1. Introduction
Bariatric surgery in the last twenty years, in line with the increase in obesity, had an exponential growth.
All over the world, the number of obese and super-obese people is growing rapidly, and more and more subjects are undergoing bariatric surgery in order to avoid the serious complications related to obesity.
According to data provided by the World Health Organization (WHO), the number of obese people in the world has doubled since 1980: in 2014 over 1.9 billion adults were overweight, including over 600 million obese. (1)
Initially we speak of obese patients especially in rich countries, in recent decades we are seeing an increase in obesity even in those countries with medium or low income.
The first criteria for access to bariatric surgery were established in 1991 by the US Nation Institute of Health. (2)
With the advent of laparoscopy and robotic and its use in obesity surgery has significantly reduced complications and hospitalization times and has made these interventions more easily accessible.
Bariatric surgery, also known as weight loss surgery, is a medical intervention for individuals suffering from obesity. It is an effective method of reducing excess weight, improving health conditions and quality of life. (3)
The use of robotic surgery in bariatrics dates back to 1999. (4)
One of the main advantages of robotic surgery is its precision. Robotic devices are equipped with high-resolution cameras that provide surgeons with a clear view of the surgical site. Additionally, robotic arms can be programmed to perform very accurate movements that human hands may not be able to do. This level of precision can lead to better patient outcomes, fewer complications, and less scarring. Another benefit of robotic surgery is reduced trauma. Because the incisions made during robotic surgery are smaller than those made during traditional surgery, patients experience less tissue damage, bleeding, and pain. This results in a faster recovery time and less time spent in the hospital. (5); (6)
There are several types of surgical procedures done for weight loss, but the most common types include gastric bypass, sleeve gastrectomy and biliopancreatic diversion with duodenal switch.
1 Gastric bypass is one of the most popular weight loss surgeries performed globally. This procedure involves creating a small stomach pouch and rerouting the small intestine to it, bypassing a section of the intestine. With this, the food intake decreases, and the body absorbs fewer calories, resulting in rapid weight loss. Gastric bypass surgery can help patients achieve a significant weight loss goal, sustain long-term weight management, and resolve associated health problems like type 2 diabetes, high blood pressure, sleep apnea.
2 Sleeve gastrectomy involves the removal of 80-85% of the stomach's size. The remaining section of the stomach will resemble a narrow tube or sleeve, limiting the amount of food that can be consumed. As a result, patients feel full faster and consume fewer calories, leading to considerable weight loss. A sleeve gastrectomy also results in improvement or resolution of several co-morbidities, including high blood pressure, hyperlipidemia, gastroesophageal reflux disease (GERD), sleep apnea.
3 Revisional bariatric surgery, also known as revision bariatric surgery, is surgery performed on patients who have had previous bariatric surgery but failed to achieve the desired results or developed complications. The primary goal of revisional bariatric surgery is to correct or improve the unsatisfactory results of the initial surgery. This may include converting from a restrictive procedure to a malabsorptive or combined procedure, or vice versa, in order to achieve more significant weight loss or to reduce associated complications.
