Submitted:
01 December 2023
Posted:
04 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
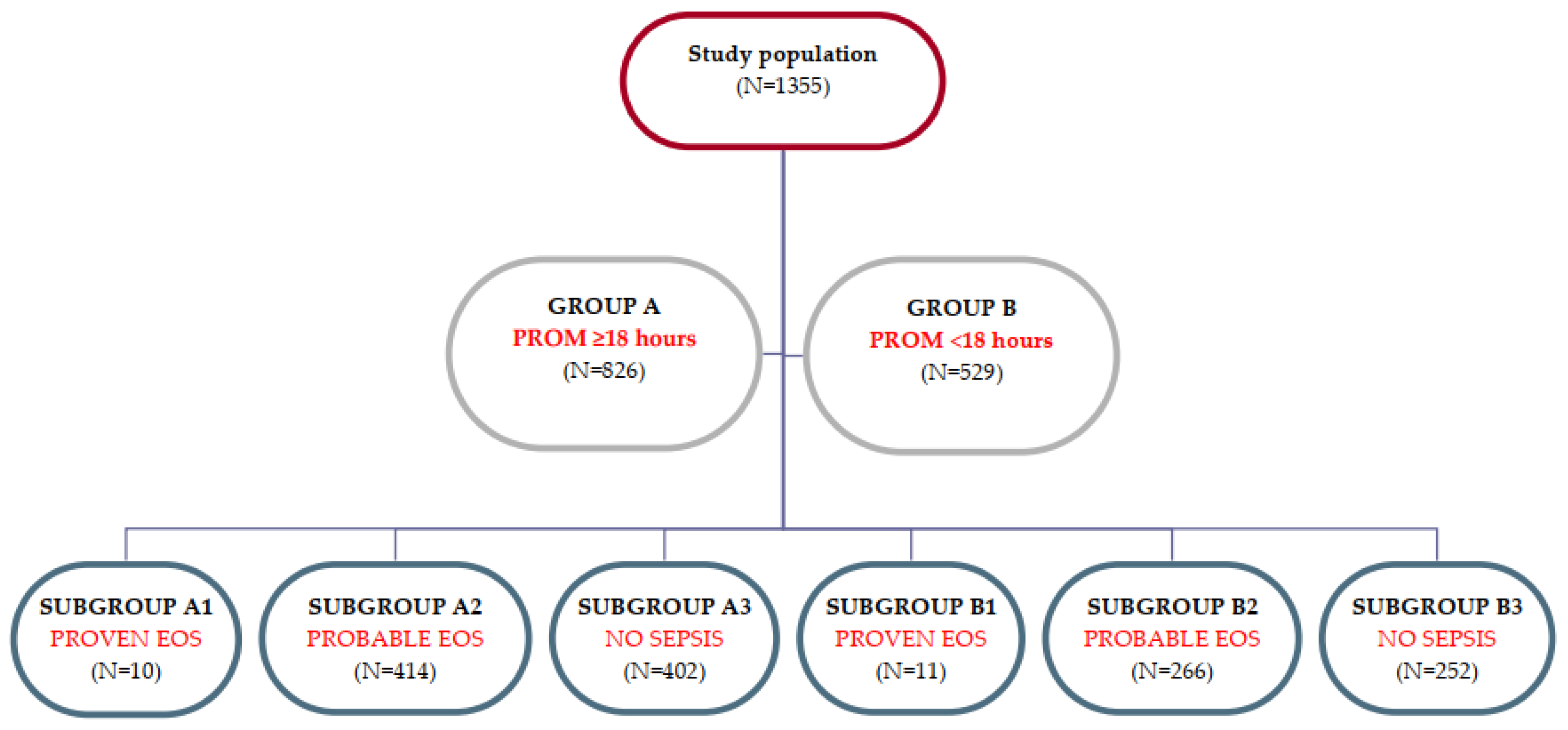
2.1. Study design
2.2. Definitions and study population
2.3. Statistical analysis
3. Results
| PROM ≥18 hours (group A) N=826 |
PROM <18 HOURS (GROUP B) n=529 |
P value | |
|---|---|---|---|
| GA mean ± SD | 36.15 ± 3.9 | 37.83 ± 2.528 | <0.001 |
| Preterm* | 332 | 86 | <0.001 |
| BW mean ± SD | 2730.3 ± 857.7 | 3146.3 ± 636.2 | <0.001 |
| CS | 371 | 245 | 0.615 |
| VB | 455 | 284 | 0.614 |
| Male | 419 | 307 | 0.009 |
| Female | 407 | 222 | 0.009 |
| Apgar 1 min - median | 7 | 8 | <0.001 |
| Apgar 5 min - median | 8 | 9 | <0.001 |
| Apgar 10 min - median | 8 | 9 | <0.001 |
| Proven EOS (A1) N=10 |
Proven EOS (B1) N=11 |
P value | Probable EOS (A2) N=414 |
Probable EOS (B2) N=266 |
P value | No sepsis (A3) N=402 |
No sepsis (B3) N=252 |
P value | |
|---|---|---|---|---|---|---|---|---|---|
| GA (mean ± SD) | 29.5 ± 4.3 | 35.3 ± 3.1 | 0.002 | 35.6 ± 4.3 | 37.6 ± 3.1 | <0.001 | 36.8 ± 3.1 | 38.1 ± 1.6 | <0.001 |
| Preterm* | 9 | 7 | 0.157 | 185 | 46 | <0.001 | 138 | 32 | <0.001 |
| BW (median) | 1484 | 2636 | 0.005 | 2605 | 3109 | <0.001 | 2889 | 3250 | <0.001 |
| CS | 4 | 8 | 0.130 | 188 | 123 | 0.519 | 179 | 114 | 0.969 |
| VB | 6 | 3 | 0.130 | 226 | 143 | 0.832 | 223 | 138 | 0.859 |
| Male | 6 | 8 | 0.014 | 204 | 152 | 0.045 | 213 | 147 | 0.181 |
| Female | 4 | 3 | 0.016 | 210 | 114 | 0.045 | 189 | 105 | 0.181 |
| Apgar 1 min (median) | 6 | 7 | 0.475 | 8 | 8 | <0.001 | 8 | 9 | <0.001 |
|
Apgar 5 min (median) |
7 | 8 | 0.453 | 8 | 9 | 0.004 | 9 | 9 |
<0.001 |
|
Apgar 10 min (median) |
7 | 8 | 0.413 | 8 | 9 | 0.006 | 9 | 9 | <0.001 |
| Duration of stay (mean ± SD) | 52.10 ± 40.5 | 22.73 ± 12.1 | <0.005 | 18.80 ± 24.6 | 9.75 ± 17.1 | <0.001 | 10.92 ± 15.1 | 4.81 ± 3.8 | <0.001 |
| Proven EOS (A1) N=10 |
Proven EOS (B1) N=11 |
P value | Probable EOS (A2) N=414 |
Probable EOS (B2) N=266 |
P value | No sepsis (A3) N=402 |
No sepsis (B3) N=252 |
P value | |
|---|---|---|---|---|---|---|---|---|---|
| Positive amniotic fluid culture | 5 | 0 | 0.007 | 58 | 15 | 0.001 | 19 | 8 | 0.83 |
| Foul smelling amniotic fluid | 2 | 3 | 0.28 | 41 | 27 | 0.41 | 16 | 16 | 0.739 |
| Maternal fever | 1 | 1 | 0.94 | 6 | 3 | 0.72 | 1 | 0 | 0.428 |
| Maternal inflammatory markers | 0 | 0 | - | 5 | 6 | 0.29 | 1 | 0 | 0.428 |
| Proven EOS (A1) N=10 |
Proven EOS (B1) N=11 |
P value | Probable EOS (A2) N=414 |
Probable EOS (B2) N=266 |
P value | No sepsis (A3) N=402 |
No sepsis (B3) N=252 |
P value | |
|---|---|---|---|---|---|---|---|---|---|
| Short term complications | |||||||||
| RDS | 9 | 7 | 0.157 | 134 | 57 | 0.002 | 68 | 5 | <0.001 |
