subsequently subjected to a Multiplexing LASER Bead analysis (Eve Technologies, Calgary, AB, Canada) to selected equine biomarkers IL-6 and IL-8. All samples from the batch were analyzed in triplicate.
Quantitative data was statistically analyzed through one-way ANOVA, followed by pairwise comparison Tukey’s HSD post hoc test. Statistical analysis was performed using the GraphPad Prism version 6.00 for Mac OS X (GraphPad Software, La Jolla California USA), and significance defined for P<0.05, represented using respectively one-four (*) referring to 0.01≤P<0.05; 0.001≤P< 0.01; 0.0001≤P<0.001 and P<0.0001.
2.9. Equine SM-MSCs + eUC-MSC CM Solution Preparation
The eSM-MSCs solution for intra-ligamental clinical application, was a combination of allogeneic eSM-MSCs suspended in eUC-MSCs CM.
Cryopreserved P3 eSM-MSCs batches were thawed and suspended in recipient animal’s heat inactivated autologous serum. For this purpose, 10 mL of whole blood was collected into two serum tubes (367820 - BD Vacutainer®). The tubes were then centrifuged at 6000 xg for 10 minutes and the supernatant (autologous serum) was collected into a 15 mL tube. The serum sample was heat inactivated for 20 minutes at 56ºC (water bath), quickly cooled down in an ice bath and sterile filtered with a syringe filter with 0.22 µm into a new 15 mL tube. For one 9x106 eSM-MSCs dose, 3x2 mL eSM-MSCs vials containing around 3x106 cells each were thawed in a 37ºC water bath and the cell suspension of the 3 vials were mixed into one 15 mL tube. 2-3 mL of autologous serum were slowly added to the tube (drop-wise) and the suspension was gently mixed. 5 mL of PBS were slowly added into the tube and the suspension gently mixed and centrifuged at 3000 xg for 10 minutes. The supernatant was discarded, and the cell pellet resuspended in a mixture of autologous serum in a ratio of 0,8:1. Cell counting and viability was determined by the Trypan Blue exclusion dye assay (T10282 - Invitrogen TM) using an automatic counter (Countess II FL Automated Cell Counter, Thermo Fisher Scientific®). Around 8.58x106 cells were counted with an average viability of 98% (triplicate count) before the first administration, and 9.42x106 cells were counted with an average viability of 100% (triplicate count) before the second one. Cell number was then adjusted to 1x107 cells/mL. At this point the conditioned medium from eUC-MSCs was thawed and added to the suspension to a final 1:1 concentration. 2 mL of the solution of eSM-MSCs suspended in eUC-MSCs CM were transferred to a perforable capped vial and preserved on ice until the moment of administration.
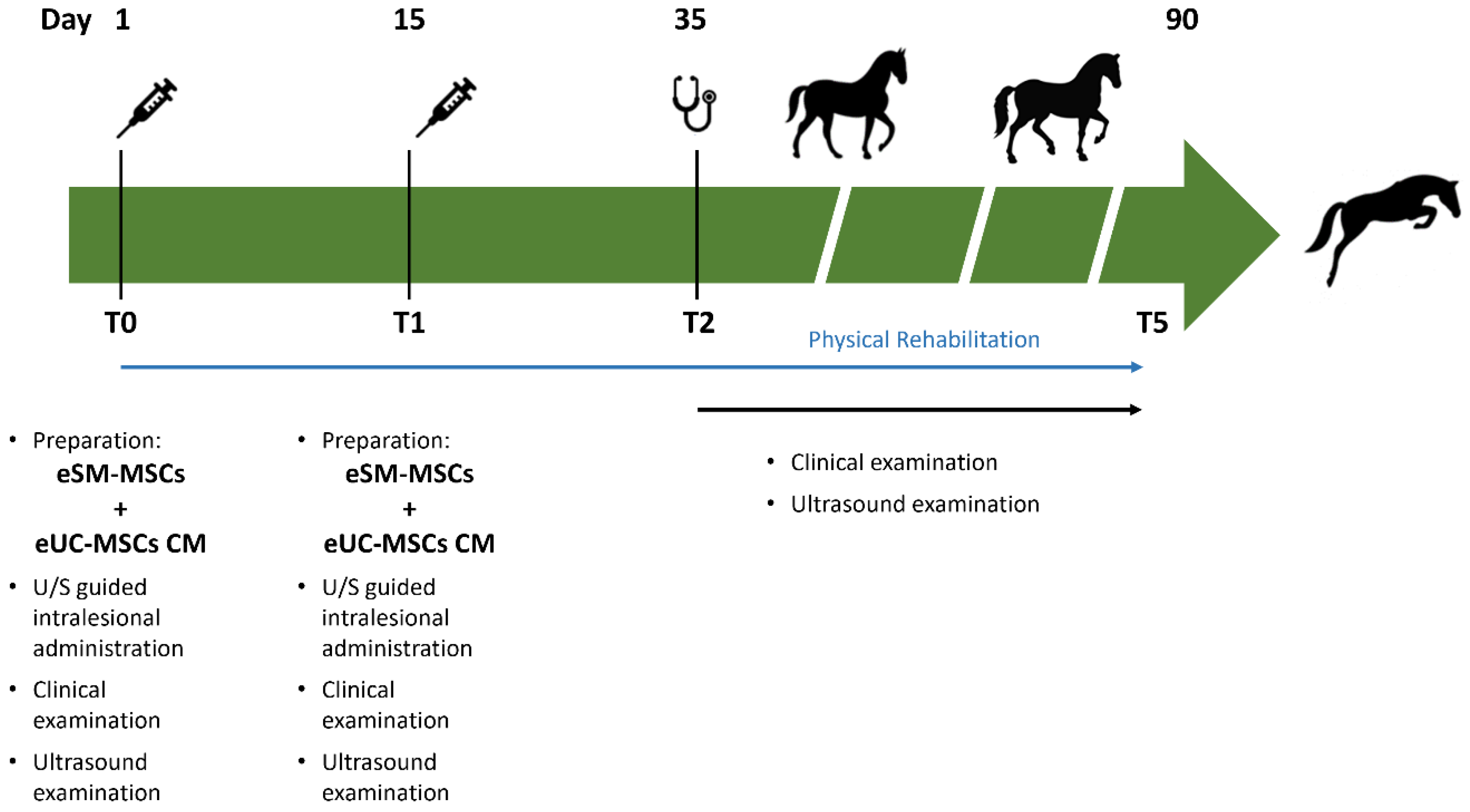
2.10. Treatment Protocol
The injured structure - LMCL - was treated with the mixture of allogenic eSM-MSCs and eUC-MSCs CM. Patient received a single endovenous administration of phenylbutazone (Phenylarthrite®, 2,2 mg/kg, IV) at the end of the treatment. No other medical treatment (including nonsteroidal anti-inflammatory drugs, intra-articular corticosteroids, hyaluronan, glycosaminoglycans, hemoderivative treatments and other MSCs preparations) were administered, except for those described in the treatment protocol, before and after allogenic eSM-MSCs + eUC-MSC CM treatment.
