Submitted:
29 November 2023
Posted:
30 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
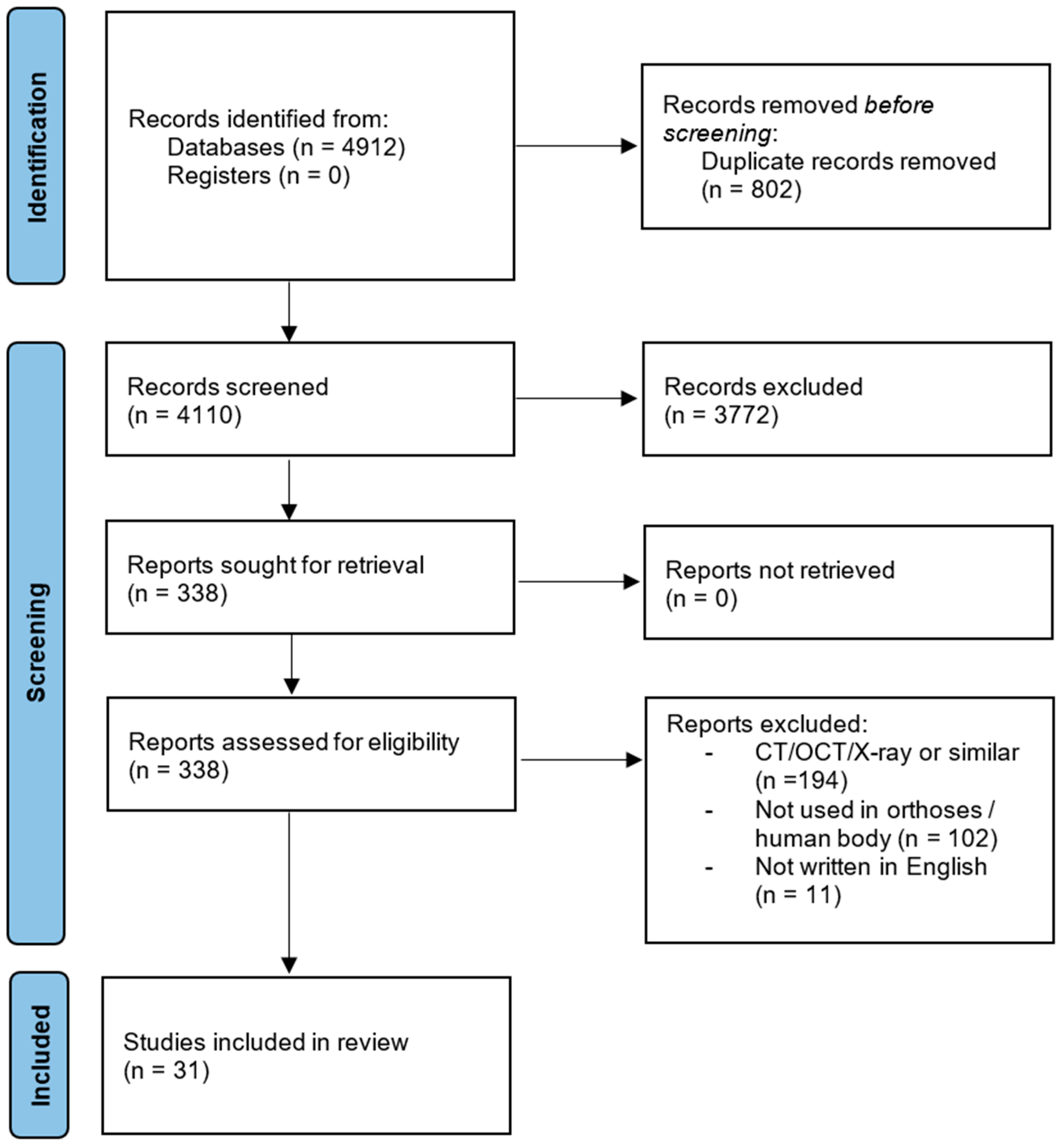
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Roberts, A.; Wales, J.; Smith, H.; Sampson, C.J.; Jones, P.; James, M. A Randomised Controlled Trial of Laser Scanning and Casting for the Construction of Ankle–Foot Orthoses. Prosthet Orthot Int 2016, 40, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Mavroidis, C.; Ranky, R.G.; Sivak, M.L.; Patritti, B.L.; DiPisa, J.; Caddle, A.; Gilhooly, K.; Govoni, L.; Sivak, S.; Lancia, M.; et al. Patient Specific Ankle-Foot Orthoses Using Rapid Prototyping. J Neuroeng Rehabil 2011, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Belokar, R.M.; Banga, H.K.; Kumar, R. A Novel Approach for Ankle Foot Orthosis Developed by Three Dimensional Technologies. IOP Conf Ser Mater Sci Eng 2017, 280, 2–7. [Google Scholar] [CrossRef]
- Dias Hensen, J.C.; Foggiatto, J.A.; Ulbricht, L.; Wan Stadnik, A.M. Additive Manufacturing of Customized Lower Limb Orthoses – A Review. Int J Innov Educ Res 2018. [Google Scholar] [CrossRef]
- Chudnofsky, C.R.; Byers, S.R.; Roberts, J.R.; Hedges, J.R.; Chanmugam, A.S. AS: Clinical Procedures in Emergency Medicine 2004.
