1. Introduction
Two-dimensional (2D) ultrasonography (US) has been widely used as a prenatal diagnostic tool for fetuses with suspected clubfoot. For decades, recent advances in fetal imaging have improved the accuracy of prenatal diagnosis of clubfoot, achieving a success rate of about 80%% [
1]. However, the false positive rate (FPR) still varies from 10% to 25% [
2,
3,
4,
5,
6]. One significant factor contributing to the inability to reduce the false positive rate is the resemblance in features between pathologic and benign feet observed during 2D US examinations. Classically, prenatal clubfoot is diagnosed based on the fact that the long bones of the tibia and fibula are characterized in the coronal plane as part of the lateral or plantar aspect of the foot, with the supinated and adducted positions.
Although the sonographic findings of pathologic clubfoot were similar to those of benign clubfoot, the treatment strategies and outcomes differed between the two groups. Pathological clubfoot is a subluxation of the talo-calcaneo-navicular joint with stiffness of the midtarsal and ankle joints, which causes underdevelopment of the calf and peroneal muscles and requires postnatal reductive treatment [
7]. Gold standard treatment of pathologic clubfoot is the conservative Ponseti method, including the reduction of deformity with weekly serial plaster casting and percutaneous Achilles tenotomy. Open surgery is the treatment of choice when conservative treatment is unsuccessful in the correction of the deformity [
8,
9]. In contrast, benign clubfoot can be easily corrected with gentle positioning without any postnatal treatment. Therefore, the two variants of the clubfoot spectrum need to be accurately differentiated during the prenatal period to allow appropriate counseling of parents and adequate planning of neonatal management.
After delivery, decisions related to the type of treatment depend on the Demiglio scoring system conducted by experienced orthopedic surgeons, which is a typical scoring method with high intra-and interobserver reliability [
10,
11,
12]. The four major components–equinus, varus, derotation of the calcaneal block, and forefoot adduction are assessed by manual examination and are used to evaluate reducibility. Postnatal evaluation of repositioning ability is based on physical examination. However, prenatal measurements using 2D US only evaluate the angle of the foot and ankle on one plane, limiting the ability to predict treatment outcomes. Previous studies focused only on evaluations in the coronal plane using 2D US and did not consider a multifaceted approach [
2,
5,
13,
14].
Recently, Marie et al. highlighted that the multiplane approach is important for differentiating between pathological and benign clubfoot to improve precise prenatal diagnosis [
15,
16]. As pathologic clubfoot involves complex subluxation, including equinus, varus, calcaneopedal block, and adduction of the forefoot, assessment from multiple planes using three-dimensional (3D) US has advantages over 2D US should be performed. In obstetrical ultrasound, the utilization of 3D US augments diagnostic capacities for congenital heart disease, musculoskeletal disease, and central nervous system disease, thus improving diagnostic accuracy. Images displayed using three simultaneous orthogonal planes and/or rendered images facilitate the assessment of structures from various angles, while also enabling the measurement of their volume [
17].
Based on this background, our study aimed to investigate the differential US parameters of pathological clubfoot in utero by utilizing 3D US.
2. Materials and Methods
2.1. Study population
Identified patients were those who were suspected of fetal clubfoot and received prenatal care at our institution (Chung-Ang University Hospital, Seoul, South Korea) and postnatal neonatal evaluation between January 1, 2018, and August 31, 2021. The inclusion criterion for this study was singleton pregnancy with prenatally suspected isolated clubfoot. Intrauterine death, neonatal death, neonate with complex malformations and multiple pregnancy were excluded. Finally, 31 of the 39 pregnancies were examined. Among the 8 cases that were excluded, 5 presented with multiple anomalies, 1 resulted in neonatal death, and 2 were twin pregnancies.
2.2. Demographic characteristics
The maternal and neonatal demographic data and medical history including maternal age, body mass index, preeclampsia, gestational diabetes, delivery mode, gestational age of delivery, preterm delivery, neonatal sex, birth weight and postnatal treatment were obtained from medical records conducted by healthcare providers. Postnatal treatment was classified into two types: Ponseti conservative treatment, which includes serial cast treatment and Achilles tendon percutaneous tenotomy, and open surgery, which involves posterior or posteromedial release. The observation period was defined as the second year of life, and pregnant women who gave birth in August 2023 were the last subjects.
2.3. Sonographic measurements
One skilled operator reviewed and assessed all the US recordings on the day of measurement. Following the as low as reasonably achievable principle, the recordings were recalled and measured after the US examination to reduce the time of exposure. For all US examinations, the 3D mode of Voluson™ E10 (© 2021 General Electric Company, New York, US) model was used.
In the coronal plane, where both the tibia and fibula are visible via 2D US, the cross section of a normal foot is not visible (
Figure 1. A). In cases where clubfoot is suspected, the lateral surface of the affected foot is observed simultaneously (
Figure 1.B). Following the saving of a 2D image indicating clubfoot, 3D ultrasound is employed to perform evaluations.
