Submitted:
14 December 2023
Posted:
18 December 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Study area
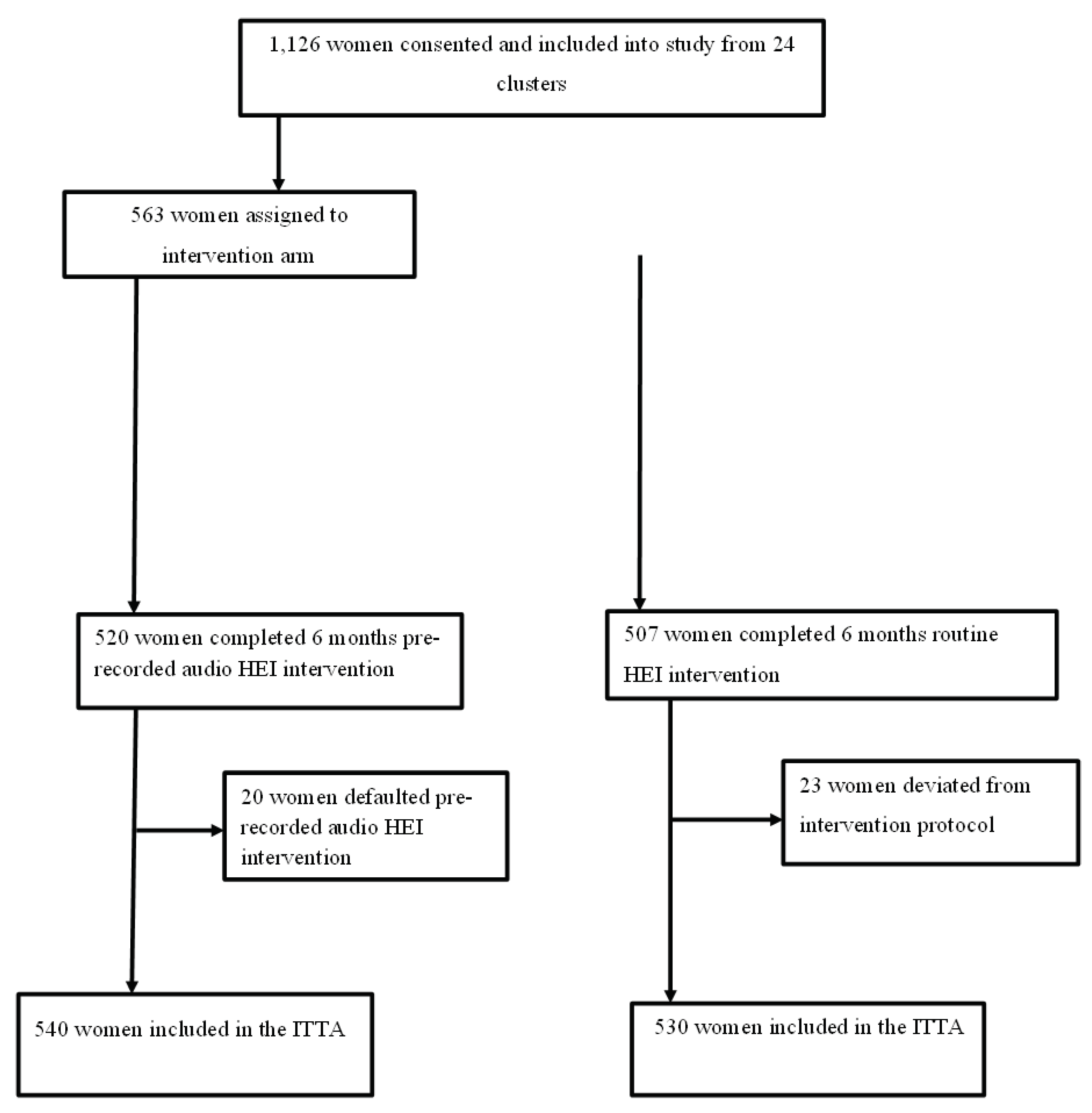
Study design and population
Sample size calculation
Randomization
Study variables
Blinding
HEI procedure
Data collection procedures
Data analysis technique
Ethics statement
Result
Reproductive health characteristics
Description of the proportion of ODS knowledge and BPCR practice
Effect of health education intervention on mothers' knowledge regarding ODS
Effect of health education intervention on BPCR practice
Random effect model of ODS knowledge and BPCR practice
Model selection criteria
Discussion
Conclusions
Supplementary Materials
Author Contributions
Acknowledgment
List of abbreviations
| ANC | Antenatal Care |
| AIC | Akaike's Information Criterion |
| ARRs | Adjusted Risk Ratio |
| BPCR | Birth Preparedness and Complication Readiness |
| BIC | Bayesian Information Criterion |
| CI | Confidence Interval |
| CRR | Crude Risk Ratio |
| EAs | Enumeration areas |
| GTP | Growth and Transformation Plan |
| HCP | Health Care Provider |
| HCG | Human Chorionic Gonadotropin |
| HEI | Health Education Intervention |
| HF | Health Facility |
| HFD | Health facility Delivery |
| HEW | Health Extension Worker |
| ICC | Intra-Cluster Correlation Coefficient |
| ITA | Intention to Treat Analysis |
| IRB | Institutional Review Board |
| MHSU | Maternal Health Service Utilization |
| ODS | Obstetric Danger Sign |
| ODK | Open Data Kit |
| PCA | Principal Component Analysis |
| PI | Principal Investigator |
| PNC | Postnatal Care |
| cRCT | Cluster Randomized Controlled Trial |
| SBA | Skilled Birth Attendant |
| SD | Standard Deviation |
| WDA | Women Development Army |
| WDT | Women Development Team |
| WRA | Women of Reproductive Age |
| WHO | World Health Organization |
| VIF | Variance Inflation Factor |
References
- World Health Organization Maternal health. Available from https://www.who.int/health-topics/maternalhealth#tab=tab_1. Accessed on May 22, 2023.
