1. Introduction
The consequences and complications of osteoporotic fractures have a more profound impact on quality of life than the most severe complications of diabetes mellitus, such as vision loss and limb amputation [
1]. In recent decades, the prevalence of osteoporosis has increased due to a sedentary lifestyle and rising life expectancy, leading to a higher incidence of fractures resulting from osteoporosis. The incidence of fractures occurring based on osteoporosis rises with advancing age [
2].
It was reported in 2000 that approximately 9 million fractures resulting from osteoporosis were diagnosed worldwide, including 1.7 million wrist fractures, 1.6 million hip fractures, and 1.4 million clinical vertebral fractures. Of these 9 million fractures, 34.8% affected European individuals. In Europe, osteoporotic fractures have imposed a more significant disease burden (DALY) than common cancers, except lung cancer [
3]. In the United States, 1.5 million osteoporotic fractures are diagnosed annually, including 700,000 vertebral fractures, 250,000 wrist fractures, 250,000 hip fractures, and 300,000 other limb fractures [
4].
The prevalence of osteoporotic fractures in Europe ranges from 18% to 26% among women aged at least 50 [
5]. In Hungary, the prevalence of osteoporotic vertebral fractures is 48 per 100,000 per year; however, this calculation is based solely on the number of hospitalized patients [
2].
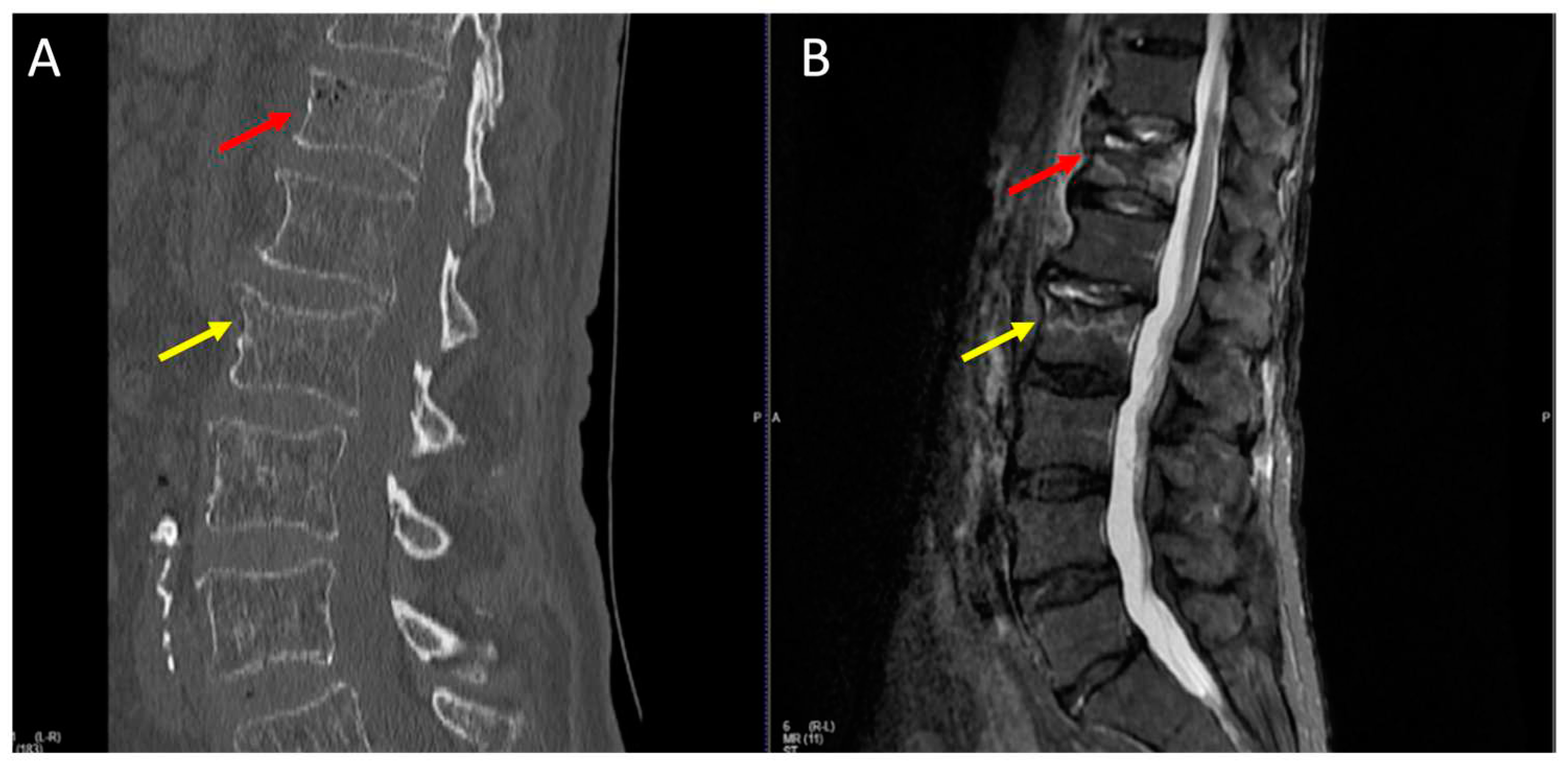
When there is a suspicion of osteoporotic vertebral fractures (OVF), employing radiological techniques like computed tomography (CT) and magnetic resonance imaging (MRI) is required. Deciding on what kind of imaging modality we have to use is widely controversial due to the time and resources required to do an MRI scan for each suspected patient. However, MRI is widely acknowledged as the most effective method for identifying bone contusions following trauma, which are typically indicative of a mix of trabecular microfractures, edema, and hemorrhage [
6,
7].
