1. Introduction
On January 11, 2020, ten days after the first notification made to the World Health Organization (WHO) by China of the first cases of pneumonia in Wuhan, the first gene sequence of the SARS-CoV-2 virus was published [
1]. This has made it possible to start the development of vaccines against the virus, and scientists, industries and other organizations around the world have collaborated to rapidly develop safe and effective vaccines. Some vaccines have been made through methods already known before the pandemic, others have been made using innovative technologies already employed in tumors but with alternate success [
2], or approaches used during previous emergencies such as the pandemic to SARS and Ebola in West Africa.
The vaccines when administered simulate the first contact with the infectious agent, stimulating an immunological response (humoral component and a cellular component) like the natural infection without causing the disease and the complications derived to acquire the active immunity. This is due to immuno-logical memory, or the ability of the immune system to remember which foreign microorganisms have attacked our body in the past and to respond in a timely manner. The absence of an immunological memory is the reason why children undergo infectious diseases more frequently than adults, in fact without vaccinations our body can take weeks to produce enough antibodies to counteract the microorganism. There are two general vaccination strategies [
3], one universal or massive, the other selective with the aim of protecting certain population groups with a particularly high-risk rate of disease, such as the elderly, pregnant women or immunosuppressed individuals or individuals who have more opportunities to infect others (e.g., health workers). When we talk about immunization programs, we must not only think about the health of the individual but also about reducing the social, psychological, economic repercussions of the disease on individuals and on the health system. In fact, a fundamental prerogative, such as that which occurred in the anti-SARS-CoV-2 vaccination plan, is the reduction of the pressure of the health and social assistance system, an area in which the Community Pharmacy can play an essential role. Vaccines can lead to individual protection and contribute to community protection. When in a population there are enough people, in many cases more than 80% of the resident population are immune to an infectious disease. It is unlikely that the disease can spread. This allows people who cannot be vaccinated (people allergic to the components of the vaccine) to benefit from others being vaccinated, as the disease does not spread easily in the community known as herd immunity. Herd immunity is not achieved with all vaccines; in fact, if a vaccine confers individual protection from a disease but does not prevent the spread of the infectious agent, failure to vaccinate the subject falls as a risk only on the same and not on the community like for tetanus vaccine. Often a single dose is not enough. For each vaccine, an optimal number of doses is established according to age and condition of the subject, and every-thing is reported in the technical sheet. If the doses are more than one, the recommended interval between doses and the minimum or maximum time between doses is indicated. In the case of SARS-CoV-2, the protection does not last a life-time and booster doses are indicated [
4]. As with all medicines, however, vaccines are not 100% effective; in fact, the effectiveness for everyone depends on a series of factors such as age, health status, previous or subsequent contact with the pathogen, the mode of administration or the vaccine itself. Vaccines are not effective immediately after the first administration, but the effectiveness increases to an acceptable level in 14 days, effect linked to the development of specific immunoglobulins.
In the case of SARS-CoV-2, mRNA vaccines were often used in the development strategy [
5]. This type of vaccines represent an innovation in that instead of providing the antigen, they provide the genetic information necessary to synthesize and express the antigen by host cells through messenger RNA (mRNA) or self-replicating RNA. This technology, despite being newly introduced, has been studied for more than a decade in cancer [
2,
6], Dr. Katalin Karikó and Dr. Drew Weissman won the Nobel Prize for Physiology and Medicine 2023 for their discoveries concerning nucleoside base modifications that enabled the development of effective mRNA vaccines against COVID-19. The mRNA contains a genetic sequence with instructions to produce the identified target protein spike, a protein found on the surface of the SARS-CoV-2 virus. The mRNA has the characteristic of being able to be inactivated very easily and is not able to enter a cell on its own. For this reason, the mRNA of the vaccine has been inserted into lipids nanoparticle, which has the function of protecting it and allowing it to enter the cells of the host. After administration, the mRNA contained within the nanoparticles enters the host cells, is read by ribosomes and the spike protein is synthesized. At this point the spike protein is transported to the surface of the cell. The presence of this protein, foreign to the host, will bring stimulation of the immune system. Specifically, it will lead to the activation of T lymphocytes and the production of antibodies that will prevent the SARS-CoV-2 virus from entering cells. It is important to note two aspects of mRNA vaccines. The first is that mRNA does not enter the nucleus of cells and therefore cannot interact with DNA. The second is that because the vaccine does not contain the virus, but only the genetic information needed to synthesize the spike protein, it cannot cause disease. There are technologies that use plasmid DNA to make host cells code the spike protein. Vaccines that use this technology often have the great advantage of being able to be produced on a large scale and have high stability. Unfortunately, however, they generally show low immunogenicity and need to be administered through special devices. Unlike what we have just seen, recombinant protein vaccines use viral proteins to induce an antigenic response. The proteins that have been used to produce vaccines are the spike protein, the receptor binding protein (RBD) and virus-like particles (VLP) like in the Novavax's Novaxovid vaccine.
The authorized vaccines were mRNA vaccine Comirnaty (Pfizer—BioNTech) and Spikevax (Moderna—NIAID), the DNA vaccine Vaxzevria (University of Oxford—AstraZeneca) and the Janssen's COVID-19 vaccine (Johnson & Johnson) were firstly used in the vaccination campaign in the different Member States. Their formulations effective against variants such as Comirnaty Original/Omicron BA.1, Comirnaty Original/Omicron BA.4-5, Spikevax bivalent Original/Omicron BA.1, and the Spikevax bivalent Original/Omicron BA.4-5 are also available [
7]. Currently, seven vaccines for COVID-19 have been approved by European Medicinal Agency (EMA) and authorized for marketing release in the E.U. In addition, the Nuvaxovid (Novavax) was approved in December 2021, the COVID-19 inactivated and adjuvanted Vaccine Valneva (Valneva Austria GmbH), and the VidPrevtyn Beta (Sanofi Pasteur) were recently released and are available for use. Those vaccines are often based on the original strain of the SARS-CoV-2 virus, while VidPrevtyn Beta is based on the Beta variant. Also, the CoronaVac (Sinovac) COVID-19 vaccine, is an inactivated virus vaccine, that has been approved for emergency use by the World Health Organization (WHO) [
8], as well as the Sinopharm Beijing Institute of Biological Products COVID-19 vaccine (BBIBP-CorV) received the authorization.
The development of the COVID-19 vaccines has been particularly rapid [
9]; the alignment of the pre-clinical and clinical development phases of vaccines has been an important element as well as the continuous and facilitated dialogue be-tween pharmaceutical company and authority thanks to the EMA Pandemic Task Force (COVID-ETF) made up of experts with various skills [
10,
11]. In the case of COVID-19 vaccines the Conditional Marketing Authorization was adopted [
12,
13] by EMA and the Italian Agency of Drugs (AIFA) authorities based on the positive benefit/risk balance of the medicinal product evaluated by the Commit-tee for Medicinal Products for Human Use (CHMP). The Conditional Marketing Authorization differs substantially from Emergency Use Authorization, which allows some countries such as the United States and Great Britain to temporarily use unauthorized medicines in emergency conditions [
12,
13], and that authorization does not correspond to a marketing authorization and could, if necessary, be withdrawn at any time.