- Brognara, L.; Fantini, M.; Morellato, K.; Graziani, G.; Baldini, N.; Cauli, O. Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials 2022. [Google Scholar] [CrossRef] [PubMed]
- Volonghi, P.; Baronio, G.; Signoroni, A. 3D Scanning and Geometry Processing Techniques for Customised Hand Orthotics: An Experimental Assessment. Virtual Phys Prototyp 2018, 13, 105–116. [Google Scholar] [CrossRef]
- Górski, F.; Wichniarek, R.; Kuczko, W.; Żukowska, M.; Lulkiewicz, M.; Zawadzki, P. Experimental Studies on 3D Printing of Automatically Designed Customized Wrist-Hand Orthoses. Materials 2020. [Google Scholar] [CrossRef] [PubMed]
- Munhoz, R.; Moraes, C.A. da C.; Tanaka, H.; Kunkel, M.E. A Digital Approach for Design and Fabrication by Rapid Prototyping of Orthosis for Developmental Dysplasia of the Hip. Revista Brasileira de Engenharia Biomedica 2016, 32, 63–73. [Google Scholar] [CrossRef]
- Oud, T.; Tuijtelaars, J.; Bogaards, H.; Nollet, F.; Brehm, M.-A. Preliminary Effectiveness of 3d-Printed Orthoses in Chronic Hand Conditions: Study Protocol for a Non-Randomised Interventional Feasibility Study. BMJ Open 2023. [Google Scholar] [CrossRef]
- Dal Maso, A.; Cosmi, F. 3D-Printed Ankle-Foot Orthosis: A Design Method. Mater Today Proc 2019, 12, 252–261. [Google Scholar] [CrossRef]
- Geoffroy, M.; Gardan, J.; Goodnough, J.; Mattie, J. Cranial Remodeling Orthosis for Infantile Plagiocephaly Created Through a 3D Scan, Topological Optimization, and 3D Printing Process. Journal of Prosthetics and Orthotics 2018, 30, 1. [Google Scholar] [CrossRef]
- Sansoni, G.; Trebeschi, M.; Docchio, F. State-of-the-Art and Applications of 3D Imaging Sensors in Industry, Cultural Heritage, Medicine, and Criminal Investigation. Sensors 2009, 9, 568–601. [Google Scholar] [CrossRef] [PubMed]
- Servi, M.; Volpe, Y.; Uccheddu, F.; Furferi, R.; Governi, L.; Lazzeri, S. A Preliminary Usability Assessment of a 3D Printable Orthosis Design System. In Proceedings of the International Conference on Human-Computer Interaction; Springer; 2018; pp. 273–280. [Google Scholar]
- Dombroski, C.E.; Balsdon, M.E.R.; Froats, A. The Use of a Low Cost 3D Scanning and Printing Tool in the Manufacture of Custom-Made Foot Orthoses: A Preliminary Study. BMC Res Notes 2014, 7, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Eder, M.; Brockmann, G.; Zimmermann, A.; Papadopoulos, M.A.; Schwenzer-Zimmerer, K.; Zeilhofer, H.F.; Sader, R.; Papadopulos, N.A.; Kovacs, L. Evaluation of Precision and Accuracy Assessment of Different 3-D Surface Imaging Systems for Biomedical Purposes. J Digit Imaging 2013, 26, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Van Nguyen, J.M.; Talbot, K.; Heales, L.; Kean, C.O.; Kong, P.W.; Stanton, R. Immediate Comfort Perception of 3d-Printed Foot Orthoses in Individuals With Unilateral Heel Pain. Prosthet Orthot Int 2021. [Google Scholar] [CrossRef] [PubMed]
- Rogati, G.; Leardini, A.; Ortolani, M.; Caravaggi, P. Validation of a Novel Kinect-Based Device for 3D Scanning of the Foot Plantar Surface in Weight-Bearing. J Foot Ankle Res 2019, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nam, H.-S.; Seo, C.H.; Joo, S.Y. ; 김동현; Park, D.-S. The Application of Three-Dimensional Printed Finger Splints for Post Hand Burn Patients: A Case Series Investigation. Ann Rehabil Med, 2018. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D. Evaluations of the Uptake and Impact of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement and Extensions: A Scoping Review. Syst Rev 2017, 6, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Baronio, G.; Harran, S.; Signoroni, A. A Critical Analysis of a Hand Orthosis Reverse Engineering and 3D Printing Process. Appl Bionics Biomech 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Grazioso, S.; Selvaggio, M.; Di Gironimo, G. Design and Development of a Novel Body Scanning System for Healthcare Applications. International Journal on Interactive Design and Manufacturing 2018, 12, 611–620. [Google Scholar] [CrossRef]
- Ciobanu, O.; Ciobanu, G.; Rotariu, M. Photogrammetric Scanning Technique and Rapid Prototyping Used for Prostheses and Ortheses Fabrication. Applied Mechanics and Materials 2013, 371, 230–234. [Google Scholar] [CrossRef]
- Krajňáková, V.; Rajťúková, V.; Hudák, R.; Živčák, J. APPLICATION OF THE ARTEC EVA SCANNER FOR ORTHOTICS IN PRACTICE. Lékař a technika - Clinician and Technology 2020, 49, 92–96. [Google Scholar] [CrossRef]
- Dessery, Y.; Pallari, J. Measurements Agreement between Low-Cost and High-Level Handheld 3D Scanners to Scan the Knee for Designing a 3D Printed Knee Brace. PLoS One 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Weigert, M.C.; Poier, P.H.; Rosenmann, G.C.; Foggiatto, J.A.; Volpato, N.; Okimoto, M.L.L.R. Indirect 3D Scanning of the Foot Plant - Comparison between a Medium and Low-Cost Tools. Advances in Transdisciplinary Engineering 2016, 4, 614–621. [Google Scholar] [CrossRef]
- Parry, E.J.; Best, J.M.; Banks, C.E. Three-Dimensional (3D) Scanning and Additive Manufacturing (AM) Allows the Fabrication of Customised Crutch Grips. Mater Today Commun 2020, 25, 101225. [Google Scholar] [CrossRef]