It is important to highlight that CT scans alone may miss some cases of OVF [
8]. However, meta-analysis studies indicate that when CT scanning is combined with MRI, the effectiveness in detecting OVF significantly increases [
8,
9]. The usefulness of MRI in diagnosing spinal fractures has been discussed in previous reports, where the sensitivity of MRI in detecting vertebral fractures was regarded as 100% [
10]. Additionally, MRI proves to be more effective than traditional radiographs or CT scans in revealing avascular necrosis and detecting occult fractures [
11]
It is essential to emphasize that while STIR sequence MR imaging has been acknowledged as more sensitive in detecting fresh fractures than CT scans, no previous analysis has investigated whether therapeutic implications or benefits are associated with detecting additional fractures. This approach, STIR MRI of the entire spine, is suitable for detecting fractures that are not yet detectable by CT scans [
12]. Its sensitivity and specificity have been reported as exceeding 94% in diagnosing fractures resulting from osteoporosis [
13,
14,
15], with a positive and negative predictive value exceeding 90%.
After the initial diagnosis of an osteoporotic vertebral fracture, regardless of whether it receives conservative or surgical treatment, there is a 34% likelihood of a secondary fracture occurring within one year. Secondary fractures manifest as contusions, wedges, or burst fractures [
16]. An adjacent segment fracture is a new fracture that occurs after surgical intervention in a nearby segment. The risk of developing adjacent segment syndrome is higher among patients undergoing percutaneous vertebroplasty (PVP) than those receiving conservative treatment [
17].
The classification of osteoporotic vertebral fractures has evolved from the previously accepted AO classification [
18], giving rise to the Osteoporotic Vertebral Fracture Classification (OF) [
19]. According to the OF classification, stage 1 fractures exhibit the sole sign of edematous changes in the vertebral body. These edematous changes are not visible on CT scans but can be detected as signal intensity enhancement on STIR sequence MR images.
A notable increase in the occurrence of minor vertebral fractures associated with osteoporosis over a ten-year period at the Manninger Jenő National Traumatology Institute of Péterfy Sándor Street Hospital and Outpatient Clinic, from November 1, 2008, to October 31, 2018). Our experience suggests that performing solely CT scan alone is insufficient for detecting fresh fractures.
The question arose about whether impending adjacent segment fractures can be observed in their initial form when diagnosing the first osteoporotic vertebral fracture using STIR sequence MR images. We hypothesize that the underlying factors for neighboring segment fractures, which may occur later, are already present during the first osteoporotic fracture in the form of early-stage abnormalities (e.g., contusions, edematous changes) detectable on STIR sequence MR images.
We aimed to determine whether MR imaging using the STIR sequence can detect additional fractures besides CT-confirmed fractures. We also aimed to compare the number of fractures detected by CT and STIR sequence MR imaging and assess the therapeutic implications of STIR sequence MR imaging results, specifically how they influence the patient's conservative or surgical treatment plan.
2. Materials and Methods
In the scope of a prospective study conducted from July 1, 2019, to November 30, 2019, we investigated a cohort of patients aged 50 and above who had experienced minor injuries resulting in vertebral fractures. The inclusion criteria were as follows: patients aged 50 or older, thoracolumbar vertebral fractures resulting from minor trauma, concurrent full spine CT scan, and full spine sagittal STIR sequence MR imaging, with no more than 24 hours between the CT and MR examinations. Exclusion criteria included a history of tumors, ankylosing spondylitis, and diffuse idiopathic skeletal hyperostosis.
Initially, a CT scan of the thoracolumbar spine was performed, followed by a full spine sagittal STIR sequence MRI examination, which also helped minimize the time the patient was placed in an immobile position due to pain.
Radiologists and neurosurgeons independently evaluated the CT and MR images. For each CT and MRI, the number of fresh fractures diagnosed by radiologists and neurosurgeons was assessed separately, broken down into cervical, thoracic, lumbar, and sacral segments. Additionally, we investigated whether individual CT and MR images indicated single (affecting a single vertebral body) or multiple (affecting more than one vertebral body) fractures, and in cases of multiple fractures, whether adjacent fractured vertebral bodies or distant (non-adjacent) fractured vertebral bodies were observed.
The number of fractures was considered a continuous variable, while the presence or absence of single or multiple fractures and neighboring fractures were treated as dichotomous variables.