| PPHN | 1 | 0 | 0.28 | 7 | 7 | 0.399 | 2 | 0 | 0.262 |
| Pulmonary hemorrhage | 0 | 1 | 0.329 | 1 | 1 | 0.002 | 1 | 0 | 0.428 |
| Pneumothorax | 1 | 0 | 0.366 | 8 | 4 | 0.002 | 2 | 2 | 0.636 |
| Severe ivH* | 0 | 1 | 0.32 | 8 | 6 | 0.772 | 0 | 0 | - |
| Long term complications | |||||||||
| nec | 1 | 0 | 0.28 | 4 | 0 | 0.049 | 0 | 0 | 0.428 |
| rop | 2 | 0 | <0.001 | 24 | 4 | 0.006 | 4 | 0 | 0.112 |
| BPD | 0 | 1 | 0.329 | 6 | 4 | 0.954 | 4 | 0 | 0.428 |
| Antibiotherapy | 9.2 | 10.7 | 0.801 | 4.6 | 8 | 0.501 | 8 | 5.8 | 0.562 |
| Duration of stay mean ± SD | 52.10 ± 40.5 | 22.73 ± 12.1 | <0.005 | 18.80 ± 24.6 | 9.75 ± 17.1 | <0.001 | 10.92 ± 15.1 | 4.81 ± 3.8 | <0.001 |
| Mortality | 1 | 0 | 0.28 | 8 | 7 | 0.54 | 7 | 0 | 0.428 |
| Microorganism | PROM ≥18 hours % | PROM <18 HOURS % | Total (%) |
|---|---|---|---|
| Staphylococcus spp. | 3 (30) | 3 (27.3) | 6 (28.5) |
| Klebsiella pneumoniae | 1 (10) | 4 (36.4) | 5 (23.8) |
| Escherichia coli | 5 (50) | 0 | 5 (23.8) |
| Streptococcus spp. | 1 (10) | 3 (27.3) | 4 (19.2) |
| Listeria monocytogenes | 0 | 1 (9) | 1 (4.7) |
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Lawama M, AlZaatreh A, Elrajabi R, Abdelhamid S, Badran E. Prolonged Rupture of Membranes, Neonatal Outcomes and Management Guidelines. J Clin Med Res. 2019; 11: 360-366. [CrossRef]
- Musilova I, Bestvina T, Hudeckova M, Michalec I, Cobo T, Jacobsson B, Kacerovsky M. Vaginal fluid interleukin-6 concentrations as a point-of-care test is of value in women with preterm prelabor rupture of membranes. American Journal of Obstetrics and Gynecology. 2016; 215: 619. [CrossRef]
- Toprak E, Bozkurt M, Dinçgez Çakmak B, Özçimen EE, Silahlı M, Ender Yumru A, Çalışkan E. Platelet-to-lymphocyte ratio: A new inflammatory marker for the diagnosis of preterm premature rupture of membranes. J Turk Ger Gynecol Assoc. 2017; 18: 122-6. [CrossRef]
- Caloone J, Rabilloud M, Boutitie F, Traverse-Glehen A, Allias-Montmayeur F, Denis L, Boisson-Gaudin C, Hot IJ, Guerre P, Cortet M, Huissoud C; ICAMs Study Group. Accuracy of several maternal seric markers for predicting histological chorioamnionitis after preterm premature rupture of membranes: a prospective and multicentric study. Eur J Obstet Gynecol Reprod Biol. 2016; 205:133-140. [CrossRef]
- Văduva CC, Constantinescu C, Radu MM, Văduva AR, Pănuş A, Ţenovici M, DiŢescu D, Albu DF. Pregnancy resulting from IMSI after testicular biopsy in a patient with obstructive azoospermia. Rom J Morphol Embryol. 2016; 57: 879-883.
- Albu DF, Albu CC, Văduva C-C, Niculescu M, Edu A. Diagnosis problems in a case of ovarian tumor-case presentation. Romanian Journal of Morphology and Embryology= Revue Roumaine de Morphologie et Embryologie. 2016; 57: 1437-1442.