In this context vaccine-vigilance is of interest. The agencies periodically re-view new safety information for all available vaccines and analyze the data through vaccine vigilance [
14] monitoring if the benefit/risk ratio (B/R) remains favorable over time during the vaccine campaign. Vaccine-vigilance is carried out with different modalities such as passive and active surveillances. Passive surveillance consists essentially of the analysis of so-called spontaneous reports and case reports, at least 3 consistent case reports are needed in the absence of any confounding factors. Active surveillance, on the other hand, means a set of proactive actions of stimulation and collection of reports at sentinel sites as groups of patients or doctors, with intensive monitoring systems and through registers consisting of lists of patients with the same characteristics of pathology or exposure to drugs or vaccines. For the new COVID-19 vaccines, the methods of storage, handling and preparation of the dose could generate errors and possibly, adverse reactions that must be reported by pharmacist. Through the analysis of spontaneous reports, signs can emerge relating to risks that need to be quantified. For this purpose, post-marketing cohort and case-control studies are mainly used, which may involve many patients and aim to verify the efficacy and safety of vaccine in the authorized therapeutic indications and in the real conditions of use. These studies allow us to identify infrequent and rare adverse reactions that did not occur during pre-registration studies conducted on small and homogeneous samples of patients and therefore to study subpopulations of subjects not previously evaluated. The Strategic Plan for SARS-CoV-2 vaccination drawn up by all the institutions involved in the management of the vaccination campaign (Ministry of Health, ISS, AIFA, etc.) provides that AIFA promotes additional activities with respect to passive pharmacovigilance, essentially represented by active pharmacovigilance and pharmaco-epidemiology studies like we proposed here in our work. The active pharmacovigilance includes all the activities of stimulation and collection of reports on the population of vaccinated subjects that are registered in the vaccination registers, the pharmaco-epidemiology includes all observational studies on cohort or case-control on the population of vaccinated or on special populations (i.e., with specific conditions). The objective of these activities is to raise safety signals for regulatory purposes, improve knowledge on new vaccines in general and adequately communicate the real risks of vaccination.
To date, in the case of COVID-19 vaccines [
15], mild and moderate adverse reactions to the two innovative -mRNA vaccines were reported very similar. Local reactions are among the most common and generally consist of pain in the arm or redness at the site where the dose was administered. In some cases, some small swelling may also occur, or axillary lymphadenopathy may be associated. However, they are mild reactions that resolve spontaneously within a short time. Among the most frequent systemic reactions are fever, chills, fatigue, headache, and muscle pain which are observed with biologics due to immunoreactions and inflammatory responses [
16,
17,
18]. More rarely, gastrointestinal symptoms, such as nausea, vomiting and diarrhea, have been reported. Myocarditis and pericarditis need further study [
19]. It has already been said that they are rare events of severe degree: the EMA estimates that they occur in 1-2 cases per 100 thousand people vaccinated, with a slightly higher incidence after administration of Spikevax compared to Comirnaty. It generally occurs in young males and mostly after the second dose. Symptoms occur within 14 days of vaccination and consist of palpitations or feeling of heart in the throat, difficulty breathing and chest pain. As for the course of the disease resolves with rest or treatment. During the vaccination campaign, other rare serious adverse reactions were also recorded, but they are not related to the Spikevax and Comirnaty vaccines, this is the case, for example, of thrombosis with thrombocytopenic syndrome that has been associated with vaccination with viral vector vaccines, and mainly occurred in women under 50 years of age [
20]. Guillain–Barré syndrome (GBS), on the other hand, is a rare neuropathy that leads to muscle weakness or even paralysis for longer or shorter periods of time.
Regarding vaccination in children, the data collected to date show that using a reduced dosage of Comirnaty in the age group 5-11 years and a standard dos-age in the age group 12-17 years, is safe as well as effective. Adverse reactions re-ported to the Pharmacovigilance System in the United States have shown that adverse reactions in this age group are like those seen in adults. In a real-world cohort, serious COVID-19 vaccine adverse effects were rare and comparisons across brands could be made, revealing that full vaccination dose, vaccine brand, younger age, female sex, and having had COVID-19 before vaccination were associated with greater odds ratio of adverse effects [
15,
21].
Therefore, three emerging safety signals were identified by COVID-19 sub-committee: transverse myelitis, hearing loss and tinnitus, and acute hepatitis. In addition, the long-term impact of myocarditis, pregnancy outcomes and GBS are being continuously monitored as recommended by the sub-committee [
14] but new signals can emerge in the long term.
The communication is of concern in the success of the vaccine campaign to combat vaccine hesitancy and risk perceptions that affect patients preference. This is part of a social and cultural context that is affected both by the immediate effects of the pandemic experience and by the profound changes that in the last 30 years have characterized the approach to prevention and health promotion and the collective perception of vaccinations. Various causes have been associated with reluctance and uncertainty in resorting to vaccination in COVID-19 [
22]. The concerns associated with COVID-19 vaccines are linked to a number of considerations that can fuel vaccine hesitancy and reduce trust in vaccines (virus news, conflicting messages, rapid vaccine development, perceived politicization of the process, distrust in traditional health information sources, spread of online misinformation and conflicting public debate on vaccines) and confirm the need for communication planned and coordinated that ensures the rapid dissemination of coherent messages, the construction of collaborations, attention to the different levels of health of the population and in particular to equity and therefore allows to avoid vaccine hesitancy and promotes individual confidence in the vaccine. Vaccine hesitancy origin can be also Ethnic based [
23,
24], and strategy can be applied to minimize it [
25]. Several risk-related characteristics are known to systematically influence people's perception. For instance, the risks associated with pandemic vaccination, primarily addressed to adults, were more accepted during the first year of anti- COVID-19 vaccination activities, but with the extension of vaccination coverage, first in the age group between 12-18 years and subsequently in the age group of 5-12 years, these risks were progressively perceived as much less acceptable. The risks related to complications of COVID-19 from not being vaccinated (i.e., the consequence of not having to make any decisions) are more accepted than the risks resulting from the proactive decision to get vaccinated. The research pointed out that very often there is a discrepancy between subjective perception of risk and objective hazard assessment [
26]. For instance, the risk can be elevated in population affected by intellectual disability [
27], and it can be neurologically based [
28]. The risk of thrombosis is higher in these patients than in the general population, despite of the extensive use of novel direct anticoagulants [
29], according to the international guideline, low-molecular-weight heparin is recommended first after careful evaluation of the side effects related to using the drug, and it is needed to evaluate bleeding risk as a universal strategy for routine thrombosis prevention using standard-dose unfractionated heparin or low-molecular-weight heparin in COVID-19 patients admitted to general hospital other than ICUs [
30]. In a minority of cases, mid-dose low-molecular-weight heparin could also be considered [
31]. In addition, a high-risk population is represented by the patients under opioid treatments that during pandemic enhanced they take home therapy for addiction with enhanced risk of overdoses [
32]. In this complex scenario, it is essential to consider some essential elements to develop effective communication strategies on COVID-19 vaccines and the local pharmacist and the family doctor play a role in translating the messages directed to a large population into a patient personalized message to reduce the vaccine hesitancy [
23,
24], often vaccine campaigns are indeed not personalized.
Pharmacists, as health professionals, play already a strategic role in strengthening healthcare through, for instance in the reconciliation of therapy [
33,
34]. The role of pharmacists is expressly contemplated in the National Plan of Chronicity [
35], which expressly provides for the full involvement of pharmacies in health education, primary and secondary prevention activities, through the provision of innovative professional services. There is talk of a new pharmacy model that, in addition to medicine, provides citizens with a series of additional services. The pharmacy, in fact, even during the COVID-19 emergency, has carried out an important assistance activity, also for the execution of tests aimed at detecting the presence of IgG and IgM antibodies and the execution of rapid anti-genic swabs for the detection of SARS-CoV-2 antigen.
Berlofa Visacri and coworkers examined the trials involving pharmacists during the pandemic and their roles [
37]. The 11 studies included in this review were conducted in the United States of America (n 4), China (n 4), Saudi Arabia (n 1), Taiwan (n 1) and Macau (n 1). Most studies described the work of pharma-cists in Hospitals (n 8), in Ambulatory Pharmacy (n 4), Community Pharmacy (n 2) and Clinics (n 1). Participants in the included studies were varied, including healthcare professionals (n 7), COVID-19 patients (n 5), general hospitalization (n 2), general population (n 2), pediatric patients (n 1), solid organ transplant patients (n 1), patients on warfarin therapy (n 1) and patients with myelofibrosis (n 1). In these studies, the various activities of the pharmacists were demonstrated, including disease prevention and infection control. These include distribution of medical devices, development of hygiene strategies, pharmaceutical counseling on drugs dispensed to COVID-19 patients and not used, proper storage and sup-ply of the drug (e.g. drug formulary for the treatment of COVID-19) guiding the supply and purchase of medications, conversion of intravenous to oral medication administration when possible, and patient care and support for healthcare professionals (e.g., ensure appropriate use of the drug for patients and healthcare professionals). All studies made one-to-one contact with recipients and in six studies they used group contact. Several methods of communication have been reported, including face-to-face (n 4), written (n 5), telephone (n 6), video conferencing (n 5) and radio station. Studies were conducted in different intervention settings, such as at the hospital bed (n 7), hospital pharmacy (n 2), community pharmacy (n 2), outpatient (n 4) and home of the recipient (n 5).