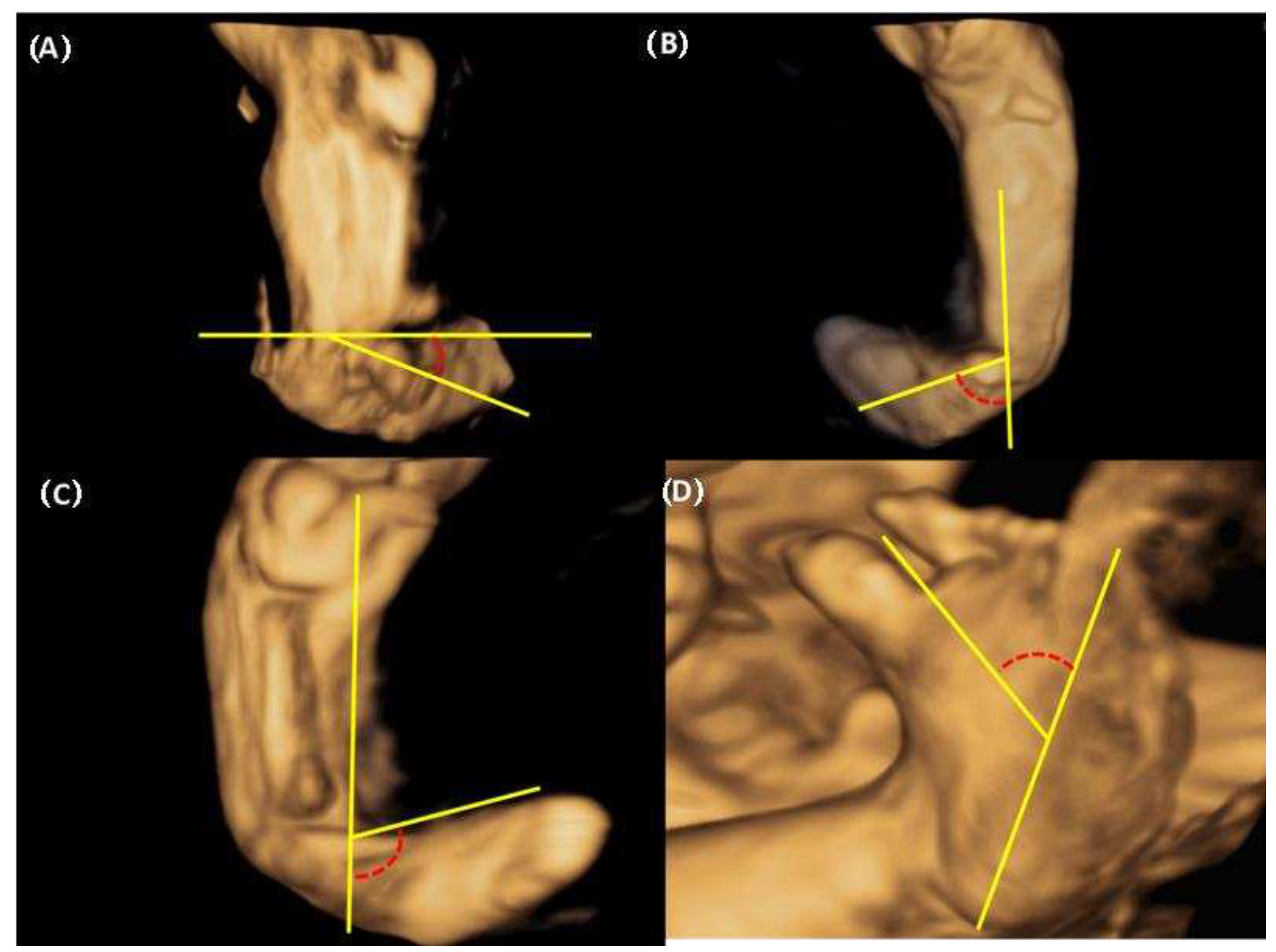
We were able to freely handle the 3D captured image at 360 degrees and reproduce the desired planes, reconstructed the sagittal, coronal (anterior and posterior), and horizontal planes. Below is an explanation of the deviation value measured at each plane (
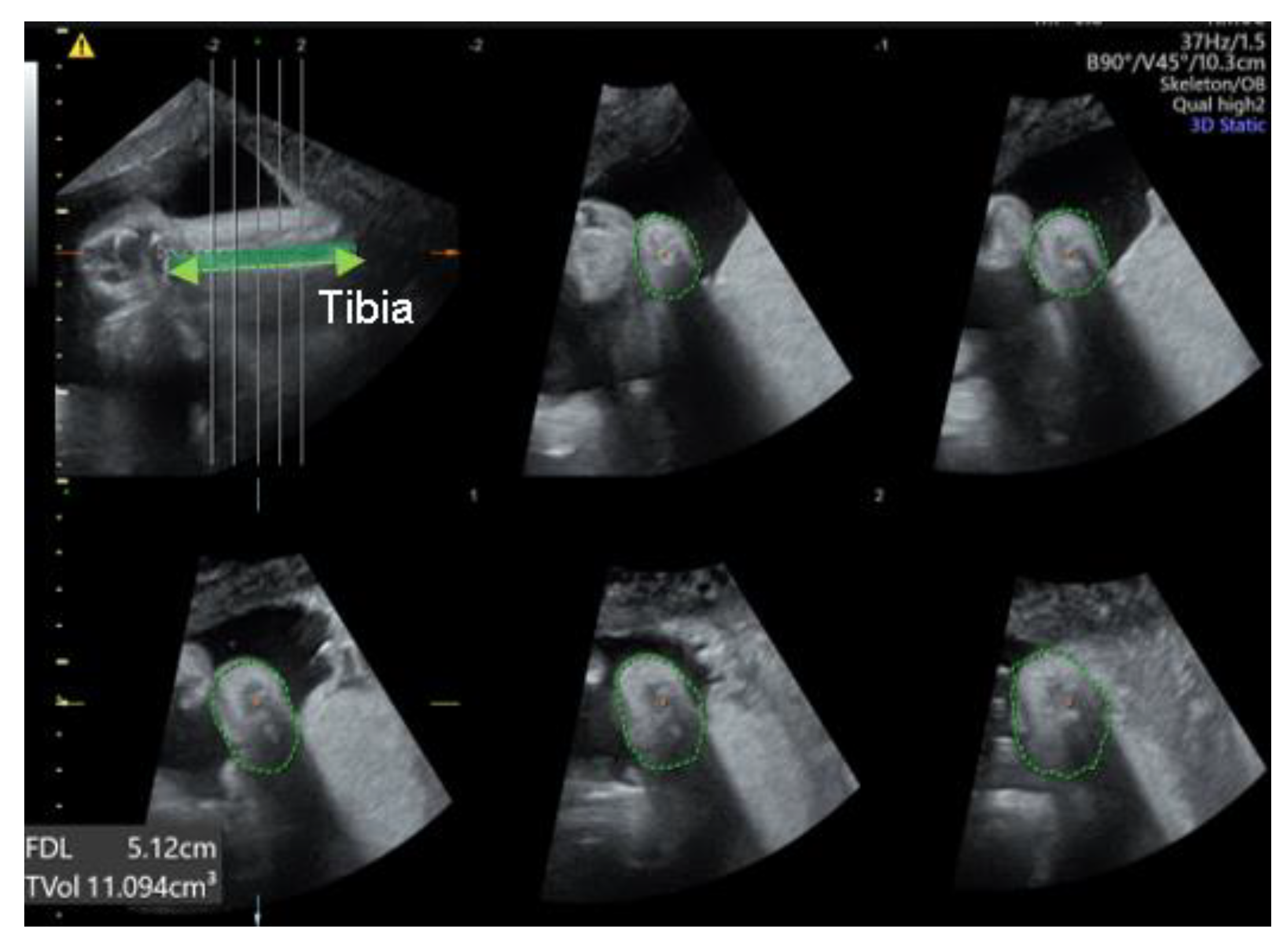
Figure 2). 1. Equinus deviation: the fixation of the foot in a plantar inward position in the sagittal plane. we measured the deviated angle between the line perpendicular to the tibia and the midline of the dorsum. 2. Varus deviation: the medial deviation of the foot in the posterior coronal plane. we measured the angle between the line parallel to the tibia and the midline of the calcaneus 3. Calcaneopedal block deviation: derotation of the calcaneal forefoot block in the frontal coronal plane. we measured the angle between the medial line of the calf and the inner line of the talus.4. Forefoot adduction in the horizontal plane. we measured the angle between the midline of the plantar and the inner line of the big toe. Calf volume and circumference were also measured because calf muscle dystrophy is a significant clinical feature of congenital clubfoot and is one of the scoring factors in the Demeglio method. First, we created a plane in which the tibia and fibula are observed. Second, designating the end of the ossified tibia bone, we divided it horizontally into five sections and measured the circumference using calipers on the skin surface. The largest calf circumference and automatic calculated calf volume were recorded (
Figure 3).
2.4. The postnatal assessment and treatment
After birth, an orthopedic surgeon assessed the clubfoot using the Dimeglio and Pirani scores and determined the therapeutic decision. The Ponseti method is a conventional treatment, which involves the placement of a series of five to seven casts over a few weeks or months. The first cast was placed on the foot within 48 hours of birth to improve treatment efficacy. When the patient required further correction of the feet, an Achilles tendon percutaneous tenotomy was performed.
