1. Introduction
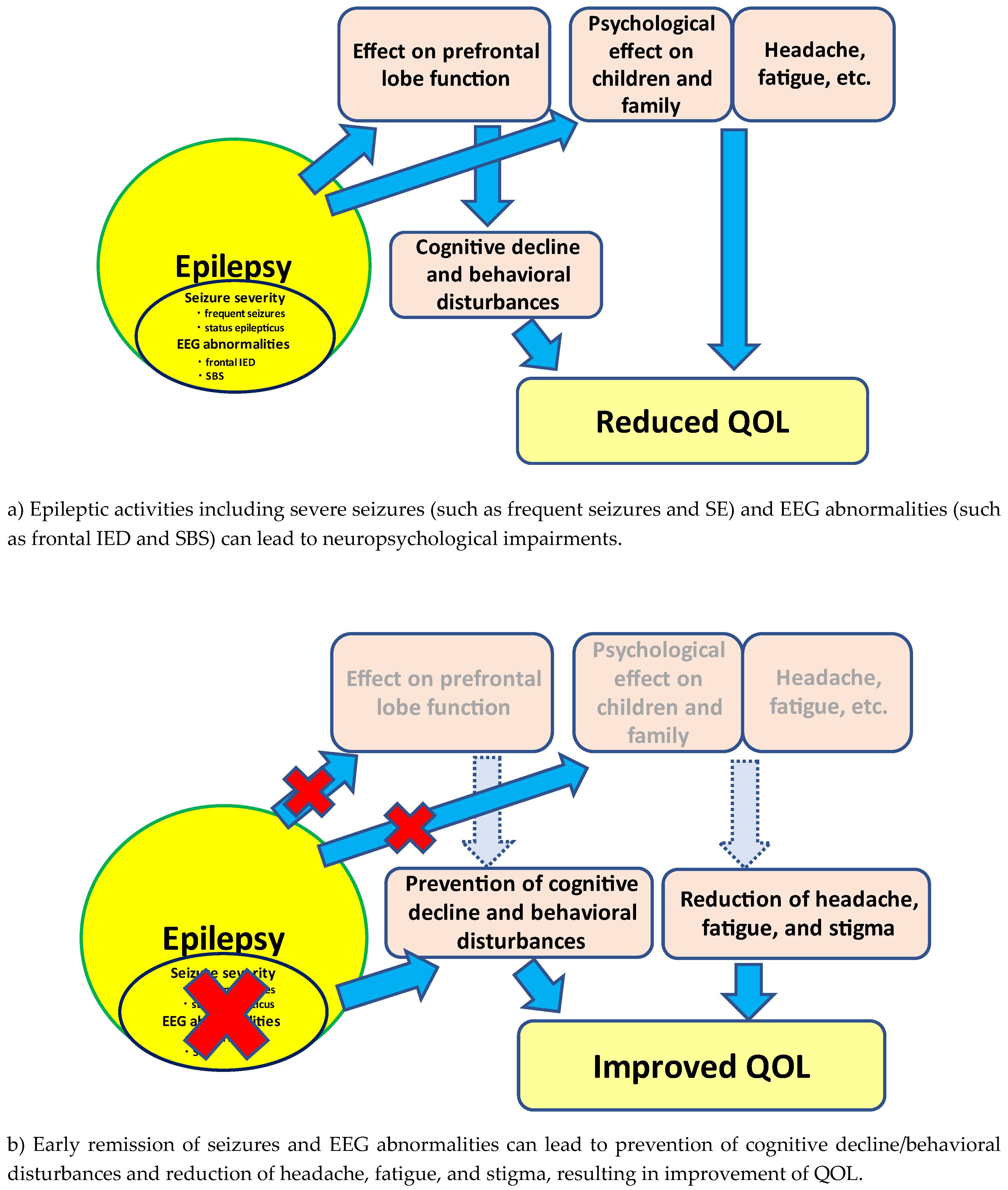
Quality of life (QOL) in children with epilepsy seems to be influenced by various factors, including clinical and social variables. Among these, seizure frequency and presence of status epilepticus (SE) are regarded as the main QOL-related factors. In addition, electroencephalogram (EEG) findings such as frequency of interictal epileptiform discharges (IEDs) may also be related to cognitive decline and behavioral disturbances. Moreover, epileptic activities such as frequent seizures and IEDs may mediate emotional states including stigma and fatigue in children with epilepsy. These findings suggest that epileptic activities including frequent seizures/presence of SE and IEDs on EEG can lead to reduced QOL in children with epilepsy.
