1. Introduction
Tuberculosis (TB) is the leading cause of death worldwide. In 2021 the World Health Organization (WHO) estimated that around 10.6 million people worldwide fell sick with TB, a 4.5% increase from 2020 [
1]. Indonesia has the second-highest global TB caseload, with a TB incidence in 2020 of 301 per 100,000 population, and a mortality rate of 34 per 100 thousand people [
2].
One essential pillar of the WHO’s End TB strategy is early diagnosis and treatment [
3]. Unfortunately, many countries rely on passive case finding, in which only those who seek care at health facilities are examined for TB [
4,
5]. As a result, many cases are missed, particularly in people who are asymptomatic, have mild symptoms or do not seek treatment at health facilities. This can lead to continuing transmission, worsening of the patient’s condition, and even death [
5].
Active case finding (ACF) is an important method of finding and diagnosing TB cases that may be missed by passive case finding. ACF involves systematic screening for active TB outside health facilities in high-risk populations, such as those living in congregate settings [
6]. Several studies have shown that ACF can increase the number of reported cases and reduce the prevalence of TB in the community [
6]. However, a recent systematic review found inconsistent results and low-quality evidence for the benefit of active case finding on incidence and prevalence. For example, randomised control trials (RCT) utilising community mobilisation and sputum drop-off in South Africa did not affect TB prevalence, whereas an RCT in Vietnam utilising door-to-door sputum testing for everyone significantly reduced TB prevalence [
7]. Nevertheless, the review concluded that ACF might effectively change TB epidemiology if it is designed for specific settings and delivered with high coverage. However, this highlights the need for further evaluations of ACF programs in different settings incorporating alternate delivery methods and diagnostic strategies [
7].
ACF activities are highly recommended in high burden countries such as Indonesia and may help to reduce underdiagnosis of TB [
4]. The WHO consolidated guidelines on systematic screening also recommend that systematic screening should be conducted among household contacts of TB patients, people living with HIV, and general population in areas with estimated TB prevalence 0.5% or higher [10]. In Indonesia, there are gaps in case detection and reporting: a TB inventory study in Indonesia in 2017 found that 44 % of TB cases had not been reported, and 30.4% had not been detected [
8]. Case detection has been further impacted by the COVID-19 pandemic, resulting in fewer cases reported [
1]. Comprehensive TB services incorporating ACF — including symptom screening and diagnostic testing — have not been widely implemented, described, or evaluated in Indonesia [
9].
Zero TB Yogyakarta (ZTBY) is a collaborative project between the Center for Tropical Medicine Universitas Gadjah Mada, the health offices of Yogyakarta Province, Kulon Progo District and Yogyakarta City, and the Burnet Institute, Melbourne. The ZTBY project conducted TB ACF in Kulon Progo Regency and Yogyakarta City from 2020 and expanded to additional districts in 2022. ZTBY active case finding screens for TB among target groups using symptom screening and mobile chest X-ray (a vehicle equipped with an X-ray device), with microbiological testing for those who screen positive. The groups targeted by the ACF have included residents of low socio-economic areas, household contacts of TB patients, people living with HIV (PLHIV), residents in prisons, residents of orphanages, Islamic boarding schools, healthcare workers, and those living in areas with high TB cases [11]. To date, the impact of the ACF service on local case notifications and populations reached has not been evaluated.
This study compares TB cases found through passive and active-case finding in the Kulon Progo District in 2021. This comparison can provide valuable insights to help us understand which case-finding strategies are most effective to detect TB cases and what needs to be done in order to improve the current TB management systems in the region.
2. Materials and Methods
This study is a retrospective review of TB case notification data. The population in this study were TB cases notified in Kulon Progo District between 1 January and 31 December 2021. It includes persons with TB found through routine case finding and those found from active-case finding activities implemented by the Zero TB Yogyakarta program.