- Cha, Y.H.; Lee, K.H.; Ryu, H.J.; Joo, I.W.; Seo, A.; Kim, D.H.; Kim, S.J. Ankle-Foot Orthosis Made by 3D Printing Technique and Automated Design Software. Appl Bionics Biomech 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Ranaldo, D.; Zonta, F.; Florian, S.; Lazzaro, J. A Facile, Semi-Automatic Protocol for the Design and Production of 3D Printed, Anatomical Customized Orthopedic Casts for Forearm Fractures. J Clin Orthop Trauma 2023, 42. [Google Scholar] [CrossRef] [PubMed]
- Sabyrov, N.; Sotsial, Z.; Abilgaziyev, A.; Adair, D.; Ali, H. Design of a Flexible Neck Orthosis on Fused Deposition Modeling Printer for Rehabilitation on Regular Usage. In Proceedings of the Procedia Computer Science; Elsevier B.V., 2021; Vol. 196; pp. 226–234. [Google Scholar]
- Roucoules, L.; Paredes, M.; Eynard, B.; Camo, P.M.; Rizzi, C. Advances on Mechanics, Design Engineering and Manufacturing III: Proceedings of the International Joint Conference on Mechanics, Design Engineering & Advanced Manufacturing, JCM 2020, June 2-4, 2020; Springer Nature, 2021; ISBN 3030705668.
- Powers, O.A.; Palmer, J.R.; Wilken, J.M. Reliability and Validity of 3D Limb Scanning for Ankle-Foot Orthosis Fitting. Prosthet Orthot Int 2022, 46, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Murzac, R.; Doicin, C.V.; Ulmeanu, M.E. Data Acquisition and Generative Design for a Smart Spinal Orthosis. Macromol Symp 2021, 396. [Google Scholar] [CrossRef]
- Ambu, R.; Oliveri, S.M.; Calì, M. Neck Orthosis Design for 3D Printing with User Enhanced Comfort Features. International Journal on Interactive Design and Manufacturing 2023. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, S.J.; Cha, Y.H.; Lee, K.H.; Kwon, J.Y. Effect of Personalized Wrist Orthosis for Wrist Pain with Three-Dimensional Scanning and Printing Technique: A Preliminary, Randomized, Controlled, Open-Label Study. Prosthet Orthot Int 2018, 42, 636–643. [Google Scholar] [CrossRef]
- Mo, S.; Leung, S.H.S.; Chan, Z.Y.S.; Sze, L.K.Y.; Mok, K.M.; Yung, P.S.H.; Ferber, R.; Cheung, R.T.H. The Biomechanical Difference between Running with Traditional and 3D Printed Orthoses. J Sports Sci 2019, 37, 2191–2197. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Liu, G.; Yu, L.; Wang, Y.; Fang, Y.; Shen, Y.; Huang, X.; Qiao, L.; Yang, J.; Zhang, Y.; et al. Effects of a 3D-Printed Orthosis Compared to a Low-Temperature Thermoplastic Plate Orthosis on Wrist Flexor Spasticity in Chronic Hemiparetic Stroke Patients: A Randomized Controlled Trial. Clin Rehabil 2020, 34, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.R.; Fang, J.J.; Wu, C.T.; Lin, R.M.; Su, P.F.; Lin, C.L. Analysis of a Customized Cervical Collar to Improve Neck Posture during Smartphone Usage: A Comparative Study in Healthy Subjects. European Spine Journal 2019, 28, 1793–1803. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Wang, I.J.; Sun, J.R.; Liu, C.H. Customized Designs of Short Thumb Orthoses Using 3D Hand Parametric Models. Assistive Technology 2022, 34, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Kim, D.K.; Cha, Y.H.; Kwon, J.Y.; Kim, D.H.; Kim, S.J. Personalized Assistive Device Manufactured by 3D Modelling and Printing Techniques. Disabil Rehabil Assist Technol 2019, 14, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, P.; Yan, M.; Xie, Y.; Huang, G. Additive Manufacturing of Specific Ankle-Foot Orthoses for Persons after Stroke: A Preliminary Study Based on Gait Analysis Data. Mathematical Biosciences and Engineering 2019, 16, 8134–8143. [Google Scholar] [CrossRef] [PubMed]
- Telfer, S.; Abbott, M.; Steultjens, M.; Rafferty, D.; Woodburn, J. Dose-Response Effects of Customised Foot Orthoses on Lower Limb Muscle Activity and Plantar Pressures in Pronated Foot Type. Gait Posture 2013, 38, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Telfer, S.; Abbott, M.; Steultjens, M.P.M.; Woodburn, J. Dose-Response Effects of Customised Foot Orthoses on Lower Limb Kinematics and Kinetics in Pronated Foot Type. J Biomech 2013, 46, 1489–1495. [Google Scholar] [CrossRef]
- Wang, K.; Shi, Y.; He, W.; Yuan, J.; Li, Y.; Pan, X.; Zhao, C. The Research on 3D Printing Fingerboard and the Initial Application on Cerebral Stroke Patient’s Hand Spasm. Biomed Eng Online 2018, 17. [Google Scholar] [CrossRef]
- Fu, J.C.M.; Chen, Y.J.; Li, C.F.; Hsiao, Y.H.; Chen, C.H. The Effect of Three Dimensional Printing Hinged Ankle Foot Orthosis for Equinovarus Control in Stroke Patients. Clinical Biomechanics 2022, 94. [Google Scholar] [CrossRef]
- El-Hakim, S.; Beraldin, J.A.; Picard, M.; Godin, G. Detailed 3D Reconstruction of Large-Scale Heritage Sites with Integrated. IEEE Comput Graph Appl 2004, 24, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.H.; Lee, K.H.; Ryu, H.J.; Joo, I.W.; Seo, A.; Kim, D.H.; Kim, S.J. Ankle-Foot Orthosis Made by 3D Printing Technique and Automated Design Software. Appl Bionics Biomech 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Hartley, R.; Zisserman, A. Multiple View Geometry in Computer Vision; Cambridge university press, 2003; ISBN 0521540518.
- Agudelo-Ardila, C.P.; Prada-Botía, G.C.; Rodrigues G, P.H. Orthotic Prototype for Upper Limb Printed in 3D: A Efficient Solution. J Phys Conf Ser 2019, 1388, 012016. [Google Scholar] [CrossRef]