Neuropsychological impairments such as cognitive decline and behavioral disturbances in children with epilepsy can be caused by several factors. Frontal lobe lesions may lead to cognitive decline and behavioral disturbances in consonance with lesion location. However, children with no lesions can also present with these disturbances. A previous study showed a negative correlation between frequency of IEDs on EEG and cognitive functions in self-limited epilepsy with centrotemporal spike (SeLECTS) [
1]. These impairments may thus relate to the topography and epileptic activities.
On the other hand, stigma is regarded to be an important QOL-related factor in epilepsy. Perception of stigma related to the epileptic condition may be very severe and is often under-recognized by clinicians. Stigma has a marked negative impact for not only children, but also their families. Reducing perceptions of stigma is thus necessary for the clinical management of childhood epilepsy.
In addition, fatigue is associated with reduced QOL in patients with epilepsy. Fatigue in patients with epilepsy may correlate with psychosocial factors, including anxiety, depression, and sleep problems [
2]. Fatigue is considered to be associated with several issues in epilepsy. A previous study showed that frequent seizures can lead to increased fatigue [
3]. Fatigue may also relate to epileptic activities.
The frontal lobes mature over a long period and so is easily damaged by various factors. Damage to the frontal regions during childhood interferes with maturational and organizational processes, which can lead to neuropsychological impairments [
4]. Results from previous investigations have suggested that severe seizures as reflected by statuses such as frequent seizures and SE can impair the developing brain [
4,
5,
6]. In combination with these studies, seizure severity and IED on EEG may lead to cognitive, behavioral, and psychological disturbances. Epileptic activities such as seizure severity and/or IEDs are important QOL-related factors in childhood epilepsy.
2. Can seizure severity lead to reduced QOL in childhood epilepsy?
2.1. Seizure severity and cognitive/behavioral disturbances; are they related?
Neuropsychological impairments such as cognitive decline and behavioral disturbances will reduce QOL in childhood epilepsy. Cognitive declines and behavioral deterioration may be induced by frontal lobe dysfunction. In addition, QOL reduction in children can also reduce QOL in the family. Frontal lobe dysfunction can thus result in reduced QOL for both the child and their family.
The frontal lobes are the largest cortical regions of the brain, comprising approximately 40% of the cerebral cortex. Among these regions, the prefrontal regions involve wide networks [
7]. Because of these connections, the prefrontal cortex can receive abundant information from all parts of the cerebrum, and can affect information processing in those parts. Prefrontal lobe neurons and glial cells are readily influenced by various factors, so prefrontal lobe functions are regarded as vulnerable for a long period [
8]. Accordingly, severe seizures, such as with frequent or prolonged seizures, more easily results in negative effects on prefrontal lobe functions than other cortical regions [
7,
8]. Considering these findings, epilepsy associated with prefrontal regions in children may be associated with several neuropsychological impairments in comparison with healthy subjects [
9].
2.1.1. Prefrontal lobe growth in frontal lobe epilepsy
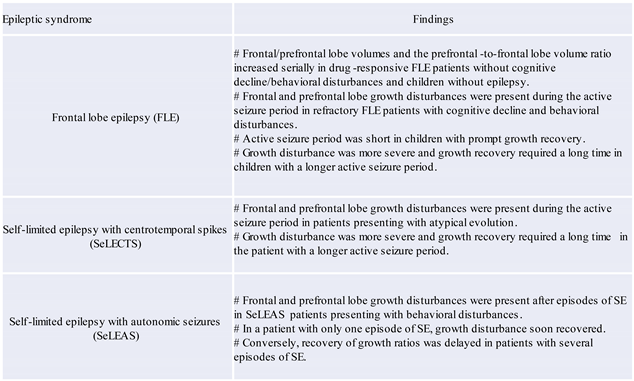
Understanding how frontal lobe epilepsy (FLE) impacts the life of the patient seems important. In a serial 3-dimensional (3D)-magnetic resonance imaging (MRI) volumetric study, growth of the frontal and prefrontal lobes in children with drug-responsive FLE without neuropsychological impairments was similar to that in healthy subjects [
8]. In contrast, frontal and prefrontal lobe growth disturbances were present during the active epileptic phase in refractory FLE patients with cognitive declines and behavioral disturbances. However, a difference in association with the active seizure period was present. The active seizure period was short in children with prompt growth recovery. In children with a longer active seizure period, the growth disturbance was more severe and growth recovery required a long time [
8] (
Table 1). Frequent seizures in children with FLE may thus induce prefrontal lobe growth disturbance, which can lead to neuropsychological impairments.