- World Health Organization Maternal mortality. Available from https://www.who.int/news-room/factsheets/detail/maternal-mortality. Accessed on May 22, 2023.
- World Health Organization (1948) Preamble to the constitution of the world Health organization as adopted by the International health Conference, New York, 19-22 June, 1946, 1948. http://www.who.int/about/definition/en/print.html.
- WHO Maternal health. Available from https://www.who.int/health-topics/maternal-health#tab=tab_1.
- Mengesha E, Taye H. The level of awarenes on danger signs of pregnancy and associated factors among ANC attendant pregnant women in Debark Town, North-West Ethiopia, 2012; 2015.
- JHPIEGO (2001) Maternal and Neonatal health (MNH) Program: Birth preparedness and complication readiness. A matrix of shared responsibilities. Maternal and Neonatal Health. 2001.
- Making pregnancy and childbirth safer (2021) Policy brief, Washington, DC. USA world population reference bureau. 1997. Available: www. measuecommunication.org. Accessed June 2021.
- Stevens RD (2000) Safe motherhood: an insight into maternal mortality in the developing world. Health Millions 26: 34-37.
- Onambele L, Guillen-Aguinaga S, Guillen-Aguinaga L, Ortega-Leon W, Montejo R, et al. (2023) Trends, Projections, and Regional Disparities of Maternal Mortality in Africa (1990–2030): An ARIMA Forecasting Approach. Epidemiologia 4: 322-351.
- Onambele L, Ortega-Leon W, Guillen-Aguinaga S, Forjaz MJ, Yoseph A, et al. (2022) Maternal Mortality in Africa: Regional Trends (2000–2017). International Journal of Environmental Research and Public Health 19: 13146.
- Oyeyemi SO, Wynn R (2015) The use of cell phones and radio communication systems to reduce delays in getting help for pregnant women in low- and middle-income countries: a scoping review. Glob Health Action 8: 28887.
- Thapa B, Manandhar K (2017) Knowledge on obstetric danger signs among antenatal mothers attending a tertiary level hospital, Nepal. Journal of College of Medical Sciences-Nepal 13: 383-387.
- Yunitasari E, Matos F, Zulkarnain H, Kumalasari DI, Kusumaningrum T, et al. (2023) Pregnant woman awareness of obstetric danger signs in developing country: systematic review. BMC Pregnancy and Childbirth 23: 357.
- Geleto A, Chojenta C, Musa A, Loxton D (2019) WOMEN's Knowledge of Obstetric Danger signs in Ethiopia (WOMEN's KODE):a systematic review and meta-analysis. Syst Rev 8: 63.
- Bolanko A, Namo H, Minsamo K (2021) Knowledge of obstetric danger signs and associated factors among pregnant women in Wolaita Sodo town, South Ethiopia: A community-based cross-sectional study. 9: 20503121211001161.
- Central Statistical Agency (CSA) (2016) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF.
- World Health Organization (2006) (WHO, Birth and Emergency Preparedness in Antenatal Care: Integrated Management of Pregnancy and Childbirth (IMPAC). Geneva, Swaziland: WHO Department of Making Pregnancy Safer; 2006. OpenURL.
- Gebre M, Gebremariam A, Abebe TA (2015) Birth preparedness and complication readiness among pregnant women in Duguna Fango District, Wolayta Zone, Ethiopia. PloS one 10: e0137570.
- Kabakyenga JK, Östergren P-O, Turyakira E, Pettersson KO (2011) Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reproductive Health 8: 33.
- Berhe AK, Muche AA, Fekadu GA, Kassa GM (2018) Birth preparedness and complication readiness among pregnant women in Ethiopia: a systematic review and Meta-analysis. Reprod Health 15: 182.
- FMOH (2020) National Reproductive Health Strategy to Improve Maternal and Child Health, FMOH, Addis Ababa, Ethiopia, 2016-2020.
- MoFED. (2010) Growth and Transformation Plan (GTP) 2010/11-2014/15. The Federal Democratic Republic of Ethiopia.
- EFMOH (2010) Ministry of Health Ethiopia, Health sector Development Program (HSDP IV). MoH. Addis Ababa, Ethiopia.