2.5. Statistical analysis
The Mann Whitney U test was used to compare continuous variables, and chi-square or Fisher's exact test were used to compare categorical variables. The chi-squared test was used to estimate categorical parameters. The Spearman correlation coefficient was used to estimate the correlation between prenatal and postnatal parameters. ROC analysis was conducted to compare the performance of prediction models. The comparison was based on the AUC values of the models. The optimal cutoff values were determined as the point which maximizes the sum of the sensitivity and specificity. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also calculated to assess the diagnostic utility of each parameter in predicting the postnatal treatment of clubfoot. Statistical analyses were performed using R software (version 3.2.4; R Foundation for Statistical Computing, Vienna, Austria), and statistical significance was accepted where P values were <0.05.
3.Results
Of the 31 pregnancies 47 feet, 16 cases of bilateral clubfoot (32 feet), and 15 cases (15 feet) of unilateral clubfoot were suspected. The median gestational weeks when the ultrasound was performed was 26 weeks of gestations. The median age at delivery was 38+4 weeks. Of the 31 neonates, 17 (54.8%) were male and 14 (45.2%) were female. After delivery, 78.7 % (37/47) were treated and 21.2 % (10/47) were observed without treatment. Additional open surgery (posterior or posteromedial release) was not performed in all patients.
Table 1 presents the results of the comparison of baseline characteristics between the treated and non-treated groups, indicating that no statistically significant differences were observed.
3.1. The differences in deviated angle, calf volume and calf circumference between treated group and non-treated group.
Table 2 presents a comparison of deviated angles measured in the relative plane using 3D US between the two groups. The degree of hindfoot varus deviation was greater in the treated group than in the non-treated group (60.5° [50.6 - 71.4] vs. 46.6° [25.8 - 52.2], p=0.042). The deviation of calcaneopedal block in the treated showed a higher degree than the non-treated group (65.6° [58.2 – 88.2] vs 26.6° [23.0 – 32.8], p <0.05). No significant differences were identified in equinus and forefoot adduction. The volume and circumference of calf had no differences between two groups. When assessing clubfoot through the conventional 2D US measurement, no statistically significant variance in the angle between the lower leg and foot was observed (80° [66 -100] vs. 95° [61 – 103.8], p=0.794).
3.2. The ROC curve for prediction of postnatal treatment
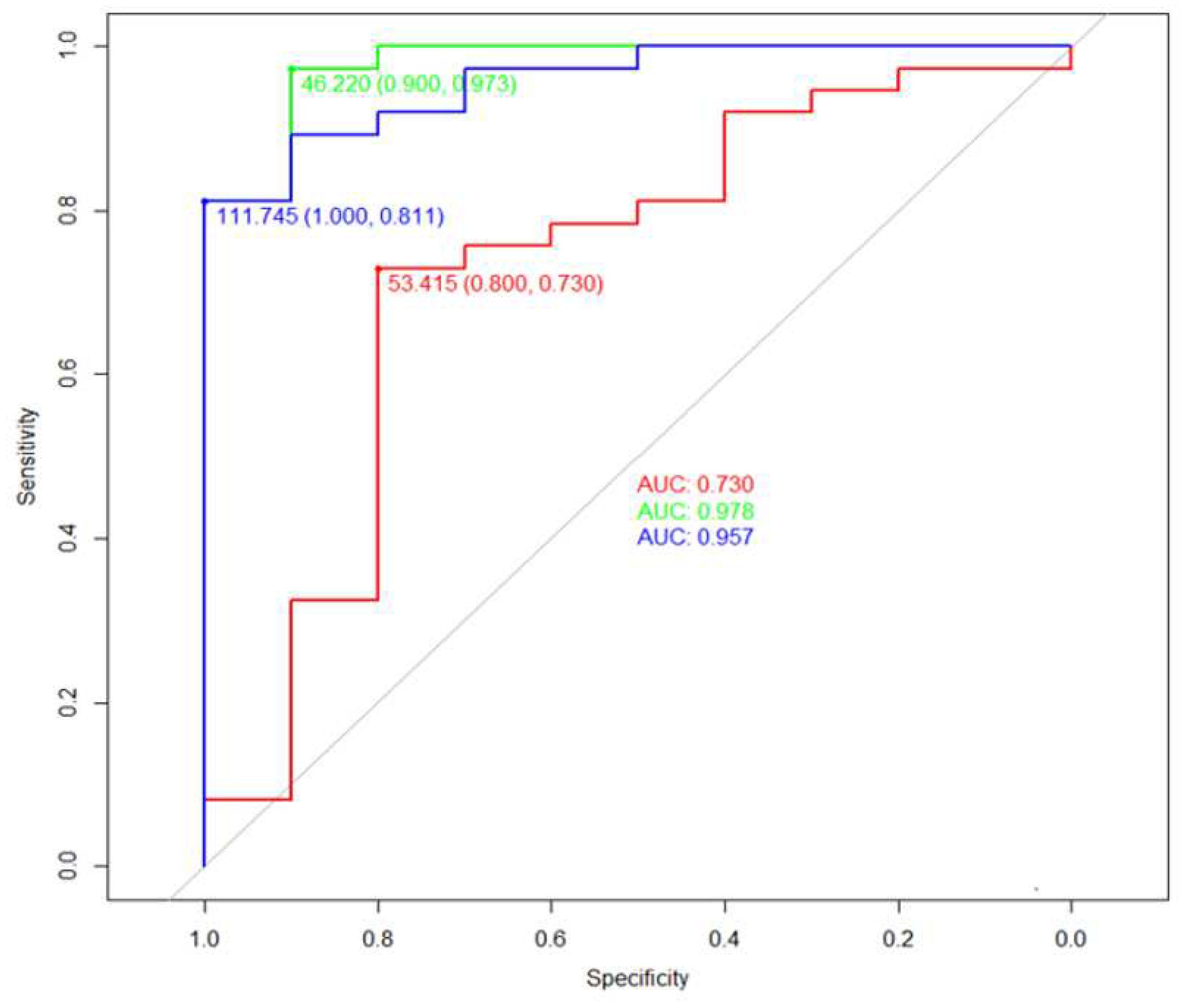
In the ROC curve analysis (
