1. Introduction
Antimicrobials are compounds that are commonly utilised to prevent and treat diseases in humans, livestocks, aquaculture and crop productivity. Their efficacy is now jeopardised because a number of antimicrobial therapies that once worked are no longer effective due to microorganism resistance. microorganisms that are resist to widely used antimicrobials are called Superbugs [
1].The World Health Organisation (WHO) has identified antimicrobial resistance as one of the top ten global public health problems facing humanity. One of the greatest challenges to global health, food security, and development today, according to the World Health Organisation (WHO), is the emergence of antibiotic resistance. Even though antibiotic resistance can arise naturally, improper usage of these medications is accelerating its global spread [
2].
Global health is significantly impacted by antimicrobial resistance (AMR). Antibiotic misuse and overuse have resulted in the emergence of drug-resistant bacteria, viruses, and fungi, which makes ordinary infections more difficult to cure and accelerates the spread of disease. The World Health Organisation has declared that AMR could result in up to 10 million deaths yearly by 2050, making it a worldwide health emergency. Antimicrobial resistance is frequently referred to as the "Silent Pandemic" and is a problem that requires current action and should be managed more effectively rather than considered as a future situation[
3].
Finding a solution that adequately addresses AMR while also preventing further AMR emergence is difficult because AMR is a complex issue involving dynamic nature of microorganisms, healthcare, social anthropology, economics, societal behaviour, health literacy, geoclimatic events, global travel, and pharmaceutical innovation and investment.at both the population and individual levels[
4].
This review will provide background information on the causes and processes of antimicrobial resistance (AMR) in brief. It will also offer insights into new and emerging solutions that are being studied and may be created in the future to address the advancement of AMR.
2. Antimicrobial Resistance Challenges and One Health Approach
Antimicrobial Resistance is a new challenge that requires a coordinated worldwide response. "One Health" accepts the idea that there is a definite link between human and animal health and the common environment, as demonstrated [
4,
5]. As the most comprehensive and worldwide responds to the issue of antibiotic resistance, the One Health concept appears to go hand in hand. Communication across the One Health triad (people, animals, and environment) about agricultural AMR is hampered by unclear language, which is further exacerbated by cultural and linguistic differences, which can lead to the belief that the other party is unaware of the facts or has ulterior objectives[
6].
Looking at any issue through the lens of One Health demands considering the interactions of people, domestic animals, wildlife, plants, and our environment. Antimicrobial usage (and misuse) in the human, animal, and environmental sectors is included in antimicrobial resistance. More importantly, the dissemination of resistant micro-organisms and resistance determinants inside, between, and across these sectors, as well as globally, must be addressed [
6].
Antibiotic use in human medicine, animal agriculture, and the environment are all interrelated variables in the development and spread of antibiotic resistance, according to One Health. For example, poor prescribing and patient noncompliance with antibiotics in human healthcare can contribute to the selection and spread of resistant microorganisms. Similarly, antibiotic usage in livestock production for growth promotion and disease prevention might contribute to the development of antibiotic resistance in animals and its subsequent transmission to people via the food chain[
7].
Figure 1.
An illustration of the One Health Approach concept [
4].
Figure 1.
An illustration of the One Health Approach concept [
4].
3. Antimicrobial Resistance as Global Health Threat
Antimicrobial resistance (AMR) has emerged as one of the most important global public health issues of the 21st century[
8]. Every year, nearly two million drug-resistant infectious illness cases and 23,000 deaths are reported worldwide. Irrational, unwise antibiotic prescribing and use are cited as major causes of AMR, and are frequently blamed and demonstrated as an irresponsible act by healthcare practitioners[
9].If left unchecked, AMR has the potential to become a major healthcare issue, maybe resulting in another pandemic. This underscores the importance of developing global health solutions based on AMR that take into consideration microdata from around the world[
10].
