Submitted:
21 December 2023
Posted:
26 December 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Material And Methods
Results
| Variable | Delta | HR | 95% CI | P of coefficient |
|---|---|---|---|---|
| Age | 5 | 2.34 | 1.98 2.77 | <0.0001 |
| Family heart attack | 1 | 1.17 | 0.89 1.54 | 0.2663 |
| Cigarettes | 9 | 1.21 | 1.06 1.38 | 0.0052 |
| Body mass index | 4 | 0.95 | 0.70 1.30 | 0.7612 |
| Subscapular skinfold | 6 | 0.95 | 0.75 1.22 | 0.7014 |
| Arm circumference | 24 | 0.91 | 0.74 1.11 | 0.3426 |
| Systolic blood pressure | 20 | 1.36 | 1.16 1.58 | <0.0001 |
| Heart rate | 13 | 0.81 | 0.69 0.96 | 0.0145 |
| Vital capacity | 0.24 | 0.92 | 0.78 1.09 | 0.3329 |
| Serum cholesterol | 40 | 1.07 | 0.93 1.23 | 0.3467 |
| Urine glucose | 1 | 1.72 | 0.89 3.32 | 0.1037 |
| CVD prevalence | 1 | 1.74 | 0.91 3.33 | 0.0950 |
Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Menotti A, Puddu PE. Lifetime prediction of coronary heart disease and heart disease of uncertain etiology in a 50-year follow-up population study. Int J Cardiol 2015; 196: 55-60. [CrossRef]
- Puddu PE, Menotti A. Natural history of coronary heart disease and heart disease of uncertain etiology: findings from a 50-year population study. Int J Cardiol 2015; 197: 260-264. [CrossRef]
- Menotti A, Puddu PE, Maiani G, Catasta G. Lifestyle behaviour and lifetime incidence of heart diseases. Int J Cardiol 2015; 201: 293-299. [CrossRef]
- Menotti A, Blackburn H, Seccareccia F, Kromhout D, Nissinen A, Karvonen M, et al. Relationship of some risk factors with typical and atypical manifestations of coronary heart disease. Cardiology 1998; 89: 59-67. [CrossRef]
- Menotti A, Lanti M, Nedeljkovic S, Nissinen A, Kafatos A, Kromhout D. The relationship of age, blood pressure, serum cholesterol and smoking habits with the risk of typical and atypical coronary heart disease death in the European cohorts of the Seven Countries Study. Int J Cardiol 2005; 106: 157-163. [CrossRef]
- Menotti A, Puddu PE, Lanti M, Kromhout D, Tolonen H, Parapid B, et al. Epidemiology of typical coronary heart disease versus heart disease of uncertain etiology (atypical) fatalities and their relationships with classic coronary risk factors. Int J Cardiol 2013; 168: 3963-3967. [CrossRef]
- Menotti A, Puddu PE. How the Seven Countries Study contributed to the launch and development of cardiovascular epidemiology in Italy. A historical perspective. Nutr Metab Cardiovasc Dis 2020; 30: 368-383. [CrossRef]
- WHO: International classification of diseases. Eight revision. Geneva, World Health Org, 1965.
- Kromhout D, Menotti A, Blackburn H. Prevention of coronary heart disease. Diet, lifestyle and risk factors in the Seven Countries Study. Kluwer Publ. Norwell Ma, USA and Dordrecht, NL, 2002: 1-267.
- Rose G, Blackburn H. Cardiovascular survey methods. Geneva, World Health Organization, 1968.