- Pribanić, T.; Petković, T.; Đonlić, M.; Hrgetić, V. On Fabrication of a Shoe Insole: 3D Scanning Using a Smartphone. In IFMBE Proceedings; 2019; Vol. 64, pp. 111–116 ISBN 9789811045042.
- Salvi, J.; Fernandez, S.; Pribanic, T.; Llado, X. A State of the Art in Structured Light Patterns for Surface Profilometry. Pattern Recognit 2010, 43, 2666–2680. [Google Scholar] [CrossRef]
- Lee, S.Y.; Majid, Z.; Setan, H. 3D Data Acquisition for Indoor Assets Using Terrestrial Laser Scanning. ISPRS Annals of Photogrammetry, Remote Sensing and Spatial Information Sciences. II-2 W 2013, 1, 221–226. [Google Scholar] [CrossRef]
- Glock, F.; Vogel, M.; Naumann, S.; Kuehnapfel, A.; Scholz, M.; Hiemisch, A.; Kirsten, T.; Rieger, K.; Koerner, A.; Loeffler, M.; et al. Validity and Intraobserver Reliability of Three-Dimensional Scanning Compared with Conventional Anthropometry for Children and Adolescents from a Population-Based Cohort Study. Pediatr Res 2017, 81, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.K. Three-Dimensional Optical Scanning for Clinical Body Shape Assessment Comes of Age. Am J Clin Nutr 2019, 110, 1272–1274. [Google Scholar] [CrossRef]
- Del Corso, M.; Abà, G.; Vazquez, L.; Dargaud, J.; Ehrenfest, D.M.D. Optical Three-Dimensional Scanning Acquisition of the Position of Osseointegrated Implants: An in Vitro Study to Determine Method Accuracy and Operational Feasibility. Clin Implant Dent Relat Res 2009, 11, 214–221. [Google Scholar] [CrossRef]
| Reference | Anatomical Zone | 3D Scanner | Software Used to Process the Data Acquired | Outcomes | Conclusions | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Name | Type of 3D Scanner | Characteristics of 3D Scanner | Scanner | CAD | ||||||||
| Dal Maso and Cosmi, 2019 [11] | Ankle-Foot | Default Camera | Photogrammetry | No data | Agisoft Photoscan Pro |
SolidWorks | 150 photos taken. 80% of calculation time was used for photo alignment, tie point cloud, sparse cloud cleaning and cleaning. Mesh exportation to STL format with ≈20000 faces. | Scanner can be used on other parts of the body. The printed orthosis had great geometrical correspondence and comfort. The method showed instability when converting STL into CAD which requires experience and ability. | ||||
| Baronio et al., 2016 [21] | Hand (including fingers) | 3D Scan-in-a-Box optical scanner | Structured light | Scans in about 4 seconds, with metric accuracy of 0.1% in relation to the size of the object size | No data |
Rhinoceros | Anatomy was obtained with 8 acquisitions (2min each). Total scanning time was 1h30min for acquisition with data cleaning and rigid alignment with 1h for mesh creation, regularization, and repair. | The methodology was geometrically satisfactory with a favourable trade-off between high-accuracy (in the reproduction of the patient anatomy) and low-cost requirements. | ||||
| Grazioso et al., 2018 [22] | Spinal | INBODY and Polhemus FastSCAN SCORPION | Photogrammetry and Laser | Photogrammetry: Circular structure, 17 pillars (7 cameras each with 5Mpx). Polhemus FastSCAN SCORPION: No data |
No data | No data | Photogrammetry allowed instantaneous capture, but processing time was longer vs. laser scanner. Deviation between scanners was +0.90 mm and −1.11mm. The laser scan obtained 13,150 faces and the inbody scan obtained 68,750 faces. | The photogrammetric scanner showed good accuracy and high-fidelity colour. The availability in medical centres could help the patients, thanks to the minimally invasive procedure and medical practitioners, in having a system which results simple to use. | ||||
| Belokar, Banga and Kumar, 2017 [3] | Ankle-Foot | No data | Laser with structured light | No data | No data | No data | The 3D scanner was rotated manually around patient’s limb to create the template model in just one minute. Time-saving approach when digitizing. |
3D scanning is suitable to produce custom orthotics. | ||||
| Ciobanu et al., 2013 [23] | Foot | Default Camera | Photogrammetric | No data | 3DSOM | No data | 20 to 40 leg shots were taken. The software automatically created a cloud of 3D points from photos and transformed the points into a 3D mesh. | Use of photogrammetry were feasible in the case of foot orthosis fabrication as a cost-effective 3D reconstruction technique. Some problems in surfaces with indentations and blind holes. | ||||
| Krajňáková et al., 2019 [24] | Shoulder, neck and face | Artec EVA | Structured light | Resolution: 0.5 mm; accuracy: 0.1 mm; distance accuracy: 0.03% at 1000 mm; texture resolution: 1.3 Mpx; | Artec Studio | No data | The scanner captured all types of hair. Better results with tousled hair and wet hair. Beard is not advisable, as the neck area will be blurred. It is possible to scan complicated body shapes. | Scanner outputs can be used in medicine for the design and manufacture of orthoses and dental implants; simulation before and after plastic surgery, preservation of cultural heritage and virtual reality. | ||||
