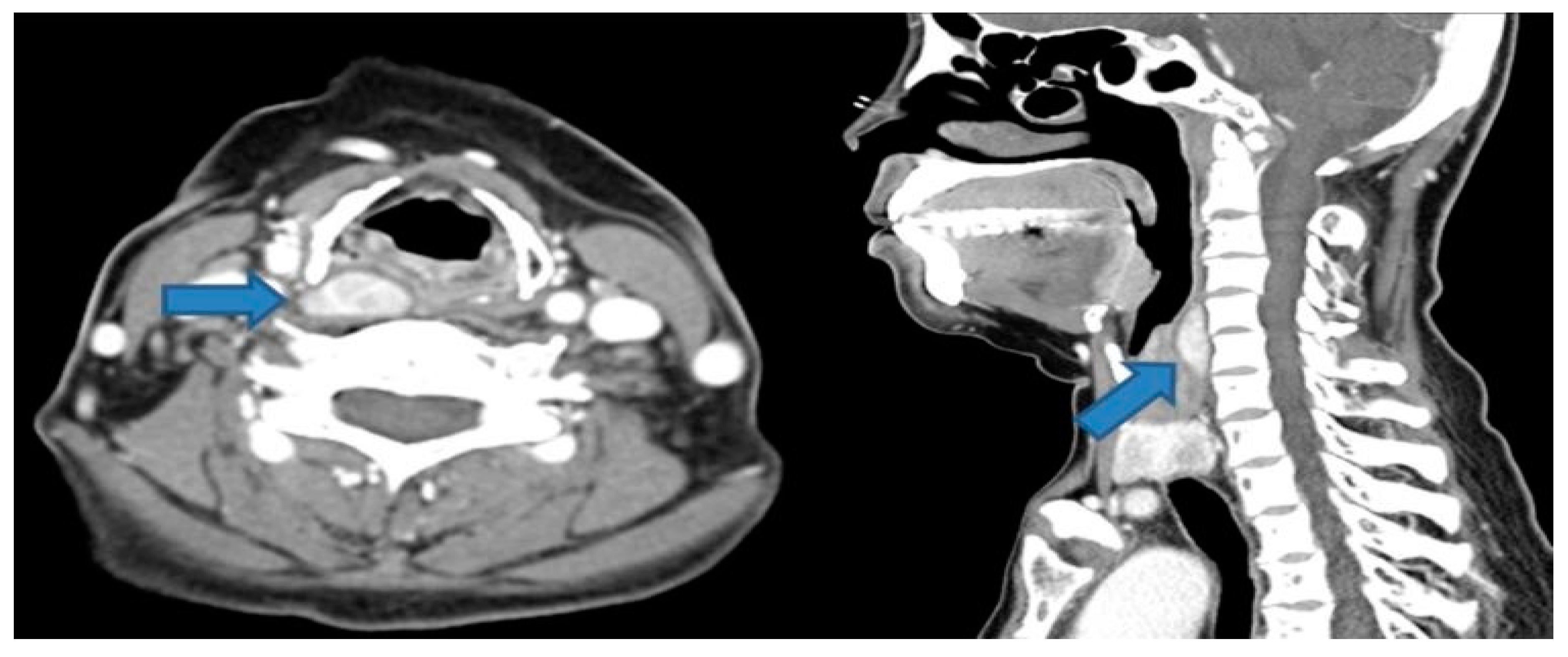
Figure 1.