- Enătescu I, Craina M, Gluhovschi A, Giurgi-Oncu C, Hogea L, Nussbaum LA, Bernad E, Simu M, Cosman D, Iacob D, Marinescu I, Enătescu VR. The role of personality dimensions and trait anxiety in increasing the likelihood of suicide ideation in women during the perinatal period. J Psychosom Obstet Gynaecol. 2021; 42: 242-252. [CrossRef]
- Enatescu VR, Bernad E, Gluhovschi A, Papava I, Romosan R, Palicsak A, Munteanu R, Craina M, Enatescu I. Perinatal characteristics and mother's personality profile associated with increased likelihood of postpartum depression occurrence in a Romanian outpatient sample. J Ment Health. 2017; 26: 212-219. [CrossRef]
- Covali R, Socolov D, Socolov R. Coagulation tests and blood glucose before vaginal delivery in healthy teenage pregnant women compared with healthy adult pregnant women. Medicine (Baltimore). 2019; 98: e14360. [CrossRef]
- Covali R, Socolov D, Socolov R, Pavaleanu I, Carauleanu A, Akad M, Boiculese VL, Adam AM. Complete Blood Count Peculiarities in Pregnant SARS-CoV-2-Infected Patients at Term: A Cohort Study. Diagnostics (Basel). 2021; 12. [CrossRef]
- Vicoveanu P, Vasilache IA, Nemescu D, Carauleanu A, Scripcariu IS, Rudisteanu D, Burlui A, Rezus E, Socolov D. Predictors Associated with Adverse Pregnancy Outcomes in a Cohort of Women with Systematic Lupus Erythematosus from Romania-An Observational Study (Stage 2). J Clin Med. 2022; 11. [CrossRef]
- Nemescu D, Constantinescu D, Gorduza V, Carauleanu A, Caba L, Navolan DB. Comparison between paramagnetic and CD71 magnetic activated cell sorting of fetal nucleated red blood cells from the maternal blood. J Clin Lab Anal. 2020; 34: e23420. [CrossRef]
- Iliescu M, Cărăuleanu A. The Portrait of a Good Doctor: Conclusions from a Patients and Medical Students Survey. Revista de Cercetare si Interventie Sociala. 2014; 47: 261-271.
- Cucu A, Costea C, Cărăuleanu A, Dumitrescu G, Sava, A, Scripcariu I, Costan, V-V, Turliuc, S, Poeata, I, Turliuc, D. Meningiomas Related to the Chernobyl Irradiation Disaster in North-Eastern Romania Between 1990 and 2015. Revista de Chimie -Bucharest- Original Edition. 2018; 69. [CrossRef]
- Turliuc, D, Turliuc, S, Cucu, S, Dumitrescu G, Cărăuleanu, A, Buzdugă, C, Camelia, Tamas, Sava, A, Costea, C. A review of analogies between some neuroanatomical terms and roman household objects. Annals of anatomy = Anatomischer Anzeiger: official organ of the Anatomische Gesellschaft. 10.1016/j.aanat.2015.07.001. 2015. [CrossRef]
- Dorfeuille N, Morin V, Tétu A, Demers S, Laforest G, Gouin K, Piedboeuf B, Bujold E. Vaginal Fluid Inflammatory Biomarkers and the Risk of Adverse Neonatal Outcomes in Women with PPROM. Am J Perinatol. 2016; 33: 1003-7. [CrossRef]
- Zhuang L, Li ZK, Zhu YF, Ju R, Hua SD, Yu CZ, Li X, Zhang YP, Li L, Yu Y, Zeng W, Cui J, Chen XY, Peng JY, Li T, Feng ZC. The correlation between prelabour rupture of the membranes and neonatal infectious diseases, and the evaluation of guideline implementation in China: a multi-centre prospective cohort study. Lancet Reg Health West Pac. 2020; 3: 100029. [CrossRef]