| Dessery and Pallari, 2018 [25] | Knee brace | Artec EVA and iSense | Structured light | Artec Eva: Resolution: 0.5 mm; frame rate: 16Hz iSense: Resolution: 0.9 (at 0.5m) ± 30mm (at 3m); frame rate: 30 Hz |
Artec Studio 9 (Artec Eva); 3DSizeMe (iSense) | Artec Studio 9 (Artec Eva); MSoft (iSense) | Three scans were performed on each participant with Artec (410s ± 118s) and iSense (507s ± 94s) from the malleolus to the upper thigh art. Processing time was 3588s ± 423s for Artec and 460s ± 169s for iSense. Mean circumferences were created to compare results. | Manual measurement is the accurate method to take lower limb measurements, but the inter- and intra-reliability is poor and information about leg shape is limited. 3D scanners can provide lower limb measurements with similar accuracy, but better repeatability ((intraclass correlation coefficient: 0.99 − 1.0) and 0.15% mean differences). | ||||
| Roberts et al., 2016 [1] | Ankle-Foot | FastSCAN | Laser | No data | No data | Rodin 4D | 134 AFOs fabricated with CAD technology and traditional plaster method in a double-blind randomised (1:1) controlled trial design was compared. No difference in time taken to cast or scan the limbs. Rectification and moulding time for cast AFOs was 55.1±26.0min and for scanned AFOs was 26.9±12.2min. | 70% of patients said they preferred to be scanned than to have their limbs cast in plaster. A significantly higher proportion of scan based AFOs failed to meet the specification stipulated by the orthotist increasing production time by 9 days. |
||||
| Weigert et al., 2016 [26] | Foot | Default Camera and Roland MDX-40 | Photogrammetry and Mechanical 3D scanner (Touch Probe / Point-to-point scanner) | Photogrammetry: Sony Xperia SP C5303 smartphone Roland MDX-40: Head course: 305 x305x105mm; Accuracy variable and up to 0.04mm |
Scanner: No data (Roland MDX-40); Memento (photogrammetry) |
CATIA; Geomagic | 62 photos taken for photogrammetry and reconstruction take 30min. MDX-40 took 26H to scan the plaster cast. Relative error between plaster model and photogrammetry was 2.85% and 0.72% between plaster model and MDX-40. | Both scans showed similar topography of the foot. Mechanical presented more irregularities; however, this mesh provided more details that the MDX-40 especially between the toes. The 2.85% relative error presented by photogrammetry could be compensated with the application of soft material on the surface. | ||||
| Volonghi, Baronio and Signoroni. 2018 [7] | Hand | Cronos 3D Dual (static scanner) and Insight3 (real-time scanner) | Structured light and optical scanner | Cronos 3D Dual: 4s per frame; 2 Mpx. Accuracy: ±30–60 μm. Insight3: Real time; 1280 × 1024 Px Accuracy: ±0.25–0.5 mm. |
Optical RevEng 2.4 | No data | Scan processing time was 7.5min for volunteers and 9min for patients. Error inferior to 0.5mm between scanners. Cronos 3D with volunteers achieved a complete. Insight3 with patients did not had any motion artifacts. | For Cronos 3D, motion artefacts relating to involuntary movements were successfully corrected. The preservation of all fine textural information of the final aligned model was demonstrated. For Insight 3, motion artefacts were reduced or even avoided. Both scanners proved appropriate for hand anatomy acquisition. | ||||
| Rogati et al., 2019 [18] | Foot | Microsoft Kinect Sensor and IQube | Structured light | Microsoft Kinect: Laser emitter an infrared and an RGB camera to obtain a 300.000 point-cloud Accuracy: 2.8 ± 0.6mm; IQube: No data |
Skanect (Kinect); No data (IQube) | Geomagic | Acquisition time for the Kinetic was 25s. The comparison between 3D scans of the plantar surface resulted in error of 2.8±0.6mm (left feet) and 2.9±0.4mm (right feet). In the arch region were 1.4±0.4mm (left feet) and 1.6±0.5mm (right feet). Good repeatability of the Kinect scans was observed. The foot dimensions were like the corresponding PodoBox (manual measurement). | The total cost of the prototype created with the Kinetic Sensor is about 200–300€, which is at least one order of magnitude lower than that of commercial laser-based foot scanners. While accuracy and repeatability results were largely consistent across subjects, and between left and right foot intra-subject, the sample of feet analysed was small. | ||||
| Dombroski, Balsdon and Froats., 2014 [15] | Foot | Microsoft Kinect | Structured light | No data | No data | MeshLab | Two AFOs were created. One by AM with Kinect and one created by TPCM. The TPCM provided the most control over movement of the medial longitudinal arch. The arch height index (AHI) was 21.2mm (shod only), 21.4mm (AM AFO) orthosis and 22.0mm (TPCM). | The 3D printing AFO resulted in a higher AHI than the shod condition, however, the differences between the 3 conditions were minimal. Variability was similar with standard deviations within 0.13 mm. Sample size of only one subject was small. Kinect could be a low-cost method of custom foot orthotic manufacturing. | ||||
| Parry, Best and Banks, 2020 [27] | Grip for the Hand | ROMER Absolute Arm | Laser | No data | Geomagic Wrap |