2.1. Setting
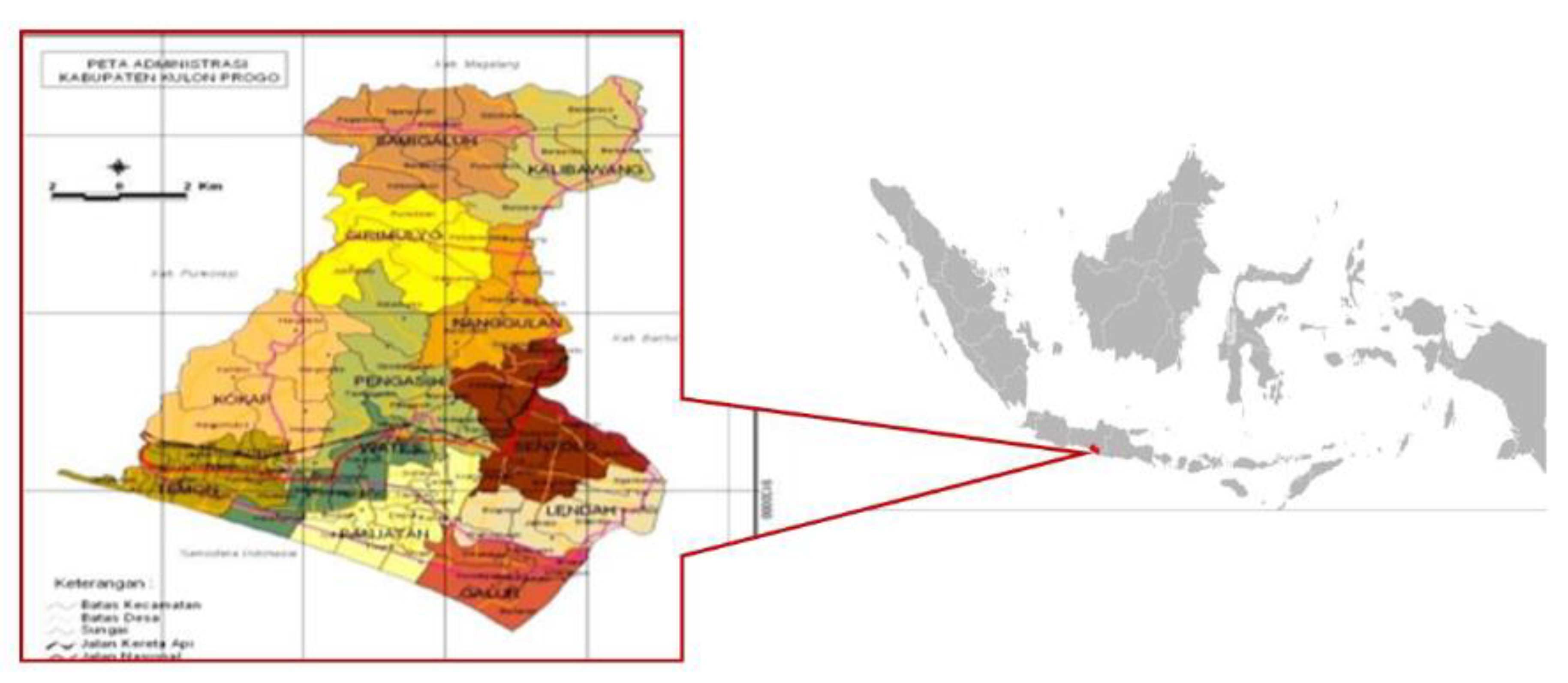
Kulon Progo District is a rural district in Yogyakarta Province, with an area of 586.28 km2. The total population is 443,283 people spread over 12 sub-districts, 87 villages and 917 sub villages [12] (Figure 3). Of the total population, 49% are men, and 51% are women. The proportion of the working-age population (15 – 64 years) is 67.8%. There are 21 primary healthcare centres (puskesmas), two government hospitals and seven private hospitals that provide TB services. There are two puskesmas (Kalibawang and Galur 2) and two hospitals (RSUD Wates, RSUD Nyi Ageng Serang) that can carry out TB microbiological examinations using the GeneXpert platform with Xpert MTB/RIF cartridges [13].