More recently, a successful administration of casirivimab/imdevimab in an outpatient setting with low adverse events was performed in a U.S. Community Pharmacy. This innovative monoclonal antibody administration service should be used as an example for a call to action of expansion of pharmacist scope of practice. The role of the pharmacist in the pediatric influenza vaccination and pediatric COVID-19 vaccines has been well supported by evidence [
38].
The role of the hospital pharmacist also emerged; they provided an essential support in the pediatric patients for compounding during pandemic in an Italian setting in the absence of evidence [
39] and in the consulting for appropriate prescription during pregnancy [
40]. A strong emotional exhaustion and stress in the study sample of community pharmacists in Italy has been reported, who reported high-risk perceptions and fear and provided an essential service, despite the high risk of infection [
41].
Considering what is happening in many countries belonging to the European Union and in the United States, the involvement of the Community Pharmacies in the possibility of administering vaccination by the pharmacist is emerging. The Italian National Government, based on specific regulations such as in art. 20, [
36] (D.L. n. 41/2021, has allowed, on an experimental basis, and limited to 2021, the administration of vaccines against SARS-CoV-2 in the Community Pharmacies but with specific obligations, such as the certification of the pharmacist by National Institute Superior of Health (ISS).
We therefore set up a novel vaccination protocol based on the art. 20, [
36] (D.L. n. 41/2021 regulatory rules for patients in our center. We have conduct-ed a monocentric retrospective observational study aimed at evaluating the pharmaceutical service provided at a local Community Pharmacy. We collected anamnestic data and any post-vaccination adverse reactions including the cardiovascular reactions and interviews with the integrated EQ5 method about the evaluation of the quality of life offered and therapy preference.
The regional consumption of vaccine, antivirals and the viremia were also analyzed in this work to monitor the prescription, the drug distribution/dispensation to the patients using the novel D.P.C. protocol and its correlation with the patient’s preference.
2. Materials and Methods
2.1. Protocol
Patients turned to the vaccination center activated at the Community Pharmacy of the ASL BT (Pharmacy Dr. Cannone Domenico Pio) to be subjected to the vaccination cycle prescribed to them according to the methods indicated with which the Italian Government [
36], based on specific rules has allowed, on an experimental basis, and limited to 2021 vaccination at the Community Pharmacy. To fulfill the framework agreement between the Government, Regions, Autonomous Provinces, FederFarma and Assofarm, the Community Pharmacy in Barlet-ta has used considerable economic resources to set up a room in accordance with the law. The measures for air exchange have been strengthened through a system with the exclusion of the recirculation function and keeping the air extractor con-stantly running. They have been used with appropriate different area:
1^ AREA of ACCEPTANCE = booking verification, informed consent collection, pre-vaccination triage.
2^AREA of PREPARATION = preparation of the solution to be injected.
3^AREA of ADMINISTRATION = vaccine administration with appropriate emergency cart and standard container for waste disposal.
4^ AREA of MONITORING = space dedicated to the permanence of the vaccinated subject for the surveillance of any adverse reactions for a time ranging from 15 min to 60 min.
The vaccine Comirnaty and Spikevax were ordered through the "Valore" portal and upon arrival at the pharmacy of the vaccine batches provided for the acceptance of the bubbles on the "GoC" portal. Subsequently, he stored the vials in refrigerators intended for the storage of pharmaceutical products with constant monitoring of the temperature set according to the information acquired from the technical data sheets of each vaccine. Before proceeding with the set-up, the vials were brought to room temperature for about 15-30 min. The vial was then inspected for particulate matter or discoloration of the vaccine. Subsequently, after disinfecting the shelf with alcohol and covering it with a sterile cloth, the pharmacist proceeded to prepare the 1mL syringes with a 23 G needle with low dead space, suitable for intramuscular (i.m.) administration. It is important to underline that about the Comirnaty vaccine it provides for a necessary preventive dilution with 1.8 ml of 0.9% NaCl with a 3 ml syringe, while for the Moderna vaccine no dilution is foreseen and therefore the amount necessary for administration will be taken directly from the vial. In addition, the vials were properly rotated or turned upside down but without ever shaking them in a whirling manner.
Assisted persons are then invited to sit in the monitoring area for a time of not less than 15 minutes. The pharmacist at the end of each vaccination session proceeded to disinfect the surface, to mark the vial used by deleting the label with marker indicating the date and time of start and end of use and adulterating the remaining solution or empty vial with ethyl alcohol. Subsequently, all the data required to ensure the updating of the vaccination registry and the traceability of the vaccine by also entering the batch number has been entered into the "Java" computer system. Upon completion of the registration operations, the vaccination certificate was printed.
Before proceeding with the execution of the vaccination act, it is necessary to acquire the Informed Consent form. Informed consent is the acceptance that the user expresses to a health treatment, freely and after having been adequately in-formed about the methods of execution, benefits, side effects, foreseeable risks, any alternative choices, and possible consequences deriving from the refusal.
Informed consent must meet the following requirements. 'Informed' means that the information must be understandable, in clear and plain language with-out using complex scientific acronyms or terms and possibly in a language well known to the user, based on validated scientific sources, specifying the nature and location of the processing, probability of success, method of execution, expected consequences and their methods of resolution, possible complications, possible alternative choices, consequences of refusal, subsequent behaviors consistent with the treatment. It must be "conscious", expressed by the subject capable of understanding and wanting after correct information; " personnel" must be issued by those who will be vaccinated (for adults), in the case of minors by those who exercise parental authority, by the guardian / legal representative / support administrator, for those who are incapable of understanding and willing. It must be collected in an "explicit" way, referring to each given vaccination and always acquired before the vaccination act. It must also be revocable at any time by the user and free, that is, collected without any form of conditioning of the person's will.
Figure 1.
Sample image of the pharmacist (J.R.D.) after acquisition of written informed consent and compilation of the triage form for the evaluation of the suitability / unsuitability of the patient, performed the inoculation of vaccines through the intramuscular route at an angle of 90 degrees in the deltoid muscle. To minimize injection pain, he invited patients to rotate their arm inwards and applied a firm and rapid puncture. This is a figure. Schemes follow the same formatting.
Figure 1.
Sample image of the pharmacist (J.R.D.) after acquisition of written informed consent and compilation of the triage form for the evaluation of the suitability / unsuitability of the patient, performed the inoculation of vaccines through the intramuscular route at an angle of 90 degrees in the deltoid muscle. To minimize injection pain, he invited patients to rotate their arm inwards and applied a firm and rapid puncture. This is a figure. Schemes follow the same formatting.
An accurate medical history is essential before the administration of any vaccine, to identify any contraindications or precautions to be taken. Health personnel, with targeted questions, using a standardized anamnestic card, get an effective pre-vaccination screening. The purposes of pre-vaccination anamnesis are identifying any conditions that indicate a precaution or constitute a contraindication to vaccination, establish good communication with the subject/family, facilitate conscious adherence to vaccination.