Fusion 360 with Nettfab | The data collection was approximately 10 min. Manufacturing time was 10h5min with a cost of €10.90 (with overheads and machine depreciation excluding labour). | The study demonstrated that AM and Scanners is a viable method of producing customised daily living aids, which is anticipated to improve quality of life for sufferers of arthritis at low-cost. | ||||
| Cha et al., (2017) [28] | Ankle-Foot | Artec Eva | Structured light | Maximum snap rate: Up to 16 fps | No data | MediACE 3D | The study compared an AM AFO with conventional AFO. In QUEST, all items were ranked as “very satisfied” or “satisfied.” The patient was more satisfied with the AM AFO regarding weight and ease of use and more effectiveness on conventional AFO. | The AM AFO focused on the weight, individualization, and comfort rather than the function. In addition, the printed AFO had the advantage of being easily wearable inside a shoe compared to the conventional AFO, which usually requires larger shoes to wear. | ||||
|
Ranaldo et al, 2022 [29] |
Forearm | Structure Sensor Mark II (Occipital) | Photogrammetry | Based on active stereo vision | Autodesk MeshMixer | Rhinoceros | The analysis was carried out on three cast meshes having different pattern distributions but an identical overall shape. All models show a perfectly elastic behaviour, with a maximum σv well below the tensile strength of the material (50 MPa) and a maximum displacement. |
This study shows that a semi-automatic, programmable tool allows to design anatomical customized orthopaedic casts with optimized features for the treatment of forearm fractures. Its main advantages are: it does not require specific CAD skills to perform the design of the orthosis; it does not take significant time for the generation of the model; the designs can be subject to finite element analysis to foresee different load scenarios and validate the choice of geometry. | ||||
| Sabyrov et al, 2021 [30] |
Neck | Sense (2nd generation) | Optical scanner | No data | No data | Fusion 360 | The extended support section, which is positioned on trapezius muscles, improved comfortability, and stability. The breathability of skin is achieved via well distributed elliptical holes. The convex shape at the front model gives convenient swallowing. Application of flexible TPE (flex) material adds flexible property, hence enhance the dressing process. Comparative to PLA material, it has a lower density, which defines low weight. The negligible deformation during numerical assessment emphasized the strength of design. |
The fabricated orthosis model possesses high accuracy in terms of the neck shape of the patient. This was accomplished through 3D scanning and further processing of the CAD model. The advantage and applicability of new cervical orthosis design and the flexible filament were demonstrated. |
||||
|
Roucoules, 2020 [31] |
Arm | 3D Romer RS1 | Optical scanner | Depth technology: Active stereoscopic Operating range: ~0.16–10 m Resolution: 1280 × 720 Framerate: Up to 90fps Field of view FOV: H69°, V43°, D77° (±3°) |
Oplà 2.0 | No data | All errors measured in the reconstruction were in the range [−2.9, 1.5] mm, the mean error of the signed distance is −0.49 mm with a standard deviation of 0.64 mm. The composition of the panel group has allowed the validation of the acquisition system on significantly different hand-wrist-arm anatomies. | Except some local errors, Oplà 2.0 performed well within the limits imposed by the accuracy requirements | ||||
| Powers, et al, 2022 [32] |
Ankle-Foot | Occipital, Inc., San Francisco CA | Infrared Structured light | No data | Design Studio software (Standard Cyborg, Inc., San Francisco CA) | No data | Excellent interrater reliability was obtained for scan-based measures. Excellent intrarater test-retest reliability was established for the scanning process. MDC values for intrarater test-retest reliability were typically around or below 4mm for foot and ankle measures, and under 6mm for circumference and length | The results of this study demonstrate that low-cost 3D limb scanning can be used to obtain valid and reliable measurements of 3D limb geometry for the purpose of AFO fitting, when collected using the clinically relevant standardized conditions presented here. | ||||
|
Murzac et al, 2021 [33] |
Spine | No data | No data | No data | Meshmixer | Fusion 360 | The scanning and processing of the obtained data can be done following the procedure described in this paper. This ensures a compliant geometry for virtual analysis of the product that will be produced for a certain user. At the same time, the generative design guarantees the choice of a geometry, manufacturing technologies and a material that leads to the choice of the optimal option from a technological and economic point of view. Also, with the help of the software filters it is possible to identify the optimal variant for the manufacturer according to the objectives set for each production cycle | The chosen option can vary from one production batch to another and from one stage of the product life cycle to another. The final concept of the spinal orthosis is designed for upper body posture correction of clinically healthy individuals, with no pre-existing congenital malformations of the spine. | ||||