- Communication BC MEASURE Evaluation [Online].Available: http://www.cpc.unc.edu/measure/prh/rh_indicators/crosscutting/bcc.
- Johns Hopkins center for communication program Social and Behavior Change Communication. health communication capacity collaborative.
- UM Ango MO, IS Abubakar, KJ Awosan, Kaoje AU, MO Raji., (2018) Effect of health education intervention on knowledge and utilization of health facility delivery services by pregnant women in Sokoto State, Nigeria. International Journal of Contemporary Medical Research 2018;5(6):F4-F9. 2018.
- Shimpuku Y MF, Horiuchi S, Kubota K, Leshabari SC. (2019) A family-oriented antenatal education program to improve birth preparedness and maternal-infant birth outcomes: A cross sectional evaluation study. Reprod Health. 2019 Jul 16;16(1):107. [CrossRef]
- Izudi J AD, McCoy SI, Bajunirwe F, Kadengye DT. (2019) Effect of health education on birth preparedness and complication readiness on the use of maternal health services: A propensity score-matched analysis. Midwifery. 2019 Nov;78:78-84. [CrossRef]
- OKAFOR OUY, Ademuyiwa Iyabo. (2020) Effect of antenatal education on knowledge and utilization of facility-based delivery services among pregnant women in two health institutions in Alimosho, Lagos state. International Journal of Research in Medical Sciences, [S.l.], v. 8, n. 10, p. 3457-3462, sep. 2020. ISSN 2320-6012.
- Somaya O. Abd Elmoniem EAR, Ahlam E. M. Sarhan, (2020) Effect of Health Educational Program on Knowledge, Attitude, and Reaction of Pregnant Women Regarding Obstetric and Newborn Danger Signs. Evidence-Based Nursing Research Vol 2 No 4. [CrossRef]
- Nabila Salem Mohamed (2019) Effect of an Educational Program on Pregnant Women’s Knowledge aboutObstetric Danger Signs. IOSR Journal of Nursing and Health Science (IOSR-JNHS) e-ISSN: 2320–1959p- ISSN: 2320–1940 Volume 8, Issue 1 Ser IV (Jan - Feb 2019), PP 08-16 wwwiosrjournalsorg.
- Behi R NM (1996) Quasi-experimental research designs. Br J Nurs. 1996 Sep 26-Oct 9;5(17):1079-81. [CrossRef] [PubMed]
- Council ratify Ethiopian’s new ethnic-Sidama statehood (2020) Borkena. com. Borkena Ethiopian News. 19 June 2020. Retrieved February 2022.
- Sidama regional state council (2022) Establishment of new zones structure and budget approval for 2015 EFY agendas report: Regional state council office, Hawassa, Ethiopia. 2022. Unpublished report.
- Sidama regional health bureau (2022) Annual regional health and health-related report: Regional Health office, Hawassa, Ethiopia. Unpulished report.
- Hayes RJ, Moulton LH (2017) Cluster randomised trials: Chapman and Hall/CRC.
- Rutterford C, Copas A, Eldridge S (2015) Methods for sample size determination in cluster randomized trials. International journal of epidemiology 44: 1051-1067.
- Hemming K, Eldridge S, Forbes G, Weijer C, Taljaard M (2017) How to design efficient cluster randomised trials. bmj 358.
- Donner A, Birkett N, Buck C (1981) Randomization by cluster: sample size requirements and analysis. American journal of epidemiology 114: 906-914.
- Killip S, Mahfoud Z, Pearce K (2004) What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. The Annals of Family Medicine 2: 204-208.
- Muluemebet Abera Wordofa ea (2014) Effect of community level intervention on maternal health care utilization: evidence from population basedinterventional-study in south-west ethiopia.
- Pervin J, Nu UT, Rahman AMQ, Rahman M, Uddin B, et al. (2018) Level and determinants of birth preparedness and complication readiness among pregnant women: A cross sectional study in a rural area in Bangladesh. PLoS One 13: e0209076.
- Hailu D, Berhe H (2014) Knowledge about obstetric danger signs and associated factors among mothers in Tsegedie district, Tigray region, Ethiopia 2013: community based cross-sectional study. Plos one 9: e83459.
- Bintabara D, Mohamed MA, Mghamba J, Wasswa P, Mpembeni RN (2015) Birth preparedness and complication readiness among recently delivered women in chamwino district, central Tanzania: a cross sectional study. Reprod Health 12: 44.
- Kabakyenga JK, Östergren PO, Turyakira E, Pettersson KO (2011) Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health 8: 33.
- Save the Children Pregnant Women Conference Best Practice from Ethiopia. Available online from https://www.healthynewbornnetwork.org/hnn-content/uploads/Pregnant-Women-Conference.pdf, Accessed October, 2023.
- Federal Democratic Republic of Ethiopia Ministry of Health (2015) Health Education, Advocacy and Community Mobilisation, Part 1. Blended Learning Module for the Health Extension Programme.
- Minister of Health of Ethiopia (2013.) Prenant women monthly Conference Manual.