The causes of AMR are multifaceted, but there is no doubt that antibiotic misuse has been a major contributor. Antibiotic use grew by 65% globally between 2000 and 2015, mostly due to a significant growth in LMICs. Drug-resistant infections were predicted to cause 4.95 million fatalities worldwide in 2019, with low- and middle-income countries (LMICs) bearing the lion's share of the clinical burden, particularly in Sub-Saharan Africa. This greatly outnumbers the annual global mortality from tuberculosis (1.5 million), malaria (643,000), and HIV/AIDS (840,000)[
2].
4. Mechanisms of Antimicrobial Resistance
Antimicrobial resistance (AMR) requires a better knowledge of the underlying molecular processes. Advances in whole genome sequencing and other high-throughput unbiased instrumental technologies for studying the molecular pathogenesis of infectious illnesses allow for the collection of enormous amounts of data accessible to bioinformatics analysis and the identification of new AMR signatures[
11].
Antimicrobial resistance is driven by a variety of mechanisms, including innate bacterial features and several environmental factors affecting both prescribers and consumers Environmental factors (e.g., population and overcrowding, rapid spread through mass travel, poor sanitation, ineffective infection control programme, and widespread agricultural use), drug-related factors (e.g., counterfeit drugs, substandard drugs, and over-the-counter availability), patient-related factors (poor compliance, poverty, lack of education, self-medication, and misconception), and physician-related factors[
12].
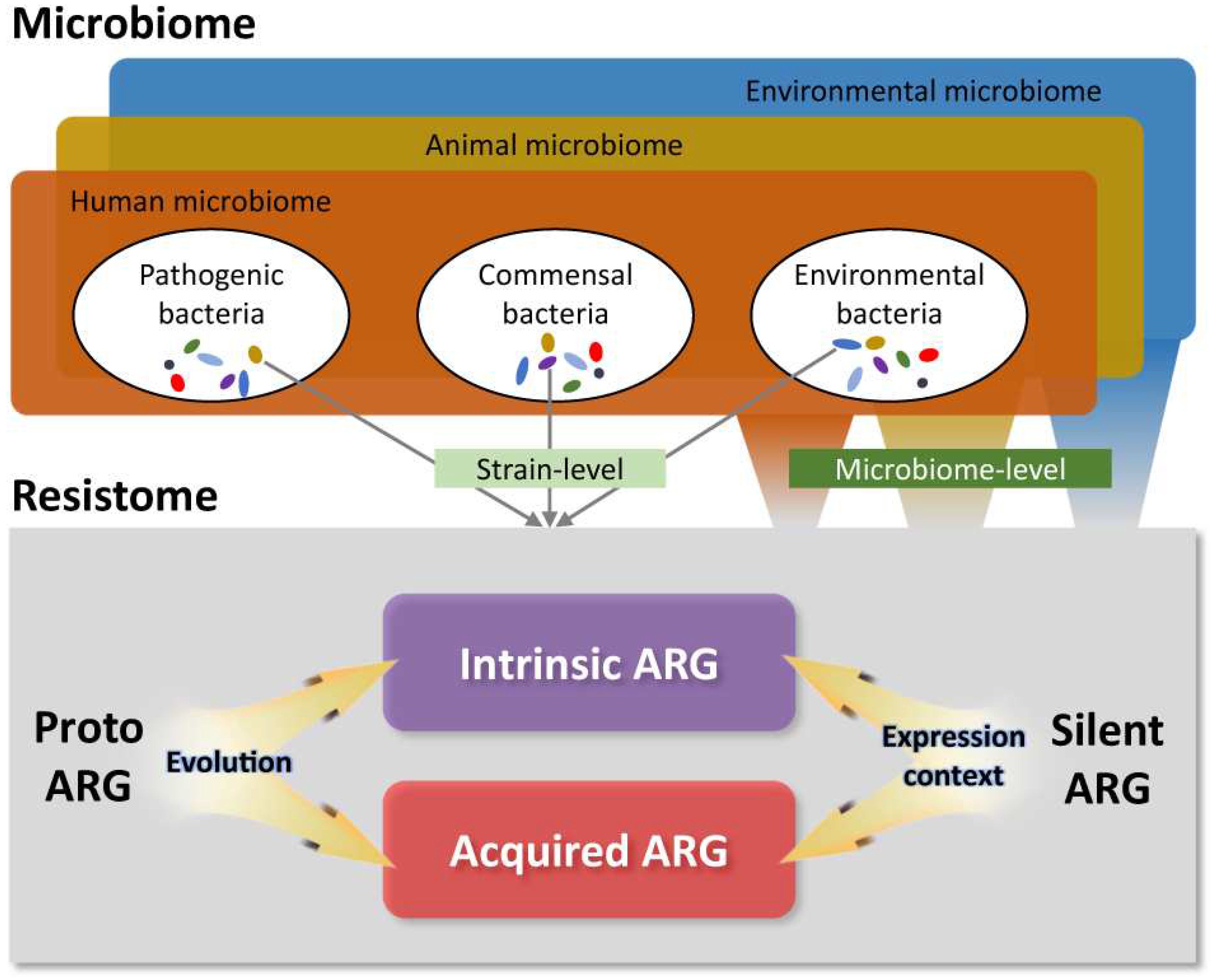
Antimicrobial resistance refers to all forms of ARGs (acquired and intrinsic resistance genes), their predecessors, and other possible resistance mechanisms within microbial communities that require evolution or changes in expression environment to bestow resistance[
13]. Genetic AMR develops as a result of bacterial genome alterations or the acquisition of antibiotic resistance genes from other bacteria. The changed or newly acquired genes bestow antibiotic resistance on the bacteria's progeny. Defined operationally, genetic AMR is the ability of a bacterial population to grow in the presence of an antibiotic at a much higher concentration, typically at least fourfold higher, than the minimum inhibitory concentration (MIC), where MIC is defined as the lowest concentration of the antibiotic that has routinely prevented visible growth of the same bacterial species in a growth-permissive culture medium[
14].
Figure 2.
The antibiotic resistance as seen via the One-Health lens [