We examined whether the full spine sagittal STIR sequence MRI modified the conservative or surgical treatment plan established based on the CT examination. The treatment plan set with the CT examination was modified based on MR imaging when:
The CT examination revealed a lumbar vertebral fracture but not a thoracic fracture, yet the concurrently conducted MR imaging confirmed a thoracic vertebral fracture. In these cases, the external orthosis was extended to the thoracic spine, and the modification of conservative treatment based on MR imaging is discussed.
The fracture confirmed by CT imaging was deemed unstable (AO A3, A4 fracture), and concurrently conducted MR imaging revealed a fracture in the vertebral body below or above the planned surgical extension during the CT examination. In these vertebral bodies, bone cement was injected using the PVP method to prevent their presumed future collapse. In these cases, the modification of surgical treatment based on MR imaging is discussed.
The fracture confirmed by CT imaging was not deemed unstable (AO A1, A2). However, the concurrently conducted MR imaging showed signal enhancement on STIR sequences in the peduncles and arches of the vertebrae or indicated ligamentous injury. In these cases, the conservative treatment based on the CT examination was modified to surgical therapy based on MR imaging.
Data statistical analysis was performed using GraphPad Prism 10 software. Descriptive statistics, including mean ± standard deviation (SD), were used to summarize continuous variables. Categorical variables were presented as frequencies and percentages. We employed the Chi-square test for independence to assess the association between CT and STIR MRI in diagnosing the fractures. A p-value less than 0.05 was considered statistically significant.
3. Results
In a prospective study conducted between July 1, 2019, and November 30, 2019, 64 patients met the inclusion criteria. The gender distribution among patients was 64% female and 36% male, with an average age of 75.5 years (SD = 9.29). The youngest patient was 52 years old, while the oldest was 91 years old.
Based on the CT scans, 161 fresh vertebral fractures were diagnosed. On the STIR MRI, 266 vertebral fractures were diagnosed (
Table 1). This includes fractures shown only on the STIR sequence MRI and those confirmed by CT examination. The MR imaging identified 1.65 times more fractures (266/161) than the CT scans (
Table 1).
Based on the results of the paired t-test (or one-sample t-test for the difference between the two samples), we significantly diagnosed more fractures with the STIR sequence MR imaging compared to CT scans (p(t) < 0.01, p = 5.34, SD = 2.46, SE = 0.31).
CT scans identified single fractures in 27% of patients (17 cases), whereas MR imaging detected them in only 9% of patients (6 cases). In the case of multiple fractures, CT scans identified them in 73% of patients (47 cases), while MR imaging detected them in 91% of patients (58 cases) (
Table 2).
Based on the chi-square test for independence and homogeneity, there was a significant difference in the number of single and multiple fractures diagnosed with CT scans versus SITR MR imaging, with a Chi-square value of (1; 128) = 6.41, p-value = 0.0113 (
Table 2 and
Figure 1).
Among multiple fractures involving multiple vertebral bodies, CT scans identified adjacent vertebral fractures in 74% of cases (35/47 cases), while STIR MR imaging detected them in 88% of cases (51/58 cases). Notably, the STIR MRI identified adjacent fractures in 1.5 times more patients than CT scans (
Table 3).
Within multiple fractures involving multiple vertebral bodies, non-adjacent vertebral fractures were observed in 26% of cases by CT scans (12 cases) and in 12% of cases by STIR MR imaging (7 cases) (
Table 3 and
Figure 1).
Based on the chi-square test for independence and homogeneity, there was no significant difference in the number of adjacent and non-adjacent fractured segments diagnosed with CT scans versus STIR MR imaging, with a chi-square value of (1; 105) = 3.175, p-value = 0.0747 (
Table 3).