- Save the Children International (SCI) Pregnant Women Conference Best Practice from Ethiopia. Available online from https://www.healthynewbornnetwork.org/hnn-content/uploads/Pregnant-Women-Conference.pdf.
- Central Statistical Agency (CSA) [Ethiopia] and ICF (2019) Mini Ethiopia Demographic and Health Survey 2019: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF. 2019.
- Vyas S, Kumaranayake L (2006) Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 21: 459-468.
- Schmidt CO, Kohlmann T (2008) When to use the odds ratio or the relative risk? Int J Public Health 53: 165-167.
- Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3: 21.
- Petersen MR, Deddens JA (2008) A comparison of two methods for estimating prevalence ratios. BMC medical research methodology 8: 1-9.
- Tabachnick BG, Fidell LS, Ullman JB (2007) Using multivariate statistics: Pearson Boston, MA.
- Kleiman E (2017) Understanding and analyzing multilevel data from real-time monitoring studies: An easily-accessible tutorial using R.
- Kleiman E (2017) Understanding and analyzing multilevel data from real-time monitoring studies: An easily- accessible tutorial using R [Internet]. PsyArXiv; 2017. Available from: psyarxiv.com/xf2pw.
- Snijders TAB, and Bosker, Roel J, (1999) Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling, second edition. London etc.: Sage Publishers, 2012.
- Koo TK LM (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 15: 155-163.
- Dziak JJ, Coffman DL, Lanza ST, Li R, Jermiin LS (2020) Sensitivity and specificity of information criteria. Brief Bioinform 21: 553-565.
- Hosmer Jr DW, Lemeshow S, Sturdivant RX (2013) Applied logistic regression: John Wiley & Sons.
- Senaviratna N, Cooray T (2019) Diagnosing multicollinearity of logistic regression model. Asian Journal of Probability and Statistics 5: 1-9.
- Bland JM AD (1995) Multiple significance tests: the Bonferroni method. BMJ. 1995 Jan 21;310(6973):170. [CrossRef]
- Hsu JC (1996) Multiple comparisons: theory and methods. London: Chapman & Hall: CRC Press, 1996.
- Wassihun B, Negese B, Bedada H, Bekele S, Bante A, et al. (2020) Knowledge of obstetric danger signs and associated factors: a study among mothers in Shashamane town, Oromia region, Ethiopia. Reproductive Health 17: 4.
- Hailu M, Gebremariam A, Alemseged F (2010) Knowledge about Obstetric Danger Signs among Pregnant Women in Aleta Wondo District, Sidama Zone, Southern Ethiopia. Ethiop J Health Sci 20: 25-32.
- Omari K. Phanice MOZ (2018) Knowledge of Obstetric Danger Signs among Pregnant Women Attending Antenatal Care Clinic at Health Facilities within Bureti Sub-County of Kericho County, Kenya, Research in Obstetrics and Gynecology, Vol. 6 No. 1, pp. 16-21. [CrossRef]
- Assaf S (2018) Counseling and Knowledge of Danger Signs of Pregnancy Complications in Haiti, Malawi, and Senegal. Matern Child Health J 22: 1659-1667.
- Girma D, Waleligne A (2022) Birth preparedness and complication readiness practice and associated factors among pregnant women in Central Ethiopia, 2021: A cross-sectional study. 17: e0276496.
- Debelie TZ AA, Anteneh KT, Limenih MA, Asaye MM, Lake Aynalem G, (2021) Birth preparedness and complication readiness practice and associated factors among pregnant women in Northwest Ethiopia: 2018. PLoS ONE 16(4): e0249083. [CrossRef]
- UM Ango MO, IS Abubakar,KJ Awosan, Kaoje AU, MO Raji, (2018) Effect of health education intervention on knowledge and utilization of health facility delivery services by pregnant women in Sokoto State, Nigeria. International Journal of Contemporary Medical Research;5(6):F4-F9.
- Gobran M, Fatah, M., Ramadan, M., Amer, G., Rabeh, M., Elshafei, R., Bosilah, A., Khalil, H., Hassanine, S, (2021).Educational Program for Pregnant Women Regarding Obstetrics Dangerous Signs in Rural Areas. Open Journal of Obstetrics and Gynecology, 11, 529-552. [CrossRef]
- Okafor OU, Yewande AI (2020) Effect of antenatal education on knowledge and utilization of facility-based delivery services among pregnant women in two health institutions in Alimosho, Lagos state. International Journal of Research in Medical Sciences 8: 3457-3462.
- Mohamed NS. Effect of an Educational Program on Pregnant Women ’ s Knowledge about Obstetric Danger Signs; 2019.
- Radoff KA, Levi AJ, Thompson LM (2013) A radio-education intervention to improve maternal knowledge of obstetric danger signs. Rev Panam Salud Publica 34: 213-219.
- EMAN M.E. SHAHIN DNS, RANIA A. MOHAMMED, M.Sc., N HOSNI MD, AHMED (2018) Effect of Health Teaching Sessions on Women's Knowledge Regarding Selected Danger Signals During Pregnancy. The Medical Journal of Cairo University 86: 4095-4106.