2.1.2. Prefrontal lobe growth in SeLECTS
SeLECTS is considered a condition free of neurological and psychological impairments. However, children with SeLECTS sometimes present with severe aggravation of epileptic manifestations and cognitive decline/behavioral disturbances. Frontal and prefrontal lobe volumes and the prefrontal-to-frontal lobe volume ratio in particular showed growth disturbances during the active seizure period in patients presenting with atypical evolution [
7]. However, differences in association with active seizure period were present. Active seizure period was short in the patient with prompt growth recovery. In the patient with a longer active seizure period, the growth disturbance was more severe, and growth recovery required a long time [
7] (
Table 1). Seizure severity in SeLECTS may thus be associated with prefrontal lobe growth disturbance, which can lead to neuropsychological impairments.
2.1.3. Prefrontal lobe growth in self-limited epilepsy with autonomic seizures
Self-limited epilepsy with autonomic seizures (SeLEAS), which represents Panayiotopoulos syndrome, is generally accepted to lack neuropsychological impairments. However, cognitive declines and behavioral disturbances may be present in at least some children with SeLEAS. SE can induce cerebral damage to various degrees. In SeLEAS patients, the seizure tends to be prolonged, with subsequent focal or focal to bilateral tonic-clonic SE [
10]. A sequential study by 3D-MRI volumetry showed that frontal and prefrontal lobe growth disturbances were present after episodes of SE in SeLEAS patients presenting with behavioral disturbances. In a patient with only one episode of SE, growth disturbance soon recovered. Conversely, recovery of growth ratios was delayed in patients with several episodes of SE [
11] (
Table 1). Moreover, cognitive scores as measured using the Wechsler intelligence scale for children dropped after SE episodes [
11]. The presence of SE in children with SeLEAS may thus induce growth disturbance of prefrontal lobe, which can lead to neuropsychological impairments.
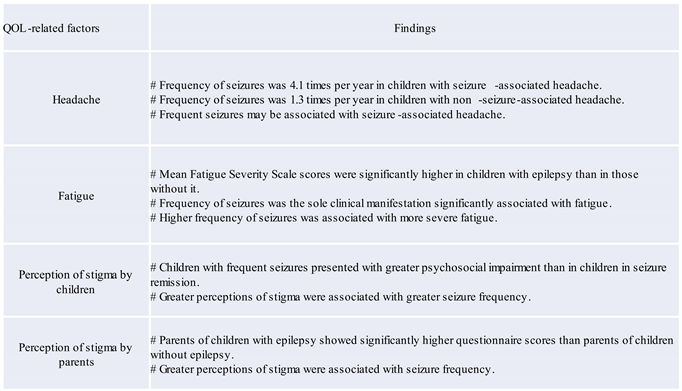
2.2. QOL-related factors; headache
Epilepsy and migraine are a heterogeneous family of neurological disorders [
12]. The prevalence of headache is extremely high, so concomitant headache can be present in many patients with epilepsy. Approximately 35% of epileptic children experienced headaches in association with seizures in our previous study [
13]. The frequency of seizures in children with and without seizure-associated headache was 4.1 and 1.3 times per year, respectively [
13] (
Table 2). Thus, seizure recurrence may induce headaches in association with seizures, which lead to reduced QOL in children with epilepsy.
2.3. QOL-related factors; fatigue
Fatigue has a negative impact on QOL in patients with various chronic diseases, including epilepsy [
14,
15,
16]. Our previous study showed that mean Fatigue Severity Scale scores in epileptic children were significantly higher than those in non-epileptic children [
17]. Frequency of seizures was identified as the only significant clinical manifestation in association with fatigue by multiple linear regression analysis. Moreover, children with frequent seizures presented with more severe fatigue [
17] (
Table 2). Accordingly, frequent seizures can lead to the presence of fatigue in children with epilepsy.
2.4. QOL-related factors; perception of stigma by children
Perception of stigma among epilepsy patients is a negative psychological issue associated with reduction of QOL. Stigma has a negative effect on self-esteem and social status and thus can lead to poor prognosis, including isolation and delayed initiation of treatment for epilepsy patients [
18]. Frequent seizures could lead to psychosocial impairments in children. Our previous study using the Child Stigma Scale showed that perceptions of stigma were severe in association with seizure frequency (
Table 2) [
19]. Thus, stigma has negative effects on social identity in children with epilepsy experiencing frequent seizures.