Patient was monitored for 48 hours after treatment and no complication was registered. Following the treatment, patient was assessed periodically to control swelling of the joint, lameness and ultrasonographic changes (echogenicity, cross sectional area and fiber alignment). Corrective asymmetrical shoeing with more support (wider branch) on the medial side was performed – “Denoix asymmetric shoe”.
2.10.1. Intralesional eSM-MSCs + eUC-MSCs CM Administration
Patient was sedated with detomidine (Domosedan®, 0,02 mg/kg, IV), the right tarsus trichotomized and skin was surgically disinfected with chlorohexidine and alcohol. The prepared therapeutic combination was aspired with a 18G needle to a 2 mL syringe and gently homogenized. Ultrasound was used to identify the lesion site, and an ultrasound guided injection with a 20G needle was performed at the lesion site. The stablished protocol included a second eSM-MSCs + eUC-MSCs CM administration 15 days after the first treatment using the same protocol.
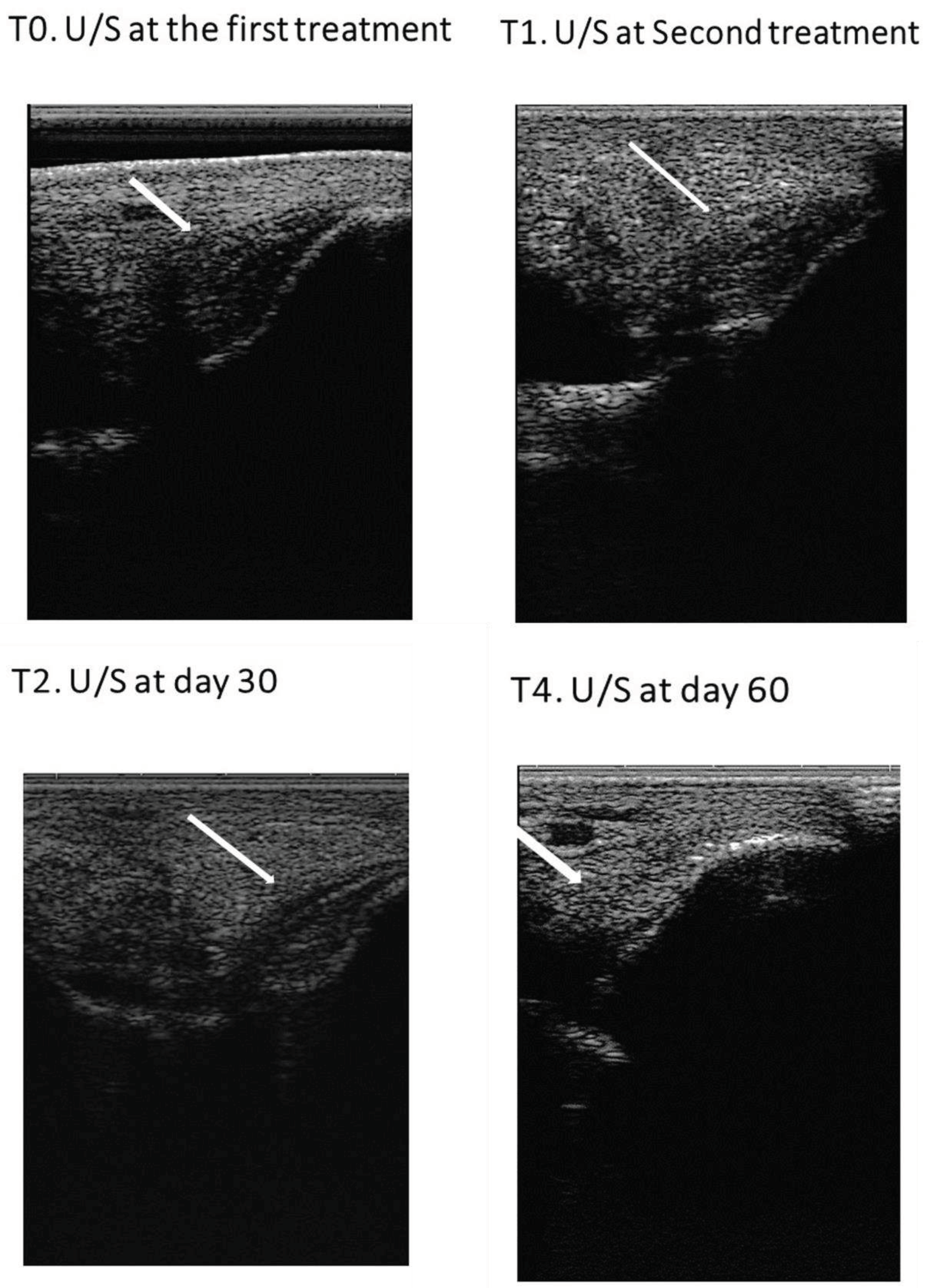
2.11. Post-Treatment Monitoring – Clinical Evaluations
Tissue regeneration was indirectly estimated through lameness evaluation, pain to pressure, limb inflammation, limb sensitivity and ultrasound image. In each assessment, the ultrasonographic exam was performed in transverse and longitudinal scans and three parameters were evaluated: lesion echogenicity, lesion longitudinal fiber alignment (FA) and cross-sectional area. The contralateral healthy limb was used as a control. Ultrasonographic evaluation was performed on assessment day, treatment day (day 1 – T0) and on days 15 (T1 – second administration), 30 (T2), 45 (T3), 60 (T4) and 90 (T5)
post-treatment (
Figure 4).