- Ritchie SJ, Tucker-Drob EM (2018) How Much Does Education Improve Intelligence? A Meta-Analysis. Psychol Sci 29: 1358-1369.
- Altindag D, Cannonier C, Mocan N (2011) The impact of education on health knowledge. Economics of Education Review 30: 792-812.
- Weinschenk AC, Dawes CT (2018) The Effect of Education on Political Knowledge: Evidence From Monozygotic Twins. American Politics Research 47: 530-548.
- Melash Belachew A, Gizachew Worku D (2021) Effect of Community-Based Intervention (Pregnant Women’s Conference) on Institutional Delivery in Ethiopia. In: Amita R, editor. Empowering Midwives and Obstetric Nurses. Rijeka: IntechOpen. pp. Ch. 10.
- Muhumuza Kananura R, Tetui M (2017) Effect of a participatory multisectoral maternal and newborn intervention on birth preparedness and knowledge of maternal and newborn danger signs among women in Eastern Uganda: a quasi-experiment study. 10: 1362826.
- Midhet F, Becker S (2010) Impact of community-based interventions on maternal and neonatal health indicators: Results from a community randomized trial in rural Balochistan, Pakistan. Reproductive Health 7: 30.
- Abera MuluEmebet (2015) effect of community level intervention on maternal health care utilization: evidence from population based interventional-study in South-west Ethiopia. Available on from https://edoc.ub.uni-muenchen.de/20581/7/Abera_Muluemebet.pdf.
- Darmstadt GL, Choi Y, Arifeen SE, Bari S, Rahman SM, et al. (2010) Evaluation of a cluster-randomized controlled trial of a package of community-based maternal and newborn interventions in Mirzapur, Bangladesh. PLoS One 5: e9696.
- Olokoba EO, Umar, A. B, Hayat, M. G, (2015) Effect of health education intervention on knowledge of birth preparedness among pregnant women attending primary health care in Zaria Metropolis.
- Fishbein M A (2000) Theory of reason action; relationship between behavioural intention and behavior evaluation.
- Ajzen I FM (2006) Understanding attitudes and predicting social behavior. Englewood Cliffs prentice Hall, USA.
- Sekyere Stephen Owusu Factors associated with antenatal care service utilization among women with children under five years in Sunyani Municipality, Ghana. Unpublished article.
- Respress ET, Jolly PE, Osia C, Williams ND, Sakhuja S, et al. (2017) A Cross-Sectional Study of Antenatal Care Attendance among Pregnant Women in Western Jamaica. J Pregnancy Child Health 4.
- Midhet F, Becker S (2010) Impact of community-based interventions on maternal and neonatal health indicators: Results from a community randomized trial in rural Balochistan, Pakistan. Reprod Health 7: 30.
- Choulagai BP, Onta S, Subedi N, Bhatta DN, Shrestha B, et al. (2017) A cluster-randomized evaluation of an intervention to increase skilled birth attendant utilization in mid- and far-western Nepal. Health Policy Plan 32: 1092-1101.
- Aboud FE, Akhter S (2011) A cluster-randomized evaluation of a responsive stimulation and feeding intervention in Bangladesh. Pediatrics 127: e1191-e1197.
- Murray DM, Varnell SP, Blitstein JL (2004) Design and analysis of group-randomized trials: a review of recent methodological developments. Am J Public Health 94: 423-432.
- Campbell MK, Piaggio G, Elbourne DR, Altman DG (2012) Consort 2010 statement: extension to cluster randomised trials. Bmj 345: e5661.
- JPTSJ H, Page M, Elbers R, Sterne J (2022) Chapter 8: Assessing risk of bias in a randomized trial. Cochrane handbook for systematic reviews of interventions version 6.