Preoperative enhanced neck CT shows about 2.6cm well-defined mass in the right retropharyngeal space at the level of upper thyroid cartilage (blue arrow). Suspicious lesion in the retropharynx is marked with blue arrows. A 51-year-old female patient with end-stage renal disease on dialysis was referred by the nephrology department due to suspected osteoporosis and the presence of osteoblastic lesions. Laboratory results indicated elevated serum calcium and parathyroid hormone levels, accompanied by decreased bone mineral density. Subsequent cervical computed tomography (CT) scans displayed a well-defined enhancing mass measuring about 2.6cm in the retropharyngeal space at the upper level of the right thyroid cartilage. (
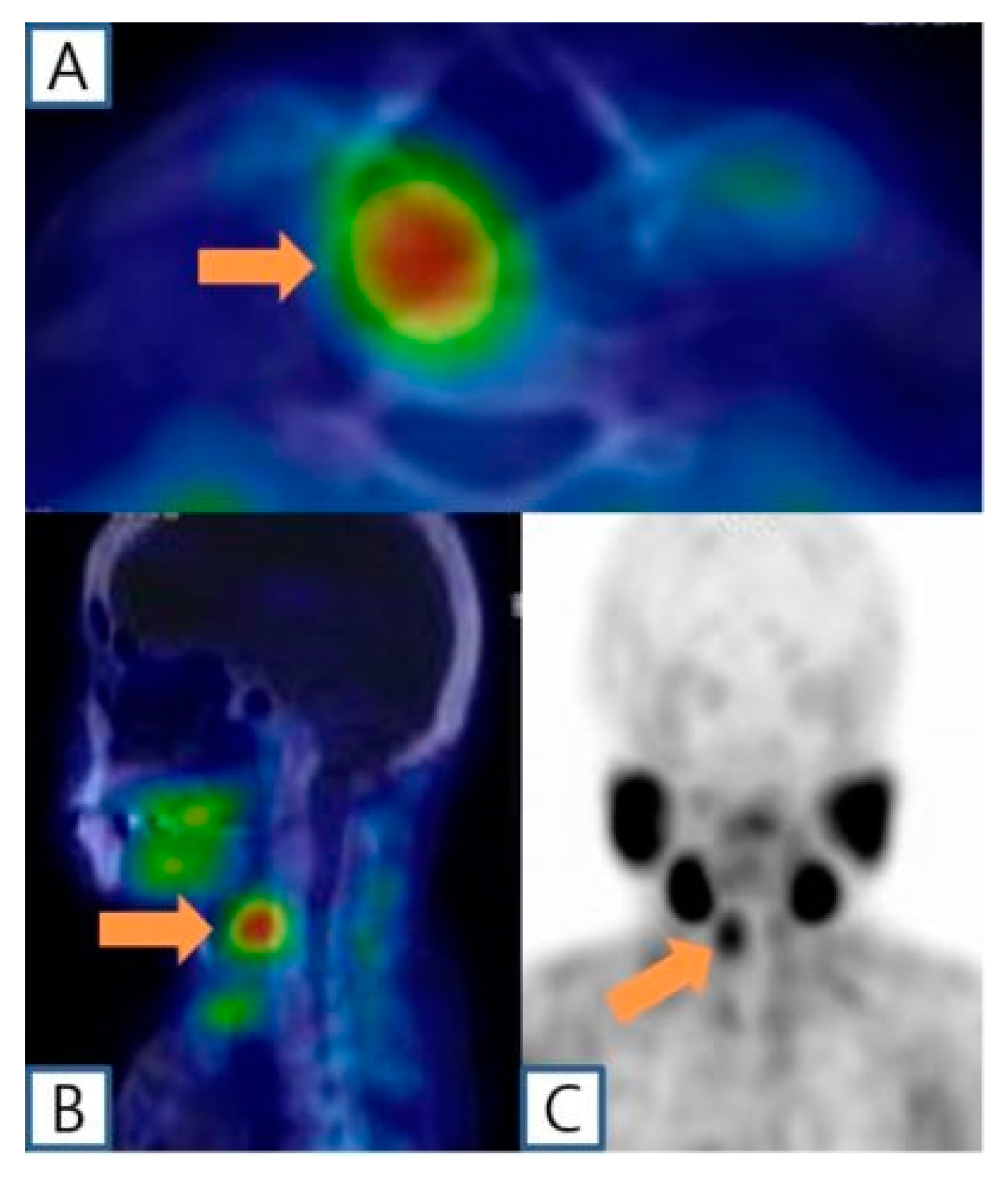
Figure 1.) Based on clinical symptoms and radiological findings, additional parathyroid imaging was performed to precisely locate the suspected parathyroid adenoma. The parathyroid scan showed the presence of an upper right parathyroid adenoma in the retropharyngeal region, prompting the patient to seek surgical consultation. (
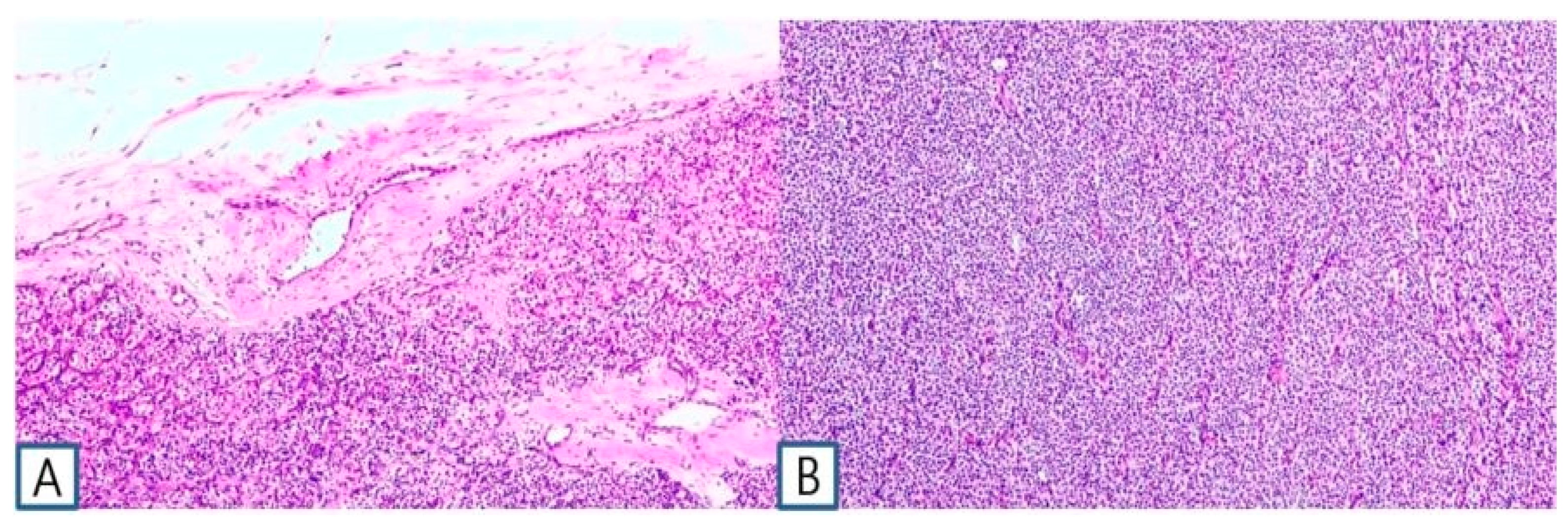
Figure 2.) A transverse incision of approximately 5cm was made slightly to the right of the midline of the neck, exposing the sternocleidomastoid (SCM) muscle. Following the lateral retraction of the SCM muscle, the right thyroid gland was discerned, and an incision was performed to reach the retropharyngeal space at the hyoid bone level. Enlarged lymph nodes were observed in the adjacent region, and by gently displacing the thyroid to the left, the parathyroid mass situated in the retropharyngeal space was revealed. Careful dissection was carried out to separate the retropharyngeal mass from the surrounding tissues. A portion of the excised mass was subjected to frozen section analysis, confirming its parathyroid origin. Intraoperative intact parathyroid hormone(iPTH) levels were measured and revealed a gradual reduction after the removal of the mass. The iPTH levels decreased to within the normal range on serum testing 20 minutes after tumor removal. Lobectomy was performed through conventional techniques without injury to the recurrent laryngeal nerve and inferior parathyroid gland. No postoperative complications were observed, and the patient was discharged on the 5th day post-surgery with maintained normal parathyroid hormone levels. Subsequent pathology results of the thyroid nodule confirmed papillary thyroid cancer with no extrathyroidal extension or neural involvement and the retropharyngeal mass was diagnosed as a parathyroid adenoma. (