| Ambu et al., 2023 [34] |
Neck | Microsoft Azure Kinect DK | Structured light | 1Mpx depth sensor, a 12Mpx RGB camera and two IR illuminators to obtain mappings of the object’s depth with high accuracy in a very short time. The illuminator used in wide field of-view mode is tilted an additional 1.3 degrees downward relative to the depth camera | No data | No data | Topology Optimization (TO) model, structurally evaluated by means of FE analysis, also in comparison with an orthosis having a ventilation pattern configured as Voronoi cells, showed a satisfactory behavior also considered that, voids are large for extension and flexion loading, stress distribution occurs in areas of limited size with reference to the extent of the upper parts where the load is applied. The highest values of maximum displacement and maximum Von Mises stress was obtained for extension loading; however, maximum displacement was lower than 2 mm, while maximum stress was under the limit value for HPB. | A scanning system made up of three synchronized low-cost sensors, suitably arranged, has been developed. This system allows a fast acquisition, about 5 s, with minimum discomfort for the patient. The scanning system is also potentially suitable to hospital setting, being low cost and provided with a GUI for semi-automatic management of the device. The manufacturing of prototypes was done with a new bio-based material, which also contribute to lightness and satisfies the aesthetic demands. Neck temperature measurements highlighted a better performance for the TO orthosis even with the insertion of a padding. TO orthosis is very promising as regards user’s comfort, an automatized strategy for the procedure will be investigated. | ||||
| Kim et al., 2018 [35] | Wrist and hand | Artec™ Eva | Structured light | No data | Artec™ Eva | Geomagic Touch and Geomagic Freeform software | The Patient-Rated Wrist Evaluation showed significant pain relief in both groups. Two items of the 28 Orthotics and Prosthetics Users’ Survey (OPUS) questions, “Put toothpaste on brush and brush teeth” and “Dial a touch tone phone,” showed high satisfaction scores, with statistically significant difference in the experimental group. | The 3D-printed wrist orthosis was superior to the cock-up orthosis in some items of the OPUS. Wrist pain was reduced in the 3D-printed wrist orthosis as well as the cock-up orthosis, so the 3D-printed wrist orthosis could possibly play the same role as the off-the shelf cock-up orthosis. | ||||
| Mo et al., 2019 [36] | Foot | David SLS HD 3D scanner | Structured light | No data | No data | Geomagic Freeform | Results showed lower peak rearfoot eversion angles during running with TPM or 3D printed (3DP) orthoses than no-orthoses control condition (CON). No differences were observed in other biomechanical parameters among the three conditions. Running with TPM and 3DP orthoses resulted in better perceived comfort in “medial-lateral control” and “heel cushioning” than CON. There were no statistical differences in all parameters between TPM and 3DP orthoses. | The present findings indicate improved comfort during running with TPM or 3DP orthoses, which hinted 3DP orthoses could be a viable alternative to TPM orthoses for clinical practice. | ||||
| Zheng et al., 2020 [37] | Wrist-hand | HCP | Optical scanner | No data | No data | Unigraphics NX 8.0 Software | After six weeks: -A significant difference was found between the two groups (experimental group and control group) in the change of Modified Ashworth Scale scores -There was no statistically significant difference between the two groups in flexion and radial-deviation angles -There was a significant difference between the two groups in the change of Fugl-Meyer Assessment scores -No statistically significant difference was found in the change of visual analogue scale scores between the two groups -A statistically significant difference was found in the change of swelling scores between the two groups -No statistically significant difference was found in the change of subjective feeling scores between the two groups. |
3D-printed orthosis showed greater changes than low-temperature thermoplastic plate orthosis in reducing spasticity and swelling, improving motor function of the wrist and passive range of wrist extension for stroke patients. | ||||
| Kuo et al., 2019 [38] | Head and neck | Go! SCAN 50, Creaform | No data | No data | No data | No data | Smartphone use increased the head and neck flexion angles in all postures, and sitting without back support showed the greatest head and neck flexion angles. The posture-correcting effect of the customized collar was better than the Aspen Vista and Sport-aid collars. In addition, the customized collar was more comfortable to wear than the other two collars in most contact areas. | Smartphone use increased both the head and neck flexion in different postures, and the proposed customized 3D-printed cervical collar significantly reduced the head and neck angles. | ||||