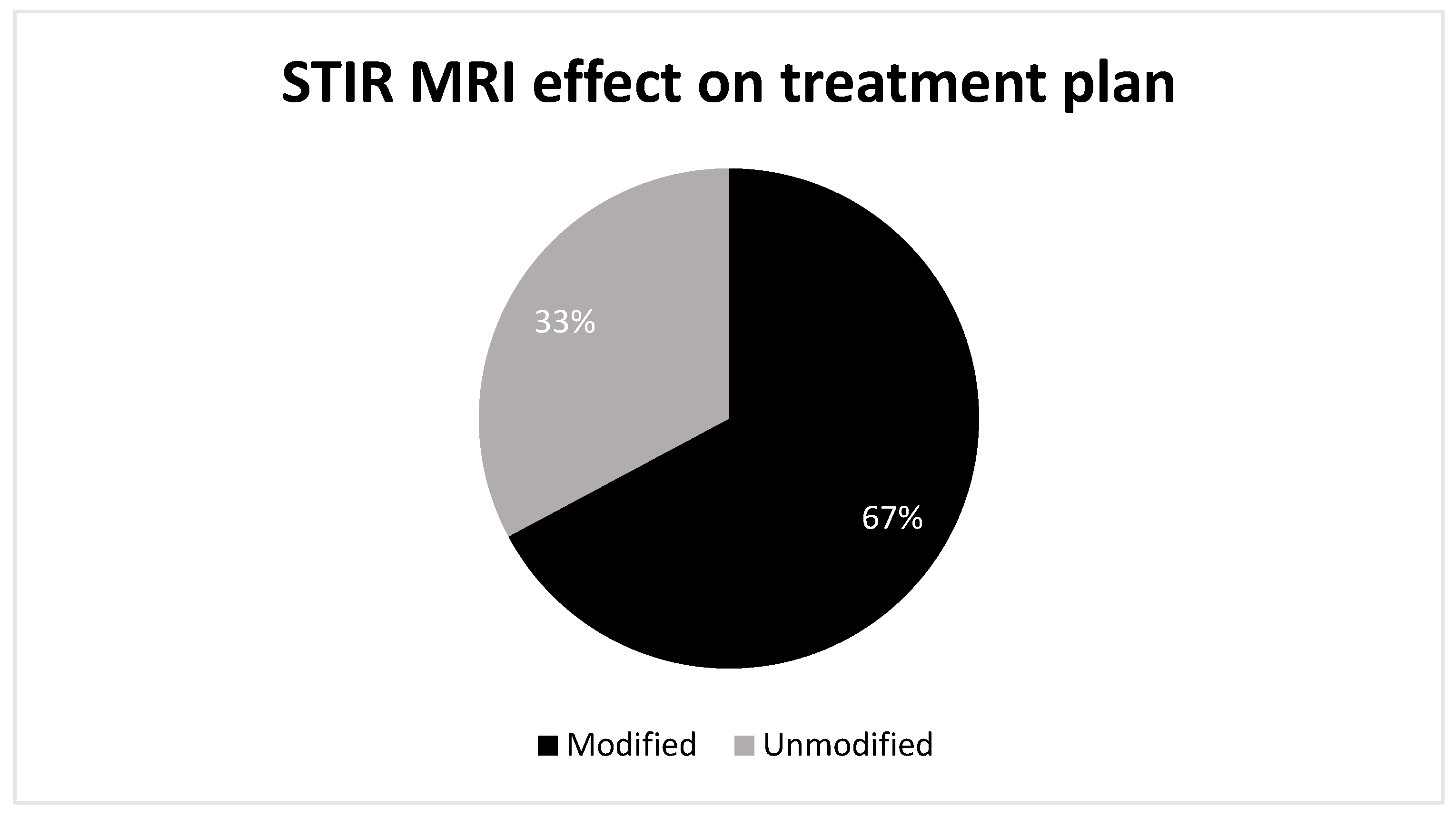
In this context, the MRI altered the conservative or surgical treatment plan established by CT scans in 67% of patients (43 cases). In 33% of cases (21 instances), the STIR MR imaging results were inconclusive regarding treatment decisions (
Figure 2).
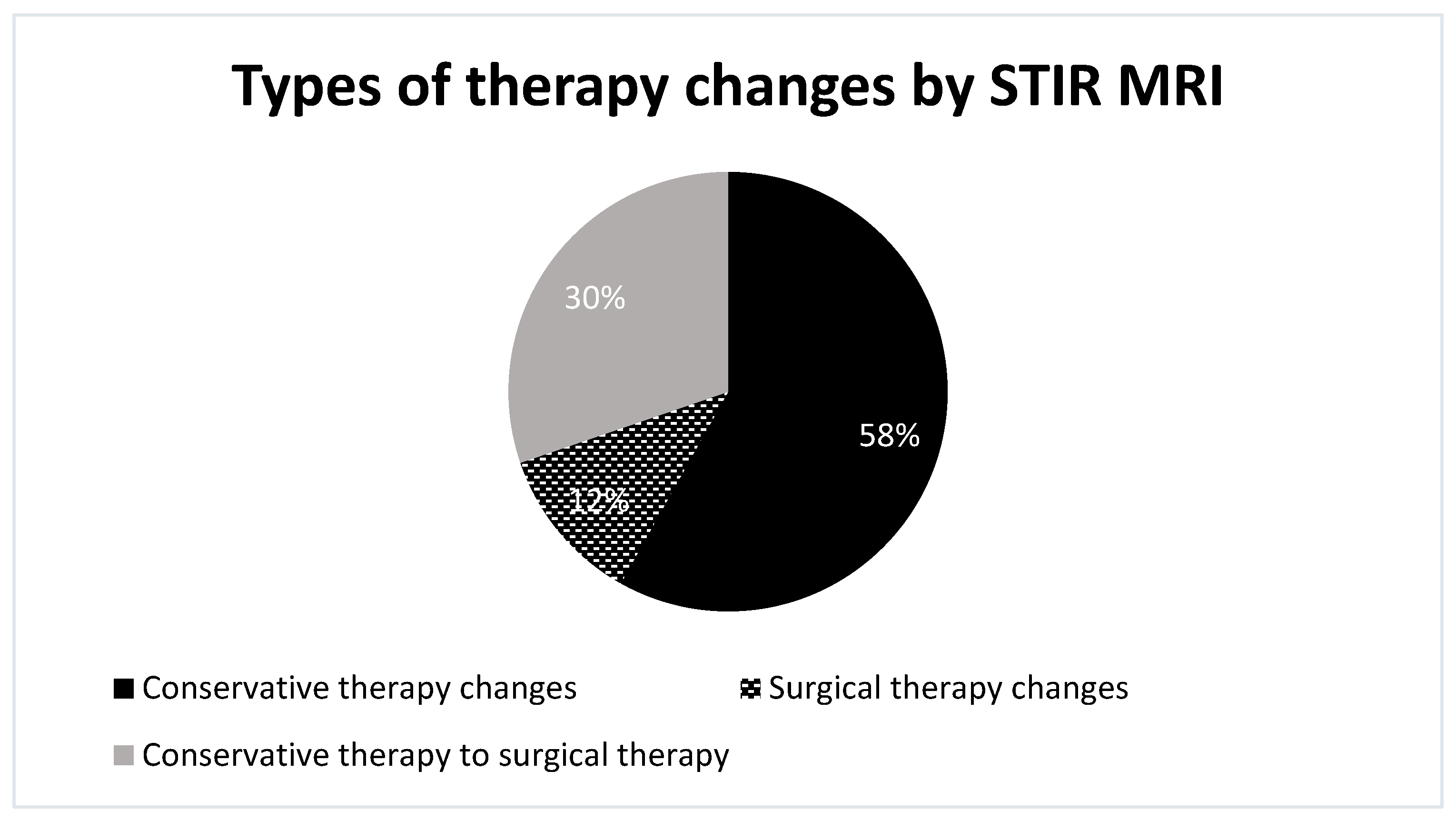
More specifically, within this group, STIR MRI scans led to changes in the type of conservative therapy in 58% of cases (25 instances), conversion from conservative to surgical treatment in 30% of cases (13 instances), and changes in the type of the surgical treatment in 12% of cases (5 instances) (
Figure 3).
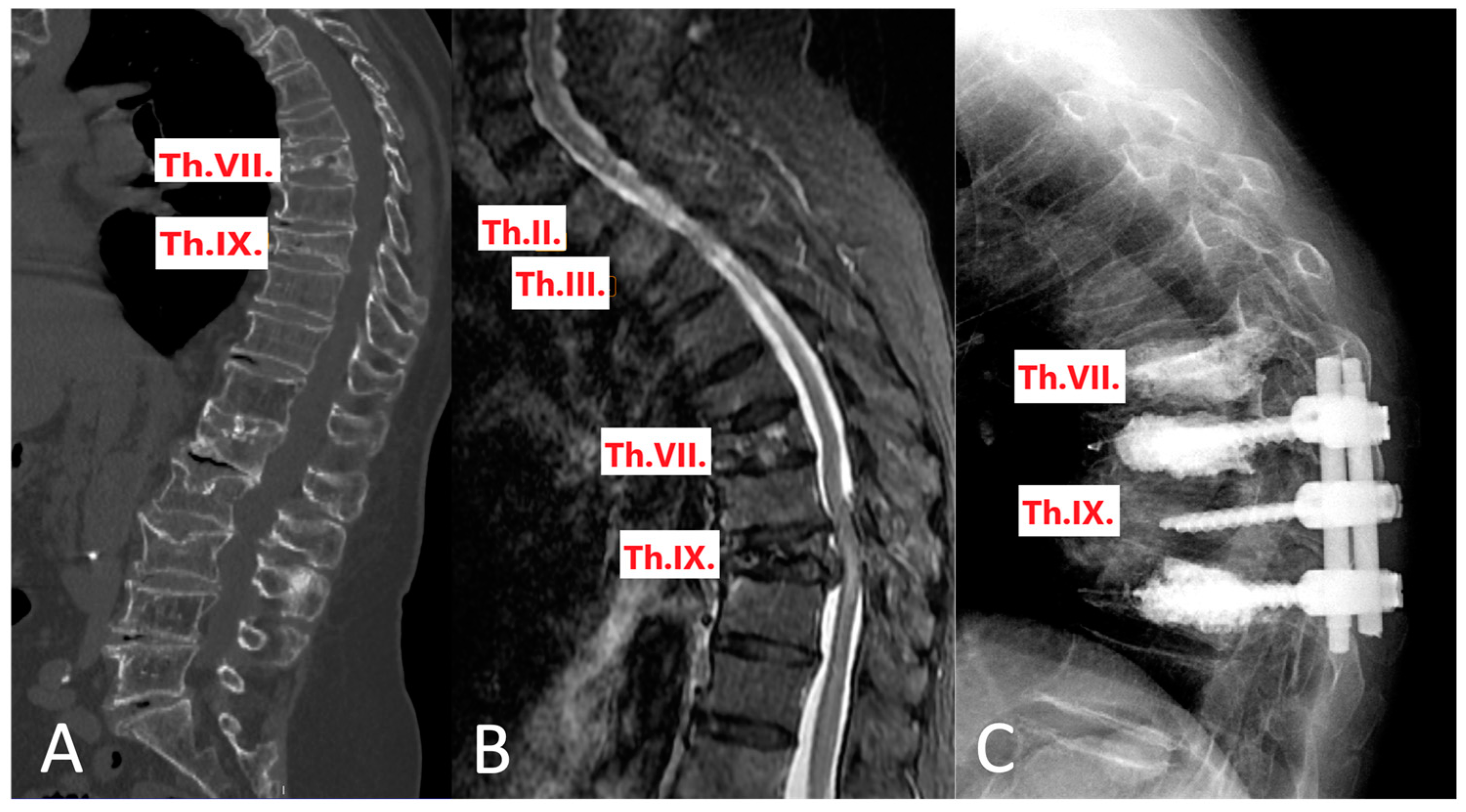
A notable case can be highlighted: A patient initially underwent a CT scan that identified fractures at the ThVII and ThIX vertebrae. However, subsequent STIR MRI imaging provided a more detailed assessment of the fracture types. Based on the CT findings, a long posterior spinal fixation was planned, from ThVII to ThX, accompanied by cementoplasty at ThVII and ThX. The STIR MRI revealed that the fracture at ThVII was only an AO1 type, where it was thought an AO3 type based on CT. Consequently, this led to a revised plan involving a shorter fixation range from ThVIII to ThX, while still proceeding with cementoplasty at ThVII and ThX (
Figure 4).
Based on the independent samples t-test, it can be concluded that there is a significant statistical correlation between the number of fractures diagnosed with STIR MR imaging versus CT imaging and the therapeutic impact of STIR MR imaging (p < 0.01).
4. Discussion