The staff who carry out the anamnesis must be specifically trained regarding precautions, incompatibilities, true and false contraindications of each vaccination and must have mastery of the materials and tools provided (anamnestic card, guide to contraindications, etc.). An observation period of at least 15 minutes after administration of the vaccine. This time interval is established considering that most fast-onset adverse events requiring health intervention begin within 10 minutes. The observation period should be extended to 60 minutes in case of a history of severe allergies to substances do not present in vaccines (food, drugs, etc.). In case of immediate allergies (within 4 hours) to the specific vaccine or its constituents, a specialist evaluation must be requested in advance. Vaccination clinics must be equipped with the pharmacological and instrumental equipment necessary for immediate interventions, in adequate and functioning quantities. Rapid onset events after vaccination are as follows: respiratory spasms (affective or hiccups), anxiety crisis, fainting – collapse, episode of hypotonia – hypo responsiveness (HHE), and manifestations of immediate hypersensitivity.
In adults or older children, the most common adverse event is syncope or vasovagal crisis, which occurs immediately after the injection or shortly after. During this episode the subject quickly pales, loses consciousness and, if standing or sitting, falls to the ground. The recovery of consciousness takes place in one or two minutes. Syncope is sometimes accompanied by brief clonic shocks, however, if this remains an isolated episode, it does not require any specific treatment, nor special investigations. Instead, more attention should be paid to immediate hypersensitivity reactions. These manifestations of hypersensitivity can be mild when symptoms are limited to an urticarial rash and/or immediate swelling at the injection site; severe when cardiorespiratory and neurological symptoms pre-dominate up to shock with severe hypo-perfusion due to relative hypovolemia, with or without bronchospasm and/or laryngospasm or glottis edema. All vaccination recipients should be prepared to deal with an anaphylactic reaction and to distinguish it from syncope, anxiety crises, convulsions, prolonged apnea attacks or other. All vaccination points including our center are equipped with an emergency cart with drugs ready for use in case of immediate hypersensitivity episode.
Generally, vaccination may be recommended in the presence of a precaution, when the benefit from administering the vaccine outweighs the risk of an adverse reaction. A contraindication is a condition in the recipient that increases the risk of a previously observed serious adverse reaction, and contraindicates the ad-ministration, whereas a precaution is a condition in the recipient that may in-crease the risk of a serious adverse reaction or that may impair the ability of the vaccine to produce immunity and therefore requires a risk/benefit assessment. From a regulatory point of view, the contraindication is a negative effect observed in clinical trials, while the precaution is based on the exclusion criteria of clinical trials (unstudied populations). At the time of vaccination, healthcare professionals performing a vaccination must check for contraindications and /or precautions for use before administering a vaccine through the vaccination history or a collection of information through a series of precise and simple questions, using a standardized card. Some of these may suggest postponing vaccination, for example in case of a severe or moderate acute illness with fever or no fever at the time of vaccination. In other cases, such as if generalized urticaria occurred immediately after administration of a previous dose or a severe allergic reaction to latex for products containing natural rubber latex in the pre-filled syringe, the benefits and risks of vaccination should be weighed up. In the case of possible in-creased risk of allergic reactions, it is possible to organize vaccination in a protected environment, i.e., in vaccination centers (unlike local pharmacies) where maximum assistance is available to deal with a possible anaphylactic reaction. There are contraindications to vaccination that are not supported by evidence. Among the most frequent are: allergies in family members, allergies to penicillin, milk proteins or other substances not contained in vaccines, fever after a previous dose of vaccine, non-serious allergic reactions after previous dose, previous febrile seizures in family members or vaccinating (precaution for measles, mumps, rubella, chickenpox), exposure to recent infectious disease, a mild acute illness without fever or with fever < 38.5°C, chronic diseases that do not have specific contraindications such as diabetes.
The Institute Superior of Health (ISS) has recently updated the indications for vaccination in pregnancy recommending the extension of the vaccination offer, with mRNA vaccines, to all pregnant women in the second and third trimesters. This recommendation stems from growing evidence on the safety of vaccination in pregnancy, both to the fetus and the mother. In fact, it is believed that the risk of abortion or problems for the fetus or newborn is like that found in unvaccinated women and in any case not higher than the probability of experiencing complications, even severe, if the infection were to be contracted during pregnancy. In addition, the woman who is vaccinated during pregnancy could transfer part of the antibodies to the fetus, via the placenta. As for the first trimester of pregnancy, vaccination is not recommended in Italy as the evidence is still few. Therefore, in this period of gestation, it is necessary to make a careful assessment of risks and benefits. In lactation, women can get vaccinated, without any need to interrupt it. The breast-feeding woman must be informed that vaccination does not expose the infant to risks and that it is possible that there is a transfer of antibodies through breast milk.
On the basis of the above considerations the eligibility criteria of the patients enrolled were:
adult male and female patients following informed and written consent;
aged male and female patients (age >65 years old) following informed and written consent;
pediatric patients following specific informed and written consent by family members.
The exclusion criteria were:
urticaria that occurred immediately after administration of a previous dose or a severe allergic reaction to latex for products containing natural rubber latex in the pre-filled syringe.
2.2. Statistics
The data were collected in the period from 29.12.2021 to 12.03.2022 and refer to a sample of 550 patients of various ages, sexes and with concomitant diseases and related drug therapy. Anamnestic data and post-vaccination adverse reactions were collected on electronic C.R.F. (Excel Microsoft) for subsequent graphic and statistical processing in anonymity [
32,
42,
43,
44,
45] according to the guide-lines indicated by Directive 679 and 680 of 2016, or the EU General Data Protection Regulation (GDPR) [
46,
47]. The responsibility for data privacy of the ASL BA is the lawyer Elisabetta Fortunato (privacy@sanita.puglia.it.). Interviews with the EQ-5D-Y method [
48] about the evaluation of the quality of the service offered and possible preference between vaccination choice and drug therapy were performed (
Table 1 supplementary files).
The Odds Ratio (O.R.) for each treatment was calculated vs other treatments = (N ADR exposed/N exposed)/(1-(N ADR exposed/N exposed)
/ (N ADR not exposed/N not exposed)/(1-(N ADR not exposed/ not exposed)).
2.3. Vaccine products and drugs
Comirnaty (Pfizer—BioNTech) is an mRNA vaccine that at the beginning of the vaccination campaign was only authorized for people aged 16 years and old-er. It is currently also authorized for the age groups 12-15 years and 5-11 years. After diluting the contents of the vial, it is administered intramuscularly (i.m.) in-to the deltoid region of the arm. In adults the dose is 0.3 ml in the formulation of 30 micrograms of mRNA per dose while in children between 5 and 11 years the dose is 0.2 ml in the formulation of 10 micrograms of mRNA per dose. As mentioned earlier, the primary cycle consists of two doses that are administered 21 days apart. In some clinical conditions of immunocompromised (e.g., trans-plants), administration of an additional dose of vaccine is recommended starting 28 days after the second dose. In addition, in all individuals aged 18 years and older, a booster dose of 0.3 ml is recommended at least 4 months, or 120 days, after completion of the primary course of vaccination [
49].
Spikevax (Moderna—NIAID) was authorized by AIFA in Italy on 7 January 2021 and is authorized from 12 years of age. This vaccine, like Comirnaty, is mRNA. It is administered i.m. in the deltoid region of the arm. The dose for the primary cycle is 0.5 ml, or 100 micrograms per dose. As mentioned above, a primary cycle consists of 2 (two) doses that are administered 28 days apart. In case of clinical conditions leading to immune impairment, an additional dose may be administered 28 days after the second dose. As with Comirnaty, people aged 18 years and over can administer a booster dose at least 4 months, or 120 days, from the completion of the primary cycle. In this case it is administered at half the dosage, i.e., 0.25 ml, containing 50 micrograms of mRNA [
50]
Vaxzevria (University of Oxford—AstraZeneca) is given by two injections of 0.5 mL into the muscle. The second injection may be given 4 to 12 weeks after the first injection. Vaxzevria is not recommended for children under 18 years of age. There is currently insufficient information available on the use of Vaxzevria in children and adolescents under 18 years of age. A preferential use of the Astra-Zeneca vaccine, in subjects between 18 and 65 years, for which more solid evidence is available. The Prot. 31355 of 15 March 2021, provides a temporary ban on the use of all lots of presents on the national territory of the "COVID-19 Vac-cine AstraZeneca", AIC no. 049314026, holder AIC Astra Zeneca AB, represented in Italy by Astra Zeneca S.p.A., after taking note of the signal of thromboembolic events. However, the European Medicines Agency (EMA) lifts, with immediate effect, on 19.03.2021 the prohibition of use according to which the benefits of the vaccine in preventing hospitalization and death from COVID-19 outweigh the risk of developing disseminated intravascular coagulation or clots in the vessels that drain blood from the brain.