Figure 4) for the prediction of postnatal treatment, the varus angle demonstrated an area under the curve (AUC) of 0.73 and suggested a diagnostic performance with 73% sensitivity, 80% specificity, 93% PPV, and 44% NPV at a diagnostic threshold of 53.4 degrees. The AUC of calcaneopedal block deviation showed the higher predictable value with 0.98 including 97% sensitivity, 90% specificity, 90% PPV, and 97% NPV at a diagnostic threshold of 46.2 degrees than the AUC of varus deviation. To enhance the accuracy of the prediction, we conducted an ROC curve analysis by incorporating varus deviation and calcaneopedal block deviation values. An AUC of 0.96 represented with 81% sensitivity, 100% specificity, 100% PPV and 59% NPV at a threshold of 111.8 degrees.
3.3. Subgroup analysis
The correlation between the number of casts and the degree of deviation
We performed sub-analysis on the number of casting administered in the treated group and correlations with the level of deviation, calf volume, and calf circumference by Spearman correlation. No significant linear relationship was found between any variable and cast count (no figures are provided).
Differences in calf volume and calf circumference values between two calves with unilateral and bilateral clubfoot.
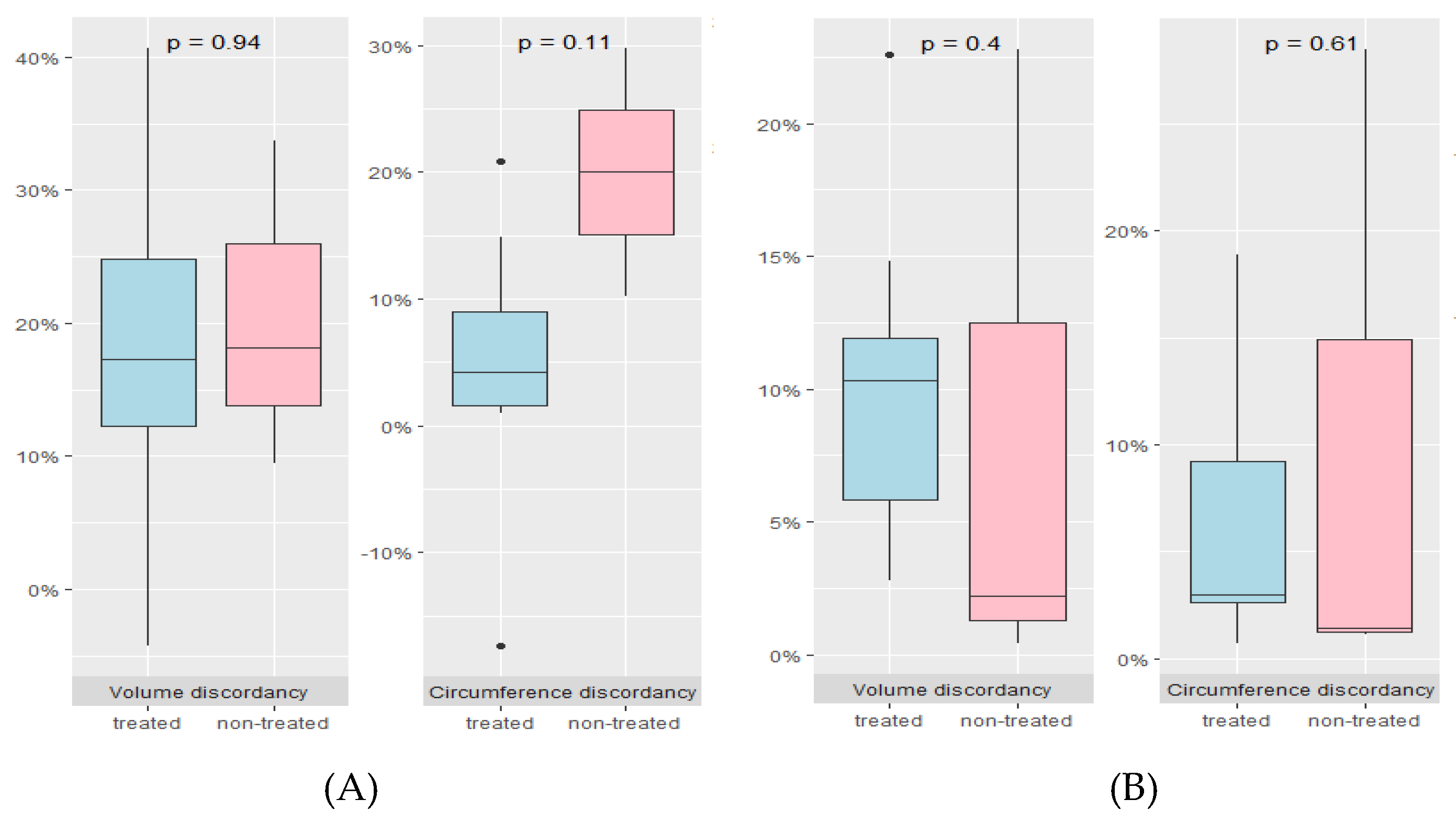
In cases of unilateral clubfoot (
Figure 5, A), as based on data obtained from 10 pregnancies (7 treated groups and 3 untreated groups), excluding 1 case with inadequate ultrasound data, no significant differences were observed with regards to calf volume (17.3 % [12.3 – 24.8] VS 18.2 % [ 13.8 – 25.9], p=0.938) and calf circumference (4.2% [1.5 – 8.9] VS 20.0 % [ 15.1 – 24.9], p=0.114) between treated and the non-treated groups. Of the 18 pregnancies who were suspected to have bilateral clubfoot, 5 patients (10 feet) were excluded due to insufficient ultrasound data. Thus, 13 patients (26 feet) were available to compare the discordance in the treated (10 patients) and untreated (3 patients) groups. (
Figure 5, B). There were no differences of calf volume discordancy (10.3% [5.8-11.9] VS 2.2% [1.3-12.5], p=0.398) and calf circumference discordancy (3.0% [2.6-9.2] VS 1.4% [1.2-14.9], p=0.612).
4. Discussion
Notably, our study is the first to evaluate the cases of clubfoot using prenatal 3D US. Our data suggested that the degree of varus deviation and calcaneopedal block was higher in the treated group than in the non-treated group. The cutoff value calcaneopedal block deviation indicated an AUC of 0.98 which is considered to be within an acceptable range and high accuracy with 96%. Prenatal diagnosis of suspected clubfoot was performed using 2D US, which is a typical method of observing the deviating angle between the calf and foot in the coronal plane. Although the postnatal Dimeglio scoring system includes four parameters (equinus deviation, varus deviation, derotation of the calcaneo-forefoot block, and forefoot adduction), and four gravity signs (plantar crease, medial crease, cavus retraction, and fibrous musculature), 2D US prenatal assessment has considered only one parameter and is insufficient for assessing the severity and postnatal outcomes of congenital foot conditions [