15].
Figure 2.
The antibiotic resistance as seen via the One-Health lens [
15].
5. Management and response to AMR
Antimicrobial resistance practices, concepts, and interventions are key stages in the prevention and control of AMR. They are intended to encourage, improve, monitor, and evaluate the judicious use of antimicrobials in order to preserve their future efficacy, as well as to promote and protect public health. Through the implementation of evidence-based interventions[
9].
Infection prevention and control is one of the most cost-effective interventions against antimicrobial resistance (AMR)[
16]. Several nations and international organisations have now included a One Health Approach in their antimicrobial resistance action plans. Antimicrobial use must be improved, as well as legislation and policy, as well as surveillance, stewardship, infection control, sanitation, animal husbandry, and the development of antimicrobial alternatives[
17].
The WHO Global Action Plan's One Health concept is appropriate and compatible with assertions made in action plans from other international and national organisations. However, there is still a long way to go until a fully integrated One Health approach to antimicrobial resistance is applied on a national and global scale. Among the numerous obstacles to overcome are competing interests among multiple sectors and organisations (involving animals, humans, and the environment), agreement on action priorities, and gaps in antimicrobial resistance surveillance, antimicrobial use policy, and infection control in many parts of the world[
17].
6. Conclusions
Significant morbidity, death, and financial cost are brought on by the restricted therapy choices for AMR infections. Surveillance, reducing the use of antibiotics in healthcare and agriculture, providing access to high-quality, reasonably priced medications, vaccinations, and diagnostics, as well as enforcing legal requirements, are all necessary immediate steps to prevent AMR.An international and national organisation working together is essential to solving this problem. In order to stop AMR from spreading and to create new antibiotics, it is helpful to understand its mechanisms.
to address the issue of antibiotic resistance, as well as the "One Health Approach," a system encompassing a multidisciplinary effort to produce the greatest possible health outcome by acknowledging the clear linkages between humans, animals, and their shared environment. The relevance of public awareness and health literacy among lay audiences must be stressed much more as part of global and local action strategies.