This study highlights the superior sensitivity of STIR sequence MR imaging over CT scans in detecting vertebral fractures in older patients. The finding that STIR MR imaging identified 1.65 times more fractures than CT scans underscores the potential underdiagnosis of vertebral fractures when relying solely on CT imaging. This has profound implications for clinical practice, particularly in the management of osteoporotic fractures.
The increased detection of both single and multiple fractures by STIR MR imaging, as evidenced by the significant differences in the paired t-test and chi-square test results, suggests that STIR MR imaging could alter the clinical perception of the extent of injury. This is particularly relevant in osteoporotic fractures, where accurate diagnosis is crucial for effective treatment planning and better patient outcome. The study's findings reinforce the hypothesis that STIR sequence MR imaging could reveal early-stage abnormalities, possibly altering treatment from conservative to surgical or modifying surgical plans.
In the late 1990s and around the turn of the century, it was already established that the sensitivity and specificity of STIR sequence MR imaging exceeded 94% [
6,
7,
8]. The positive and negative predictive values were over 90% for diagnosing fractures resulting from osteoporosis [
20].
Markus Lenski and colleagues aimed to assess the associated osteoporotic and long-standing fractures using STIR MR imaging in patients with recent traumatic fractures. Their approach involved STIR MR imaging, which identified associated fractures in 26% of cases and long-standing fractures in 60% of cases. The likelihood of associated fractures decreased as the number of long-standing fractures and T-scores increased. Lower T-scores and fewer long-standing fractures were identified as risk factors for such fractures. STIR MR imaging helps detect missed spinal fractures in the thoracic and lumbar spine [