| Chu et al., 2020 [39] | Hand | Occipital Inc. | Structure light | No data | Apple Corp., Cupertino | Digital Vernier Caliper | The QUEST revealed the highest score in the mean satisfaction level. The items evaluated were dimension, weight, adjustments, safety, durability, simplicity, comfort, and effectiveness. | The new process saves time and is highly accurate in clinical practice. The short thumb orthosis prototype created by the proposed design procedure offers satisfactory functional quality in numerous aspects and high practicality in clinical practice. | ||||
| Lee et al., 2019 [40] | Hand | Artec Eva, Artec | Optical scanner | No data | No data | Geomagic Freeform | The JHFT score improved after application 3D printed devices. In most QUEST items, 3D printed devices showed better results than ready-made assistive devices. The typing speed became faster in 3D printed devices than in ready-made assistive devices. The patient was satisfied with the orthosis in writing a pen, eating food and typing keyboard because of its fitness to his hand and easy-to-use. | The study designed and manufactured a patient-specific assistive device optimized for patient function after estimating the disability status of a patient with brain injury through 3D printing techniques. | ||||
| Liu et al., 2019 [41] | Ankle-foot | EinScan—Pro, SHINING 3D | Laser | No data | No data | Geomagic Studio | With respect to the temporal-spatial parameters, the velocity and stride length in the gait with AFO increased significantly as compared to the gait without AFO. The cadence increased, double limb support phase decreased, and the step length difference decreased in the gait with AFO; however, the difference was not statistically significant. | This study confirmed the feasibility of patient specific AFO fabricated by AM techniques and demonstrated the process of modifying AFO models successfully. The specific ankle-foot orthoses fabricated by material PA12 have a significant effect on the improvement of velocity and stride length in people with stroke. | ||||
| Telfer et al., 2013a [42] | Foot | No data | Laser | No data | No data | No data | Significant group effects were seen with customized FOs reducing above knee muscle activity in pronated foot types compared to normal foot types. Interaction effects were seen for gastrocnemius medialis and soleus. Significant linear effects of posting level were seen for plantar pressure at the lateral rearfoot, midfoot and lateral forefoot. A group effect was also seen for plantar pressure at the medial heel. | This study provides evidence that a customized FOs can provide a dose response effect for selected plantar pressure variables, but no such effect could be identified for muscle activity. Foot type may play an important role in the effect of customized orthoses on activity of muscles above the knee. | ||||
| Telfer et al., 2013b [43] | Foot | No data | Laser | No data | No data | No data | Significant and linear effects of posting were seen for the peak and mean rearfoot eversions, peak and mean ankle eversion moments, and peak and mean knee adduction moment variables. Group effects were observed for the peak and mean forefoot abduction and for the peak knee adduction moment | These data indicate that a dose–response effect, with a linear trend for both the rearfoot and knee, exists for customized FOs used to treat pronated foot type. | ||||
| Wang et al. 2018 [44] | Hand | No data | No data | No data | No data | No data | Have acquired completed data from 13 patients. The time of them wearing the fingerboard every day varied from 1 to 8 h, and most of them reflected that they felt comfortable and there was no feeling of worsened pain or finger skin allergy. In addition, the patients’ grip strength, hand function and range of motion improved by varying degrees while their muscular tensions declined by varying degrees. The tension and bending resistance of the fingerboard all met the patients’ treatment requirements. | With the advantages of being accurate and customized, 3D printing fingerboard can benefit patients fixing and orthopedic treatment, and even prevent and treat cerebral stroke patient’s finger spasm. | ||||
| Fu et al., 2022 [45] | Ankle-Foot | Sense (2nd generation) | Optical scanner | No data | No data | Rhinoceros | The study acquired data from 10 hemiplegic stroke participants. Gait performance and Plantar Pressure for AM AFO, standard AFO and Barefoot on 10-m walking. Plantar pressure of hemiplegic leg increased at in AM AFO compared with bare foot. Contact area and peak pressure increased with AM AFO vs standard AFO and barefoot. QUEST was made to evaluate participant satisfaction. Mixed results for satisfaction obtained without statistical differences. | Dynamic plantar pressure measurement is feasible and useful for evaluation of ankle equinovarus deformity in hemiplegic stroke patients. AM AFO has at least the same ability to increased medial midfoot plantar pressures over affected leg compared with standard AFO. More medial weight bearing and more symmetric contact area over sole with AM AFO, which is more similar to physiological finding in normal subject. | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