EMA's Safety Committee concluded its preliminary review of a signal for thrombi outbreaks in people vaccinated with the AstraZeneca COVID-19 vac-cine. The Committee confirmed that the benefits of the vaccine in combating the still widespread threat of COVID-19 (which in turn causes clotting problems and can be fatal) continue to outweigh the risk of side effects, the vaccine is not associated with an increased overall risk of thrombi-related events (thromboembolic events) in those who receive it, there is no evidence of problems related to specific batches of the vaccine or to particular production sites, however, the vaccine may be associated with very rare cases of thrombi in the presence of thrombocytopenia, i.e. low levels of platelets (blood elements that promote clotting) with or without bleeding, including rare cases of thrombi in the vessels that drain blood from the brain as in the cerebral thrombosis of the venous sinuses (CVST). These rare cases, around 20 million people in the UK and European Economic Area (EEA) have received the vaccine as of 16 March 2021, and EMA has found only 7 cases of thrombi in multiple blood vessels as in the disseminated intravascular coagulation (CID) and 18 cases of CVST. A causal link with the vaccine is not proven, but it is possible and deserves further analysis. The Pharmacovigilance Risk Assessment Committee (PRAC) involved experts in blood diseases in its re-view and worked closely with other health authorities. Overall, the number of thromboembolic events reported post-vaccination, both in pre-authorization studies and in post-vaccination reporting (469 reports, 191 of which from the EEA), is lower than expected in the general population. This allows the PRAC to confirm that there is no increased overall risk of thrombi. However, some concerns remain in younger patients, particularly related to these rare cases.
The Committee's experts examined in detail the cases of CID and CVST re-ported by Member States, 9 of which were fatal. Most of these occurred in people under the age of 55, mostly women. Because these events are rare and COVID-19 itself often causes blood clotting disorders in patients, it is difficult to estimate the expected incidence for these events in people who have not received the vaccine. However, based on pre-COVID-19 data, it was calculated that, as of 16 March 2021, less than 1 case of CID was expected to occur among people under 50 years of age within 14 days of vaccine administration. This was not evident in the older population given the vaccine. In conclusion, AIFA with a circular of 7.04.2021 conformed that the Vaxzevria vaccine is approved from 18 years of age, based on current evidence, considering the low risk of thromboembolic adverse reactions in the face of high mortality from COVID-19 in the most advanced age groups, recommends its preferential use in people over the age of 60. By virtue of the data available to date, those who have already received a first dose of the Vaxzevria vaccine, can complete the vaccination cycle with the same vaccine [
51].
The Janssen's COVID-19 vaccine (Johnson & Johnson) vaccine which is indicated for active immunization in the prevention of novel coronavirus disease (COVID-19), caused by the SARS-CoV-2 virus, in individuals aged 18 years and older; is given as a single 0.5 mL dose by injection i.m. only, preferably into the deltoid muscle of the arm.
Following administration of the Janssen COVID-19 vaccine, blood clots have been observed very rarely in association with low platelet levels. This condition included severe cases with blood clots even at unusual sites (e.g., brain, intestines, liver, spleen), in some cases with the presence of bleeding. The cases occurred in the three weeks following vaccination and mainly in women under 60 years of age. This condition also resulted in death. The CTS met on 20.04.2021 for an up-date on the discussion and conclusions of the PRAC-EMA on the evaluation of the safety signal related to cases of thrombosis with thrombocytopenia occurring after administration of the Janssen COVID-19 vaccine. The EMA reiterates that the benefits of the vaccine in the prevention of COVID-19 outweigh the risks of side effects throughout the population included in the authorized indication (subjects from 18 years of age). A combination of thrombosis and thrombocytopenia, in some cases accompanied by bleeding, has been observed very rarely following vaccination with the COVID-19 Janssen vaccine. For this reason, the same conditions of use as the Vaxzevria vaccine are recommended for the Janssen vaccine. Therefore, the Janssen vaccine, which is approved for use from 18 years of age, should preferably be given to people over 60 years of age [
52].
Finally, the Nuvaxovid (Novavax) vaccine was authorized by AIFA in Italy at the end of December 2021 and is authorized in people from 18 years of age. The development platform is different from previous vaccines in that it is a vac-cine based on a recombinant protein, the spike protein, and an adjuvant. It is ad-ministered as two-dose course 21 days apart. Doses are 0.5ml each and contain 5 micrograms of spike protein per dose [
53].
2.3.2. Antiviral drug and D.P.C. protocol
Paxlovid (nirmatrelvir/ritonavir) [
54], Pfizer Europe MA EEIG, is used for treating COVID-19 in adults who do not require supplemental oxygen and who are at increased risk of the disease becoming severe. Nirmatrelvir is a protease reversible inhibitor of coronavirus 3CLpro mainly metabolized by cytochrome P450 (CYP)3A4, and ritonavir, an inhibitor of the CYP3A isoforms that potentiate nirmatrelvir by fixing its suboptimal pharmacokinetic properties. Patients take two nirmatrelvir 150 mg tablets and one ritonavir 100 mg tablet twice daily for five days, starting within five days of symptoms showing. Paxlovid is expected to reduce the risk of hospital admission and death in unvaccinated people at risk of severe disease from 7% to 0.8%, despite with the omicron variant, this benefit was reduced.
This drug is provided to the patients using the novel D.P.C. protocol that al-lows the acquisition of drugs by ASL-BA in stock following a centralized procedure at better condition and their capillary distribution by the Community Pharmacies that dispense the drugs within 24 hours to the patients at 7 euro/patient for the service. This drug is available in 50 thousand doses per month.
2.4. Vaccine Effectiveness
The effectiveness in our setting was evaluated in relation to different out-comes. We evaluated the efficacy in reducing severe forms of the disease, hospitalizations and intensive care unit permanence, and mortality from COVID-19 in our patients. In addition, although to a lesser extent, also the capability in reducing the number of infections (symptomatic and asymptomatic) of SARS-CoV-2.
In the report of 7 December 2021, efficacy was estimated from data for the period from 5 July to 5 December 2021. The report shows how COVID-19 vac-cines are extremely useful in preventing disease outcomes: the efficacy that is estimated is 88.7% against hospitalizations, 93.5% for Intensive Care Unit (ICU) admissions and 89.2% against deaths. As expected, the impact on SARS-CoV-2 diagnoses, i.e., for all infections, symptomatic and asymptomatic, is more modest, but still close to 65%. It should be noted that the percentages shown derive from an estimate and are therefore subject to margins of uncertainty. For subjects who have completed the primary cycle for more than 5 months (150 days) the effectiveness in preventing severe forms of the disease (which include hospitalized, hospitalized, ICU, deaths) is reduced by about 9%, from 92.6% to 83.7%. The ad-ministration of an additional dose, or a booster dose, has the effect of bringing the efficacy back above 93%. More marked is the effect of time on the ability to pre-vent diagnoses of SARS-CoV-2, or the set of asymptomatic and symptomatic infections. In this case, the effectiveness of vaccination, for those who have completed the vaccination cycle for more than 5 months, is reduced by more than 30% from 74.3% to 39.6%. Even in this case, however, the administration of an additional dose, or a booster dose, brings the vaccination efficacy above 76%. These data are consistent with estimates obtained from surveillance in other countries and highlight the need to administer the booster dose from a minimum of 4 months to a maximum of 6 months from the second dose.