18]. Few previous studies have attempted to evaluate severity and predict postnatal outcomes using 2D US. Glotzbecker, M.P. et al. developed a sonographic scoring system that classifies the severity of clubfoot into three categories (mild, moderate, and severe) and demonstrated diagnosed severe cases based on the scoring system, leading to a decrease in the FPR (19%–7%) [
14,
19]. Following this result, a prospective study based on the aforementioned scoring system suggested that the accuracy of diagnosis in cases with severe, moderate, and mild scores was 94%, 70%, and 25%, respectively [
19]. However, this study did not provide a measurement tool for improving the diagnostic accuracy of mild clubfoot. Recently, Lanna et al. attempted to improve prenatal diagnosis using 2D US with a multiplanar view. The angle between the long axis of the foot and lower leg; foot width, and length, the width-to-length ratio of the foot; tibia length, and calf width ratio were examined to predict postnatal treatment. They suggested that the angle between the long axis of the foot showed the highest accuracy at a diagnostic threshold of 80 degrees (AUC 0.98, confidence interval 0.94–1.00) [
16]. We also recorded the angles using conventional 2D US to evaluate the diagnostic superiority of the angle using 3D US but did not obtain significant difference values between the treated and non-treated groups. This result is inconsistent with the study by Lanna et al, which found that the angle in the treatment group was higher than that in the non-treatment group in 2D US. Our hypothesis was that the treated group would exhibit a reduction in calf volume and circumference in utero due to calf muscle dystrophy [
20]. Calf volume and circumference exhibited no significant variance between the treated and untreated groups. The nomogram from previous research [
21] indicates that calf muscle size and diameter increase with each week of gestation. The different weeks of gestation at which ultrasound was performed for each subject in our study may have contributed to these results. We aimed to compare the calf development of our subjects with normal calf development based on gestational weeks, using the calf nomogram developed by R. Hershkovitz et al. However, the method for measuring calf development recommended in the previous nomogram was unsuitable, given that our study applied a different assessment method through the use of 3D US.