- Hemsfield SB, MacManus C, Smith J, Stevens V, Nixon DW. Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr 1982; 36:680-690. [CrossRef]
- Anderson JT, Keys A. Cholesterol in serum and lipoprotein fractions: its measurement and stability. Clin Chem 1956; 2:145-159. [CrossRef]
- Keys A, (ed) Blackburn H, Menotti A, Buzina R, Mohacek I, Karvonen MJ, et al. Coronary heart disease in seven countries. Circulation 1970, 41, suppl 1: 1-211. [CrossRef]
- Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “p <0.05”. Am Statistician 2019; 73: 1-19. [CrossRef]
- Menotti A, Puddu PE, Kafatos AG, Tolonen H, Adachi H, Jacobs DR Jr. Cardiovascular mortality in 10 cohorts of middle-aged men followed-up 60 years until extinction: The Seven Countries Study. J Cardiovasc Dev Dis 2023; 10: 201. [CrossRef]
- Menotti A, Lanti M, Maiani G, Kromhout D. Forty-year mortality from cardiovascular diseases and their risk factors in men of the Italian rural areas of the Seven Countries Study. Acta Cardiol 2005; 60: 521-531. [CrossRef]
- Puddu PE, Piras P, Menotti A. Competing risks and lifetime coronary heart disease incidence during 50 years of follow-up. Int J Cardiol 2016; 219: 79-83. [CrossRef]
- Puddu PE, Piras P, Menotti A. Lifetime competing risks between coronary heart disease mortality and other causes of death during 50 years of follow-up Int J Cardiol 2017; 228: 359-363. [CrossRef]
- Menotti A, Puddu PE. Risk factors measured in middle-aged men predicting coronary events in geriatric age. Int J Cardiol 2016; 222: 1116-1121. [CrossRef]
- Llyod-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PWF et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006; 113: 791-798. [CrossRef]
- Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet 1999; 353:89-92. [CrossRef]
- Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation 2002; 106: 3068-3672. [CrossRef]
- Seshadri S, Wolf PA. Lifetime risk of stroke and dementia: current concepts, and estimates from the Framingham Study. Lancet Neurol 2007; 12: 1106-1114. [CrossRef]
- Lloyd-Jones DM, Wilson PWF, Larson MG, Beise A, Leip EP, D’Agostino RB et al. Framingham risk score and prediction of lifetime risk for coronary heart disease. Am J Cardiol 2004; 94: 20-24. [CrossRef]
- Lloyd-Jones, DM. Short-term versus long-term risk for coronary artery disease: implications for lipid guidelines. Curr Opin Lipidol 2006; 6: 619-625. [CrossRef]
- Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA 2012; 308:1795-1801. [CrossRef]
- Stenling A, Haggstrom C, Norberg M, Norstrom F. Lifetime risk predictions for cardiovascular diseases: competing risks analyses on a population-based cohort in Sweden. Atherosclerosis 2020; 312: 90-98. [CrossRef]
- Wang Y, Liu J, Wang W, Wang M, Qi Y, Xie W et al. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese Multi-Provincial Cohort Study, Eur J Prev Cardiol 2015; 22: 380-388. [CrossRef]
- Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-1913. [CrossRef]
- Prospective Studies Collaboration. Blood cholesterol and vascular mortality by age, sex and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55000 vascular deaths. Lancet 2007; 370: 1829-1839. [CrossRef]
- Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373:1083-1096. [CrossRef]
- Abraham G, Havulinna AS, Bhalala OG, Byars, De Livera AM, Yetukuri L et al. Genomic prediction of coronary heart disease. Eur Heart J 2016; 37: 3267-3278. [CrossRef]
- Puddu PE, Piras P, Kafatos A, Adachi H, Tolonen H, Menotti A. Competing risks of coronary heart disease mortality versus other causes of death in 10 cohorts of middle-aged men of the Seven Countries Study followed for 60 years to extinction. J Cardiovasc Dev Dis 2023; 10: 482. [CrossRef]
- Puddu PE, Menotti A. Heart diseases of uncertain etiology: a new definition of heart failure for epidemiological studies. J Cardiovasc Dev Dis 2023; 10: 132. [CrossRef]
- Jacobs DR Jr, Woo JG, Sinaiko AR, Daniels SR, Ikonen J, Juonala M, et al. Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med 2022; 386: 1877-1888. [CrossRef]

| Causes of death | N | Rate per 1000 |
Proportion % within selected groups of CVD |
|---|---|---|---|
| All causes | 1708 | 998 | ---- |
| All cardiovascular diseases CVD | 785 | 459 | ---- |
| Selected sub groups of CVD | |||
| Coronary heart disease | 281 | 164 | 38.7 |
| Stroke | 230 | 134 | 31.6 |
| Heart disease of uncertain etiology | 216 | 126 | 29.7 |
| Pool of selected groups of CVD | 727 | 425 | 100.0 |
| Risk Factor | Overall (N=1712) | CHD | Stroke | HDUE | P of ANOVA |
|---|---|---|---|---|---|
| Age, years | 49.1 (5.1) | 49.0 (5.1) | 49.7 (5.0) | 49.5 (5.2) | 0.4144 |
| Family heart attack (0-1), % (*) | 40.3 (1.8) | 40.9 (2.9) | 40.4 (3.2) | 39.4 (3.3) | 0.9380 (**) |
| Cigarettes, N/day | 8.7 (0.5) | 8.9 (9.4) | 7.4 (8.8) | 8.0 (8.9) | 0.1627 |