Rehabilitation program consisted of an exercise-controlled program including stall confinement and a regular and increasing time exercise, as presented on
Table 2 [
1,
44,
45,
46,
47]. Exercise was early initiated, at the second day after treatment, with low level movements – hand walking. Early movements should include weight-bearing, strengthening and flexibility activities, whereas stall rest alone should be used as infrequently as possible [
45].
After eSM-MSCs + eUC-MSCs CM treatment, patient underwent a rehabilitation program consisting of two days of box rest followed by 13 days of 10 minutes hand-walk. Bandage applied on treatment day was removed 24h after treatment. At day 15 the second treatment was performed followed by the same 15-day rehabilitation program, until day 30. Between day 30 and day 45 the work consisted of 20 min hand-walking, between day 45 and day 60 the work was 30 minutes of hand-walking, between day 60 and day 75, 30 minutes of hand walking plus 5 minutes trot and finally between day 75 and day 90, patient underwent 30 minutes of hand-walking plus 10 minutes of trot.
Veterinary assessment at day 90 (T5) determined if the horse could return to regular work based on clinical recovery (limb sensitivity and lameness evaluation) and ultrasonographic lesion improvement, evidenced by normal echogenicity, good fiber alignment and normal cross-sectional area of the ligament when compared with contralateral limb.
4. Discussion
The state of the art concerning regenerative and biological therapies involves the use of multipotent MSCs and more recently, the resource to its secretion products suggests the combination of the therapeutic advantages of MSCs administration and cell-free approaches emerges as an innovative strategy, with increased therapeutic potential. This concept is currently patented proprietary technology (PCT/IB2019/052006, WO2019175773 – Compositions for use in the treatment of musculoskeletal conditions and methods for producing the same leveraging the synergistic activity of two different types of mesenchymal stromal/ stem cells – Regenera®).
This clinical case report discloses the application of such strategy and details on the evaluation of the synergistic effect of eSM-MSCs and eUC-MSCs populations in the treatment of an equine ligament desmitis, utilizing the cells themselves and cell-derived secretome, respectively.
Equine SM-MSCs and UC-MSCs are an interesting subject for those who study cellular and cell-based therapies due to their promising ability to promote tissue regeneration with high capacity of regeneration of articular structures, tendon and ligaments. Their osteogenic, myogenic and tenogenic superiority, suggests these as good candidates for efforts to regenerate musculoskeletal tissues, as evidenced [
48,
49] and previously reported by the research group [
43]. Additionally, the evaluation of each secretome is important to understand biological potential and their synergistic action with other cell sources.
The latest studies highlight the importance of paracrine action of MSCs through the release of soluble and non-soluble factors, primarily secreted in the extracellular space by MSCs – secretome [
29]. Secretome paracrine signaling can be considered as the primary mechanism by which MSCs contribute to healing processes, becoming their study an interesting subject [
50,
51].
Mocchi et al, agreed that secretome is assuming the center of a new potential therapeutic strategy in different diseases [
29,
52]. Avoiding the need of living cell implantation, secretome presents itself as a big promise as a pharmaceutical product suitable for regenerative medicine [
53,
54].
Equine SM-MSCs secrete high levels of KC/GRO, MCP-1, Il-6, FGF-2, G-CSF, GM-CSF and IL-8 , as previously described [
43]. This profile supports their reported benefits in fibroblast intense activity (KC/GRO) and lesion reperfusion (MCP-1), both essential to successful completion of musculoskeletal tissue after ischemic injury [
55]. The production of FGF-2 is also significant and recognized for proliferation of tenogenic stem cells, enhancing cell proliferation and collagen production [
56]. Other factors such as G-CSF and GM-CSF also depict potential as skeletal muscle repair mediator, including those with pro-inflammatory functions [
57,
58]. Pro-inflammatory factors such as those found at these cells secretome (GM-CSF, G-CSF, Il-6, IL-8 and IL-17), are frequently regarded as deleterious, however they are involved in damage signaling and subsequent activation of resident tendon cells for effective healing, stimulating tendon cell proliferation [
59,
60].
The current analysis focused on the secretion of IL-6 and IL-8 by the eUC-MSCs as complement to the eSM-MSCs activity, due to their known activity in tissue regeneration. Interleukin-6 bares pro-inflammatory and angiogenic functions, capable of increasing the expression of other growth factors (GF). Immunosuppressive properties are also described, which may be prime motors for the success of allogenic MSC implantation [
61,
62]. This pro-inflammatory nature is associated with the induction of acute-phase proteins, inducing a potent regeneration of various tissues such as liver, kidney, neural tissues and others, supporting their potential as a therapeutic approach for regenerative medicine [
63,
64].
Previous studies have likewise demonstrated IL-6 is a potent anti-inflammatory cytokine significantly up-regulated in injured tendons [
65]. This cytokine has been demonstrated to have an important role in regulating tendon-derived stem cells (TDSC) activity and differentiation, however inhibiting their tenogenic differentiation,
in vitro [
66], while in an
in vivo model (IL-6 −/− mice), it was demonstrated to be involved in the complex mechanisms that contribute to mechanical and organizational properties of injured tendons [
67].