4. Since its introduction in 2007 by Torres et al. As a simplified procedure derived from BPD/DS, SADI-S has been increasingly adopted in the treatment of morbid obesity due to its reduced operative risk and weight loss and remission of metabolic disease comparable to that of BPD/DS. Although traditionally performed laparoscopically, the recent introduction of robotic surgical systems has led to the application of robotics in SADI-S procedures. SADI-S is a surgical procedure that combines mass absorption with gastric restriction, especially in recent years it is increasingly finding use for its short-term weight loss and reduction of complications compared to biliopancreatic diversion or duodenal switch. (16)
2. Materials and Methods
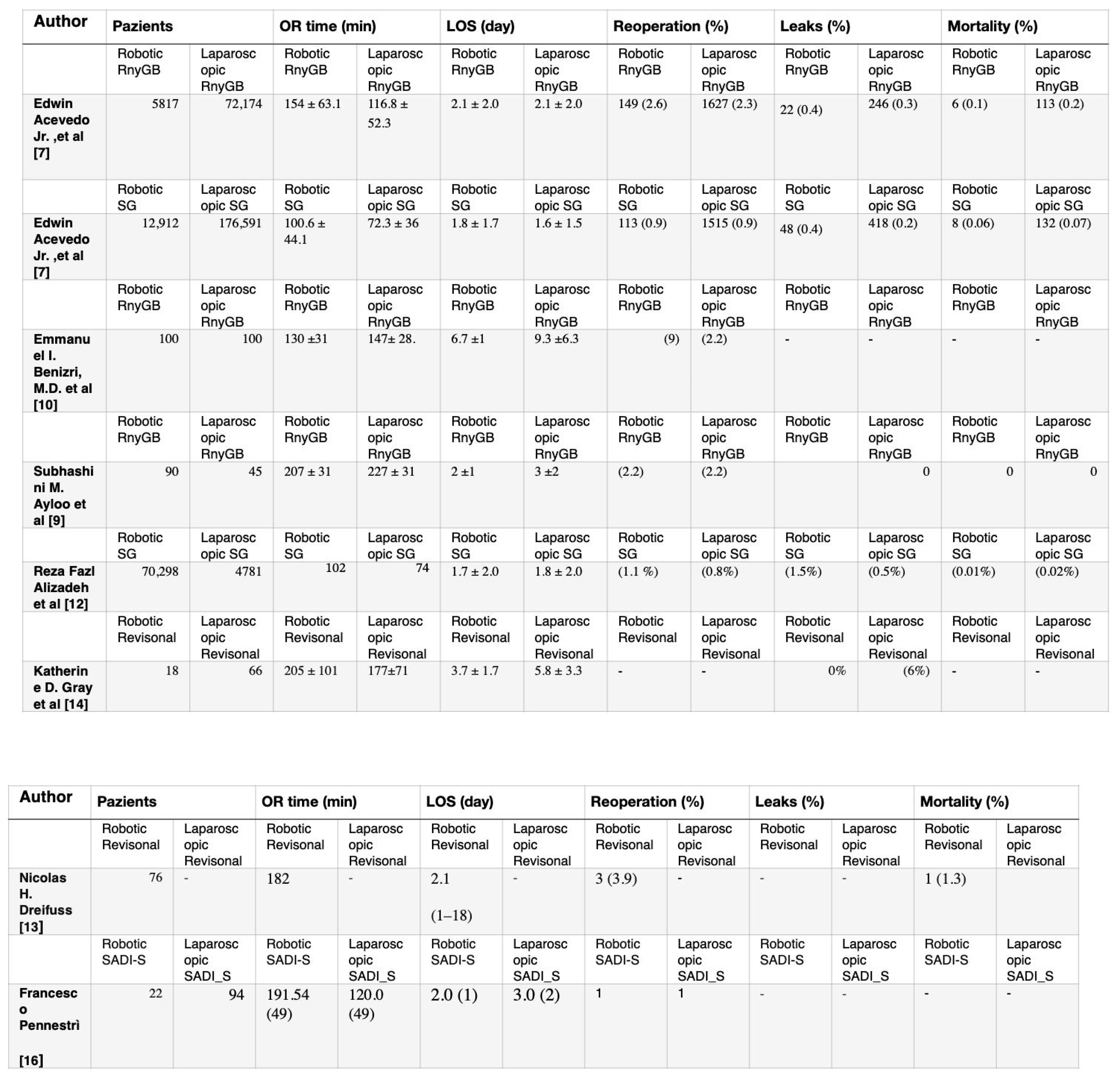
We used Pubmed and selected 10 articles that compare and analyze the use of robotic surgery and laparoscopic surgery. Only two articles selected for the amount of data, comparing laparoscopic Sleeve Gastrectomy (LSG) with robotic Sleeve Gastrectomy (RSG).
We analyzed 4 articles correlating robotic Roux-en-Y gastric bypass (R-RnYGB) versus laparoscopic Roux-en-Y gastric bypass (L-RnYGB) in terms of postoperative recovery, weight loss, pain, procedure duration and revision surgery, mortality, bleeding, transfusion, and infection.