Prior to the commencement of ZTBY activities, TB case finding in Kulon Progo usually consisted of passive case finding in which TB cases were detected among persons seeking care at the health facilities. Additionally, household contacts of TB patients (index cases) were investigated by primary health centres in collaboration with trained local village cadres. Sputum samples were collected from household contacts and tested.
Active case finding in this study is a part of ZTBY activities that involved mobile chest X-ray for TB screenings. ZTBY ACF was conducted in sub villages where TB cases had been found in the last five years. We also targeted groups for screening such as household contacts of TB patients, residents at Islamic boarding schools, orphanages, and people living with HIV. We held multi-sectoral meetings with puskesmas, local governments, cadres, and community leaders two weeks before conducting in ACF in a locale. These meetings were used to explain the ACF activity to key stakeholders and discuss their concerns and potential challenges in conducting ACF. These stakeholders were then asked to invite the target population.
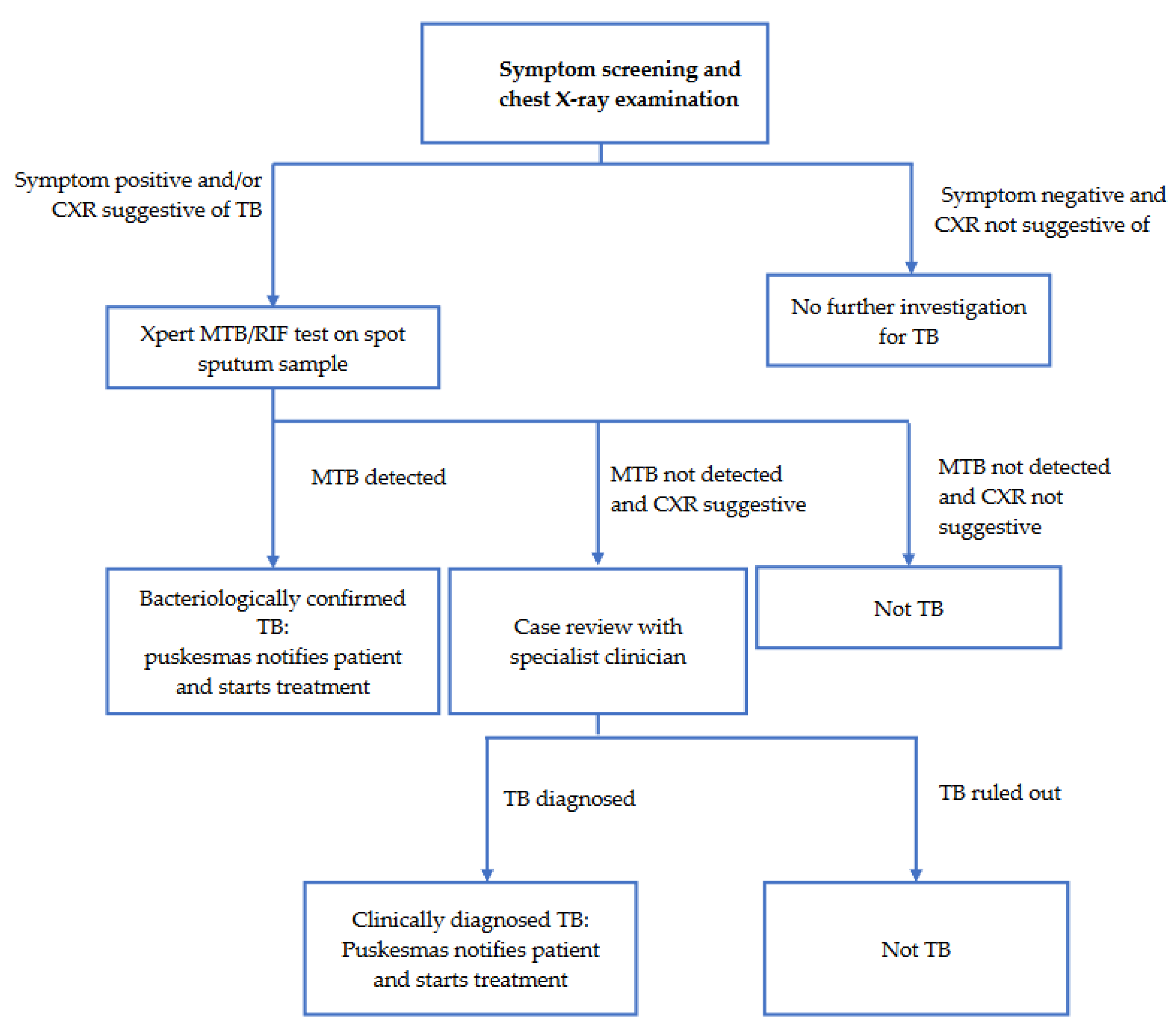
The ACF service was set up at sites within or proximal to the target village. The specific site for setting up the mobile ACF service was chosen based on its accessibility to the target population. People presenting to the ACF service were registered, checked for TB symptoms and had a chest x-ray examination performed. From January to April 2021, the x-ray results were read by a doctor within the ACF team. In May 2021, the ACF service commenced using qXR software (qure.AI, India) for computer-assisted X-ray interpretation. Participants with TB symptoms or a chest x-ray suggestive of TB (based on the doctor’s interpretation