Another
in vivo study demonstrated that human Achilles tendon presented high levels of various growth factors after exercise. From these, IL-6 was present in the largest amount, suggesting this cytokine was responsible of transforming collagen under biomechanical stimulation. An experimental infusion of IL-6 in the peritendinous tissue followed by exercise suggested this IL stimulates collagen synthesis, corroborating the hypothesis that IL-6 is an important growth factor of the connective tissue in healthy human tendons[
68].
These observations suggest IL-6 has an important role in tendon regeneration, despite the need for further research to more accurately understand IL-6 real role in vivo.
Interleukin-8 is also a recognized pro-inflammatory mediator and a potent angiogenic factor associated with increase in vascular endothelial growth factor (VEGF) concentration. Interleukin-8 was directly related to VEGF stimulation helping revascularization and ligamentization of a grafted tendon [
69]. Interleukin-8 has a similar effect to IL-6 but has a longer half-life [
70].
Up-regulation of both IL-6 and IL-8 is consistent with tissues healing and its inflammatory phase. A study with human Achilles tendon presented that IL-6, IL-8 and IL-10 were upregulated in a tendon healing phase with absence of inflammation, indicating that these cytokines may be associated with anti-inflammatory and regenerative activity on tendon healing process [
65].
Herein, the
in vitro production of these bioactive molecules by the MSCs populations under study was addressed, suggesting diverse biological potential of both cell types for immunomodulative and regenerative therapy, magnifying their potential benefits, confirming its immunosuppressive, angiogenic and pro-inflammatory profile, thus validating their complementarity and synergistic activity in anti-inflammatory and regenerative events as stated before [
71].
The presence of MSCs derived secretome, in the form of conditioned medium, represents therefore a new class of therapeutics with broad application for the treatment of disease and injury and a differentiating element in this therapeutic application. The influence of fibroblastic proliferation, angiogenic stimulation and development of mature vascular structures who provide a wide variety of GF, accomplishes not only lesion repair with regenerated tissue but also strengthening of the entire ligament, reducing the risk of lesion recurrence [79].
To sum up, eSM-MSCs and eUC-MSCs secretome factors are able to promote tendon/ligament healing by stimulating reperfusion, reactivating growth programs, reducing inflammation and fatty infiltration, stimulating cell proliferation, collagen production and tenogenic differentiation [
72].
The existence of a cell and secretome bank, whose mediators are very well identified, with recognized benefits in tissue regeneration, becomes clinically very appealing and advantageous. This allows early medical intervention in acute cases, with prompt procedures, promoting tissue regeneration, enabling a better functional outcome and a rapid and sustainable return to sportive career.
Cells allogeneic nature is a key factor in this clinical case and in this therapeutic product, because they are available for ready to use application. No adverse or rejection reactions were observed, further supporting their potential as alternatives to autologous therapies, which bare relevant drawbacks to their widespread application, such as the health status of the source tissue donor (and its impact in their regenerative performance) and the time required for tissue processing and therapeutic dosage production. The allogeneic approach enables a curated selection of tissue donors, as well as the production and validation of both MSCs and secretome, which can be stored and be readily available for acute application in the event of injury.
Once substantiated the therapeutic potential of the combination eSM-MSCs and eUC-MSCs CM for the treatment of tendinopathies and desmopathies, the approach presented suitable for the application in the tarsus medial ligament lesion reported.
Tarsus medial collateral ligament lesions are the most prevalent, being the long ligament the most affected. Occasionally lesions of multiple CLs have been found [
12,
73]. Rotational forces beyond the normal range of joint motion occurring during tight turns or forced asymmetrical movements, causing abnormal hock extension, increasing strain on the CLs being a main cause of this type of lesion Usually CL injuries present themselves as acute lameness with tibiotarsic joint effusion and therefore should be included in the differential diagnosis of the swollen hock [
4]. As stated by,
Sherlock et al, 2011, prognosis for medial tarsal collateral ligament desmitis appears good for survival but fair for return to previous levels of performance and requires prolonged periods of rest and a controlled exercise program [
9]. Conventional treatments present high percentages of recurrence and lameness is often present. Another study presents the treatment of this type of lesion with Platelet rich plasma (PRPs), achieving a return to the same level work in 180 days, in 81% of the horses [
26].
In the presented case, the therapeutic combination of eSM-MSC and eUC-MSC CM was considered successful as is registered a return to full work in 90 days, reducing in 50% the time to return to full work when compared with other therapies in the same type of lesion. The physical and orthopedic outcome of the patient, as well as the ultrasonographic recovery of the ligament was considered complete at day 60 (T4). The horse presented no lameness (Score 0/0, AAEP Lameness Score). Lameness evaluation is a clinically relevant marker of orthopedic injury improvement and was used as our primary outcome as severe lesions in tendons, ligaments, and joints present with lameness as the main clinical sign. In opposition to reference literature descriptions, in the present case there was a significative reduce in required rest period. This is a great attainment comparing with recovery times described in literature concerning equine clinical trials of desmitis of collateral ligament of tarsus and equine tendonitis [
8,
9,
13,
23,
74,
75] – in 2 days the horse started rehabilitation program
versus 30 days to 180 days of rest [
10] and return to full work after 90 days versus 180 days presented in other studies - reduction in 50% of time recovery [
26,
76]. In 30 days the ligaments cross-sectional area returned to normal size, good fiber alignment and echogenicity was achieved
versus 30-120 days usually described, a recovery that might represent up to 75% of U/S recovery time [
8,
10]. It must be highlighted that, in the majority of cases, only scar tissue repair occurs and regeneration is never accomplished with conventional treatments. At day 45 (T3) there was an impressive ultrasonographic recovery and at day 60 (T4) a successful ligament recovery, with no signs of scar tissue, good fiber alignment and echogenicity was achieved. Only a slight distension of the right tarsus was, and remains, perceptible comparing with contralateral limb. After rehabilitation program, the patient returned to the same physical work and even exceed the previous performance level. In fact, currently, the animal is competing on a higher level. The absence of lesion relapse 18 months after injury is also noteworthy.