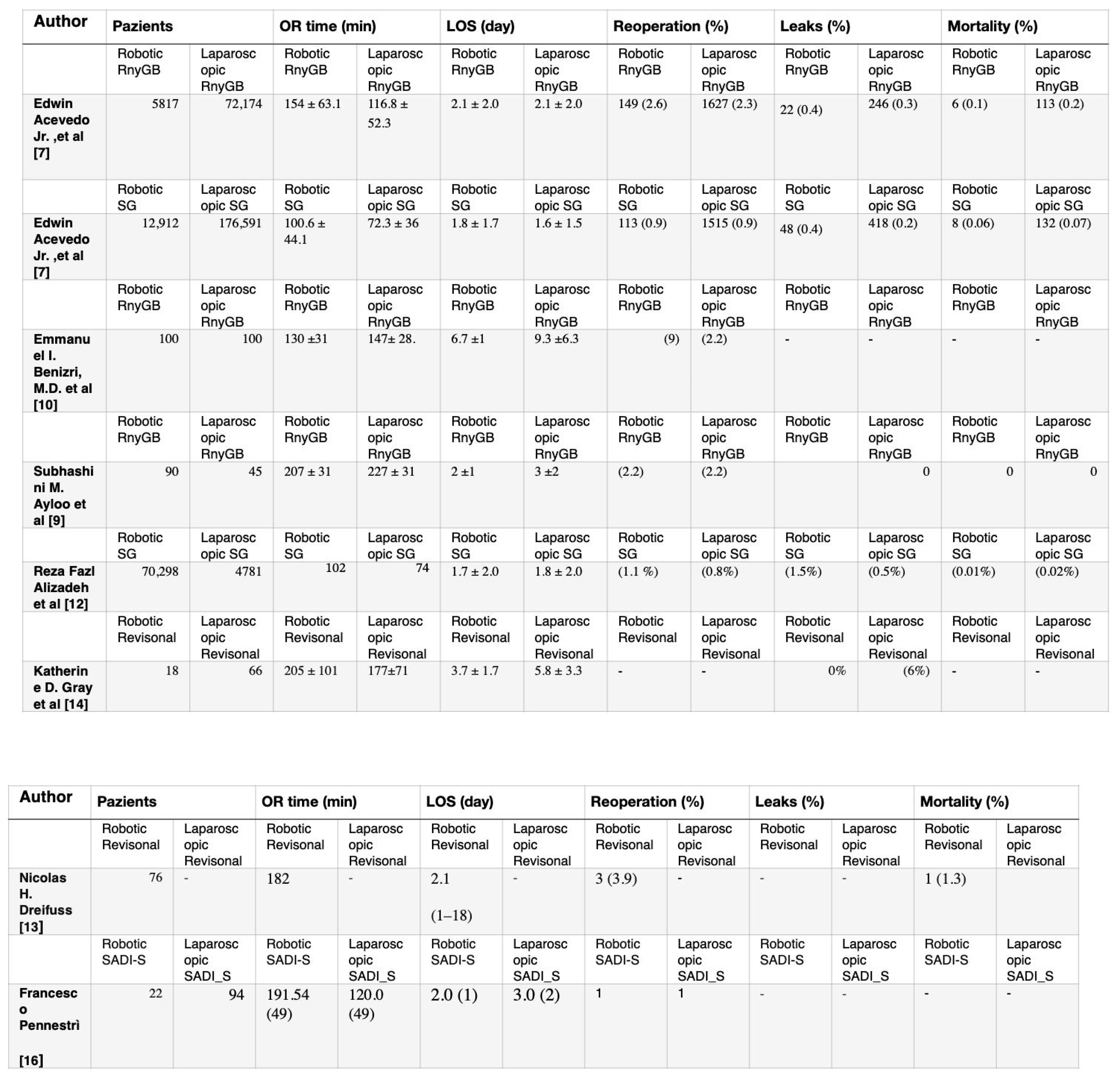
Two articles were selected to analyze the differences between Sadis Laparoscopic (L-DS) vs Sadis Robotica (R-DS).
Four articles were analyzed that compared revisional bariatric surgery (RBS), performed with laparoscopic technique or performed with robotic surgery.
In this review we will analyze operative times, bleeding, losses, hospital stay times, recovery times and weight gain, healthcare costs and clinical benefits.