- Mukhopadhyay S, Puopolo KM, editors. Risk assessment in neonatal early onset sepsis. Seminars in perinatology; 2012: Elsevier. [CrossRef]
- Sgro M, Yudin MH, Lee S, Sankaran K, Tran D, Campbell D. Early-onset neonatal sepsis: It is not only group B streptococcus. Paediatr Child Health. 2011; 16: 269. [CrossRef]
- Shim GH, Kim SD, Kim HS, Kim ES, Lee HJ, Lee JA, et al. Trends in epidemiology of neonatal sepsis in a tertiary center in Korea: a 26-year longitudinal analysis, 1980-2005. J Korean Med Sci. 2011; 26: 284-289. [CrossRef]
- Shah BA, Padbury JF. Neonatal sepsis: an old problem with new insights. Virulence. 2014; 5: 170-178. [CrossRef]
- Ganesan P, Shanmugam P, Sattar SB, Shankar SL. Evaluation of IL-6, CRP and hs-CRP as Early Markers of Neonatal Sepsis. J Clin Diagn Res. 2016; 10: Dc13-17. [CrossRef]
- Ovayolu A, Ovayolu G, Karaman E, Yuce T, Turgut A, Bostancıeri N. Maternal serum endocan concentrations are elevated in patients with preterm premature rupture of membranes. J Perinat Med. 2019; 47: 510-515. [CrossRef]
- Benitz WE. Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol. 2010; 37: 421-438. [CrossRef]
- Helmbrecht AR, Marfurt S, Chaaban H. Systematic Review of the Effectiveness of the Neonatal Early-Onset Sepsis Calculator. J Perinat Neonatal Nurs. 2019; 33: 82-88. [CrossRef]
- Hornik CP, Benjamin DK, Becker KC, Benjamin DK Jr, Li J, Clark RH, Cohen-Wolkowiez M, Smith PB. Use of the complete blood cell count in early-onset neonatal sepsis. Pediatr Infect Dis J. 2012; 31: 799-802. [CrossRef]
- Sharma D, Farahbakhsh N, Shastri S, Sharma P. Biomarkers for diagnosis of neonatal sepsis: a literature review. J Matern Fetal Neonatal Med. 2018; 31: 1646-1659. [CrossRef]
- Gandhi P, Kondekar S. A Review of the Different Haematological Parameters and Biomarkers Used for Diagnosis of Neonatal Sepsis. EMJ Hematology. 2019: 85-92. [CrossRef]
- Hedegaard SS, Wisborg K, Hvas AM. Diagnostic utility of biomarkers for neonatal sepsis--a systematic review. Infect Dis (Lond). 2015; 47: 117-124. [CrossRef]
- Vouloumanou EK, Plessa E, Karageorgopoulos DE, Mantadakis E, Falagas ME. Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta-analysis. Intensive Care Med. 2011; 37: 747-762. [CrossRef]
- Hincu MA, Zonda GI, Stanciu GD, Nemescu D, Paduraru L. Relevance of Biomarkers Currently in Use or Research for Practical Diagnosis Approach of Neonatal Early-Onset Sepsis. Children (Basel). 2020; 7. [CrossRef]
- Odabasi IO, Bulbul A. Neonatal Sepsis. Sisli Etfal Hastan Tip Bul. 2020; 54: 142-158. [CrossRef]
- Tuzun F, Ozkan H, Cetinkaya M, Yucesoy E, Kurum O, Cebeci B, Cakmak E, Ozkutuk A, Keskinoglu P, Baysal B, Kumral A, Duman N. Is European Medicines Agency (EMA) sepsis criteria accurate for neonatal sepsis diagnosis or do we need new criteria? Plos one. 2019; 14: e0218002. [CrossRef]
- Gibbs RS, Blanco JE, St. Clair PJ, Castaneda YS. Quantitative bacteriology of amniotic fluid from women with clinical intraamniotic infection at term. Journal of Infectious Diseases. 1982; 145: 1-8. [CrossRef]
- Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014; 27: 21-47. [CrossRef]
- Achten NB, Dorigo-Zetsma JW, van Rossum AMC, Oostenbrink R, Plötz FB. Risk-based maternal group B Streptococcus screening strategy is compatible with the implementation of neonatal early-onset sepsis calculator. Clin Exp Pediatr. 2020; 63: 406-410. [CrossRef]
- Polcwiartek LB, Smith PB, Benjamin DK, Zimmerman K, Love A, Tiu L, Murray S, Kang P, Ebbesen F, Hagstrøm S, Clark RH, Greenberg RG. Early-onset sepsis in term infants admitted to neonatal intensive care units (2011-2016). J Perinatol. 2021; 41: 157-163. [CrossRef]
- Karabulut B, Alatas SO. Diagnostic Value of Neutrophil to Lymphocyte Ratio and Mean Platelet Volume on Early Onset Neonatal Sepsis on Term Neonate. J Pediatr Intensive Care. 2021; 10: 143-147. [CrossRef]
- Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB, Kipnis P, Escobar GJ. A Quantitative, Risk-Based Approach to the Management of Neonatal Early-Onset Sepsis. JAMA Pediatr. 2017; 171: 365-371. [CrossRef]
- Ko MH, Chang HY, Li ST, Jim WT, Chi H, Hsu CH, Peng CC, Lin CY, Chen CH, Chang JH. An 18-year retrospective study on the epidemiology of early-onset neonatal sepsis - emergence of uncommon pathogens. Pediatr Neonatol. 2021; 62: 491-498. [CrossRef]
- Shaaban HA, Safwat N. Mean platelet volume in preterm: a predictor of early onset neonatal sepsis. J Matern Fetal Neonatal Med. 2020; 33: 206-211. [CrossRef]
- Arcagok BC, Karabulut B. Platelet to Lymphocyte Ratio in Neonates: A Predictor of Early onset Neonatal Sepsis. Mediterr J Hematol Infect Dis. 2019; 11: e2019055. [CrossRef]
- Stocker M, van Herk W, El Helou S, Dutta S, Schuerman FABA, van den Tooren-de Groot RK, Wieringa JW, Janota J, van der Meer-Kappelle LH, Moonen R, Sie SD, de Vries E, Donker AE, Zimmerman U, Schlapbach LJ, de Mol AC, Hoffman-Haringsma A, Roy M, Tomaske M, F Kornelisse R, van Gijsel J, Visser EG, Plötz FB, Heath P, Achten NB, Lehnick D, van Rossum AMC. C-Reactive Protein, Procalcitonin, and White Blood Count to Rule Out Neonatal Early-onset Sepsis Within 36 Hours: A Secondary Analysis of the Neonatal Procalcitonin Intervention Study. Clin Infect Dis. 2021; 73: 383-390. [CrossRef]
- Marks L, de Waal K, Ferguson JK. Time to positive blood culture in early onset neonatal sepsis: A retrospective clinical study and review of the literature. J Paediatr Child Health. 2020; 56: 1371-1375. [CrossRef]
- Koenig JM, Keenan WJ. Group B streptococcus and early-onset sepsis in the era of maternal prophylaxis. Pediatr Clin North Am. 2009; 56: 689-708. [CrossRef]
- Stoll BJ, Hansen NI, Sánchez PJ, Faix RG, Poindexter BB, Van Meurs KP, Bizzarro MJ, Goldberg RN, Frantz ID 3rd, Hale EC, Shankaran S, Kennedy K, Carlo WA, Watterberg KL, Bell EF, Walsh MC, Schibler K, Laptook AR, Shane AL, Schrag SJ, Das A, Higgins RD; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011; 127: 817-826. [CrossRef]