or a qXR score > 0.5) were asked to produce a single spot sputum sample on site. Spot sputum samples were then transported to a laboratory for testing with GeneXpert MTB/RIF test. The puskesmas whose catchment covered the target village then entered the data of persons with presumptive TB in the SITB (Sistem Informasi Tuberkulosis – Indonesia’s national case-based electronic TB surveillance system). The laboratory performing the test was then expected to update the SITB with the test results. If the GeneXpert test results were positive, the puskesmas informed the patient. If the geneXpert result was negative but the CXR was suggestive of TB, the puskesmas doctor in coordination with the ACF team consulted with clinician specialists to diagnose or rule out clinical TB. All patients with TB diagnosis, both bacteriological and clinical were invited to start treatment at their nearest puskesmas. The puskesmas was responsible for notifying bacteriological and clinical TB diagnoses and cases started on treatment in the SITB.
Figure 1 shows the screening and diagnostic algorithm for ZTBY ACF.
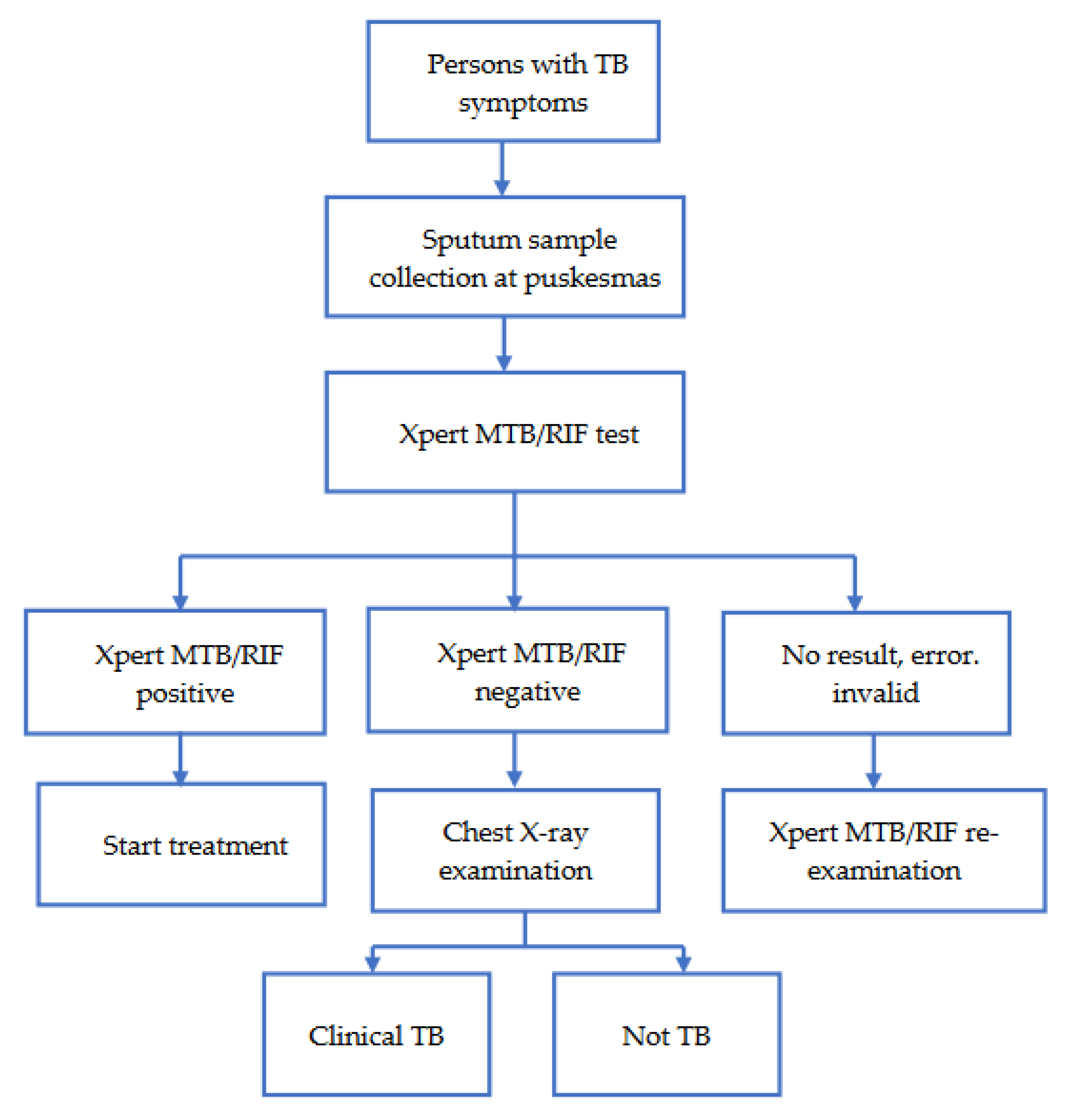
In passive-case finding, patients presenting to the puskesmas with TB symptoms were investigated for TB. These patients were asked to produce an early morning sputum sample to be tested with a GeneXpert MTB/RIF test. The patients were recorded in SITB once the sputum samples were collected and transported to the laboratory. If the test result was positive, puskesmas invited the patient to start treatment. If the result was negative, the puskesmas referred the patient for chest x-ray examination and used the chest x-ray to help decide if the patient had clinical TB or not. The puskesmas was responsible for reporting on diagnosis and treatment initiation of bacteriological and clinical cases in the SITB.