2.5. QOL-related factors; perception of stigma by parents
Epilepsy in children can be a risk factor for stress in their parents [
20,
21,
22,
23]. Parents of children with intractable epilepsy tend to experience severe anxiety in relation to recurrent seizures, and this parental state of anxiety can lead to poor adaptive function in children [
24]. Frequent seizures are thus an important issue with respect to parenting stress [
25]. Parents of children with epilepsy showed higher scores on the Parent Stigma Scale than parents of healthy children [
26]. Moreover, greater perceptions of stigma by parents correlated with higher seizure frequency [
26] (
Table 2). Accordingly, frequent seizures in children with epilepsy can lead to greater perceptions of stigma by parents.
3. Can EEG abnormalities lead to QOL reduction in children with epilepsy?
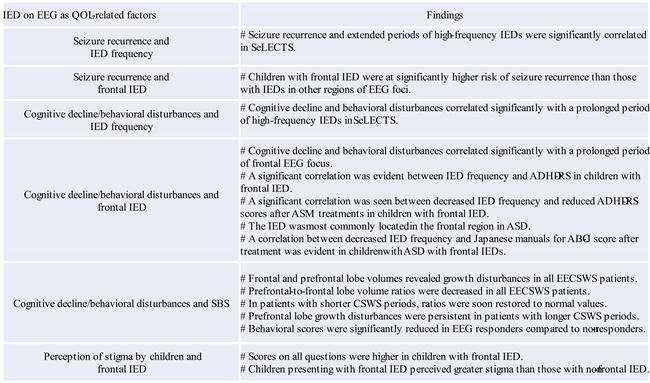
3.1. Association between IEDs on EEG and seizure recurrence
EEG abnormalities such as IEDs can be conceptualized as pathological neuronal discharges [
27]. This can lead to the fact that IEDs on EEG are associated with seizure recurrence. In SeLECTS, recurrent seizures and prolonged periods of frequent IEDs were correlated [
28]. This finding suggests that the occurrence of frequent IEDs and the prolongation of this state may lead to recurrent seizures in SeLECTS. In addition, seizure recurrence may be associated with the location of EEG foci. Our study showed that frontal IED induced recurrent seizures after a first unprovoked seizure more often than other EEG foci [
29] (
Table 3). Thus, frequency of IED and frontal IEDs may be associated with recurrent seizures.
3.2. Association between IEDs on EEG and cognitive/behavioral disturbances
Neuropsychological impairments such as cognitive decline and behavioral disturbances are seen more often in children with more severe EEG abnormalities [
30,
31,
32]. Children can exhibit behavioral disturbances in association with IEDs on EEG without clinical seizures [
33,
34]. Cognitive decline and behavioral disturbances were present in relation to a prolonged period of frequent IEDs in SeLECTS [
35]. Moreover, these disturbances were also associated with a prolongation of the frontal EEG focus [
35] (
Table 3). Cognitive function can deteriorate in children with frequent IEDs. In addition, neuropsychological functioning can recover with the normalization of EEG findings [
36]. Thus, neuropsychological impairments may be associated with IEDs on EEG in SeLECTS (
Table 3). Tassinari et al. reported that neurophysiological impairments associated with the negative myoclonus or inhibitory seizures seen in atypical SeLECTS suggest involvement of the frontal cortex, either primarily or secondarily [
37]. Moreover, frontal and prefrontal lobe growth disturbances persisted even after seizure disappearance in atypical SeLECTS [
7]. These findings suggest that clinical features in atypical SeLECTS may be associated with frontal lobe dysfunctions, which can lead to neuropsychological impairments. In combination with these findings, frontal IED can lead to cognitive declines and behavioral disturbances.
Frontal IED is considered to show various pathogeneses. In children with attention deficit hyperactivity disorder (ADHD) presenting with IED, frequency of IEDs was significantly correlated with ADHD-rating scale (ADHD-RS) score in frontal IED group, but not in Rolandic discharge (RD) group [
38] (
Table 3). In addition, the same study also showed reductions in IED frequency were significantly correlated with ADHD-RS score reductions due to antiseizure medication (ASM) treatment in the frontal IED group, but not in the RD group [
38] (
Table 3). These findings suggest that frontal IED can exacerbate behavioral disturbances in children with ADHD.
IED in children with autism spectrum disorder (ASD) is frequently located in the frontal region [
39]. ASD children with epilepsy with frontal IEDs presented behavioral improvement (reductions in score according to the Japanese manuals for the Aberrant Behavior Checklist (ABC-J)) in association with EEG improvement (reductions in IED frequency) after ASM treatment [
40] (
Table 3). This finding suggests that behavioral disturbances can be associated with frequency of IED on EEG, and ASM treatment can lead to both reduced IED frequency and problems of behavior in ASD children with epilepsy with frontal IEDs [
40]. Thus, frontal IEDs can lead to exacerbation of behavioral disturbances.