Additionally, we hypothesize that unilateral pathologic clubfoot results in decreased calf volume and circumference in the affected foot compared to the contralateral normal foot. In contrast, bilateral pathologic clubfoot does not show any differences in either factor. We performed a subgroup analysis to compare calf volume and circumference discordance between the treated and non-treated groups in unilateral clubfoot and bilateral clubfoot, respectively. In bilateral clubfoot, the volume and circumference of both calves did not differ between the treatment and non-treatment groups, but in unilateral clubfoot, there was also no difference between the treatment and non-treatment groups. This is inconsistent with our hypothesis. We consider that the number of subjects used in this analysis was small, 10 (unilateral clubfoot) and 13 (bilateral clubfoot), and therefore not statistically significant. To overcome this limitation, we are conducting a further study to establish nomogram for normal fetal calf volume and circumference using 3D US. The importance of calcaneopedal block derotation as a determinant of treatment outcomes in orthopedics is widely recognized [
22,
23]. Brazell et al. (2019) reported that correction of the equinus deformity should only be considered after reaching a calcaneopedal block derotation of at least 20-30 degrees [
22]. There are limitations in accessing 2D US for assessing calcaneopedal block derotation in utero. To assess calcaneopedal block derotation, measure the angle after creating a frontal plane with the fetus’ knee facing forward. In the 2D method, the angle is measured in a plane where both the tibia and fibula are visible, but this is not necessarily the exact coronal plane. We utilized 3D US to establish a precise coronal plane that can assess calcaneopedal block deviation and ultimately overcome clinical limitations. Our findings suggested that this parameter is the most accurate predictor in prenatal ultrasound.
Our study is limited by the small sample size and absence of verification of the intraobserver and interobserver reliability of our measurement method. Our first trial using a 3D US assessment tool for predicting postnatal clubfoot outcomes suggested that a multiplane approach could improve prenatal diagnostic accuracy. This improved assessment can provide accurate information and decrease the emotional burden of parental counseling. This study needs more prospective data including calf volume and circumference to evaluate muscular dystrophy.
5. Conclusions
Our study suggested a new measure of calcaneopedal block deviation by US assessment to replace the conventional 2D US evaluation method for prenatal clubfoot diagnosis. Calcaneopedal block deviation holds significant importance for postnatal clubfoot assessment, and our findings demonstrate that it can be a reliable indicator of clubfoot in the fetus prenatal 3D ultrasound assessment. Prenatal measurement of calcaneopedal block deviation could enhance the accuracy of diagnosing clubfoot during prenatal care, which was earlier assessed solely through 2D ultrasound. Furthermore, these findings underscore the necessity of implementing 3D ultrasound in the diagnosis of congenital musculoskeletal disorders, including clubfoot.
Author Contributions
Conceptualization, Yoo-min Kim, Gwang Jun Kim and In Ho Choi; formal analysis, Yejin Jo and Yoo-min Kim; writing—original draft preparation, Yoo-min Kim, Ji Su Seong, Ji Hoi Kim, Gina Nam and Na mi Lee; writing—review and editing, Gwang Jun Kim and In Ho Choi; visualization, Yejin Jo and Yoo-min Kim; supervision, Gwang Jun Kim and In Ho Choi; funding acquisition, Yoo-min Kim. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Chung-Ang University Research Scholarship Grant in 2021.
Institutional Review Board Statement
This retrospective study received approval from the Institutional Review Board at Chung-Ang University Hospital in accordance with the Declaration of Helsinki. (protocol code: 2306-019-19476, approval date: Aug 10th,2023).
Informed Consent Statement
Informed consent is not applicable. this is a retrospective study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We thank all sonographers and research nurses for their dedicated assistance with this trial, as follows: Jinyoung Kim (Chungang University Hospital) and Hye Sueng Hong (Chungang University Hospital).
Conflicts of Interest
No potential conflicts of interest were disclosed by the authors.