| Body mass index, kg/m2 | 25.2 (3.7) | 25.8 (3.7) | 25.3 (3.7) | 25.0 (3.7) | 0.0579 |
| Subscapular skinfold, mm | 11.8 (5.8) | 12.7 (6.2) | 12.1 (6.3) | 11.4 (5.7) | 0.0664 |
| Arm circumference, mm | 268.6 (23.6) | 270.0 (23.1) | 269.6 (23.6) | 268.7 (22.8) | 0.8503 |
| Systolic blood pressure, mmHg | 143.6 (21.0) | 146.4 (21.8) | 145.0 (21.9) | 142.7 (20.5) | 0.1638 |
| Heart rate, beats/min | 71.3 (12.9) | 71.7 (12.7) | 71.6 (12.4) | 68.4 (13.7) | 0.0075 |
| Vital capacity, L/m2 | 1.65 (0.24) | 1.63 (0.25) | 1.63 (0.23) | 1.67 (0.24) | 0.1736 |
| Serum cholesterol, mg/dl | 201.6 (40.8) | 209.6 (42.2) | 204.4 (38.8) | 198.0 (39.3) | 0.0066 |
| Urine glucose (0-1), % (*) | 5.1 (0.8) | 4.6 (1.3) | 6.1 (1.6) | 4.6 (1.4) | 0.7071 (**) |
| CVD prevalence (0-1), % (*) | 4.7 (0.8) | 4.6 (1.3) | 4.8 (1.4) | 4.6 (1.4) | 0.9958 (**) |
| Variable | Delta | HR | 95% CI | P of coefficient |
|---|---|---|---|---|
| Age | 5 | 1.41 | 1.23 1.61 | <0.0001 |
| Family heart attack | 1 | 1.18 | 0.87 1.50 | 0.1814 |
| Cigarettes | 9 | 1.18 | 1.06 1.32 | 0.0034 |
| Body mass index | 4 | 1.16 | 0.91 1.48 | 0.2232 |
| Subscapular skinfold | 6 | 0.95 | 0.78 1.15 | 0.6067 |
| Arm circumference | 24 | 0.87 | 0.74 1.03 | 0.1135 |
| Systolic blood pressure | 20 | 1.36 | 1.20 1.54 | <0.0001 |
| Heart rate | 13 | 0.99 | 0.99 1.13 | 0.9396 |
| Vital capacity | 0.24 | 0.84 | 0.73 0.96 | 0.0094 |
| Serum cholesterol | 40 | 1.27 | 1.13 1.42 | <0.0001 |
| Urine glucose | 1 | 1.06 | 0.60 1.90 | 0.8335 |
| CVD prevalence | 1 | 1.50 | 0.85 2.64 | 0.1619 |
| Variable | Delta | HR | 95% CI | P of coefficient |
|---|---|---|---|---|
| Age | 5 | 1.71 | 1.50 2.03 | <0.0001 |
| Family heart attack | 1 | 1.14 | 0.87 1.49 | 0.3323 |
| Cigarettes | 9 | 1.03 | 0.90 1.18 | 0.6414 |
| Body mass index | 4 | 0.95 | 0.72 1.26 | 0.7200 |
| Subscapular skinfold | 6 | 0.97 | 0.78 1.22 | 0.8092 |
| Arm circumference | 24 | 0.95 | 0.80 1.16 | 0.6730 |
| Systolic blood pressure | 20 | 1.28 | 1.10 1.48 | 0.0009 |
| Heart rate | 13 | 1.05 | 0.91 1.22 | 0.4740 |
| Vital capacity | 0.24 | 0.85 | 0.73 0.98 | 0.0306 |
| Serum cholesterol | 40 | 1.17 | 1.02 1.34 | 0.0203 |
| Urine glucose | 1 | 1.82 | 1.04 3.19 | 0.0370 |
| CVD prevalence | 1 | 1.51 | 0.81 2.81 | 0.1912 |
| End-point | Q 1 | Q2 | Q3 | Q4 | Q5 | Ratio Q5/Q1 | P of chisquared |
|---|---|---|---|---|---|---|---|
| Coronary heart disease | 16.0 | 16.3 | 21.0 | 24.2 | 22.4 | 1.4 | 0.4298 |