2.5. Vaccinovigilance
Suspected vaccine reactions are reported electronically by filling the reporting form, both available on the AIFA website, or by filling it directly online on the Vigifarmaco website following the guided procedure. For the new COVID-19 vaccines, the same card currently in use for all other vaccines and the current re-porting method is used. To define the temporal relationship between vaccination and adverse event, and to identify any therapeutic errors or defects in vaccine quality, we collected information on the date and time of vaccination, type, name and batch number of the vaccine, site, mode and route of administration and dose number (1st, 2nd etc.). The report form is sent to the Local Pharmacovigilance Manager (RLFV) responsible for the territory who validates the report and inserts it into the National Pharmacovigilance Network (RNF). The Local Pharmacovigilance Manager responsible for the territory shall validate the reporting form within 7 days of receipt. Validation means the verification of the consistency of the data and the presence of minimum reporting requirements (a patient, a medicine, a reaction, a signaler). Once included in the Network, the report is subjected to a further quality control by the Regional Pharmacovigilance Centers and AIFA that verify the completeness of the information on the patient and the vaccine, possibly request further follow-up information and evaluate the causal link. From the RNF, reports pass daily through the European database Eudravigi-lance and from this to the global database of the WHO, VigiBase.
An adverse event is any undesirable medical event that occurs in a patient or in a subject included in a clinical trial who is given a medicinal product, and which does not necessarily have a causal relationship with the treatment itself. Adverse drug reaction (ADR), on the other hand, implies that there is a causal relationship between a medicine/vaccine and an adverse event/effect is possible.
When an adverse event is reported, the data is analyzed to determine whether there is a causal link with the vaccine. Adverse events could also be due to illness or anxiety about receiving the vaccine.
Safety concepts also used here were: "danger" that represents an objective event that can create damage to people, while "risk" represents a potential dam-age of variable severity determined by exposure to danger, so the risk expresses a possibility (probability) of damage in relation to exposure to the danger, and can be measured in objective terms.
3. Results
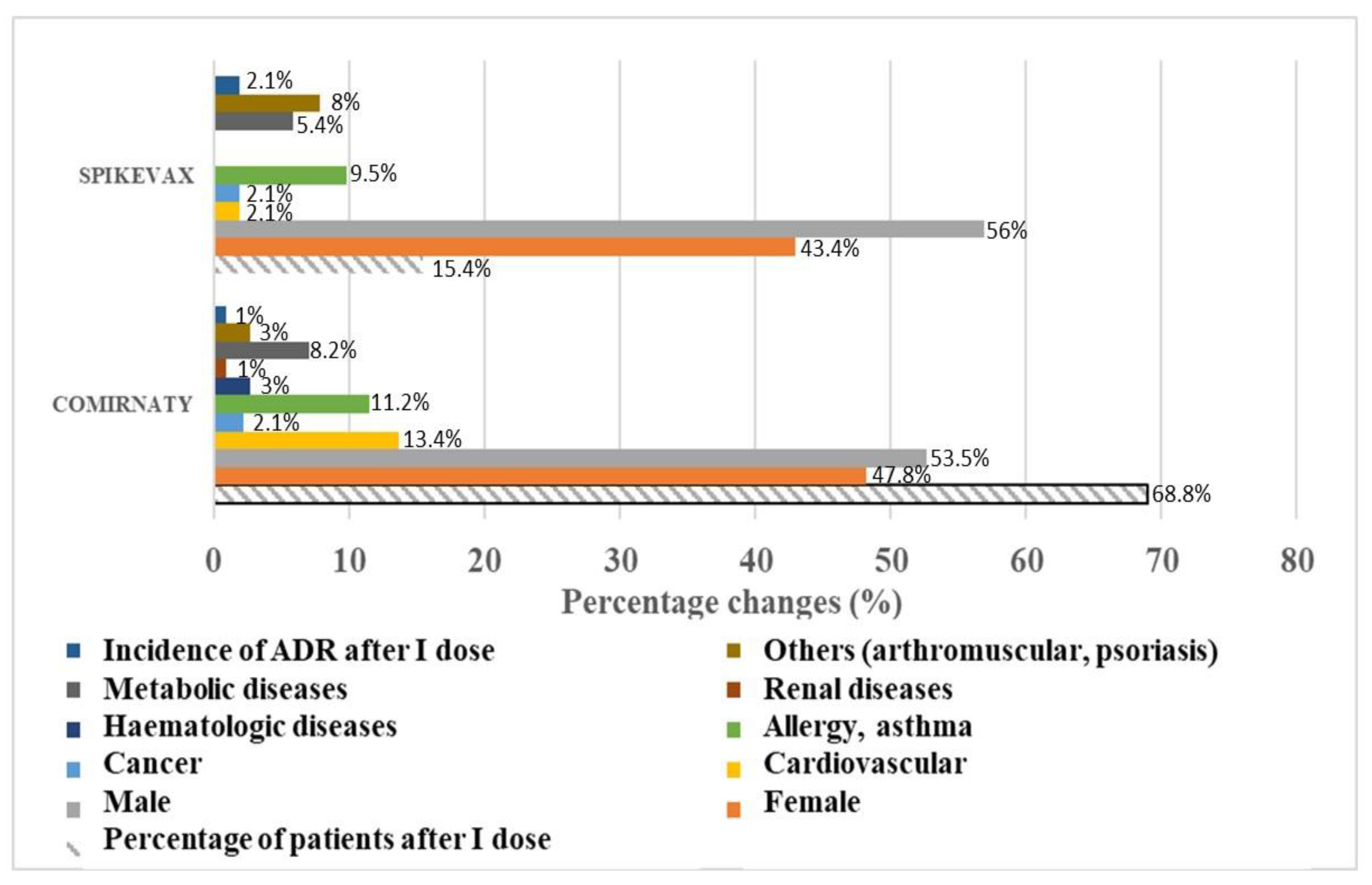
In our center, a total number of 550 patients composed by adult patients (N patients = 418), aged patients (N patients = 73) and pediatric patients (N patients = 59) were vaccinated on 12.03.2022. The data were analyzed retrospectively and reported according to age groups. Vaccination administration has been well tolerated in all population groups in our center. The vaccines were reactogenic after the first dose in > 75% of the patients with mild and moderate injection site reactions. The two most administered vaccines were Comirnaty (N patients = 371) and Spikevax (N patients = 81) in the population. The adult sample was homogeneous in relation to gender for Comirnaty with an imbalance towards the male sex in the sample treated with Spikevax. The distribution of concomitant diseases in the two treated samples was comparable about tumors, metabolic diseases and allergic diseases and intolerances, but differed in relation to the arthro-muscular diseases most represented in the sample treated with Spikevax and cardiovascular diseases instead more represented in the sample treated with Comirnaty (
Figure 2).
The incidence of moderate immune-allergic reactions was approximately double in the sample treated with Spikevax vs the sample treated with Comirnaty and affected the female sex (
Figure 2). In detail, in adult patients, vaccination administration caused mild and moderate injection site reactions in all patients tolerable as expected, and in some patient’s adverse reactions expected within 24-48 hours and reported in the data sheet that did not require hospitalization or medical intervention.
Uncommon reactions of moderate degree with an incidence of 1.39% and 2.86% in the adult female patients were respectively observed with Comirnaty and Spikevax however expected as one case of skin rush in a 23-year-old woman not affected by diseases, a case of high fever with a T>40.5 ° C in a 22-year-old woman who did not respond to paracetamol in the absence of diseases, a case of peripheral edema in a 36-year-old woman with a history of food intolerance and chemicals, and one case of syncope in a 35 female patient with hypertension. These reactions did not require medical intervention or hospitalization and resolved (
Table 2).