Figure 2 shows the PCF algorithm.
2.2. Data collection and analysis
This study utilised secondary data collected in 2021 from the Sistem Informasi Tuberkulosis (SITB) in Kulon Progo and Zero TB Yogyakarta’s REDCap database. The SITB is the Indonesian Ministry of Health’s case-based digital TB surveillance system. Health facilities such as hospitals, puskesmas, clinics, laboratories, and pharmacy installations, are required to use the platform to manage and report TB cases in Indonesia. REDCap (Research Electronic Data Capture) is a secure, web-based software platform that supports data capture for research studies [14,15]. Zero TB Yogyakarta collected demographic and clinical data on persons presenting to its services. The clinical data included microbiological, radiological and diagnosis, which was collected using REDCap electronic data capture tools on a server hosted by the Universitas Gadjah Mada.
Persons undergoing microbiological investigation and starting TB treatment are meant to be entered in the SITB, regardless of whether they were initially screened from passive or active case finding. A national identification number (NIK) is recorded in the SITB and in the ZTBY REDCap data. The NIK was used to link the ZTBY REDCap data with the SITB data. After linkage, identifiable data was removed from the dataset and the data were analysed using Stata version 17. Patients were considered to have been found through ACF if they were in the ZTBY REDCap data. Patients were considered to be found through ACF and notified in SITB if the NIK in SITB matched an NIK in ZTBY REDCap. Patients were considered as found through PCF if they were notified in the SITB and were not matched with an NIK in ZTBY REDCap. Categorical variables were analysed by frequency and proportion.