21].
However, F. D. Lensing and colleagues' research shed light on the significantly lower sensitivity of STIR sequence MR imaging in individuals aged 57 and above compared to those younger than 57. Consequently, elderly patients with osteopenia may have acute fractures without an increased signal intensity on the STIR sequence MR imaging [
22].
Paula J. Richards' research results suggest that if the lateral cervical CT results are negative, MR imaging is necessary. Furthermore, MR imaging is justified for local neurological abnormalities, intervertebral disc or spine column injuries, and preparation for surgery. In such cases, obtaining at least one sagittal STIR sequence MR image of the entire spine is advisable to detect non-contiguous fractures and edematous changes and conduct a detailed CT examination for edematous changes [
23].
Similar to our approach, Ranjana Gupta and colleagues found that STIR sequence MR imaging should be included in routine spine examinations (lumbar spine). By adding the STIR sequence, they detected 24 conditions (fractures, atypical appendicitis, sacroiliitis, and joint degenerative changes) that were not diagnosable without the STIR sequence in a sample of 35 patients [
24].
R.L. Williams and colleagues stated spinal instability can be rapidly diagnosed with MR imaging without additional tests. They examined 22 patients with fresh fractures and unstable spines using T1W gradient echo (GE) and STIR sequence MR imaging. They noted both bone and soft tissue injuries, as well as indirect signs of instability (e.g., soft tissue hemorrhage). Unlike us, they did not rely on CT scans and obtained STIR sequence and T1W GE images [
25].