We did not observe moderate and severe reactions with other vaccines due to the rarity of the event and the low sample size. Of the 5 patients vaccinated with Janssen at the first and second doses, they were then switched to Comirnaty (N patients=3) and Spikevax (N patients=2) at the booster dose without showing intolerance or adverse reactions. Of the 8 patients vaccinated with Vaxervria (Astrazeneca), they switched to the second dose to Comirnaty (N patients=2) and the booster dose (N patients=2), and some to the booster dose of Spikevax (N patients=4) without consequences or intolerances. We did not observe any significant reactions in patients already infected (N patients = 40) then subjected to the second dose of vaccine of which 13 vaccinated with Spikevax and the remaining majority with Comirnaty.
The elderly population (N patients = 73) was less represented in our sample and showed a comparable distribution between men and women; it showed a vaccination distribution with a slight prevalence of patients vaccinated with Comirnaty compared to other vaccines. Elderly patients were mostly suffering from cardiovascular disease (N patients = 18) and metabolic comorbidity (N patients = 12) with sporadic cases of benign prostatic hyperplasia and cancer. In this elderly population, the vaccination procedure was well tolerated with an incidence of the moderate ADR of 1.36% due to Comirnaty. We observed a case of moderate pruritus (
Table 3) in an elderly woman suffering from another pathological condition reaction already reported in the literature [
55]. One case of persistent diarrhea in a hypertensive female patient with dizziness receiving ibesartan (150 mg) and vertisec (24 mg) who was SARS-CoV-2 positive at the first dose was vaccinated with the dose II of Vaxervria and doses IIII and IV of Comirnaty.
Finally, we had a sample of patients (N patients = 58, N female = 36, male =22) in pediatric age treated mainly with Comirnaty and the remaining part with Spikevax. In other cases, patients had suffered a first infection. A case of moderate vagal hypotension has been detected of non-immunological origin in a female patient, that is reported also by others with Comirnaty after I dose [
21], and a case of redness face swelling of allergic origin has been also observed in a male patient. In this population the vaccination procedure was tolerated but with a high incidence of the moderate ADR of 3.44% due to Comirnaty.
The calculated Odds Ratio of Comirnaty vs other treatments for all age groups was 0.8 indicating a favorable outcome of this vaccine treatment. We therefore evaluated the quality of life and the pharmaceutical service. Our data pooled on a sample of 100 patients following self-administration showed that the quality of pharmaceutical service has highlighted how the service rendered has produced high satisfaction scores (Table 4) with no gender effect in the higher satisfied group with code 111111 but manifesting mild problems in the group with male prevalence (N male/N female= 4/2 cases), moderate problems with female prevalence (N female/N male=14/12 cases), and severe problems and less satisfaction within the group with codes 212221, 222221 and 323331 (N female=3 cases).
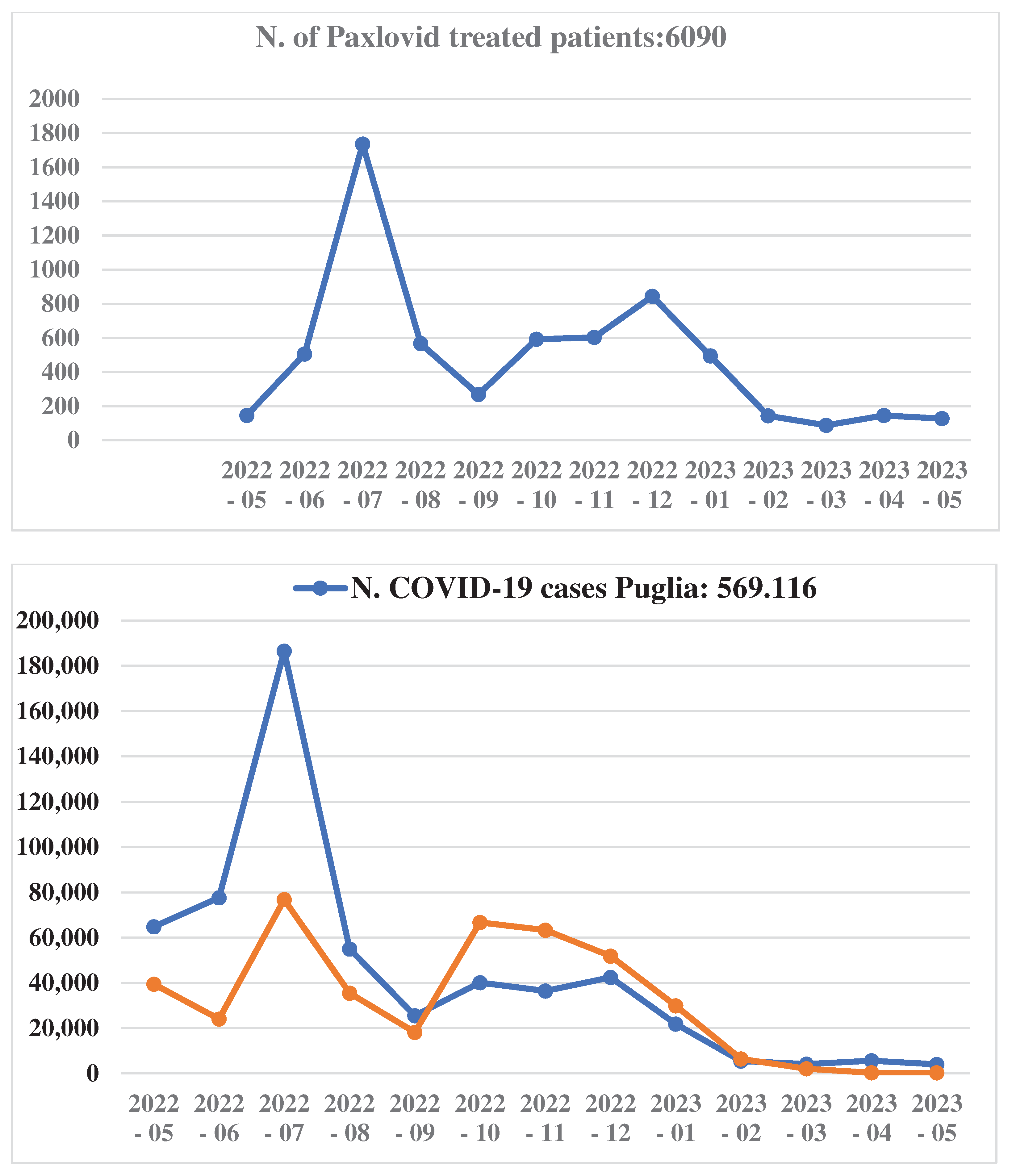
The analysis (EQ-5D-Y) of the treatment prescriptions shows that the 3 patients out of 100 patients were eligible for drug therapy to maintain the vaccine efficacy in case of new infections on 12.03.2022. These patients were at high risk of developing severe disease; to date they were safely treated and not hospitalized. We, therefore, collected data on COVID-19 therapy of the patients for one year starting from 1 May 2022 to 1 May 2023. We found a very well correlation between Paxlovid, distributed and dispensed by the Community Pharmacy by the D.P.C. protocol, vaccine administrations and the COVID-19 cases (
Figure 3) in Puglia region from the 08-2022 to 05-2023 despite of the expected lower number of patients treated with Paxlovid vs the vaccinated patients with 1.47% of the patients eligible for the antiviral drug therapy. While an increased number of COVID-19 cases uncorrelated to the vaccine administration were observed during the first four months of observations (
Figure 3). The average daily number of hospitalizations in May and July 2022 were, respectively, N=487 and N=497 as an aggregated data suggesting that the number of hospitalizations despite the increase in infections remain stable.