2.3. Ethical approval
Ethics approval was obtained from The Medical and Health Research Ethics Committee (MHREC), Faculty of Medicine, Public Health and Nursing Universitas Gadjah Mada.
3. Results
Between 1 January and 31 December 2021
, a total of 255 TB cases were diagnosed in Kulon Progo, of which 106 (41.6%) were bacteriologically confirmed (
Table 1). The TB patients’ ages ranged from 0 to 85 years (mean 46.3, SD 21.4) (
Table 1). Most cases were people aged 16-60 (63.5%, 162/255) and male (58.8%, 150/255) (
Table 1). The proportion of clinical TB diagnoses among cases found from active-case finding was 74.7% (68/91) while the proportion among passive-case finding was 49.4% (81/164) (
Table 1). Active-case finding contributed 91 (35.7%) TB cases to the total cases detected in Kulon Progo in 2021 (
Table 1).
ZTB ACF screened 12,406 participants in 2021 and 12,019 (96.8%, 12,019/12,406) of them underwent chest X-ray. Those with symptoms or a chest X-ray result suggestive of TB (12.2%, 1,514/12,406) had their sputum taken for Xpert MTB/RIF rapid molecular diagnostic testing. There were 23 (0.18%, 23/12,406) ACF participants who had a bacteriologically confirmed diagnosis of TB on GeneXpert testing, and there were 68 (0.54%, 68/12,406) ACF participants diagnosed with TB clinically.
There were 42 cases from active case finding that were not found in the SITB data. Of these, 33 (78.6%) were recorded in the ZTBY REDCap database as having started TB treatment. Most of the cases from ACF that were unreported in the SITB were clinically diagnosed with TB (78.6%, 33/42) (
Table 2).
4. Discussion
In this study examining 2021 TB notification data from Kulon Progo district in Indonesia, three key findings were made: 1) ACF contributed a high proportion of the total number of TB cases detected in the district; 2) ACF detected more clinical TB than bacteriological compared to passive case finding; and 3) 46% of cases diagnosed through ACF were not reported in the SITB, the national TB reporting database.
Active case finding (ACF) contributed 35.7% of the 255 cases notified in Kulon Progo district in 2021. This contribution is consistent with several studies that showed increased TB case detection through ACF [16,17,18,19]. For example, community-based ACF in India and Cambodia have been reported to increase TB case detection beyond what is found through routine case-finding activities [16,18]. Our study design does not allow us to infer the extent to which the 91 cases found through ACF represent additional yield over routine case finding in Kulon Progo and these persons might still have presented to health facilities in the absence of ACF. Despite this uncertainty, the yield of cases from ACF suggests it is acceptable and feasible in Kulon Progo and therefore could be viable as an approach for finding cases among populations that might not promptly seek care for TB at health facilities.
Notably, among ACF cases, there were higher proportions of cases in people aged over 60 years, of males and of persons who were employed. These are perhaps indications that ACF is more successful than PCF in reaching and finding cases among certain population groups. The study period coincided with the COVID-19 pandemic and it is therefore also possible that the observed differences between ACF and PCF cases reflect how case finding strategies were differentially affected by the pandemic and its impact on care seeking for TB.
ACF detected a higher proportion of clinical TB compared to passive case finding. This may be the result of the use of chest X-ray screening in the ACF model of care which contrasts with the lack of chest X-ray services at most of the health centres in Kulon Progo. Chest X-ray is important in TB screening and diagnosis and its use can result in increased case detection relative to case finding without chest X-ray [20]. In Indonesia, chest X-ray has not been widely used for TB ACF and case finding has focused on bacteriologically confirmed cases. However, growing evidence shows that subclinical TB may significantly affect ongoing transmission, and there is important individual benefit to TB diagnosis and treatment for patients who have clinical TB [21].