Giuseppe M. and colleagues aimed to quantify overlooked osteoporotic fractures and assess the role of MR imaging in early diagnosis and classification. They compared MR imaging to X-ray examinations. Their results showed that MR imaging modified the original diagnosis in 52% of patients. In 43.9% of cases, MR imaging detected one or more new fractured vertebrae that were not visible on X-rays. In 14 cases, MR imaging contradicted the fracture diagnosis made by X-ray examination [
26].
MRI identified contusions in 36.4% of cases (93 patients), which were not visible on X-ray examinations. MR imaging modified the classification of fractures in 28.9% of cases. These findings underscore the potential of MRI to provide more accurate and comprehensive information compared to traditional X-ray examinations [
26].
In contrast to the mentioned studies, we conducted research comparing the effectiveness of CT and MR imaging. A study published for the first time in 2005 by J. Grünhagen and colleagues aimed to classify spinal injuries using CT and MR imaging according to the Magerl classification [
21]. They examined 46 fractured vertebrae of 39 patients using CT and MR imaging (transverse and sagittal T1W spin echo, sagittal T2W spin echo, and sagittal STIR sequence).
Each fractured vertebra was categorized twice independently using CT and MR images according to the Magerl classification, and these classifications were then compared. The results showed that out of 46 fractures, only 5 received a different classification based on CT images compared to MR images. MR imaging revealed more bone lesions and detected the ligamentum longitudinal rupture in 5 patients [
27].
Kofi-Buaku Atsina and colleagues examined the importance of full spine MR imaging after a full spine CT examination in cases of single or multiple vertebral fractures. They analyzed patients who had suffered blunt injuries and underwent both full spine CT and MR imaging. Sagittal T2W or T1W sequences were combined with the STIR sequence. The findings from CT and MRI were compared. A total of 156 patients were examined, and 29 had additional injuries (bone and/or soft tissue injuries) indicated by MR imaging compared to CT imaging. These other injuries were categorized as contusions or compression fractures without significant volume reduction, which the research group considered "likely not to have influenced the treatment plan" [
28].
However, they were unaware of whether these additional fractures influenced the treatment plan, as no neurosurgeons or spine surgeons were involved in the assessment; only radiologists participated.
In contrast, our research systematically explored the influence of STIR sequence MR imaging results on treatment plans compared to plans based solely on CT imaging. Our findings demonstrated that in most cases (63%), the information derived from STIR MR imaging led to adjustments in the treatment plan, diverging from the initial plan constructed solely based on CT imaging. Furthermore, we did not rely exclusively on reporting during data collection but analyzed CT and STIR MR images slice by slice while searching for signs of fresh fractures.
Moreover, the alteration of treatment plans in 67% of cases based on STIR MRI findings further demonstrates the clinical relevance of this imaging modality. This suggests that incorporating STIR MRI which takes only 5-10 minutes to complete into the diagnostic pathway could lead to more comprehensive management strategies for patients with osteoporotic fractures, potentially reducing the risk of secondary fractures and improving overall outcomes.
The study conclusively demonstrates the superior efficacy of STIR sequence MR imaging over CT scans in detecting vertebral fractures in older patients. This advanced diagnostic capability significantly influences treatment plans, advocating for the integration of STIR MRI in evaluating osteoporotic fractures. These findings, highlighting the potential for improved patient outcomes through more accurate fracture detection, underscore the need for further research to establish STIR MRI as a standard diagnostic tool in osteoporosis management.
Future research should validate these findings in a larger, more diverse population and explore the long-term outcomes of treatment modifications based on MR imaging. The potential for STIR MRI to significantly impact the management of osteoporotic fractures warrants further investigation.
Author Contributions
Conceptualization, R.V, and A.V.; methodology, R.V., S.A., M.W.A-S.; formal analysis and investigation, all authors; data curation, R.V., S.A.; writing—original draft preparation, R.V., S.A., M.W.A-S.; writing—review and editing, A.V., M.W.A-S; supervision, A.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki. Ethical review and approval were not applicable in this study. This study was conducted retrospectively.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study to do the procedures and to publish this paper.
Data Availability Statement
All data produced or examined in this study have been included in this published article.