References
- Offerdal, K.; Jebens, N.; Blaas, H.G.; Eik-Nes, S.H. Prenatal ultrasound detection of talipes equinovarus in a non-selected population of 49 314 deliveries in Norway. Ultrasound Obstet Gynecol 2007, 30, 838–844. [Google Scholar] [CrossRef]
- Tillett, R.L.; Fisk, N.M.; Murphy, K.; Hunt, D.M. Clinical outcome of congenital talipes equinovarus diagnosed antenatally by ultrasound. J Bone Joint Surg Br 2000, 82, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Bar-On, E.; Mashiach, R.; Inbar, O.; Weigl, D.; Katz, K.; Meizner, I. Prenatal ultrasound diagnosis of club foot: outcome and recommendations for counselling and follow-up. J Bone Joint Surg Br 2005, 87, 990–993. [Google Scholar] [CrossRef] [PubMed]
- Shipp, T.D.; Benacerraf, B.R. The significance of prenatally identified isolated clubfoot: is amniocentesis indicated? Am J Obstet Gynecol 1998, 178, 600–602. [Google Scholar] [CrossRef] [PubMed]
- Keret, D.; Ezra, E.; Lokiec, F.; Hayek, S.; Segev, E.; Wientroub, S. Efficacy of prenatal ultrasonography in confirmed club foot. J Bone Joint Surg Br 2002, 84, 1015–1019. [Google Scholar] [CrossRef] [PubMed]
- Mammen, L.; Benson, C.B. Outcome of fetuses with clubfeet diagnosed by prenatal sonography. J Ultrasound Med 2004, 23, 497–500. [Google Scholar] [CrossRef]
- Bleck, E.E. Club foot. Dev Med Child Neurol 1993, 35, 927–931. [Google Scholar] [CrossRef] [PubMed]
- Ganger, R.; Radler, C.; Handlbauer, A.; Grill, F. External fixation in clubfoot treatment - a review of the literature. J Pediatr Orthop B 2012, 21, 52–58. [Google Scholar] [CrossRef]
- Ferreira, R.C.; Costa, M.T. Recurrent clubfoot--approach and treatment with external fixation. Foot Ankle Clin 2009, 14, 435–445. [Google Scholar] [CrossRef]
- Hefti, F. Pediatric Orthopedics in Practice. Springer Verlag Science & Business Med 2007. [Google Scholar]
- Chu, A.; Labar, A.S.; Sala, D.A.; van Bosse, H.J.; Lehman, W.B. Clubfoot classification: correlation with Ponseti cast treatment. J Pediatr Orthop 2010, 30, 695–699. [Google Scholar] [CrossRef]
- Bergerault, F.; Fournier, J.; Bonnard, C. Idiopathic congenital clubfoot: Initial treatment. Orthop Traumatol Surg Res 2013, 99, S150–159. [Google Scholar] [CrossRef]
- Treadwell, M.C.; Stanitski, C.L.; King, M. Prenatal sonographic diagnosis of clubfoot: implications for patient counseling. J Pediatr Orthop 1999, 19, 8–10. [Google Scholar] [CrossRef]
- Glotzbecker, M.P.; Estroff, J.A.; Spencer, S.A.; Bosley, J.C.; Parad, R.B.; Kasser, J.R.; Mahan, S.T. Prenatally diagnosed clubfeet: comparing ultrasonographic severity with objective clinical outcomes. J Pediatr Orthop 2010, 30, 606–611. [Google Scholar] [CrossRef]
- Brasseur-Daudruy, M.; Abu Amara, S.; Ickowicz-Onnient, V.; Touleimat, S.; Verspyck, E. Clubfoot Versus Positional Foot Deformities on Prenatal Ultrasound Imaging. J Ultrasound Med 2020, 39, 615–623. [Google Scholar] [CrossRef]
- Lanna, M.; Casati, D.; Torre, C.; Monforte, S.; Andreacchio, A.; Faiola, S.; Cetin, I.; Rustico, M. Congenital isolated clubfoot: Correlation between prenatal assessment and postnatal degree of severity. Prenat Diagn 2020, 40, 1547–1552. [Google Scholar] [CrossRef]
- Goncalves, L.F. Three-dimensional ultrasound of the fetus: how does it help? Pediatr Radiol 2016, 46, 177–189. [Google Scholar] [CrossRef]
- Cosma, D.; Vasilescu, D.E. A Clinical Evaluation of the Pirani and Dimeglio Idiopathic Clubfoot Classifications. J Foot Ankle Surg 2015, 54, 582–585. [Google Scholar] [CrossRef]
- Glotzbecker, M.P.; Estroff, J.A.; Curtis, T.A.; Kalish, L.A.; Spencer, S.A.; Parad, R.B.; Kasser, J.R.; Mahan, S.T. Prospective evaluation of a prenatal sonographic clubfoot classification system. Fetal Diagn Ther 2013, 34, 236–240. [Google Scholar] [CrossRef]
- Ippolito, E.; De Maio, F.; Mancini, F.; Bellini, D.; Orefice, A. Leg muscle atrophy in idiopathic congenital clubfoot: is it primitive or acquired? J Child Orthop 2009, 3, 171–178. [Google Scholar] [CrossRef]
- Hershkovitz, R.; Tepper, R. Sonographic nomogram of the fetal calf between 15 and 42 weeks' gestation using 3-dimensional sonography. J Ultrasound Med 2008, 27, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Brazell, C.; Carry, P.M.; Jones, A.; Baschal, R.; Miller, N.; Holmes, K.S.; Georgopoulos, G. Dimeglio Score Predicts Treatment Difficulty During Ponseti Casting for Isolated Clubfoot. J Pediatr Orthop 2019, 39, e402–e405. [Google Scholar] [CrossRef] [PubMed]
- Dimeglio, A.; Bensahel, H.; Souchet, P.; Mazeau, P.; Bonnet, F. Classification of clubfoot. J Pediatr Orthop B 1995, 4, 129–136. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).