3. Results
Gastric Bypass
In a study with 77,991 between 2015 and 2016 there were no substantial differences in length of stay, weight loss, weight regain.The study consistently found significantly longer operative times with the robot-assisted surgical approach, and despite controlling for operative time and conversion rate as indicators of surgeon experience, the study revealed higher and sustained readmission rates in robot-assisted cohort. The analysis reported lower rates of mortality, transfusion, superficial surgical site infection (SSI), aggregate bleeding, and aggregate wound infection in the robotic cohort. However, after adjusting for operative time and conversion rate, only superficial SSI and aggregate wound infection remained significantly lower in the robot-assisted group.. (7)
Another study between 2009 and 2016 presents a comparative analysis between robotic-assisted gastric bypass (RA-GB) and historical laparoscopic gastric bypass (L-GB) cohorts, aiming to evaluate their outcomes and safety profiles. The study includes a review of complication rates, anastomotic leaks, operative times, and percentage of excess weight loss.
The RA-GB cohort showed a lower overall complication rate than the L-GB cohort, although this difference did not persist for severe complications. RA-GB was associated with a shorter hospital stay without increasing operative time, suggesting its comparable efficacy to L-GB. Notably, the rate of revision surgery was higher in the L-GB group but was not linked to a higher complication rate, consistent with literature indicating similar adverse event rates between primary and primary gastric bypass procedures. revisional.
Regarding anastomotic leak rates, the study revealed an incidence of 3%, within the usual range reported in the literature. Notably, the anastomosis technique differed between groups, with manual anastomoses in RA-GB and mechanical anastomoses in L-GB. Literature findings regarding anastomotic leaks with robotic approaches vary, with some studies suggesting fewer leaks compared to laparoscopic methods.
Comparative studies often indicate longer operative times for RA-GB, but this study found no significant differences, aligning with some reports suggesting better operative times with greater experience in robotic procedures.(8)
The study by Subhashini M. Ayloo et al. compares patient demographics, intraoperative characteristics, and postoperative outcomes between robot-assisted gastric bypass (R-RYGBP) and laparoscopic gastric bypass (L-RYGBP) procedures. In the R-RYGBP group, there was a significantly younger cohort of patients, with statistically significant differences in age compared to the L-RYGBP group.
Operative times in the R-RYGBP group averaged 207 minutes, of which approximately 57 minutes were dedicated to performing the gastrojejunostomy anastomoses and an average robot setup time of 13 minutes. Overall, R-RYGBP procedures were completed in less time than L-RYGBP procedures (average 207 versus 227 minutes).
Both groups showed no mortality and early morbidity rates were comparable, except for one patient in each group who experienced specific complications: a gastrointestinal leak from the excluded stomach in the L-RYGBP group and a pulmonary embolus in the R-RYGBP group.
The length of hospital stay was shorter for patients receiving R-RYGBP compared to L-RYGBP (mean 2 vs. 3 days). Readmissions were more frequent in the R-RYGBP group, mainly for dehydration and abdominal pain, although the difference was not statistically significant.Late morbidity, however, was significantly higher in the L-RYGBP group than in the R-RYGBP group, with four cases in the former and only one in the latter. This late morbidity included gastrojejunostomy stricture and marginal ulcers.
Regarding the follow-up results, the average excess weight loss in the R-RYGBP group showed a positive trend at 3 months, 6 months and 1 year after surgery. However, no statistically significant difference was observed between the R-RYGBP and L-RYGBP groups in terms of excess weight loss during the follow-up period.
Use of the robot to perform gastrojejunostomy during laparoscopic Roux-en-Y gastric bypass did not increase operative time, complications, or mortality. The results of the robot-assisted procedure are comparable to those found with the conventional laparoscopic method. (9)
In a study in the 2013 a total of 736 surgeries in opposition to much of the literature noted an increase in leak, complications, bleeds, and open conversions in robotic versus laparoscopic surgeries. (10)
Sleeve Gastrectomy
In the comparative analysis of over 35,000 cases of sleeve gastrectomy, the robotic-assisted version was found to be associated with a significantly longer operative duration (p < 0.0001) and a prolonged post-operative hospital stay (p < 0. 0001). Most perioperative outcomes were similar between the robotic-assisted and laparoscopic sleeve gastrectomy groups. Some outcomes were more common in the robotic-assisted intervention group, including intervention at 30 days (p = 0.01), presence of drainage at 30 days (p < 0.0001), sepsis (p = 0.01 ) and contamination of organic cavities. Although we did not find higher rates of hospitalization and reoperation in our robotically assisted gastrectomy group.