Acknowledgments
We want to express our sincere gratitude to the Department of Neurosurgery and Neurotraumatology staff at Péterfy Hospital—Manninger Jeno ̋ National Traumatology Institution in Budapest, Hungary.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vokó Z, Gáspár K, Inotai A, Horváth C, Bors K, Speer G, et al. Osteoporotic fractures may impair life as much as the complications of diabetes. J Eval Clin Pract. 2017 Dec;23(6):1375–80. [CrossRef]
- Péntek M, Horváth C, Boncz I, Falusi Z, Tóth E, Sebestyén A, et al. Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999-2003. Osteoporos Int. 2008 Feb;19(2):243–9. [CrossRef]
- Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006 Dec;17(12):1726–33. [CrossRef]
- Riggs BL, Melton LJ. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995 Nov;17(5 Suppl):505S-511S. [CrossRef]
- Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017 May;28(5):1531–42. [CrossRef]
- Miller MD, Osborne JR, Gordon WT, Hinkin DT, Brinker MR. The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med. 1998;26(1):15–9. [CrossRef]
- Qaiyum M, Tyrrell PN, McCall IW, Cassar-Pullicino VN. MRI detection of unsuspected vertebral injury in acute spinal trauma: incidence and significance. Skeletal Radiol. 2001 Jun;30(6):299–304. [CrossRef]
- Schoenfeld AJ, Bono CM, McGuire KJ, Warholic N, Harris MB. Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma. 2010 Jan;68(1):109–13; discussion 113-114. [CrossRef]
- Kepler CK, Bogner EA, Herzog RJ, Huang RC. Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J. 2011 Apr;20(4):550–6. [CrossRef]
- Terakado A, Orita S, Inage K, Kubota G, Kanzaki T, Mori H, et al. A Clinical Prospective Observational Cohort Study on the Prevalence and Primary Diagnostic Accuracy of Occult Vertebral Fractures in Aged Women with Acute Lower Back Pain Using Magnetic Resonance Imaging. Pain Res Manag. 2017;2017:9265259. [CrossRef]
- Wang YF, Teng MMH, Chang CY, Wu HT, Wang ST. Imaging manifestations of spinal fractures in ankylosing spondylitis. AJNR Am J Neuroradiol. 2005 Sep;26(8):2067–76.
- Blattert TR, Schnake KJ, Gonschorek O, Gercek E, Hartmann F, Katscher S, et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine Journal. 2018 Sep 1;8(2_suppl):50S-55S. [CrossRef]
- Heynen B, Tamigneaux C, Pasoglou V, Malghem J, Vande Berg B, Kirchgesner T. MRI detection of radiographically occult fractures of the hip and pelvis in the elderly: Comparison of T2-weighted Dixon sequence with T1-weighted and STIR sequences. Diagn Interv Imaging. 2019 Mar;100(3):169–75. [CrossRef]
- Breitenseher MJ, Metz VM, Gilula LA, Gaebler C, Kukla C, Fleischmann D, et al. Radiographically occult scaphoid fractures: value of MR imaging in detection. Radiology. 1997 Apr;203(1):245–50. [CrossRef]
- Wang B, Fintelmann FJ, Kamath RS, Kattapuram SV, Rosenthal DI. Limited magnetic resonance imaging of the lumbar spine has high sensitivity for detection of acute fractures, infection, and malignancy. Skeletal Radiol. 2016 Dec;45(12):1687–93. [CrossRef]
- Green R a. R, Saifuddin A. Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol. 2004 Mar;33(3):129–35. [CrossRef]
- Percutaneous Vertebroplasty for Treatment of Painful Osteoporotic Vertebral Compression Fractures. Ont Health Technol Assess Ser. 2010 Oct 1;10(19):1–45. [CrossRef]
- Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. [CrossRef]
- Schnake KJ, Blattert TR, Hahn P, Franck A, Hartmann F, Ullrich B, et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018 Sep;8(2 Suppl):46S-49S. [CrossRef]
- Yuan WH, Mu-Huo Teng M, Hsu HC, Sun YC, Chang CY. Are Non-contrast MR Images enough for Detection of Fracture Levels Prior to Percutaneous Vertebroplasty in Patients with Osteoporosis? Interv Neuroradiol. 2008 Nov;14(Suppl 2):79–84.
- Lenski M, Büser N, Scherer M. Concomitant and previous osteoporotic vertebral fractures. Acta Orthop. 2017 Apr;88(2):192–7. [CrossRef]
- Lensing FD, Bisson EF, Wiggins RH, Shah LM. Reliability of the STIR Sequence for Acute Type II Odontoid Fractures. AJNR Am J Neuroradiol. 2014 Aug;35(8):1642–6. [CrossRef]
- Richards PJ. Cervical spine clearance: a review. Injury. 2005 Feb;36(2):248–69; discussion 270.
- Gupta R, Mittal P, Mittal A, Mittal K, Gupta S, Kaur R. Additional merit of coronal STIR imaging for MR imaging of lumbar spine. J Craniovertebr Junction Spine. 2015;6(1):12–5. [CrossRef]
- Williams RL, Hardman JA, Lyons K. MR imaging of suspected acute spinal instability. Injury. 1998 Mar;29(2):109–13. [CrossRef]
- Marongiu G, Congia S, Verona M, Lombardo M, Podda D, Capone A. The impact of magnetic resonance imaging in the diagnostic and classification process of osteoporotic vertebral fractures. Injury. 2018 Nov;49 Suppl 3:S26–31. [CrossRef]
- Grünhagen J, Egbers HJ, Heller M, Reuter M. [Comparison of spine injuries by means of CT and MRI according to the classification of Magerl]. Rofo. 2005 Jun;177(6):828–34. [CrossRef]
- Atsina KB, Rozenberg A, Selvarajan SK. The utility of whole spine survey MRI in blunt trauma patients sustaining single level or contiguous spinal fractures. Emerg Radiol. 2019 Oct;26(5):493–500. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).