| Variables | Intervention group | Control group | Total | P- value |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Age of mothers | 0.671 | |||
| 15-19 | 0 (0) | 1 (0.2) | 1 (0.1) | |
| 20-24 | 177 (32.8) | 168 (31.7) | 345 (32.2) | |
| 25-29 | 106 (19.6) | 120 (22.6) | 226 (21.1) | |
| 30-34 | 91 (16.9) | 86 (16.2) | 177 (16.5) | |
| 35-39 | 102 (18.9) | 89 (16.8) | 191 (17.9) | |
| 40-44 | 64 (11.9) | 65 (12.3) | 129 (12.1) | |
| 45-50 | 0 (0) | 1 (0.2) | 1 (0.1) | |
| Ethnicity | 0.431 | |||
| Sidama | 485 (89.8) | 470 (88.7) | 955 (89.3) | |
| Amhara | 23 (4.3) | 18 (3.4) | 41 (3.8) | |
| Gurage | 12 (2.2) | 12 (2.3) | 24 (2.2) | |
| Wolayita | 20 (3.7) | 30 (5.7) | 50 (4.7) | |
| Religions | 0.311 | |||
| Protestant | 422 (78.1) | 391 (73.8) | 813 (76.0) | |
| Orthodox | 45 (8.3) | 32 (6.0) | 77 (7.2) | |
| Catholic | 38 (7.0) | 66 (12.5) | 104 (9.7) | |
| Muslim | 35 (6.5) | 41 (7.7) | 76 (7.1) | |
| Mothers' education status | 0.461 | |||
| Cannot read and write | 36 (6.7) | 39 (7.4) | 75 (7.0) | |
| Can read and write only (without formal education) | 8 (1.5) | 13 (2.5) | 21 (2.0) | |
| Have formal education | 496 (91.9) | 478 (90.2) | 974 (91.0) | |
| Marital status | ||||
| Married | 540 (100) | 530 (100) | 1070 (100) | |
| Husband education status | 0.291 | |||
| Cannot read and write | 23 (4.3) | 34 (6.4) | 57 (5.3) | |
| Can read and write only (without formal education) | 6 (1.1) | 6 (1.1) | 12 (1.1) | |
| Have formal education | 511 (94.6) | 490 (92.5) | 1001 (93.6) | |
| Women's occupation status | 0.001 | |||
| Housewife | 386 (71.5) | 409 (77.2) | 795 (74.3) | |
| Farmer | 12 (2.2) | 37 (7.0) | 49 (4.6) | |
| Government employee | 71 (13.1) | 41 (7.7) | 112 (10.5) | |
| Merchant | 71 (13.1) | 43 (8.1) | 114 (10.7) | |
| Husband occupation status | 0.001 | |||
| Government employee | 77 (14.3) | 40 (7.5) | 117 (10.9) | |
| Merchant | 299 (55.4) | 247 (46.6) | 546 (51.0) | |
| Farmer | 164 (30.4) | 243 (45.8) | 407 (38.0) | |
| Family size | 0.115 | |||
| Small (1-5) | 341 (63.1) | 359 (67.7) | 700 (65.4) | |
| Large (greater than 5) | 199 (36.9) | 171 (32.3) | 370 (34.6) | |
| Use of mass media | 0.001 | |||
| No | 234 (43.3) | 299 (56.4) | 533 (49.8) | |
| Yes | 306 (56.7) | 231 (43.6) | 537 (50.2) | |
| Wealth quintile | 0.001 | |||
| Lowest | 131 (24.3) | 82 (15.5) | 213 (19.9) | |
| Second | 77 (14.3) | 138 (26.0) | 215 (20.1) | |
| Middle | 88 (16.3) | 126 (23.8) | 214 (20.0) | |
| Fourth | 113 (20.9) | 101 (19.1) | 214 (20.0) | |
| Highest | 131 (24.3) | 83 (15.7) | 214 (20.0) |
| Variables | Intervention group | Control group | Total | P- value |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Age at first marriage© | 18.62 + 0.97 | 18.53 + 1.21 | 18.57 + 1.09 | 0.179 |
| Age at first pregnancy © | 19.38 + 1.01 | 19.32 + 1.18 | 19.35 + 1.01 | 0.414 |
| Total number of gravidities | 0.540 | |||
| 1 | 141 (26.6) | 128 (23.7) | 269 (25.1) | |
| 2-4 | 259 (48.9) | 277 (51.3) | 536 (50.1) | |
| >5 | 130 (24.5) | 135 (25.0) | 265 (24.8) | |
| Previous history of abortions | ||||
| No | 481 (89.1) | 463 (87.4) | 944 (88.2) | 0.384 |
| Yes | 59 (10.9) | 67 (12.6) | 126 (11.8) | |
| Total number of deliveries | ||||
| 1 | 182 (33.7) | 182 (34.3) | 364 (34.1) | 0.942 |
| 2-4 | 228 (42.2) | 225 (42.5) | 453 (42.3) | |
| >5 | 130 (24.1) | 123 (23.2) | 253 (23.6) | |
| Infection during the current pregnancy | 0.252 | |||
| No | 473 (87.6) | 476 (89.8) | 949 (88.7) | |
| Yes | 67 (12.4) | 54 (10.2) | 121 (11.3) | |
| Previous history of stillbirth | 0.322 | |||
| No | 501 (92.8) | 483 (91.1) | 984 (92.0) | |