The clinical re-evaluations determined a fast, efficient and very successful clinical recovery.
In a “One-health” perspective, the health of animals and human coexist in a coherent system. Thus, the possibility of translational results from equine to human musculoskeletal pathologies is very important as equines play an important role as model for human musculoskeletal disorders, given the high level of anatomic and physiologic analogy between equine and human structures [87,88]. Preclinical studies using equine models of orthopedic disorders are adequate to screen potential procedures for human clinical use, as methods of assessing putative repair techniques have not been developed in vitro [89,90].
From an ethical perspective, it is also significant to state that, in the particular context of orthopedic research, many studies can be conducted in naturally occurring disease (without premeditated disease induction) and that the horse often poses as both model as well as final beneficiary of the developed therapies, alleviating the ethical burden of such studies.
Author Contributions
Conceptualization, I.L.R, B.L, P.S, I.B., L.M.A, J.M.S, and A.C.M.; methodology, I.L.R, B.L, P.S, A.C.S., M.V.B, A.R.C, B.P, R.D.A, J.M.S and A.C.M; software, I.L.R, A.C.S., M.V.B, R.D.A and J.M.S.; validation, I.L.R, A.C.S, R.D.A. M.V.B., B.L, P.S, A.R, A.R.C, L.M.A, B.P, J.M.S, A.C.M.; formal analysis, I.L.R.; investigation, I.L.R, B.L, P.S, A.C.S., M.V.B, A.R.C, A.R, L.M.A, B.P, I.B., R.D.A, J.M.S, and A.C.M.; re-sources, R.D.A., J.M.S and A.C.M; data curation, I.L.R, P.S, B.L .; writing—original draft preparation, I.R.L, B.L, P.S, .; writing—review and editing, I.L.R, B.L, P.S. L.M.A., C.M.M., I.B. ; visualization, I.R.L, B.L, P.S, A.C.S, M.V.B, A.R.C, A.R, L.M.A, R.D.A, J.M.S and A.C.M.; supervision, R.D.A., C.M.M., L.M.A, J.M.S and A.C.M; project administration, A.C.M..; funding acquisition, R.D.A. and A.C.M. All authors reviewed the final work and approved its submission. All authors agreed to be personally accountable for the author’s own contributions and for ensuring that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and documented in the literature. All authors have read and agreed to the published version of the manuscript.
Figure 1.
Anatomy of medial aspect of right tarsocrural joint. This image evidences the complexity of the tarsocrural joint structures. Long medial collateral ligament is highlighted in soft green.
Figure 1.
Anatomy of medial aspect of right tarsocrural joint. This image evidences the complexity of the tarsocrural joint structures. Long medial collateral ligament is highlighted in soft green.
Figure 2.
Secretome. Multipotent Mesenchymal Stem/ Stromal Cells release a variety of factors, -soluble and -non soluble in the microenvironment which modulate the biology and tissue response of the cells, such as cytokines, chemokines, growth factors and extracellular vesicles.
Figure 2.
Secretome. Multipotent Mesenchymal Stem/ Stromal Cells release a variety of factors, -soluble and -non soluble in the microenvironment which modulate the biology and tissue response of the cells, such as cytokines, chemokines, growth factors and extracellular vesicles.
Figure 3.
Horse clinical inspection. Evidence of increased volume of the right tarsocrural joint. (a) frontal view and (b) medial view.
Figure 3.
Horse clinical inspection. Evidence of increased volume of the right tarsocrural joint. (a) frontal view and (b) medial view.
Figure 4.
Timeline of eSM-MSCs treatment protocol and rehabilitation program. T0 is the day of the first treatment with the administration of eSM-MSCs + eUC-MSCs CM combination. Beside the intralesional application of the therapeutic combination, a clinical and ultrasound examinations were also performed. T1 refers to the second application of the composition 15 days after T0, when the same procedure was repeated. On the other assessment days – T2, T3, T4 and T5, a clinical and ultrasound examination were performed. At the same time, a physical rehabilitation plan was carried out.
Figure 4.
Timeline of eSM-MSCs treatment protocol and rehabilitation program. T0 is the day of the first treatment with the administration of eSM-MSCs + eUC-MSCs CM combination. Beside the intralesional application of the therapeutic combination, a clinical and ultrasound examinations were also performed. T1 refers to the second application of the composition 15 days after T0, when the same procedure was repeated. On the other assessment days – T2, T3, T4 and T5, a clinical and ultrasound examination were performed. At the same time, a physical rehabilitation plan was carried out.