Figure 3.) Ultimately, significant clinical improvement was achieved, and the patient is under regular observation and follow-up. pHPT is a common endocrine disorder characterized by the excessive secretion of parathyroid hormone, leading to hypercalcemia, which can manifest with symptoms such as osteoporosis, generalized weakness, and, in severe cases, altered consciousness. It occurs in approximately 1 in 500 women and 1 in 2,000 men, and the primary treatment involves the complete removal of hyperfunctioning parathyroid tissue [
1]. The majority of parathyroid tumors encountered in clinical practice are identified during the diagnostic workup for pHPT, which is characterized by hypercalcemia and elevated parathyroid hormone levels. Parathyroid adenomas exhibiting tissue invasion and lacking concurrent hyperparathyroidism are uncommon [
2]. Additionally, primary hyperparathyroidism can be induced by causes such as parathyroid hyperplasia, multiple parathyroid adenomas, and parathyroid carcinoma [
3]. Even in the absence of symptoms, the hyperfunction of the parathyroid glands should be treated with complete excision to prevent life-threatening arrhythmias and associated severe complications [
4]. Therefore, precise localization of the parathyroid tumor along with accurate excision is crucial for the effective management of this condition [
5]. The parathyroid glands exhibit considerable variation in their locations, and the superior parathyroid glands are commonly situated in proximity to the superior thyroid artery, constituting around 80% of cases. This description pertains to the localization of the superior parathyroid gland, and deviations in the position of the parathyroid glands may arise due to congenital displacement and other contributing factors. Variability also exists in the position and migration path between superior and inferior parathyroid glands, with superior parathyroid gland location changes being less frequent compared to the inferior parathyroid glands. These variations are attributed to embryological reasons. Ectopic parathyroid glands are known to occur frequently in cases of recurrent hyperparathyroidism after initial parathyroidectomy [