| Yes | 39 (7.2) | 47 (8.9) | 86 (8.0) | |
| Previous history of neonatal death | 0.041 | |||
| No | 527 (97.6) | 505 (95.3) | 1032 (96.4) | |
| Yes | 13 (2.4) | 25 (4.7) | 38 (3.6) | |
| Last pregnancy planned | 0.001 | |||
| No | 100 (18.5) | 185 (34.9) | 285 (26.6) | |
| Yes | 440 (81.5) | 345 (65.1) | 785 (73.4) | |
| Encountered ODS during last pregnancy | 0.012 | |||
| No | 501 (92.8) | 468 (88.3) | 969 (90.6) | |
| Yes | 39 (7.2) | 62 (11.7) | 101 (9.4) | |
| Faced ODS during last childbirth | 0.926 | |||
| No | 495 (91.7) | 485 (91.5) | 980 (91.6) | |
| Yes | 45 (8.3) | 45 (8.5) | 90 (8.4) | |
| Confronted ODS during last postpartum period | 0.444 | |||
| No | 500 (92.6) | 497 (93.8) | 997 (93.2) | |
| Yes | 40 (7.4) | 33 (6.2) | 73 (6.8) |
| Variables | Knowledge of obstetric danger sign | CRR (99% CI) | ARR (99% CI) | |
|---|---|---|---|---|
| Good | Poor | |||
| Individual level determinants | ||||
| Study group | ||||
| Control | 192 (36.2) | 338 (63.8) | Ref | Ref |
| Intervention | 371 (68.7) | 169 (31.3) | 1.92 (1.37, 2.69) | 1.71 (1.14, 2.57)* |
| Women's occupation | ||||
| Housewife | 378 (47.5) | 417 (52.5) | Ref | Ref |
| Farmer | 17 (34.7) | 32 (65.3) | 0.82 (0.60, 1.12) | 0.82 (0.54, 1.25) |
| Government employee | 86 (76.8) | 26 (23.2) | 1.58 (1.41, 1.76) | 1.02 (0.86, 1.20) |
| Merchant | 82 (71.9) | 32 (28.1) | 1.45 (1.33, 1.58) | 1.19 (1.07, 1.32) |
| Husband occupation | ||||
| Government employee | 93 (79.5) | 24 (20.5) | Ref | Ref |
| Merchant | 300 (54.9) | 246 (45.1) | 0.70 (0.61, 0.79) | 0.82 (0.69, 0.98) |
| Farmer | 170 (41.8) | 237 (58.2) | 0.56 (0.47, 0.67) | 0.84 (0.65, 1.09) |
| Use of mass media | ||||
| No | 212 (39.8) | 321 (60.2) | Ref | Ref |
| Yes | 351 (65.4) | 186 (34.6) | 1.56 (1.30, 1.87) | 1.22 (0.95, 1.57) |
| Wealth quintile | ||||
| Lowest | 148 (69.5) | 65 (30.5) | Ref | Ref |
| Second | 95 (44.2) | 120 (55.8) | 0.75 (0.62, 0.91) | 0.92 (0.75, 1.13) |
| Middle | 78 (36.4) | 136 (63.6) | 0.60 (0.45, 0.79) | 0.79 (0.60, 1.04) |
| Fourth | 102 (47.7) | 112 (52.3) | 0.77 (0.65, 0.90) | 0.95 (0.78, 1.16) |
| Highest | 140 (65.4) | 74 (34.6) | 1.03 (0.88, 1.20) | 0.99 (0.82, 1.19) |
| Previous history of neonatal death | ||||
| No | 551 (53.4) | 481 (46.6) | Ref | |
| Yes | 12 (31.6) | 26 (68.4) | 0.82 (0.51, 1.30) | 0.85 (0.46, 1.58) |
| Last pregnancy planned | ||||
| No | 111 (38.9) | 174 (61.1) | Ref | Ref |
| Yes | 452 (57.6) | 333 (42.4) | 1.29 (1.07, 1.56) | 1.20 (0.98, 1.47) |
| Faced health problems during the pregnancy | ||||
| No | 506 (52.2) | 463 (47.8) | Ref | Ref |
| Yes | 57 (56.4) | 44 (43.6) | 1.24 (1.05, 1.47) | 1.13 (0.93, 1.37) |
| Road access | ||||
| Inaccessible | 358 (47.2) | 400 (52.8) | Ref | Ref |
| Accessible | 205 (65.7) | 107 (34.3) | 1.41 (1.21, 1.64) | 1.03 (0.85, 1.26) |
| Received model family training | ||||
| No | 316 (47.2) | 354 (52.8) | Ref | Ref |
| Yes | 247 (61.8) | 153 (38.3) | 1.33 (1.23, 1.45) | 1.18 (1.05, 1.34)* |
| Availability of transport | ||||
| No | 220 (40.4) | 324 (59.6) | Ref | Ref |
| Yes | 343 (65.2) | 183 (34.8) | 1.57 (1.43, 1.72) | 1.31 (1.16, 1.49)* |
| Community-level determinants | ||||
| Place of residence | ||||
| Rural | 398 (49.8) | 402 (50.2) | Ref | Ref |
| Urban | 165 (61.1) | 105 (38.9) | 1.21 (0.82, 1.76) | 0.91 (0.70, 1.18) |
| Cluster-level mass media use | ||||
| Low | 325 (49.0) | 338 (51.0) | Ref | Ref |
| High | 238 (58.5) | 169 (41.5) | 1.19 (0.80, 1.76) | 0.89 (0.68, 1.16) |
| Cluster-level distance | ||||
| Big problem | 160 (54.6) | 133 (45.4) | Ref | Ref |