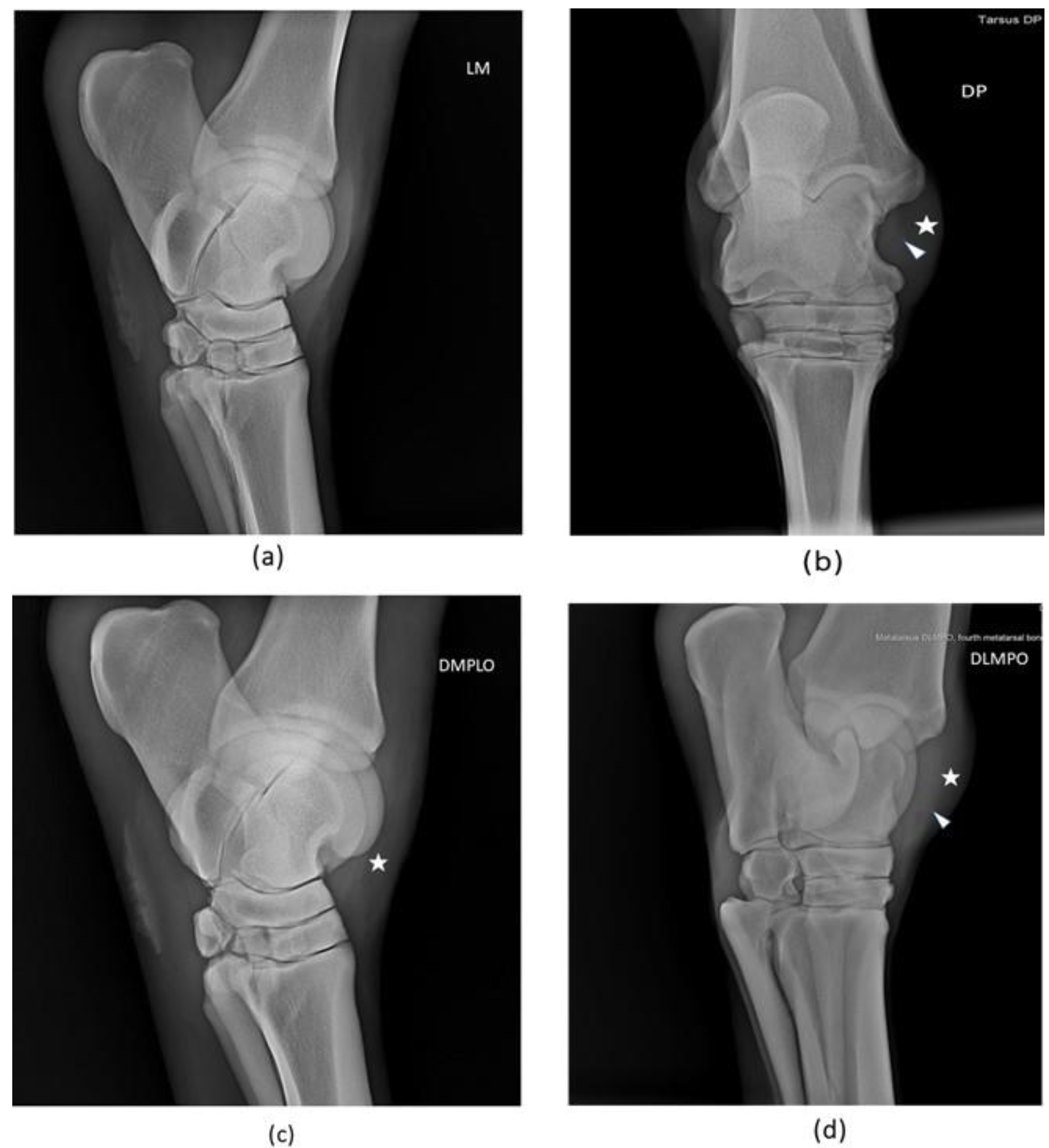
Figure 5.
Radiographic views of patient right tarsus: (a) Lateromedial (LM), (b) Dorsoplantar (DP), (c) Oblique dorsomedial-plantarolateral (DMPLO), (d) Oblique dorsolateral-plantaromedial (DLPMO). The white head of the arrow (△) points to increased radiopacity of the long medial collateral ligament and the star (*) signals soft tissue swelling and joint distension. There are no significant radiological alterations of articular surfaces.
Figure 5.
Radiographic views of patient right tarsus: (a) Lateromedial (LM), (b) Dorsoplantar (DP), (c) Oblique dorsomedial-plantarolateral (DMPLO), (d) Oblique dorsolateral-plantaromedial (DLPMO). The white head of the arrow (△) points to increased radiopacity of the long medial collateral ligament and the star (*) signals soft tissue swelling and joint distension. There are no significant radiological alterations of articular surfaces.
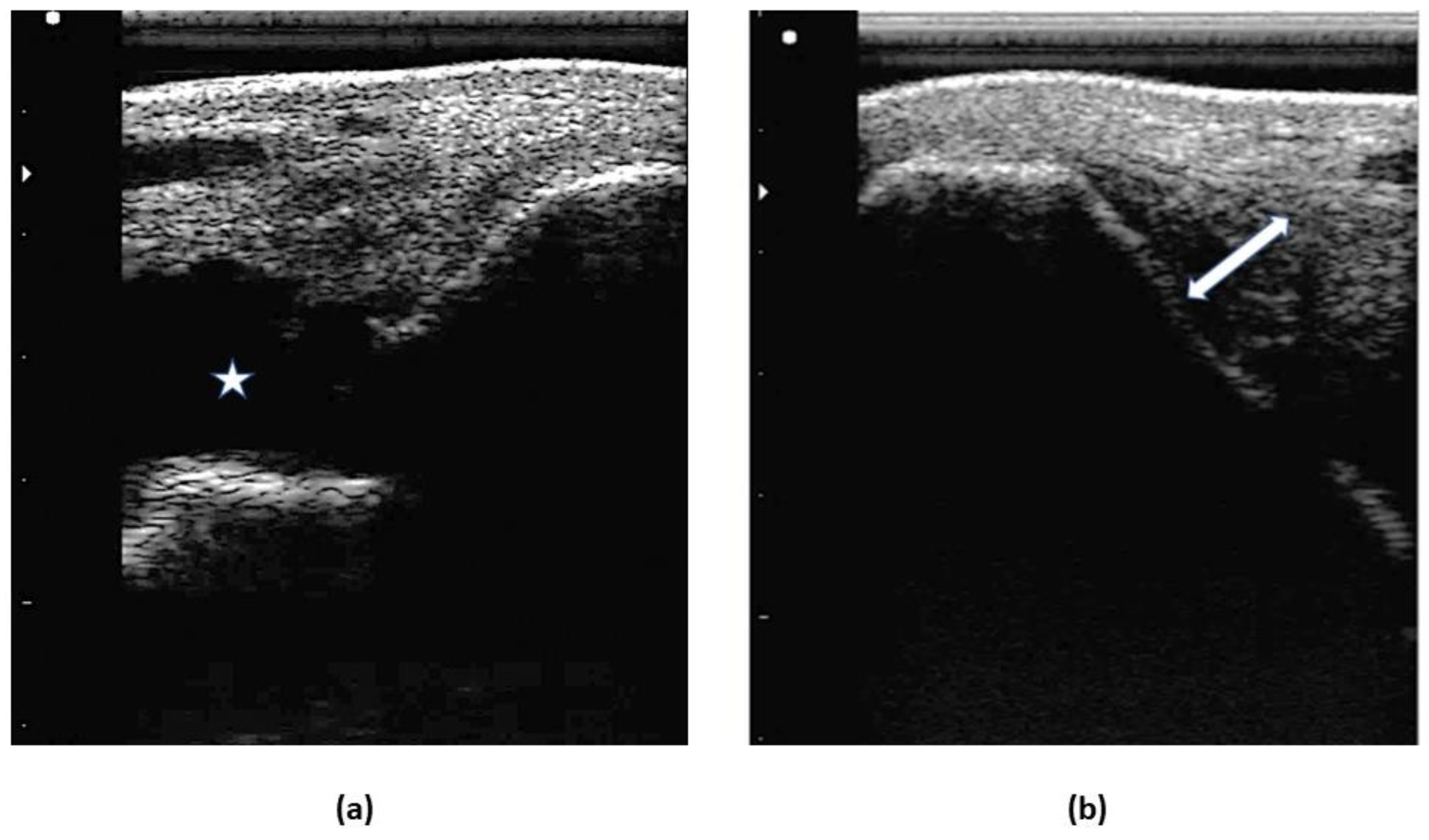
Figure 6.