- Sabry N, Abdelhakeem M, Mohamed H, Baheeg G. Validity of Platelet to Lymphocyte Ratio and Neutrophil to Lymphocyte Ratio in Diagnosing Early-onset Neonatal Sepsis in Full-term Newborns. Journal of Comprehensive Pediatrics. 2022. [CrossRef]
- Al-Matary A, Heena H, AlSarheed AS, Ouda W, AlShahrani DA, Wani TA, Qaraqei M, Abu-Shaheen A. Characteristics of neonatal Sepsis at a tertiary care hospital in Saudi Arabia. J Infect Public Health. 2019; 12: 666-672. [CrossRef]
- Kim SJ, Kim GE, Park JH, Lee SL, Kim CS. Clinical features and prognostic factors of early-onset sepsis: a 7.5-year experience in one neonatal intensive care unit. Korean J Pediatr. 2019; 62: 36-41. [CrossRef]
- Dong Y, Basmaci R, Titomanlio L, Sun B, Mercier JC. Neonatal sepsis: within and beyond China. Chin Med J (Engl). 2020; 133: 2219-2228. [CrossRef]
- Gkentzi D, Kortsalioudaki C, Cailes BC, Zaoutis T, Kopsidas J, Tsolia M, Spyridis N, Siahanidou S, Sarafidis K, Heath PT, Dimitriou G. Epidemiology of infections and antimicrobial use in Greek Neonatal Units. Arch Dis Child Fetal Neonatal Ed. 2019; 104: 293-297. [CrossRef]
- Barcaite E, Bartusevicius A, Tameliene R, Kliucinskas M, Maleckiene L, Nadisauskiene R. Prevalence of maternal group B streptococcal colonisation in European countries. Acta Obstet Gynecol Scand. 2008; 87: 260-271. [CrossRef]
- Wirth T, Bergot M, Rasigade JP, Pichon B, Barbier M, Martins-Simoes P, Jacob L, Pike R, Tissieres P, Picaud JC, Kearns A, Supply P, Butin M, Laurent F. Niche specialization and spread of Staphylococcus capitis involved in neonatal sepsis. Nat Microbiol. 2020; 5: 735-745. [CrossRef]
- Chiesa C, Natale F, Pascone R, Osborn JF, Pacifico L, Bonci E, De Curtis M. C reactive protein and procalcitonin: reference intervals for preterm and term newborns during the early neonatal period. Clin Chim Acta. 2011; 412: 1053-1059. [CrossRef]
- Eichberger J, Resch E, Resch B. Diagnosis of Neonatal Sepsis: The Role of Inflammatory Markers. Front Pediatr. 2022; 10: 840288. [CrossRef]
- Eschborn S, Weitkamp JH. Procalcitonin versus C-reactive protein: review of kinetics and performance for diagnosis of neonatal sepsis. J Perinatol. 2019; 39: 893-903. [CrossRef]
- Mjelle AB, Guthe HJT, Reigstad H, Bjørke-Monsen AL, Markestad T. Serum concentrations of C-reactive protein in healthy term-born Norwegian infants 48-72 hours after birth. Acta Paediatr. 2019; 108: 849-854. [CrossRef]
- Saldir M, Tunc T, Cekmez F, Cetinkaya M, Kalayci T, Fidanci K, Babacan O, Erdem G, Kocak N, Sari E, Akgul EO, Kul M. Endocan and Soluble Triggering Receptor Expressed on Myeloid Cells-1 as Novel Markers for Neonatal Sepsis. Pediatr Neonatol. 2015; 56: 415-421. [CrossRef]
- Zonda GI, Zonda R, Cernomaz AT, Paduraru L, Grigoriu BD. Endocan serum concentration in uninfected newborn infants. J Infect Dev Ctries. 2019; 13: 817-822. [CrossRef]
- Zonda GI, Zonda R, Cernomaz AT, Paduraru L, Avasiloaiei AL, Grigoriu BD. Endocan - a potential diagnostic marker for early onset sepsis in neonates. J Infect Dev Ctries. 2019; 13: 311-317. [CrossRef]