6]. However, in the present case, where there was no prior surgical history, the occurrence in the retropharyngeal space highlights the utility of technetium scanning for preoperative diagnosis. Localization of parathyroid tumors has employed various methods, including ultrasound, computed tomography, and nuclear imaging with technetium (Tc) 99m sestamibi. Neck ultrasound showed the least diagnostic accuracy at 84%, whereas computed tomography and Tc 99m scans presented higher accuracy rates of 92% and 90%, respectively. Isolated parathyroid adenomas have the potential to emerge at any anatomical site along their embryological descent pathway, with the mediastinum being the predominant location, constituting approximately 38%. In approximately 18% of instances, they may be localized within the thyroid gland itself. In uncommon cases, their origin may be traced to the parapharyngeal space [
7]. The incidence of concurrent thyroid cancer and pHPT varies between 3.1% and 17%, and there is ongoing debate surrounding the underlying reasons for this correlation [
8]. While certain authors attribute this simultaneous presence to chance, alternative researchers propose a connection to elevated endogenous calcium levels or potential involvement of growth factors like epithelial growth factors and insulin-like growth factors, suggesting their role as goitrogenic factors [
9,
10]. It is significant to highlight in this case that the incident occurred in the absence of any previous head and neck irradiation history. While the concurrent presence of thyroid cancer and parathyroid adenoma is infrequent, it is crucial to entertain the diagnosis of this co-occurrence in cases of pHPT to avert the necessity for reoperation, as exemplified in our patient's case. A comprehensive understanding of pHPT is imperative when considering surgery for parathyroid tumors, as is a thorough understanding of the anatomical location and variations of the parathyroid glands. Demonstrated in this case, the emergence of a parathyroid adenoma in the retropharyngeal space emphasizes the need for thorough assessment to avoid misinterpretation as a distinct condition associated with thyroid cancer. Additionally, the assessment of anatomical variations through the application of appropriate diagnostic tools can prove beneficial in guiding decisions related to the clinical presentation, diagnostic approaches, surgical treatment, and surgical strategies for parathyroid tumors.