There was a lower rate of transfusions (p = 0.07) and overall bleeding complications (p = 0.05) in the robotically assisted gastrectomy group. A 4.5-fold decrease in aggregate renal complications was also observed in the group of patients treated with robotic-assisted surgery. The reported higher rates of bleeding complications in laparoscopic versus robotic-assisted sleeve gastrectomy remain unclear and require further study. After controlling for operative duration and conversion rate in our subsequent 1:3 case-control analysis, most outcomes did not change. However, the rate of intra-operative or post-operative transfusion became significantly higher (p = 0.01) in the conventional laparoscopic gastrectomy group.(11)
Laparoscopy is the standard surgical approach for sleeve gastrectomy. However, robotically assisted sleeve gastrectomy (RSG) is an alternative procedure performed only in a few select centers. This study with 75 patients compared outcomes between RSG and laparoscopy (LSG) using a national database of accredited bariatric centers. There was a low rate of use of RSG, with only 6.4% of all sleeve gastrectomy cases performed with this approach. RSG has been associated with a higher rate of serious complications, as well as higher rates of escape and surgical site infections.
This study identified higher escape and greater severe morbidity with RSG compared to LSG. A possible explanation for the increase in interference in RSG could be linked to the surgeon's learning curve in its use. However, there is no established minimum caseload for proficiency in robotically assisted sleeve gastrectomy, and the MBSAQIP database does not provide data on surgeon experience with RSG.
RSG has been associated with longer operative times than LSG, and the costs of robotic equipment are significantly higher. However, cost data were not available in the MBSAQIP database. Previous studies have reported higher costs for RSG compared to LSG. Regarding the length of hospital stay, there are no consistent findings across series of published studies. (12)
Revisional Bariatric Surgery
Robotic surgery is finding more and more use in revisional bariatric surgery. In a study of 454 patients undergoing revision surgery, procedures performed in robotic surgery were compared with those performed in laparoscopy. Robotic surgeries are characterized by a longer duration, fewer bleedings, leaks, lower conversion rates and shorter length of hospital stay. (13) A retrospective review was conducted of adult patients undergoing laparoscopic revisional bariatric surgery (LRBS) or robotic revisional bariatric surgery (RRBS) from September 2007 to December 2016. A total of 84 patients underwent revision surgery 47 patients for weight regain the remaining patients were revised for anatomic complications . It has been noted how complications increase in revision surgery and how the use of robotic surgery in more complex operations helps to reduce complication rates, hospital stays and may reduce conversions to open surgery.
In a retrospective study the conversion rate in robotic vs. laparoscopic revision surgery was analyzed, noting that the conversion rates to open surgery were higher in patients operated on in robotics, but the robotic approach was used for more complex interventions. (15)
Edwin Acevedo et. represents one of the largest retrospective case control studies with 26,404 revision cases. Revisional bariatric surgery is known for higher mortality and morbidity rates than primary procedures. This study compares perioperative outcomes of laparoscopic and robotic revisional bariatric surgery via a retrospective analysis of the MBSAQIP PUF database.
The Analysis found that robot-assisted bariatric surgery required longer operating times, prolonged hospital stays, and more complications than conventional laparoscopy. While most results were similar between gastric bypass and sleeve gastrectomy groups, robot-assisted surgery showed higher rates of complications in specific indicators in sleeve gastrectomy, reporting higher rates of conversion, reoperation, readmission, among others .(11)
SADI-S
Francesco Pennestrì et all. analyze 116 patients underwent SADIS, 85 (73.3%) for primary procedure and 31 (26.7%) for revisional one.
This study presents the results of a single anastomosis duodenoileal bypass with sleeve gastrectomy (SADIS) in a high-volume bariatric center in Italy, focusing on different surgical approaches. This single-center study is the first case-control analysis comparing these approaches in the Italian context, covering 116 patients, evaluating both laparoscopic and robotic methods. The study strategically suggests the robotic approach for complex cases, particularly in patients with high BMI or previous abdominal surgeries, where the advantages of the robotic system, such as three-dimensional visualization and wrist-worn instruments, facilitate complex laparoscopic tasks such as suturing.