In addition, secondary bilateral synchrony (SBS) on EEG may be associated with cognitive decline and behavioral disturbances. The majority of children with epileptic encephalopathy with continuous spikes and waves during slow sleep (EECSWS), as a representative epileptic syndrome of SBS, present neuropsychological impairments. Our previous study showed that the volumes of frontal and prefrontal lobes were small in EECSWS children compared with healthy children [
41] (
Table 3). Moreover, prefrontal lobe growth disturbance was prolonged in children with longer CSWS periods in comparison with those with shorter CSWS periods [
41] (
Table 3). These findings suggest that persistent severe abnormalities on EEG may induce prefrontal lobe growth disturbance, which can lead to neuropsychological impairments.
From a therapeutic perspective, the association between reduction of IED frequency and behavioral improvement after ASM treatment has been evaluated in epilepsy patients presenting with SBS [
42]. Scores for behavioral disturbances measured using the ABC-J were decreased in both EEG responders and EEG non-responders following ASM treatment. Moreover, reductions in ABC-J scores were significantly better in EEG responders than in non-responders. These findings suggest that EEG findings such as SBS can lead to behavioral disturbances, and that behavioral improvements may be achievable in association with EEG improvement [
42] (
Table 3).
3.3. Association between EEG abnormalities and stigma
The emotional state can be influenced by various epileptic activities, including EEG abnormalities. A previous study showed that frontal EEG abnormalities might affect neuropsychological functions [
43]. Our previous study indicated an association between EEG abnormalities and perceived stigma [
44]. Children with frontal IED had higher scores on the Child Stigma Scale than those with IED in other regions. This finding suggests that frontal IED may be associated with a greater perception of stigma. Thus, frontal IED may play a role as an emotional mediator such as stigma [
44] (
Table 3).
4. How do we manage the treatment of epilepsy in children?
4.1. Is urgent suppression of clinical seizures needed?
As mentioned above, the presence of frequent seizures and SE can induce growth disturbance of prefrontal lobe, leading to neuropsychological impairments [
8,
11] (
Figure 1). In addition, recovery from prefrontal lobe growth disturbance may depend on the active seizure period. Disturbance of prefrontal lobe growth can recover more rapidly in children with a shorter active seizure period. However, such recovery may be delayed in children with a longer active seizure period [
8]. These findings support the hypothesized relationship between seizure activities and behavioral disturbances of “seizure activity per se disrupts behavior” as suggested by Austin et al. [
45]. In addition, SE in children can lead to prefrontal lobe growth disruption. In our volumetric study, more frequent SE episodes could lead to poorer outcomes [
11]. Accordingly, SE can lead to neuropsychological impairments in association with prefrontal lobe growth disruptions (
Figure 1). Another study indicated that damage to the frontal regions during childhood can cause deteriorations in neurobehavioral development [
46].
Based on these findings, the therapeutic strategy for childhood epilepsy may require remission of seizures as soon as possible to prevent neuropsychological impairments.
4.2. Is urgent suppression of IED on EEG needed?
As inferred from various studies, frequent IEDs and frontal IED can lead to neuropsychological impairments [
35] (
Figure 1). Reductions in IEDs on EEG may be related to behavioral improvements in children with ADHD/ASD with frontal IED with or without clinical seizures [
38,
40,
47]. Accordingly, frontal IED can lead to neurodevelopmental deterioration in ADHD/ASD, and ASM treatment may affect both IED reduction and behavioral improvement in children with ADHD/ASD with frontal IED.
With respect to EECSWS-related neurodevelopmental deterioration, previous studies have underlined the parallel course of EECSWS and neuropsychological impairments [
48]. Neuropsychological impairments may appear concurrent with the appearance of EEG abnormalities [
49] (
Figure 1). Moreover, these impairments may improve concurrent with the disappearance of EEG abnormalities rather than clinical seizures. In children with SBS, behavioral improvements can be associated with EEG improvement [
42]. These findings suggest that the active phase of “epilepsy”, not only “clinical seizures”, can be a prognostic factor, and the urgent suppression of IEDs such as SBS may thus be warranted to prevent neurodevelopmental deteriorations in children presenting with SBS [
50].
Based on these findings, urgent suppression of EEG abnormalities such as frontal IED and SBS may be required to prevent neuropsychological impairments.