| Stroke | 16.5 | 18.7 | 22.6 | 21.3 | 20.9 | 1.3 | 0.8498 |
| Heart disease of uncertain etiology | 19.0 | 17.1 | 18.0 | 21.8 | 24.1 | 1.3 | 0.8576 |
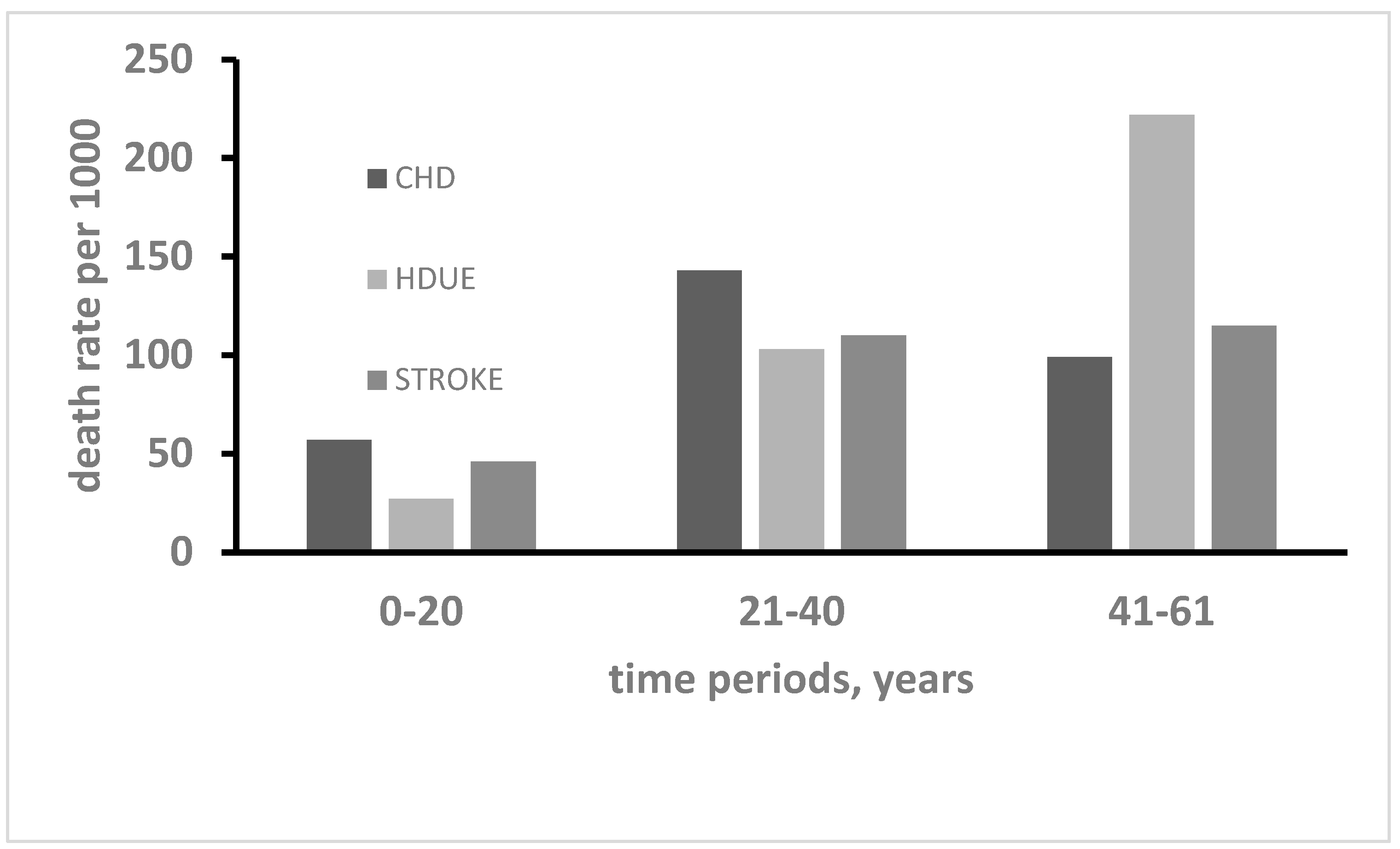
| Variable | Time period 1 Year 0 to 20 |
Time period 2 Year 21 to 40 |
Time period 3 Year 41 to 61 |
P of ANOVA | |||
|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | ||
| Age | 51.6 | 4.9 | 49.3 | 4.7 | 44.6 | 3.2 | <0.0001 |
| Cigarettes | 9.2 | 9.5 | 8.8 | 9.3 | 4.9 | 7.4 | <0.0001 |
| Systolic blood pressure | 155.9 | 25.6 | 141.8 | 17.4 | 134.1 | 15.5 | <0.0001 |
| Heart rate | 74.3 | 14.8 | 69.7 | 12.0 | 67.7 | 10.7 | <0.0001 |
| Vital capacity | 1.55 | 0.25 | 1.66 | 0.23 | 1.75 | 0.22 | <0.0001 |
| Serum cholesterol | 210.6 | 40.6 | 205.6 | 40.3 | 190.7 | 38.2 | <0.0001 |
| Urine glucose* | 7.3 | 2.1 | 4.5 | 1.2 | 1.7 | 1.2 | 0.0626 ** |
| CHD (as primary) versus OTHER CAUSES |
OTHER CAUSES (as primary) versus CHD |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk factor | coefficient | P value | HR | 95% CI | coefficient | P value | HR | 95% CI | t-test | |||
| Age | -0.0150 | 0.2390 | 0.93 | 0.82 | 1.05 | 0.0461 | <0.0001 | 1.26 | 1.19 | 1.34 | -4.31** | |
| Family heart attack | 0.1244 | 0.3102 | 1.13 | 0.89 | 1.44 | -0.0069 | 0.9044 | 0.99 | 0.89 | 1.11 | 0.97 | |
| Cigarettes | 0.0035 | 0.5592 | 1.03 | 0.93 | 1.15 | 0.0066 | 0.0258 | 1.06 | 1.01 | 1.12 | -0.46 | |
| BMI $ | 0.0210 | 0.5170 | 1.09 | 0.84 | 1.40 | 0.0052 | 0.7414 | 1.02 | 0.90 | 1.16 | 0.44 | |
| Subscapular skinfold | 0.0053 | 0.7582 | 1.03 | 0.84 | 1.26 | -0.0138 | 0.1012 | 0.92 | 0.83 | 1.02 | 1.00 | |
| Arm circumference | -0.0011 | 0.7486 | 0.97 | 0.83 | 1.15 | -0.0024 | 0.1488 | 0.94 | 0.87 | 1.02 | 0.34 | |
| Systolic blood pressure | 0.0063 | 0.0490 | 1.13 | 1.00 | 1.29 | 0.0014 | 0.4296 | 1.03 | 0.96 | 1.11 | 1.32 | |
| Heart rate | -0.0038 | 0.4354 | 0.95 | 0.84 | 1.08 | 0.0037 | 0.1444 | 1.05 | 0.98 | 1.12 | -137 | |
| Vital capacity | -0.2883 | 0.2984 | 0.93 | 0.82 | 1.06 | -0.1117 | 0.4124 | 0.97 | 0.91 | 1.02 | -0.57 | |
| Serum cholesterol | 0.0042 | 0.0042 | 1.18 | 1.05 | 1.33 | -0.0009 | 0.1972 | 0.96 | 0.91 | 1.02 | 3.13* | |
| Urine glucose | -0.0736 | 0.8104 | 0.93 | 0.51 | 1.70 | 0.1772 | 0.2342 | 1.19 | 0.89 | 1.60 | -0.74 | |
| CVD prevalnce | 0.0464 | 0.8776 | 1.05 | 0.58 | 1.89 | -0.0040 | 0.9840 | 1.00 | 0.70 | 1.41 | 0.15 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