Furthermore, recent robotic platforms provide multi-quadrant access without repositioning, facilitating complex bariatric surgeries. Data shows longer operative times for robotic procedures compared to laparoscopy, but the learning curve has demonstrated a reduction in operative time in cases.
Earlier complications occurred in the robotic group, but overall complication rates were comparable between the laparoscopic and robotic approaches.
Addressing challenges in cost analysis and the need for larger comparative studies with extended follow-ups, the results suggest the safety and efficacy of SADIS across all surgical approaches. Laparoscopic procedures show advantages in terms of operative time, the robotic approach could be promising in managing complex cases, potentially reducing the need for multi-stage procedures (17)
Lun Wang et all. marks the first attempt to estimate the learning curve associated with fully robotic SADI-S. The results indicate that the learning curve for this approach includes 27 cases. Surgeons intending to perform robotic SADI-S should undergo structured robotic training to effectively address the initial learning phase.
This study demonstrates the feasibility of a fully robotic SADI-S in the management of morbid obesity, with a short-term complication rate of 6.9%, of which major complications were identified in 2.9% of cases. Notably, no statistical difference in morbidity was observed between the initial 27 patients (learning phase) and the subsequent 75 patients (mastery phase), suggesting relative safety during the initial phase of the learning curve.
Operative time averaged 186 minutes, aligning with the range reported for robotic SADI-S in previous literature. A tendency towards an increase in operating time, especially in the initial phase, reflects the surgeon's competence linked to greater surgical experience. However, the abnormal increases in operative time observed in some patients during the late phase were due to double measurement of small bowel length using different methods during surgery.
Comparison with laparoscopic SADI-S results revealed similar short- and long-term complication rates, although this study reported a longer mean operative time and hospital stay. Notably, the robotic approach produced weight outcomes comparable to laparoscopic SADI-S despite differences in technique and patient demographics.
Robotic SADI-S, while showing similar outcomes to laparoscopic procedures, presents concerns regarding the perceived higher costs associated with robotic surgery.
This retrospective study, although the largest to date on outcomes of fully robotic SADI-S, requires further investigation to clarify the comparative advantages and cost implications of robotic versus laparoscopic SADI-S through controlled studies with rigorous methodologies .(18)
4. Discussion
Bariatric surgery offers numerous benefits.
The primary benefit of bariatric surgery is significant and sustained weight loss. Patients can lose 50% or more of their excess weight following bariatric surgery. (19)
Bariatric surgery has been shown to improve or resolve several co-morbidities, including type 2 diabetes, high blood pressure, sleep apnea, hyperlipidemia, GERD, etc. Furthermore, bariatric surgery seems to play a role in the treatment of infertility of obese women (20), showing encouraging results also in those intending to undergo an assisted reproductive technology treatment. (21)
It can lead to improved quality of life by reducing obesity-related physical limitations, enhancing self-esteem, improving body image, and increasing social activity.
Bariatric surgery is a viable option for people struggling with obesity who have tried unsuccessfully to lose weight through traditional methods. While the procedure does carry some risks, the potential benefits can be life-changing for patients who commit to making significant lifestyle changes after surgery. It is important to discuss all options with a qualified healthcare professional to determine the best course of action for individual needs, also considering the complications associated with bariatric surgery such as malabsorption and micronutrients deficiency (22)
Bariatric surgery, a major procedure used to treat obesity and related conditions, has seen significant advancement with the introduction of robotic technology. However, an evaluation of the existing evidence shows conflicting results regarding the effectiveness, safety and costs associated with the use of robotic surgery compared to laparoscopy, especially in different types of bariatric surgeries such as gastric bypass, sleeve gastrectomy, revisional bariatric surgery and the SADI-S.
An analysis of a study of more than 77,000 patients in 2015-2016 found no significant differences in length of stay, weight loss, and weight regain between robotic surgery and laparoscopy. However, it was found that the robotic surgical approach required longer operating times and had higher remission rates, although some morbidity indicators, such as superficial surgical site infections and wound infections, were lower in the robotic group.
Another comparative study between robotic and laparoscopic gastric bypass surgery revealed a reduced incidence of overall complications in the robotic group, with shorter hospital stay times, suggesting comparable effectiveness between the two approaches. However, robotic surgery appeared associated with a higher frequency of revision surgery in the laparoscopic group, although it did not correlate with an increase in complications.