5. Future Perspectives
As observed in these studies, epileptic activities, including seizure severity such as frequent seizures and SE and EEG abnormalities such as frontal IED and SBS, can lead to reduced QOL in children with epilepsy. Better control of seizures and remission of EEG abnormalities may improve QOL in children with epilepsy. However, caution must be taken when generalizing the results to children with epilepsy. Early remission of seizures and EEG abnormalities can lead to improvements in behavioral impairments. However, improvement or reduction of other aspects such as headache, fatigue, and stigma by ASM treatment have not yet been identified. Studies with a larger sample size are needed to evaluate the correlation between remission of seizures/EEG abnormalities and improvement of these aspects in children with epilepsy.
6. Conclusion
Cognitive declines and behavioral disturbances are not always evident in children with epilepsy. However, severe seizures, such as frequent seizures and SE, and some forms of IEDs can lead to neuropsychological impairments. To prevent these impairments, physicians should focus on controlling seizures and suppressing EEG abnormalities as early as possible. Based on the findings from various studies, therapeutic management may be desirable to achieve seizure remission and EEG abnormalities such as frontal IED and SBS as soon as possible to improve QOL in children with epilepsy.
Conflicts of Interest
Dr. Hideaki Kanemura has received speaker’s fees from Eisai Co., Ltd.
References
- Weglage, J.; Demsky, A.; Pietsch, M.; Kurlemann, G. Neuropsychological, intellectual, and behavioral findings in patients with centrotemporal spikes with and without seizures. Dev. Med. Child Neurol. 1997, 39, 646-651. [CrossRef]
- Hamelin, S.; Kahane, P.; Vercueil, L. Fatigue in epilepsy: A prospective inter-ictal and post-ictal survey. Epilepsy Res. 2010, 91, 153-160. [CrossRef]
- Hernandez-Ronquillo, L.; Moien-Afshari, F.; Knox, K.; Britz, J.; TellezZenteno, J.F. How to measure fatigue in epilepsy? The validation of three scales for clinical use. Epilepsy Res. 2011, 95, 119-129. [CrossRef]
- Hoare, P. The development of psychiatric disorder among school children with epilepsy. Dev. Med. Child Neurol. 1984, 26, 3-13.
- Austin, J.K.; Risinger, M.W.; Beckett, L.A. Correlates of behavior problems in children with epilepsy. Epilepsia 1992, 33, 1115-1122. [CrossRef]
- Holmes, G.L.; Ben-Ari, Y. The neurobiology and consequences of epilepsy in the developing brain. Pediatr. Res. 2001, 49, 320-325. [CrossRef]
- Kanemura, H.; Hata, S.; Aoyagi, K.; Sugita, K.; Aihara, M. Serial changes of prefrontal lobe growth in the patients with benign childhood epilepsy with centrotemporal spikes presenting with cognitive impairments/behavioral problems. Brain Dev. 2011, 33, 106-113. [CrossRef]
- Kanemura, H.; Sano, F.; Tando, T.; Sugita, K.; Aihara, M. Repeated seizures induce prefrontal growth disturbance in frontal lobe epilepsy. Brain Dev. 2012, 34, 175-180. [CrossRef]
- Sinclair, D.B.; Wheatley, M.; Snyder, T. Frontal lobe epilepsy in childhood. Pediatr. Neurol. 2004, 30, 169-176. [CrossRef]
- Fejerman, N.; Caraballo, R.H. Early-onset benign childhood occipital epilepsy (Panayiotopoulos type). In: Fejerman, N.; Caraballo, R.H. (Eds.) Benign Focal Epilepsies in Infancy, Childhood and Adolescence. Montrouge, John Libbey Eurotext, 2007, 115-144.
- Kanemura, H.; Sano, F.; Ohyama, T.; Aoyagi, K.; Sugita, K.; Aihara, M. Sequential prefrontal lobe volume changes and cognitive dysfunctions in children with Panayiotopoulos syndrome presenting with status epilepticus. Epilepsy Res. 2015, 112, 122-129. [CrossRef]
- Andermann, F. Clinical features of migraine–epilepsy syndrome. In: Andermann, F.; Lugaresi, E. editors. Migraine and epilepsy. Boston: Butterworths, 1987, 3-30.
- Kanemura, H.; Sano, F.; Ishii, S.; Ohyama, T.; Sugita, K.; Aihara, M. Characteristics of headache in children with epilepsy. Seizure 2013, 22, 647-650. [CrossRef]
- Vercoulen, J.H.; Hommes, O.R.; Swanink, C.M.; Jongen, P.J.; Fennis, J.F.; Galama, J.M.; et al. The measurement of fatigue in patients with multiple sclerosis. A multidimensional comparison with chronic fatigue syndrome and healthy subjects. Arch. Neurol. 1996, 53, 642-649.