This study found a high proportion of TB cases, and nearly half of all cases diagnosed by ACF were not reported in the National TB program information system/surveillance. Our study’s findings are consistent with those from a joint external monitoring mission that identified underreporting as a significant problem in the Indonesian program [22]. Similarly, the Indonesia TB Inventory study from 2016-2017 estimated 44% of cases diagnosed were unreported, with those clinically diagnosed, extra-pulmonary and pediatric cases being more likely to be under-reported. Failure to report cases can result in underestimation of TB burden in district areas, leading to inadequate program planning and resources allocation. Failure to report cases could potentially also have an impact on the reported treatment success rate.
Limitations of this study include that the number of unreported cases from passive-case finding could not be estimated. Data from SITB may be incomplete or missing and not reflect the actual number of cases diagnosed and started on treatment. There were possibly clinical TB patients diagnosed and treated at primary health care that were not reported in the SITB and, therefore, not identified by this study. The tendency to under-report clinical cases might explain why ACF cases were not reported in SITB. Further investigation is needed to understand why health facilities may not be reporting clinical cases and help district health to review and strengthen TB surveillance in Kulon Progo. In addition, missing or incorrect NIKs in SITB and ZTBY RECDap could have affected linkage and could have resulted in underestimation of the number of cases from ACF that were actually reported in SITB because linkage could not be made in the absence of the correct NIK in both data sets. Lastly, we could not accurately assess the extent to which ACF resulted in additional yield of TB cases since there was no comparison with a non-intervention area, and the limitations of longitudinal comparison would have been compounded by the effect of the COVID-19 pandemic.
5. Conclusions
In this rural setting, ACF using chest x-ray detected a higher proportion of clinical TB than passive case finding, and a high proportion of cases detected by ACF were unreported in the notification system. This suggests, introducing TB ACF programs, attention to reporting of cases and linkage to case is important. Improvement of case-finding activities is needed to detect more TB cases, especially those with subclinical TB or who have recently developed active TB that may be missed by existing case-finding systems.
Author Contributions
Conceptualization, J.S.K., R.A.A., S.M., D.O., B.D., and R.T.; methodology, J.S.K., R.A.A., S.M.; validation, J.S.K., and D.O.; writing—original draft preparation, J.S.K.; writing—review and editing, J.S.K., R.A.A., B.D., P.D.C., G.C., and R.T.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by The Australian Department of Foreign Affairs and Trade (DFAT) through TB PRIME Structured Operational Research and Training Initiative (SORT-IT) organized by Gadjah Mada University, Menzies Institute, and Burnet Institute.
Institutional Review Board Statement
Ethics approval was obtained from The Medical and Health Research Ethics Committee (MHREC), Faculty of Medicine, Public Health and Nursing Gadjah Mada University, under protocol number KE/FK/1355/EC/2022.
Informed Consent Statement
This study used secondary data collected from Kulon Progo’s SITB database and Zero TB Yogyakarta’s REDCap database. However, written informed consent was obtained from all participants during active case finding activities.
Data Availability Statement
The datasets generated and analyzed during the study are available upon request to the corresponding author.
Acknowledgments
We would like to acknowledge and thank the Disease Prevention and Control Division of Kulon Progo Health Office and staff working in the TB program in Kulon Progo health facilities for their collaborative support.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- World Health Organization. Global Tuberculosis Report 2022. 2022. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022.
- Kementerian Kesehatan RI. PROFIL KESEHATAN INDONESIA TAHUN 2021. 2021.
- WHO. Gear up to end TB: introducing the end TB strategy. 2015. https://apps.who.int/iris/handle/10665/156394.
- Shewade HD, Gupta V, Satyanarayana S, Kumar S, Pandey P, Bajpai UN, et al. Active versus passive case finding for tuberculosis in marginalised and vulnerable populations in India: comparison of treatment outcomes. Glob Health Action 2019;12:1656451. [CrossRef]
- World Health Organization. Diagnostic and treatment delay in tuberculosis. 2006. https://apps.who.int/iris/handle/10665/116501.