With respect to anastomotic leak rate comparisons, the analyzes differentiated the anastomosis techniques used between the two groups, showing in some studies less leakage with the robotic approach compared to the laparoscopic one. Although some studies indicate longer operating times for the robotic approach, others suggest that with increasing experience in robotic procedures, times may improve.
When performing sleeve gastrectomy surgery, a comparative analysis of more than 35,000 cases found significantly longer operative duration and prolonged hospital stay in the robotic approach, with some more frequent complications such as sepsis and organ cavity contamination. However, one of the aggregate renal problems was reported in the group of patients who underwent robotic surgery.
In the specific case of SADI-S (single anastomosis duodeno-ileal switch), a comparative analysis between the laparoscopic and robotic approaches highlighted a longer operative duration for robotic procedures, but with a comparable level of short- and long-term interactions term compared to laparoscopic surgery.
While robotic surgery may have technical advantages, such as three-dimensional visualization and wrist-worn instruments, it may require longer operating times and higher costs. However, experience and practice can reduce operating times and improve the effectiveness of robotic surgery, making it a valid option in particular complex cases.
Ultimately, despite the advances in robotic surgery, more research is needed to fully understand the benefits, costs, and best practices in applying robotic technology in different bariatric procedures. Long-term prospective and randomized studies are essential to delineate the role of robotic surgery and compare its advantages and disadvantages compared to laparoscopic surgery in bariatric surgery.
We can note that there are still very few studies on robotic bariatric surgery but among those analyzed we can say that the use of the robot in bariatric surgery is safe and a valid treatment option, without a significant increase in complications and mortality compared at laparoscopy. Almost all the studies analyzed report a longer duration of robotic interventions but no other significant difference. In revisional bariatric surgery and gastric bypass it seemed to have a slightly lower complication rate than laparoscopic surgery, in terms of bleeding and leaks.
5. Conclusions
While robotic surgery demonstrates technical advantages such as enhanced visualization and specialized instruments, it often entails lengthier operative times and heightened expenses. Comparative studies reveal varying outcomes across different bariatric procedures, suggesting a nuanced landscape where robotic approaches exhibit comparable effectiveness in some aspects but might also entail specific drawbacks like longer hospital stays or certain complications.
The current body of research on robotic bariatric surgery remains limited, yet the available evidence suggests that, overall, robotic interventions seem safe and a valid treatment option.
Author Contributions
Conceptualization, A.V. and P.A.; methodology, S.N.; software, P.A.; validation, G.N., A.V., P.A. and N.S.; formal analysis, A.V.; investigation, A.V.; data curation, A.V., G.N; writing—original draft preparation, A.V., P.A; writing—review and editing, A.V., P.A.; supervision, G.N.; project administration, A.V..
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Federico II University of Naples.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Table
References
- (https://www.epicentro.iss.it/obesita/epidemiologia-mondo).
- Consensus Development Conference Panel. NIH conference: gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;115(12):956-961. [CrossRef]
- Musella M, Milone M, Gaudioso D, et al. A decade of bariatric surgery. What have we learned? Outcome in 520 patients from a single institution. Int J Surg. 2014;12 Suppl 1:S183-S188. [CrossRef]
- Cadiere GB, Himpens J, Vertruyen M, Favretti F. The world’s first obesity surgery performed by a surgeon at a distance. Obes Surg 1999;9:206-9. ).
- Talamini MA, Chapman S, Horgan S, Melvin WS, Academic Robotics Group. A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc 2003;17:1521-4.
- Bindal V, Bhatia P, Kalhan S, Khetan M, John S, Ali A, et al. Robot-assisted excision of a large retroperitoneal schwannoma. JSLS 2014;18:150-.
- Outcomes in conventional laparoscopic versus robotic-assisted primary bariatric surgery: a retrospective, case–controlled study of the MBSAQIP database .Edwin Acevedo Jr.1 · Michael Mazzei1 · Huaqing Zhao2 · Xiaoning Lu2 · Rohit Soans1 · Michael A. Edwards3 ).