- Dittner, A.J.; Wessely, S.C.; Brown, R.G. The assessment of fatigue: A practical guide for clinicians and researchers. J. Psychosom. Res. 2004, 56, 157-170.
- Christensen, D.; Johnsen, S.P.; Watt, T.; Harder, I.; Kirkevold, M.; Andersen, G. Dimensions of post-stroke fatigue: A two-year follow-up study. Cerebrovasc. Dis. 2008, 26, 134-141. [CrossRef]
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Association between seizure frequency and fatigue levels in children with epilepsy. J. Paediatr. Child Health 2018, 54, 1336-1340. [CrossRef]
- Jacoby, A.; Baker, G.; Smith, D.; Dewey, M.; Chadwick, D. Measuring the impact of epilepsy: The development of a novel scale. Epilepsy Res. 1993, 16, 83-88. [CrossRef]
- Kanemura, H.; Sano, F.; Sugita, K.; Aihara, M. Presence of monthly seizures affects perceived stigma in children with epilepsy. J. Pediatr. Epilepsy 2014, 3, 85-92. [CrossRef]
- Rodenburg, R.; Meijer, A.M.; Dekovic, M.; Aldenkamp, A.P. Parents of children with enduring epilepsy: predictions of parenting stress and parenting. Epilepsy Behav. 2007, 11, 197-207.
- Modi, A.C. The impact of a new pediatric epilepsy diagnosis on parents: parenting stress and activity patterns. Epilepsy Behav. 2008, 13, 169-173. [CrossRef]
- Chiou, H.H.; Hsieh, L.P. Parenting stress in patients of children with epilepsy and asthma. J. Child Neurol. 2008, 23, 301-306.
- Cushner-Weinstein, S.; Dassoulas, K.; Salpekar, J.A.; Henderson, S.E.; Pearl, P.L.; Gaillard, W.D.; et al. Parenting stress and childhood epilepsy: the impact of depression, learning, and seizure-related factors. Epilepsy Behav. 2008, 13, 109-114. [CrossRef]
- Kerne, V.; Chapieski, L. Adaptive functioning in pediatric epilepsy: contributions of seizure-related variables and parental anxiety. Epilepsy Behav. 2015, 43, 48-52. [CrossRef]
- Braams, O.; Meekes, J.; Braun, K.; Schappin, R.; van Rijen, P.C.; Hendriks, M.P.H.; et al. Parenting stress does not normalize after child’s epilepsy surgery. Epilepsy Behav. 2015, 42, 147-152.
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Seizure severity in children with epilepsy is associated with their parents’ perception of stigma. Epilepsy Behav. 2016, 63, 42-45. [CrossRef]
- Wolff, M.; Weiskopf, N.; Serra, E.; Preissl, H.; Birbaumer, N.; Kraegeloh-Mann, I. Benign partial epilepsy in childhood: selective cognitive deficits are related to the location of focal spikes determined by combined EEG ⁄ MEG. Epilepsia 2005, 46, 1661-1667. [CrossRef]
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Sequential EEG characteristics may predict seizure recurrence in rolandic epilepsy. Seizure 2014, 23, 646-650. [CrossRef]
- Kanemura, H.; Sano, F.; Ohyama, T.; Mizorogi, S.; Sugita, K.; Aihara, M. EEG characteristics predict subsequent epilepsy in children with their first unprovoked seizure. Epilepsy Res. 2015, 115, 58-62. [CrossRef]
- Massa, R.; de Saint-Martin, A.; Carcangiu, R.; Rudolf, G.; Seegmuller, C.; Kleitz, C.; et al. EEG criteria predictive of complicated evolution in idiopathic Rolandic epilepsy. Neurology 2001, 57, 1071-1079. [CrossRef]
- Verrotti, A.; Latini, G.; Trotta, D.; Giannuzzi, R.; Cutarella, R.; Morgeseet, G.; et al. Typical and atypical rolandic epilepsy in childhood: a follow-up study. Pediatr. Neurol. 2002, 26, 26-29. [CrossRef]
- Vinayan, K.P.; Biji, V.; Thomas, S.V. Educational problems with underlying neuropsychological impairment are common in children with benign epilepsy of childhood with centrotemporal spikes (BECTS). Seizure 2005, 14, 207-212. [CrossRef]
- Ronen, G.M.; Richards, J.E.; Cunningham, C.; Secord, M. Can sodium valproate improve learning in children with epileptiform bursts but without clinical seizures? Dev. Med. Child Neurol. 2000, 42, 751-755.