Images of the first ultrasonographic exam. Desmitis of LMCL insertion at the medial malleolus: (a) increased amount of hypoechoic fluid within the joint, signaled with the star (*) (b) disruption of the fibers at the insertion, signaled with the double arrow (↔).
Figure 6.
Images of the first ultrasonographic exam. Desmitis of LMCL insertion at the medial malleolus: (a) increased amount of hypoechoic fluid within the joint, signaled with the star (*) (b) disruption of the fibers at the insertion, signaled with the double arrow (↔).
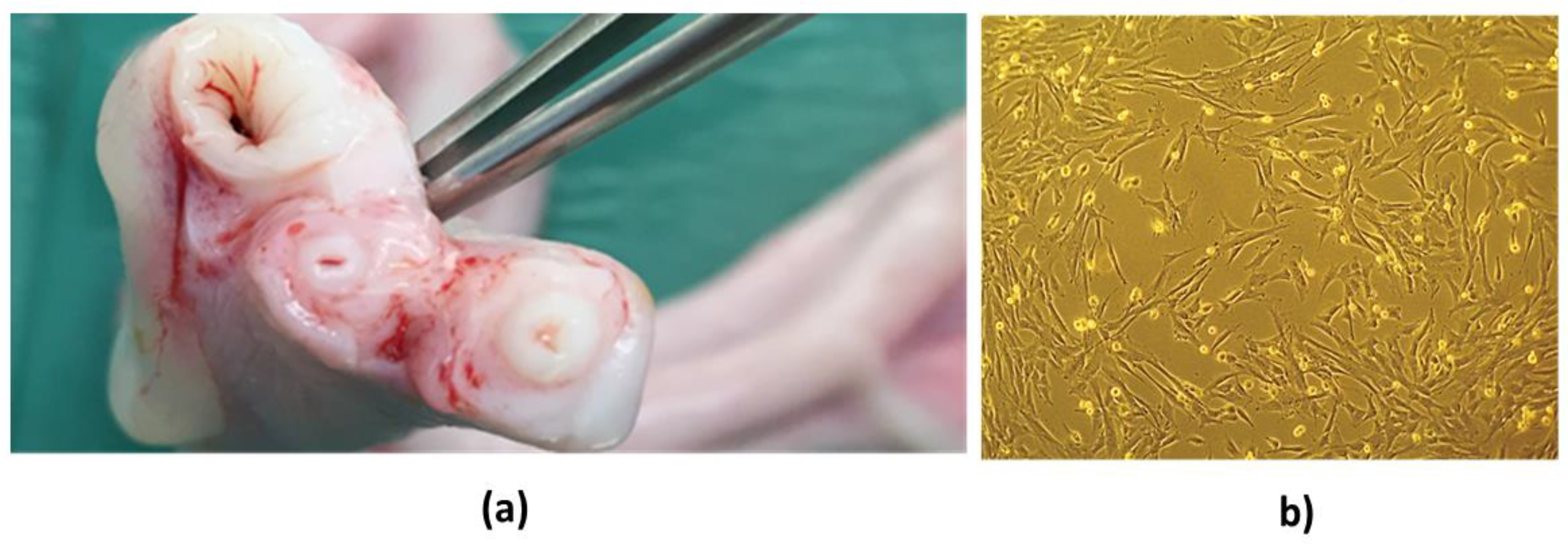
Figure 7.
Isolation of MSC from equine umbilical cord tissue. (a) Umbilical cord tissue. (b) Isolated population of eUC-MSCs at P3 – plastic adhesion, monolayer, and fibroblast-like shape of eUC- MSCs may be observed.
Figure 7.
Isolation of MSC from equine umbilical cord tissue. (a) Umbilical cord tissue. (b) Isolated population of eUC-MSCs at P3 – plastic adhesion, monolayer, and fibroblast-like shape of eUC- MSCs may be observed.