- Seliem W, Sultan AM. Presepsin as a predictor of early onset neonatal sepsis in the umbilical cord blood of premature infants with premature rupture of membranes. Pediatr Int. 2018; 60: 428-432. [CrossRef]
- Ruan L, Chen GY, Liu Z, Zhao Y, Xu GY, Li SF, Li CN, Chen LS, Tao Z. The combination of procalcitonin and C-reactive protein or presepsin alone improves the accuracy of diagnosis of neonatal sepsis: a meta-analysis and systematic review. Crit Care. 2018; 22: 316. [CrossRef]
- Liu C, Fang C, Xie L. Diagnostic utility of procalcitonin as a biomarker for late-onset neonatal sepsis. Transl Pediatr. 2020; 9: 237-242. [CrossRef]
| Parameters | PROM >18 hours GROUP A |
PROM <18 hours GROUP B |
Independent t-Test | |||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | T | P value | |||||
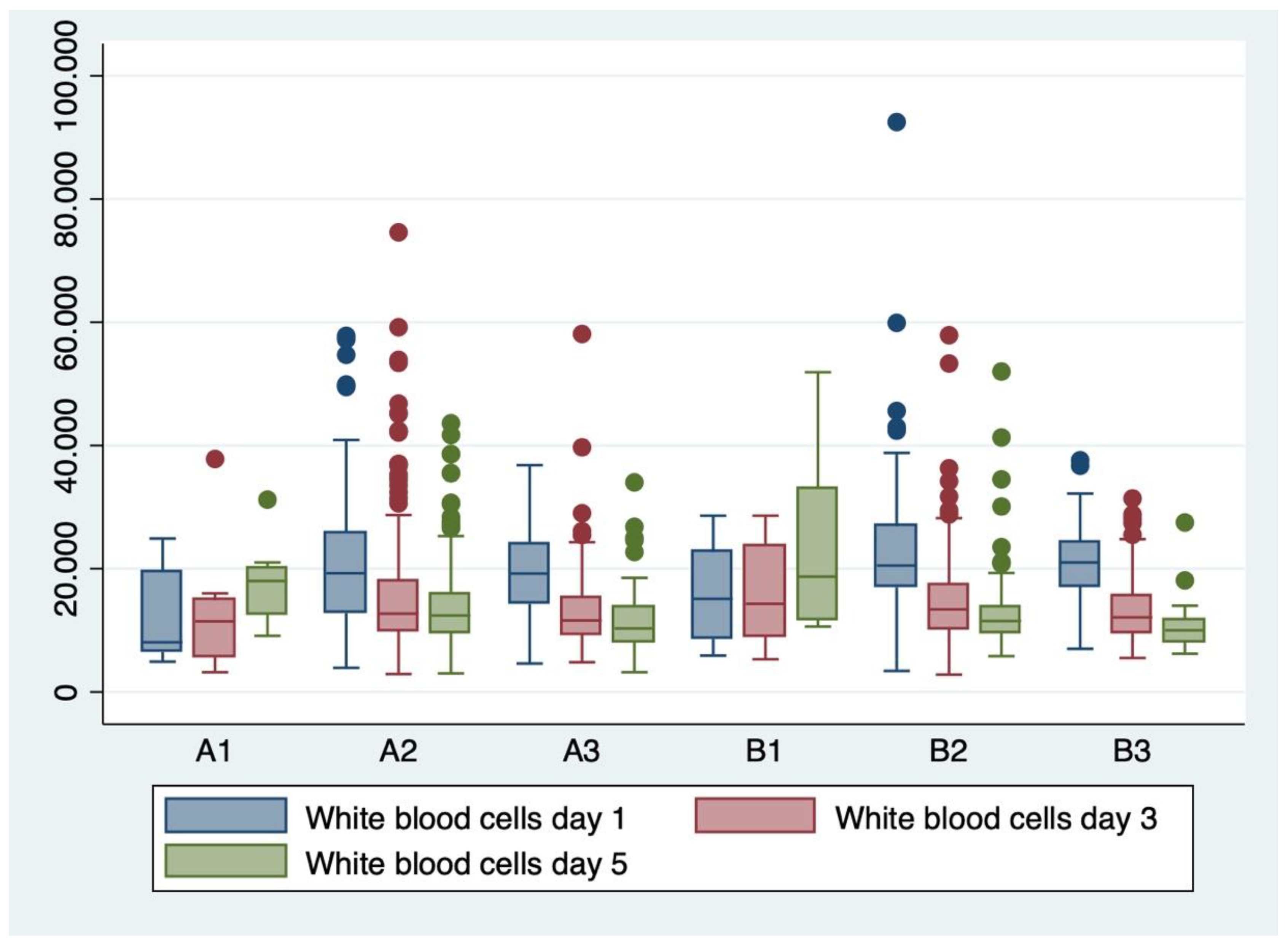
|
WBC x 103 /mm3 D1/D3/D5 |
19.54 ± 8.02 |
14.45 ± 8.21 |
13.1 ± 6.34 |
21.2 ± 7.87 |
14.34 ± 6.54 |
13.19 ± 7.61 |
-3.7 0.2 0.0 |
<0.001 >0.05 >0.05 |
| I/T ratio | 0.14 ± 0.11 |
0.15 ± 0.08 |
-0.53 | >0.05 | ||||
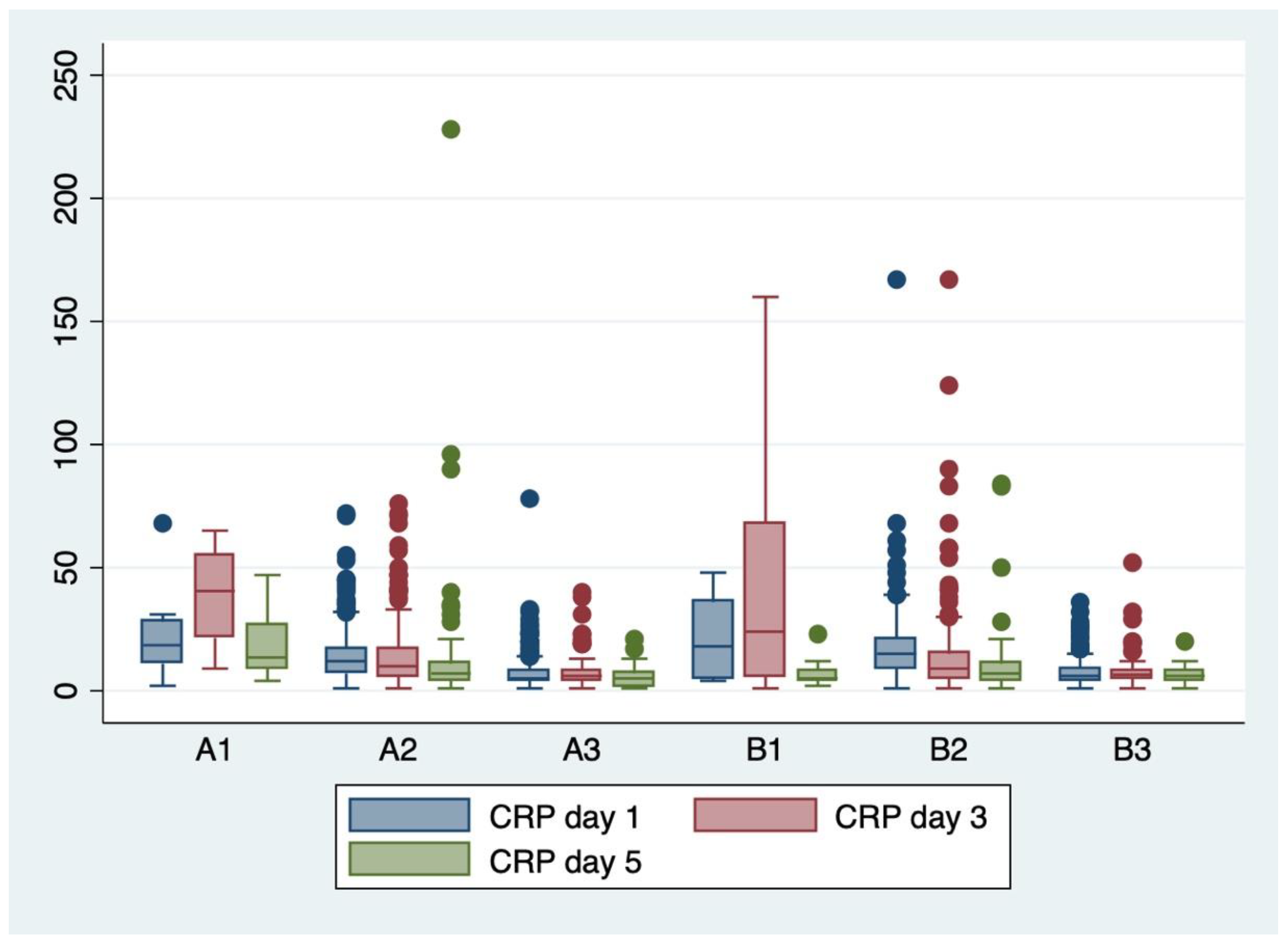
|
CRP mg/L D1/D3/D5 |
10.83 ± 9.56 |
11.86 ± 11.26 |
8.58 ± 15.06 |
13.02 ± 12.4 |
12.97 ± 18.35 |
8.51 ± 9.40 |
-3.3 -1.0 0.0 |
<0.001 >0.05 >0.05 |
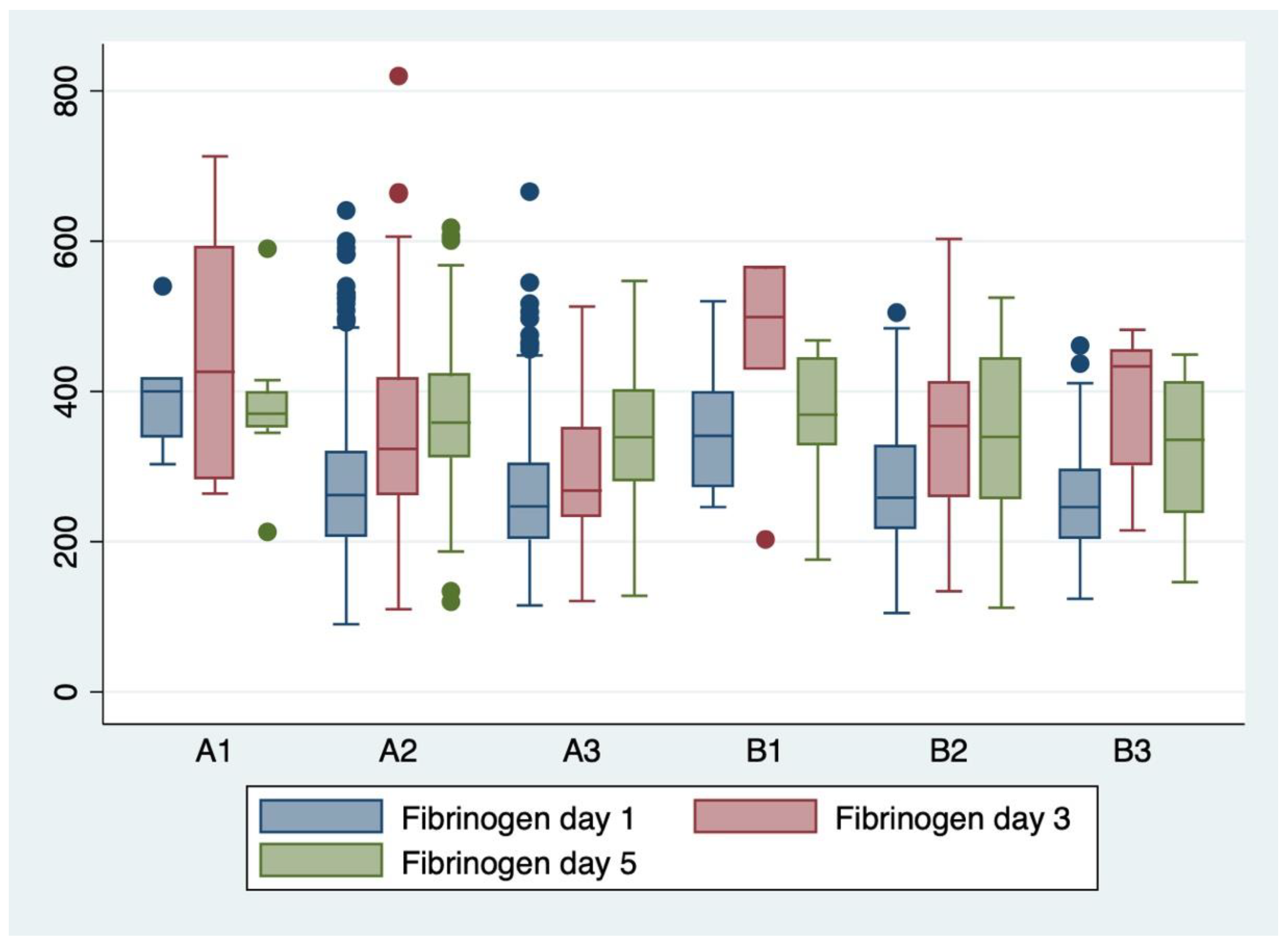
|
Fibrinogen D1/D3/D5 |
270 ± 98.3 |
332 ± 118.6 |
362 ± 88.3 |
268 ± 79.8 |
362± 114.2 |
340 ± 108.9 |
0.16 -1.7 1.4 |
>0.05 >0.05 >0.05 |
|
PROVEN SEPSIS Subgroup A1 Subgroup B1 |
Day 1 | Day 3 | Day 5 | Independent t-test |
|
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | t | P value | |
| WBC x 103 /mm3 | 12.05 ± 7.74 | 13.15 ± 10.89 | 17.71 ± 6.98 | -0.8 -0.5 -1.0 |
>0.05 >0.05 >0.05 |
| 15.1 ± 8.03 | 15.49 ± 8.13 | 23.67 ± 15 | |||
| I/T ratio | 0.20 ± 0.08 | 2.0 | >0.05 | ||
| 0.12 ± 0.04 | |||||
| CRP mg/L | 21.5 ± 19.10 | 38.5 ± 18.75 | 20.64 ± 14.25 | 0.4 0.0 2.1 |
>0.05 >0.05 >0.05 |
| 19.57 ± 16.93 | 38.36 ± 7.56 | 47.88 ± 6.48 | |||
| Fibrinogen | 399 ± 81.4 | 450 ± 191 | 380 ± 103 | 0.7 -0.0 0.3 |
>0.05 >0.05 >0.05 |
| 355 ± 109.4 | 457 ± 125 | 358 ± 104 | |||
|
Suspected EOS Subgroup A2 Subgroup B2 |
Day 1 | Day 3 | Day 5 | Independent t-test |
|
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | t | P value | |
| WBC x 103 /mm3 | 20.13 ± 9.15 | 13.92 ± 9.15 | 15.31 ± 9.05 | -2.4 0.6 0.7 |
<0.05 >0.05 >0.05 |
| 21.9 ± 9.18 | 13.23 ± 6.9 | 14.83 ± 7.09 | |||
| I/T ratio | 0.14 ± 0.12 | -0.4 | >0.05 | ||
| 0.15 ± 0.09 | |||||
| CRP mg/L | 13.96 ± 10.17 | 13.4 ± 6.7 | 17.6 ± 9.78 | -3.0 -0.3 0.2 |
<0.05 >0.05 >0.05 |
| 17 ± 4.37 | 13.8 ± 9.32 | 18 ± 10.7 | |||
| Fibrinogen | 277 ± 104 | 343 ± 120 | 364 ± 87.6 | 0.1 -0.0 1.3 |
>0.05 >0.05 >0.05 |
| 275 ± 84.7 | 344 ± 109 | 342 ± 110 | |||
|
No sepsis Subgroup A3 Subgroup B3 |
Day 1 Mean ± SD |
Day 3 Mean ± SD |
Day 5 Mean ± SD |
t | P value |
| WBC x 103 /mm3 | 19.09 ± 6.44 | 13.02 ± 6.13 | 11.42 ± 4.80 | -3.0 -0.5 0.9 |
<0.05 >0.05 >0.05 |
| 20.76 ± 5.57 | 13.39 ± 5.19 | 10.55 ± 3.99 | |||
| I/T ratio | 0.104 ± 0.09 | -3.5 | >0.05 | ||
| 0.14 | |||||
| CRP mg/L | 7.03 ± 6.5 | 7.18 ± 5.77 | 4.99 ± 3.38 | -0.9 -0.7 -2.0 |