| Not big problem | 403 (51.9) | 374 (48.1) | 0.90 (0.62, 1.29) | 1.03 (0.77, 1.38) |
| Cluster-level poverty | ||||
| Low | 417 (50.4) | 411 (49.6) | Ref | Ref |
| High | 146 (60.3) | 96 (39.7) | 1.18 (0.79, 1.77) | 1.25 (0.90, 1.74) |
| Variables | Birth preparedness and complication readiness | CRR (99% CI) | ARR (99% CI) | ||||
|---|---|---|---|---|---|---|---|
| Poor | Well | ||||||
| Individual level determinants | |||||||
| Study group | |||||||
| Control | 206 (38.9) | 324 (61.1) | Ref | Ref | |||
| Intervention | 347 (64.3) | 193 (35.7) | 1.70 (1.18, 2.44) | 1.55 (1.01, 2.39)* | |||
| Women's occupation | |||||||
| Housewife | 421 (53.0) | 374 (47.0) | Ref | Ref | |||
| Farmer | 35 (71.4) | 14 (28.6) | 0.67 (0.47, 0.95) | 0.67 (0.49, 0.94) | |||
| Government employee | 22 (19.6) | 90 (80.4) | 1.68 (1.52, 1.85) | 1.13 (0.98, 1.30) | |||
| Merchant | 39 (34.2) | 75 (65.8) | 1.35 (1.18, 1.54) | 1.08 (0.96, 1.22) | |||
| Husband occupation | |||||||
| Government employee | 95 (81.2) | 22 (18.8) | Ref | Ref | |||
| Merchant | 294 (53.8) | 252 (46.2) | 0.67 (0.59, 0.75) | 0.90 (0.78, 1.03) | |||
| Farmer | 164 (40.3) | 243 (59.7) | 0.52 (0.45, 0.61) | 0.89 (0.74, 1.06) | |||
| Use of mass media | |||||||
| No | 202 (37.9) | 331 (62.1) | Ref | Ref | |||
| Yes | 351 (65.4) | 186 (34.6) | 1.65 (1.37, 2.00) | 1.26 (1.06, 1.51)* | |||
| Wealth quintile | |||||||
| Lowest | 143 (67.1) | 70 (32.9) | Ref | Ref | |||
| Second | 94 (43.7) | 121 (56.3) | 0.71 (0.58, 0.86) | 0.87 (0.69, 1.10) | |||
| Middle | 75 (35.0) | 139 (65.0) | 0.58 (0.42, 0.79) | 0.77 (0.57, 1.03) | |||
| Fourth | 98 (45.8) | 116 (54.2) | 0.74 (0.62, 0.88) | 0.92 (0.76, 1.13) | |||
| Highest | 143 (66.8) | 71 (33.2) | 1.07 (0.90, 1.28) | 1.04 (0.87, 1.24) | |||
| Previous history of neonatal death | |||||||
| No | 540 (52.3) | 492 (47.7) | Ref | Ref | |||
| Yes | 13 (34.2) | 25 (65.8) | 0.88 (0.60, 1.28) | 0.96 (0.65, 1.42) | |||
| Last pregnancy planned | |||||||
| No | 110 (38.6) | 175 (61.4) | Ref | Ref | |||
| Yes | 443 (56.4) | 342 (43.6) | 1.31 (1.09, 1.57) | 1.24 (1.06, 1.44)* | |||
| Faced health problems during the pregnancy | |||||||
| No | 487 (50.3) | 482 (49.7) | Ref | Ref | |||
| Yes | 66 (65.3) | 35 (34.7) | 1.50 (1.27, 1.77) | 1.37 (1.17, 1.62)* | |||
| Road access | |||||||
| Inaccessible | 366 (48.3) | 392 (51.7) | Ref | Ref | |||
| Accessible | 187 (59.9) | 125 (40.1) | 1.29 (1.08, 1.54) | 0.93 (0.77, 1.11) | |||
| Received model family training | |||||||
| No | 319 (47.6) | 351 (52.4) | Ref | Ref | |||
| Yes | 234 (58.5) | 166 (41.5) | 1.30 (1.18, 1.42) | 1.15 (1.04, 1.27)* | |||
| Availability of transport | |||||||
| No | 227 (41.7) | 317 (58.3) | Ref | Ref | |||
| Yes | 326 (62.0) | 200 (38.0) | 1.48 (1.31, 1.68) | 1.24 (1.09, 1.43)* | |||
| Community-level determinants | |||||||
| Place of residence | |||||||
| Rural | 388 (48.8) | 412 (51.5) | Ref | ||||
| Urban | 165 (61.1) | 105 (38.9) | 1.27 (0.91, 1.76) | 0.91 (0.71, 1.15) | |||
| Cluster-level mass media use | |||||||
| Low | 318 (48.0) | 345 (52.0) | Ref | Ref | |||
| High | 235 (57.7) | 172 (42.3) | 1.22 (0.85, 1.76) | 0.88 (0.72, 1.09) | |||
| Cluster-level distance to nearest health facility | |||||||
| Big problem | 154 (52.6) | 139 (47.4) | Ref | Ref | |||
| Not big problem | 399 (51.4) | 378 (48.6) | 0.93 (0.66, 1.32) | 1.05 (0.83, 1.33) | |||
| Cluster-level poverty | |||||||
| Low | 399 (48.2) | 429 (51.8) | Ref | Ref | |||
| High | 154 (63.6) | 88 (36.4) | 1.34 (0.98, 1.84) | 1.49 (1.04, 2.12) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