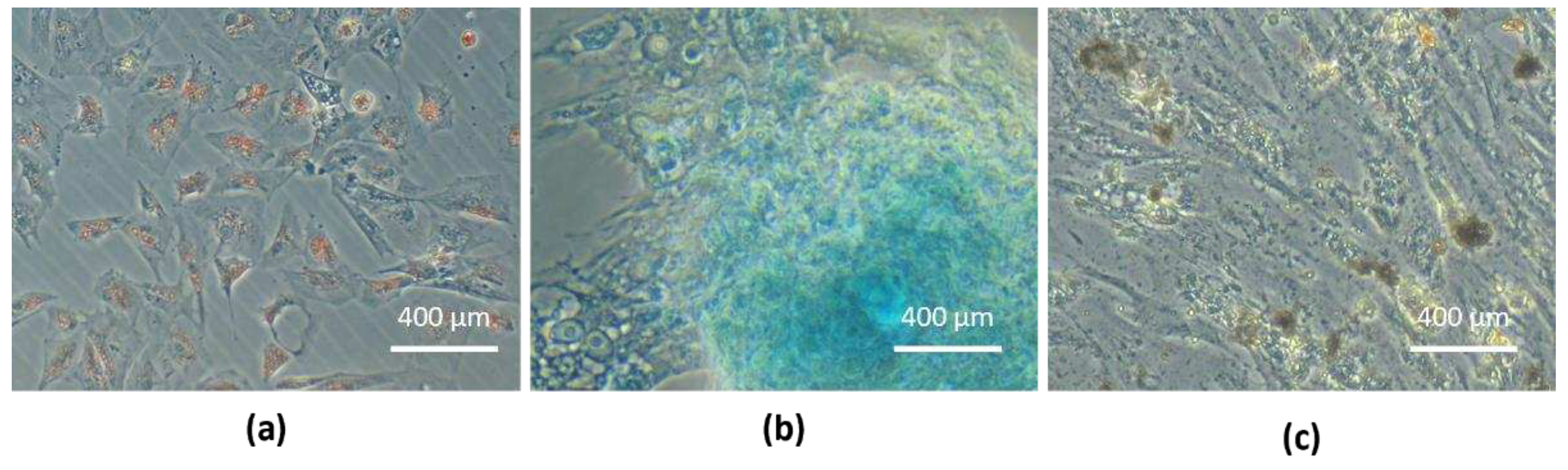
Figure 8.
Tri-lineage differentiation: (a) eUC-MSCs adipogenic differentiation, cytoplasmatic lipid vacuoles stained in red (Oil Red O staining); (b) eUC-MSCs chondrogenic differentiation, proteoglycans in extracellular matrix stained in blue (Alcian Blue staining); (c) eUC-MSCs osteogenic differentiation, extracellular phosphate deposits stained in brown (Von Kossa staining).
Figure 8.
Tri-lineage differentiation: (a) eUC-MSCs adipogenic differentiation, cytoplasmatic lipid vacuoles stained in red (Oil Red O staining); (b) eUC-MSCs chondrogenic differentiation, proteoglycans in extracellular matrix stained in blue (Alcian Blue staining); (c) eUC-MSCs osteogenic differentiation, extracellular phosphate deposits stained in brown (Von Kossa staining).
Figure 10.
Bioactive molecules in secretome – IL-6 and IL-8: Differences of production by eSM-MSCs and eUC-MSCs. Results presented as (mean ± SEM). * Corresponds to 0.01 ≤ p < 0.05, ** to 0.001 ≤ p < 0.01, *** to 0.0001 ≤ p < 0.001, and **** to p < 0.0001.
Figure 10.
Bioactive molecules in secretome – IL-6 and IL-8: Differences of production by eSM-MSCs and eUC-MSCs. Results presented as (mean ± SEM). * Corresponds to 0.01 ≤ p < 0.05, ** to 0.001 ≤ p < 0.01, *** to 0.0001 ≤ p < 0.001, and **** to p < 0.0001.
Figure 11.
Images of ultrasonographic follow-up. (a) Day 1 (T0), (b) day 15 (T1), (c) day 30 (T2) and (d) day 60 (T3). Indicators of ligamentar regeneration: increased echogenicity and fiber alignment, decrease of cross-sectional area and synovial fluid accumulation within the joint space.
Figure 11.
Images of ultrasonographic follow-up. (a) Day 1 (T0), (b) day 15 (T1), (c) day 30 (T2) and (d) day 60 (T3). Indicators of ligamentar regeneration: increased echogenicity and fiber alignment, decrease of cross-sectional area and synovial fluid accumulation within the joint space.
Table 1.
Score systems used to assess lameness and response to flexion test [
42].
Table 1.
Score systems used to assess lameness and response to flexion test [
42].
| Parameter |
Score |
Clinical implication |
| AAEP Grading |
0 |
No Lameness |
| 1 |
Lameness not consistent |
| 2 |
Lameness consistent under certain circumstances |
| 3 |
Lameness consistently observable on a straight line. |
| 4 |
Obvious lameness at walk: marked nodding or shortened stride |
| 5 |
Minimal weight bearing lameness in motion or at rest |
| Flexion Test |
0 |
No flexion response |
| 1 |
Mild flexion response |
| 2 |
Moderate flexion response |
| 3 |
Severe flexion response |
Table 2.
Physical rehabilitation program.
Table 2.
Physical rehabilitation program.
| Week |
Exercise |
| 0-2 |
2 days: stall confinement
Handwalk: 10 min
Day 15: new treatment |
| 3-4 |
2 days: stall confinement
Handwalk: 10 min
VET-CHECK + U/S |
| 5 |
Handwalk: 15 min |
| 6 |
Handwalk: 20 min
VET-CHECK + U/S |
| 7 |
Handwalk: 25 min |
| 8 |
Handwalk: 30 min
VET-CHECK + U/S |
| 9-10 |
Handwalk: 30 min + 5 min trot |
| 11-12 |
Handwalk: 30 min + 10 min trot
VET-CHECK + U/S |