>0.05 >0.05 <0.05 |
| 7.57 ± 5.6 | 7.80 ± 6.93 | 6.22 ± 3.42 | |||
| Fibrinogen | 257 ± 86 | 293 ± 92.67 | 350 ± 88 | 0.1 -2.5 0.8 |
>0.05 <0.05 >0.05 |
| 255 ± 68.11 | 383 ± 99.59 | 320 ± 115 | |||
| Serum biomarkers | Groups | ANOVA results | Bonferroni test | |||||
|---|---|---|---|---|---|---|---|---|
| F score | P value | Mean difference | Standard error | P value | 95% confidence interval lower limit | 95% confidence interval upper limit | ||
|
WBC day 1 |
A1-B1 | 7.13 | <0.001 | -3.05 | 3.45 | 1.000 | - 13.21 | 7.11 |
| A2-B2 | -8.71 | 2.56 | 0.010 | -16.24 | -1.17 | |||
| A3-B3 | -8.08 | 2.53 | 0.022 | -15.53 | -0.64 | |||
| WBC day 3 | A1-B1 | 2.79 | 0.016 | -2.34 | 3.59 | 1.000 | -12.92 | 8.24 |
| A2-B2 | 0.48 | 0.68 | 1.000 | -1.53 | 2.50 | |||
| A3-B3 | -0.037 | 0.90 | 1.000 | -3.03 | 2.28 | |||
| WBC day 5 | A1-B1 | 8.27 | <0.001 | -5.96 | 3.23 | 0.98 | -15.49 | 3.57 |
| A2-B2 | 0.68 | 0.82 | 1.000 | -1.73 | 3.10 | |||
| A3-B3 | 0.87 | 1.28 | 1.000 | -2.91 | 4.66 | |||
| CRP day 1 | A1-B1 | 41.43 | <0.001 | 1.92 | 4.92 | 1.000 | -12.55 | 16.40 |
| A2-B2 | -3.05 | 0.82 | 0.003 | -5.47 | -0.64 | |||
| A3-B3 | -0.54 | 0.91 | 1.000 | -3.22 | 2.13 | |||
| CRP day 3 | A1-B1 | 21.4 | <0.001 | 0.13 | 6.33 | 1.000 | -18.50 | 18.78 |
| A2-B2 | -0.39 | 1.16 | 1.000 | -3.84 | 3.05 | |||
| A3-B3 | -0.61 | 1.79 | 1.000 | -5.91 | 4.68 | |||
| CRP day 5 | A1-B1 | 3.2 | 0.007 | 11.19 | 6.37 | 1.000 | -7.59 | 29.98 |
| A2-B2 | 0.45 | 1.41 | 1.000 | -3.72 | 4.62 | |||
| A3-B3 | 24.70 | 4.90 | 0.04 | 10.27 | 39.14 | |||
| Fibrinogen day 1 | A1-B1 | 5.2 | <0.001 | 43.9 | 55.08 | 1.000 | -118.29 | 206.09 |
| A2-B2 | 1.41 | 9.02 | 1.000 | -25.16 | 27.98 | |||
| A3-B3 | 1.34 | 10.40 | 1.000 | -29.28 | 31.97 | |||
| Fibrinogen day 3 | A1-B1 | 4.96 | <0.001 | -7.19 | 63.63 | 1.000 | -195.52 | 181.14 |
| A2-B2 | 5.60 | 1.61 | 0.008 | 0.86 | 10.36 | |||
| A3-B3 | -90.39 | 42.92 | 0.541 | -217.45 | 36.65 | |||
| Fibrinogen day 5 | A1-B1 | 0.73 | 0.59 | 21.16 | 50.95 | 1.000 | -130.06 | 172.39 |
| A2-B2 | 22.34 | 16.88 | 1.000 | -27.75 | 72.44 | |||
| A3-B3 | -1.23 | 2.34 | 1.000 | -8.14 | 5.68 | |||
| Serum biomarkers | P value | 95% Confidence interval |
|---|---|---|
| WBC day 1 | 0.005 | 0.016- 0.09 |
| WBC day 3 | 0.028 | -0.08- -0.004 |
| WBC day 5 | 0.769 | -0.04- 0.03 |
| CRP day 1 | 0.004 | -0.01- 0.02 |
| CRP day 3 | 0.063 | -0.0008- 0.03 |
| CRP day 5 | 0.483 | -0.044- 0.021 |
| Fibrinogen day 1 | 0.642 | -0.002- 0.001 |
| Fibrinogen day 3 | 0.823 | -0.002- 0.002 |
| Fibrinogen day 5 | 0.117 | -0.004- 0.0004 |
| Biomarker | AUC value |
|---|---|
| WBC day 1 | 0.55 |
| WBC day 3 | 0.47 |
| WBC day 5 | 0.49 |
| CRP day 1 | 0.76 |
| CRP day 3 | 0.66 |
| CRP day 5 | 0.62 |
| Fibrinogen day 1 | 0.34 |
| Fibrinogen day 3 | 0.37 |
| Fibrinogen day 5 | 0.35 |
| I/T | 0.58 |
| PCT | 0.78 |
| WBC+ CRP+Fibrinogen (day 1) | 0.83 |
| WBC+ CRP+Fibrinogen (day 3) | 0.90 |
| WBC+ CRP+Fibrinogen (day 5) | 0.70 |
| I/T+ PCT | 0.76 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