4. Discussion
In our work we evaluated the vaccine procedure in terms of tolerability and satisfaction of the pharmacy service in 550 patients in our Pharmacy Community. As expected, the vaccines were reactogenic after the first dose in most of the patients with mild and moderate reactions with younger age and female gender as risk factors. Similarly, around 75% of the COVID-19 vaccinations led to reactogenicity and nearly 25% of them led to one or more days of work loss especially in female gender of younger age [
56]. Uncommon reactions of moderate-severe degree in the adult female patients were observed with Comirnaty and Spikevax. The moderate immune-allergic reactions detected in our center are in line with what has been observed in the literature where young women even without his-tory of intolerance reactions or allergic reactions have manifested this type of re-actions to mRNA vaccines both immediate anaphylactic and delayed with an imbalance in favor of Comirnaty vs Spikevax [
21,
55], trend that is also confirmed in our center. In the elderly population also affected by comorbidity, the vaccination procedure was well tolerated. In the pediatric population the vaccination procedure showed an incidence of the moderate ADR of 3.44% due to Comirnaty higher than that observed in the adult and aged populations suggesting of a higher susceptibility of these patients’ population. The vaccination with Comirnaty showed also a favorable O.R. <1 vs other treatment for all age groups. We failed to observe myocarditis in our population. While myocarditis of moderate degree of severity were reported in 129 patients following mRNA COVID-19 vaccination affecting mostly male patients in a metanalysis study in a large cohort of patients [
19]. Also, thromboembolic events were not observed in our patients in contrast to what recently reported in a large population [
20]. Despite diabetes type II and insulin response has been associated with negative prognosis in COVID-19 patients for different causes such as association of pathogenic factors [
42,
57,
58,
59,
60], and also loss of control and monitoring during pandemic [
61], no ADR were observed in the diabetic patients that were represented in the 5.8-7% of our patients under vaccination program. Therefore, the vaccination procedure adopted experimentally at the Community Pharmacy was found to be safe and effective. The population has joined the vaccination campaign at the pharmaceutical site, responding positively to the proposed pharmaceutical ser-vice. The minor reactions observed but not reported in this report were in line with those reported by the technical data sheets of the vaccines as well as the moderate immune-allergic reactions that did not require medical intervention and hospitalization but resolved at the patients' homes. The trend of moderate immune-allergic reactions observed in young women in our center are in line with what has recently been reported in the literature and supports the involvement of Community Pharmacies as an essential site for a systematic collection of data of epidemiological interest to direct targeted therapeutic choices. The lower scores evaluating the Quality of Life was observed in the female.
To reduce the pressure in the NHS during the pandemic, the Community Pharmacy have been invited by the government to also participate in the flu vaccination campaign of the NHS, integrating the flu vaccination network of the NHS to patients over 65, people with chronic and immunosuppressed diseases, children aged 6 months to 6 years and pregnant or postpartum women.
The Community Pharmacy other than in vaccination campaign played a key role in the dispensing the antivirals in the eligible patients in concert with the pharmaceutical service at the ASL-BA center responsible for the Puglia region on behalf of third parties (D.P.C.) protocol. It should be remembered that in Italy two oral antiviral drugs have so far been authorized for the treatment of COVID-19 in adults who do not require additional oxygen therapy and who have a high risk of developing a severe form of COVID-19: Paxlovid (nirmatrelvir/ritonavir) of the Pfizer Europe MA EEIG, and Lagevrio (molnupiravir ) of Merck Sharp & Dohme.
For Paxlovid Italy transposed the European authorization on 31 January 2022, published in the Official Gazette no. 26 of 1 February 2022. This classifies the medicine for reimbursement by the National Health Service in "C not negotiated [C(nn)]" and assigns the following supply regimen: medicine subject to limited medical prescription, to be renewed from time to time, sold to the public on prescription of hospital centers identified by the regions (RNRL).
Lagevrio (molnupiravir) in Italy its distribution has been authorized by Decree of the Ministry of Health of 26 November 2021. Molnupiravir works by interfering with the virus's ability to replicate; since it does not target the Spike protein, its effectiveness does not depend on the variants. Its effectiveness, however, is conditioned by the timeliness of treatment, which must begin at most within 5 days from the onset of disease, confirmed by positive swab, and ideally within 72 hours. The progression to severe forms of COVID-19, with the involvement of the lungs, occurs after a few days from the onset of infection, but the duration of this period is very variable. In addition, the situation can sometimes precipitate with-in a few hours and require hospitalization in intensive care. The patients to be treated with molnupiravir are selected by general practitioners or Special Assistance Continuity Units (USCA), while the prescription is due to doctors working within the facilities identified by the regions for administration. Patients who have at least one of the following risk factors associated with evolution to severe disease are eligible for treatment: active oncological or hematological diseases, chronic renal failure (excluding patients on dialysis or with eGFR < 30 mL/min/1.73 m2), severe broncho pneumopathy, primary or acquired immunodeficiency, obesity (BMI >= 30), severe cardiovascular disease (heart failure, coronary artery disease, cardiomyopathy) and uncompensated diabetes mellitus. The therapy consists of taking four capsules a day, for a total of 5 days. This drug is an important additional tool to counteract the risks related to infection, however it cannot be considered an alternative to vaccines. Currently, molnupiravir is less cost/effective than Paxlovid and there will be less investment.
The intravenous antiviral for the treatment of COVID-19 is also authorized in Italy Veklury (remdesivir) of the Gilead Sciences Company. This is the first antiviral medicine to have received authorization, by decision of the European Commission of 3 July 2020, for the "treatment of coronavirus disease 2019 (COVID-19), in adult and adolescent patients (aged 12 years and older and weighing at least 40 kg) with pneumonia requiring supplemental oxygen therapy". This authorization was implemented in Italy with the decision published in the GU no. 250 of 09-10-2020, containing the classification of the medicinal product in class [C(nn)], with the following supply regimen: medicine subject to limiting medical prescription, usable exclusively in a hospital environment or in a similar structure (HOSP). Since 30 December 2021, following the European authorization of an extension of indication, Veklury is also indicated for the treatment of COVID-19 in adults not hospitalized for COVID-19 and not on oxygen therapy with onset of symptoms for no more than 7 days and in the presence of predisposing clinical conditions that represent risk factors for the development of severe COVID-19.
The prescription of antivirals for the treatment of COVID-19 is subject to a monitoring register and involves the use of the card relating to the drugs subject to monitoring. In addition, all antivirals are subject to additional monitoring. This allows the rapid identification of new security information. Healthcare professionals are asked to report any suspected adverse reactions using the National Pharmacovigilance Network.
The AIFA Technical Scientific Commission (CTS) is oriented in favor of the prescription of new antiviral drugs against COVID-19 by family doctors and dispensing by Community Pharmacies "according to the mechanism of distribution on behalf of third parties (D.P.C.). The idea is to allow prescription even to general practitioners precisely to facilitate more widespread access.
Paxlovid requires adequate training for family doctors, gives numerous drug interactions to be evaluated carefully but the goal is to use it more and safely, given that so far, we have used it less than expected and today we have such a quantity as to make it available to a wider audience of prescribers and patients [
62]. This drug is distributed on behalf of third parties (D.P.C.) in all regions, i.e., purchased by the regional ASL-BA that will make them available in Community Pharmacies, and the citizen will be able to pick it up directly from the pharmacy on the prescription of the general practitioner within 24 hours. Also, in this case the Pharmacists of the Community, Hospital and Territorial collaborated with the National Authorities in favor of use and dispensing the antivirals therapy as supported by our consumable data in the period 2022 after the vaccination campaign.
Our data indicated that 3% the patient’s preference for antiviral Paxlovid after the vaccination campaign at the 12.03.2022 to maintain the vaccine efficacy in case of new infections. The patient’s percentage preference calculated on a small sample by quality of life questioner was aligned to the trend of the medical prescription in all Puglia region during one year of monitoring starting from 01 May 2022 to 01 May 2023 with the 1.47% of the patients eligible for the antiviral drug therapy. During the first four months of observation the number of COVID-19 cases were uncontrolled by the applied therapy because of several reasons for instance the initial difficulty in patients recruitment and the unavailability of the vaccines but a marked reduction of COVID-19 cases in our Puglia Region was observed in the latest 8 months of observations being very well correlated with therapy. These findings indicate an appropriate prescription and distribution of the therapy in our setting.