- Binnie, C.D. Cognitive impairment during epileptiform discharges: is it ever justifiable to treat the EEG? Lancet Neurol. 2003, 2, 725-730.
- Kanemura, H.; Sano, F.; Aoyagi, K.; Sugita, K.; Aihara, M. Do sequential EEG changes predict atypical clinical features in rolandic epilepsy? Dev. Med. Child Neurol. 2012, 54, 912-917.
- Baglietto, M.G.; Battaglia, F.M.; Nobili, L.; Tortorelli, S.; De Negri, E.; Calevoet, M.G.; et al. Neuropsychological disorders related to interictal epileptic discharges during sleep in benign epilepsy of childhood with centrotemporal or Rolandic spikes. Dev. Med. Child Neurol. 2001, 43, 407-412. [CrossRef]
- Tassinari, C.A.; Rubboli, G.; Shibasaki, H. Neurophysiology of positive and negative myoclonus. Electroencephalogr. Clin. Neurophysiol. 1998, 107, 181-195. [CrossRef]
- Kanemura, H.; Sano, F.; Tando, T.; Hosaka, H.; Sugita, K.; Aihara, M. EEG improvements with antiepileptic drug treatment can show a high correlation with behavior recovery in children with ADHD. Epilepsy Behav. 2013, 27, 443-448. [CrossRef]
- Kanemura, H.; Sano, F.; Tando, T.; Sugita, K.; Aihara, M. Can EEG characteristics predict development of epilepsy in autistic children? Eur. J. Paediatr. Neurol. 2013, 17, 232-237.
- Kanemura, H.; Sano, F.; Hoshino, H.; Aihara, M. Efficacy of perampanel in epilepsy patients with autism spectrum disorder. Epilepsy Res. 2021, 170, 106550. [CrossRef]
- Kanemura, H.; Aihara, M. Sequential prefrontal lobe volume changes in epileptic patients with continuous spikes and waves during slow sleep. In: Gadze, Z.P. editor. Epilepsy in Childen - Clinical and Social Aspects. Croatia, INTECH, 2011, 13-24.
- Kanemura, H.; Sano, F.; Hoshino, H.; Takayama, K.; Aihara, M. Effects of perampanel on secondary bilateral synchrony and behavioral problems in adolescents with epilepsy showing insufficient response with levetiracetam. Seizure 2020, 80, 131-137. [CrossRef]
- Coan, J.A.; Allen, J.J.B. The state and trait nature of frontal EEG asymmetry in emotion. In: Hugdahl, K.; Davidson, R.J. editors. The Asymmetry Brain. Cambridge MA, MIT Press, 2003, 565-615.
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Correlation between perceived stigma and EEG paroxysmal abnormality in childhood epilepsy. Epilepsy Behav. 2015, 52, 44-48. [CrossRef]
- Austin, J.K.; Dunn, D.W.; Caffrey, H.M.; Perkins, S.M.; Harezlak, J.; Rose, D.F. Recurrent seizures and behavior problems in children with first recognized seizures: a prospective study. Epilepsia 2002, 43, 1564-1573. [CrossRef]
- Aihara, M.; Aoyagi, K.; Goldberg, E.; Nakazawa, S. Age shifts frontal cortical control in a cognitive bias task from right to left: part I. Neuropsychological study. Brain Dev. 2003, 25, 555-559. [CrossRef]
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Effect of levetiracetam on behavioral problems in pervasive developmental disorder children with epilepsy. Eur. J. Paediatr. Neurol. 2014, 18, 482-488. [CrossRef]
- De Negri, M.; Baglietto, M.G.; Battaglia, F.M.; Gaggero, R.; Pessagno, A.; Recanati, L. Treatment of electrical status epilepticus by short diazepam (DZP) cycles after DZP rectal bolus test. Brain Dev. 1995, 17, 330-333. [CrossRef]
- Morikawa, T.; Seino, M.; Yagi, K. Long-term outcome of four children with continuous spike-waves during sleep, In: Roger, J.; Bureau, M.; Dravet, C.H.; Dreifuss, F.E.; Perret, A.; Wolf, P. editors. Epileptic syndromes in infancy, childhood and adolescence. 2nd ed, London, John Libbey, 1992, 257-266.
- Kanemura, H.; Aihara, M. Neurobiological effects of CSWS on brain growth: A magnetic resonance imaging volumetric study. J. Pediatr. Epilepsy 2012, 1, 187-193. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).