- Less Morbidity with Robot-Assisted Gastric Bypass Surgery than with Laparoscopic Surgery? J. Cahais1 & R. M. Lupinacci1 & O. Oberlin1 & N. Goasguen1 & K. Zuber2 & A. Valverde1.
- Robot-assisted versus Laparoscopic Roux-en-Y Gastric Bypass: Is There a Difference in Outcomes? Subhashini M. Ayloo • Pietro Addeo • Nicolas Christian Buchs • Galaxy Shah • Pier Cristoforo Giulianotti.
- Perioperative outcomes after totally robotic gastricbypass: a prospective nonrandomized controlled studyEmmanuel I. Benizri, M.D.a,b,*, Myriam Renaud, M.D.a, Nicolas Reibel, M.D.a,Adeline Germain, M.D.a, Olivier Ziegler, M.D.a,c,d, Rasa Zarnegar, M.D.e,Ahmet Ayav, M.D.a, Laurent Bresler, M.D.a, Laurent Brunaud, M.D.a.
- Outcomes in conventional laparoscopic versus robotic-assisted revisional bariatric surgery: a retrospective, case–controlled study of the MBSAQIP database Edwin Acevedo1 · Michael Mazzei1 · Huaqing Zhao2 · Xiaoning Lu2 · Michael A. Edwards1,3.
- Robotic versus laparoscopic sleeve gastrectomy: a MBSAQIP analysis Reza Fazl Alizadeh1 · Shiri Li1 · Colette S. Inaba1 · Andreea I. Dinicu1 · Marcelo W. Hinojosa1 · Brian R. Smith1 · Michael J. Stamos1 · Ninh T. Nguyen1.
- Robotic Revisional Bariatric Surgery: a High-Volume Center Experience Nicolas H. Dreifuss1 & Alberto Mangano1 & Chandra Hassan1 & Mario A. Masrur1.
- Perioperative Outcomes of Laparoscopic and Robotic Revisional Bariatric Surgery in a Complex Patient Population Katherine D. Gray1 & Maureen D. Moore1 & Adham Elmously1 & Omar Bellorin1 & Rasa Zarnegar1 & Gregory Dakin1 & Alfons Pomp1 & Cheguevara Afaneh1,2.
- Moon, R.C.; Segura, A.R.; Teixeira, A.F.; Jawad, M.A. Feasibility and safety of robot-assisted bariatric conversions and revisions. Surg. Obes. Relat. Dis. 2020, 16, 1080–1085. [Google Scholar] [CrossRef] [PubMed]
- Single Anastomosis Duodeno-Ileal Switch (SADIS): A Systematic Review of Efficacy and Safety. Saeed Shoar1 & Lauren Poliakin1 & Rebecca Rubenstein1 & Alan A. Saber1.
- Robotic vs. laparoscopic approach for single anastomosis duodenal-ileal bypass with sleeve gastrectomy: a propensity score matching analysis Francesco Pennestrì1,3 · Luca Sessa1,2 · Francesca Prioli1,3 · Pierpaolo Gallucci1 · Luigi Ciccoritti1 · Francesco Greco1 · Carmela De Crea1,3 · Marco Rafaelli1,3.
- Outcomes of totally robotic single-anastomosis duodenaleileal bypass with sleeve gastrectomy: A large single-centre series Lun Wang, Zeyu Wang, Tao Jiang.
- Abdul Wahab R, le Roux CW. A review on the beneficial effects of bariatric surgery in the management of obesity. Expert Rev Endocrinol Metab. 2022 Sep;17(5):435-446. Epub 2022 Aug 10. [CrossRef] [PubMed]
- Musella M, Milone M, Bellini M, et al. The potential role of intragastric balloon in the treatment of obese-related infertility: personal experience. Obes Surg. 2011;21(4):426-430. [CrossRef]
- Milone M, Sosa Fernandez LM, Sosa Fernandez LV, et al. Does Bariatric Surgery Improve Assisted Reproductive Technology Outcomes in Obese Infertile Women?. Obes Surg. 2017;27(8):2106-2112. [CrossRef]
- Milone M, Di Minno MN, Lupoli R, et al. Wernicke encephalopathy in subjects undergoing restrictive weight loss surgery: a systematic review of literature data. Eur Eat Disord Rev. 2014;22(4):223-229. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).