- World Health Organization. Optimizing active case-finding for tuberculosis: Implementation lessons from South-East Asia. Regional Office for South-East Asia; 2021. https://apps.who.int/iris/handle/10665/343105.
- Burke RM, Nliwasa M, Feasey HRA, Chaisson LH, Golub JE, Naufal F, et al. Community-based active case-finding interventions for tuberculosis: a systematic review. Lancet Public Health 2021;6:e283–99. [CrossRef]
- TB Inventory Study Team. Tuberculosis Inventory Study in Indonesia 2016-2017 n.d. https://cdn.who.int/media/docs/default-source/hq-tuberculosis/global-task-force-on-tb-impact-measurement/meetings/2018-05/tf7_p04_indonesia_inventory_study_results.pdf?sfvrsn=8cd8d1c5_5 (accessed October 16, 2023).
- Siahaan ES, Bakker MI, Pasaribu R, Khan A, Pande T, Hasibuan AM, et al. Islands of Tuberculosis Elimination: An Evaluation of Community-Based Active Case Finding in North Sumatra, Indonesia. Trop Med Infect Dis 2020;5:163. [CrossRef]
- WHO. WHO consolidated guidelines on tuberculosis, Module 2: Systematic screening for tuberculosis disease. 2021. https://www.who.int/publications/i/item/9789240022676.
- Chan G, Triasih R, Nababan B, du Cros P, Wilks N, Main S, et al. Adapting active case-finding for TB during the COVID-19 pandemic in Yogyakarta, Indonesia. Public Health Action 2021;11:41–9. [CrossRef]
- BPS Kabupaten Kulon Progo. Kabupaten Kulon Progo Dalam Angka 2022 2022. https://kulonprogokab.bps.go.id/publication/2022/02/25/818e21fa047337595988fea4/kabupaten-kulon-progo-dalam-angka-2022.html.
- Dinas Kesehatan Kab. Kulon Progo. Profil Kesehatan Kabupaten Kulon Progo tahun 2022. 2022.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [CrossRef]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [CrossRef]
- Morishita F, Eang MT, Nishikiori N, Yadav R-P. Increased Case Notification through Active Case Finding of Tuberculosis among Household and Neighbourhood Contacts in Cambodia. PLoS One 2016;11:e0150405. [CrossRef]
- Yassin MA, Datiko DG, Tulloch O, Markos P, Aschalew M, Shargie EB, et al. Innovative Community-Based Approaches Doubled Tuberculosis Case Notification and Improve Treatment Outcome in Southern Ethiopia. PLoS One 2013;8:e63174. [CrossRef]
- Parija D, Patra TK, Kumar AM V., Swain BK, Satyanarayana S, Sreenivas A, et al. Impact of awareness drives and community-based active tuberculosis case finding in Odisha, India. The International Journal of Tuberculosis and Lung Disease 2014;18:1105–7. [CrossRef]
- Sanaie A, Mergenthaler C, Nasrat A, Seddiq MK, Mahmoodi SD, Stevens RH, et al. An Evaluation of Passive and Active Approaches to Improve Tuberculosis Notifications in Afghanistan. PLoS One 2016;11:e0163813. [CrossRef]
- Nguyen LH, Codlin AJ, Vo LNQ, Dao T, Tran D, Forse RJ, et al. An Evaluation of Programmatic Community-Based Chest X-ray Screening for Tuberculosis in Ho Chi Minh City, Vietnam. Trop Med Infect Dis 2020;5:185. [CrossRef]
- Kendall EA, Shrestha S, Dowdy DW. The Epidemiological Importance of Subclinical Tuberculosis. A Critical Reappraisal. Am J Respir Crit Care Med 2021;203:168–74. [CrossRef]
- JEMM. The Republic of Indonesia Joint External Monitoring Mission for Tuberculosis. n.d. https://tbindonesia.or.id/wp-content/uploads/2021/06/INDONESIA-JEMM-2020-Eng-1.pdf.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).