To ensure that there is always an adequate supply of potent antimicrobials available in the globe to support human and animal health, today and in the future, success will require collaboration across individuals, communities, and governments.
Funding
No funding was received for this work.
Conflicts of Interest
The author declares no conflict of interest.
References
- Programme(UNEP), U.N.E., Antimicrobial resistance: a global threat. 2023.
- Walsh, T.R., et al., Antimicrobial resistance: addressing a global threat to humanity. 2023, Public Library of Science San Francisco, CA USA. p. e1004264. [CrossRef]
- Tang, K.W.K., B.C. Millar, and J.E. Moore, Antimicrobial resistance (AMR). British Journal of Biomedical Science, 2023. 80: p. 11387. [CrossRef]
- Moo, C.-L., et al., Mechanisms of antimicrobial resistance (AMR) and alternative approaches to overcome AMR. Current drug discovery technologies, 2020. 17(4): p. 430-447. [CrossRef]
- Coghlan, S., et al., A bolder One Health: expanding the moral circle to optimize health for all. One Health Outlook, 2021. 3: p. 1-4. [CrossRef]
- Nardulli, P., et al., The Role of Stakeholders’ Understandings in Emerging Antimicrobial Resistance: A One Health Approach. Microorganisms, 2023. 11(11): p. 2797. [CrossRef]
- Cella, E., et al., Joining forces against antibiotic resistance: The one health solution. Pathogens, 2023. 12(9): p. 1074. [CrossRef]
- Prestinaci, F., P. Pezzotti, and A. Pantosti, Antimicrobial resistance: a global multifaceted phenomenon. Pathogens and global health, 2015. 109(7): p. 309-318. [CrossRef]
- Majumder, M.A.A., et al., Antimicrobial stewardship: Fighting antimicrobial resistance and protecting global public health. Infection and drug resistance, 2020: p. 4713-4738. [CrossRef]
- Aljeldah, M.M., Antimicrobial resistance and its spread is a global threat. Antibiotics, 2022. 11(8): p. 1082. [CrossRef]
- Van Camp, P.-J., D.B. Haslam, and A. Porollo, Bioinformatics approaches to the understanding of molecular mechanisms in antimicrobial resistance. International journal of molecular sciences, 2020. 21(4): p. 1363. [CrossRef]
- Salam, M.A., et al. Antimicrobial resistance: a growing serious threat for global public health. in Healthcare. 2023. MDPI. [CrossRef]
- Reygaert, W.C., An overview of the antimicrobial resistance mechanisms of bacteria. AIMS microbiology, 2018. 4(3): p. 482. [CrossRef]
- Schrader, S.M., J. Vaubourgeix, and C. Nathan, Biology of antimicrobial resistance and approaches to combat it. Science translational medicine, 2020. 12(549): p. eaaz6992. [CrossRef]
- Kim, D.-W. and C.-J. Cha, Antibiotic resistome from the One-Health perspective: Understanding and controlling antimicrobial resistance transmission. Experimental & Molecular Medicine, 2021. 53(3): p. 301-309. [CrossRef]
- Lacotte, Y., et al., Infection prevention and control research priorities: what do we need to combat healthcare-associated infections and antimicrobial resistance? Results of a narrative literature review and survey analysis. Antimicrobial Resistance & Infection Control, 2020. 9: p. 1-10. [CrossRef]
- Collignon, P.J. and S.A. McEwen, One health—its importance in helping to better control antimicrobial resistance. Tropical medicine and infectious disease, 2019. 4(1): p. 22. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).