1. Introduction
Large to massive rotator cuff tears (LMRCTs) are challenging to manage, especially in achieving satisfactory healing. They are almost always accompanied by chronic tendon wear, severe retraction, muscle atrophy, and fatty degeneration.[1,2,3] Among the numerous repair techniques for LMRCTs, Burkhart was the first to introduce partial repair.[4] Its basic principle is to maintain a force couple that enables sufficient shoulder function, leading to functional repair, not anatomical repair of the part.[5] Partial repair is relatively simple compared with other complex techniques, and good results have been reported.[6] Although partial repair is not a perfect solution, it is a treatment technique recognized to produce somewhat favorable results among the existing methods [8]; surgeons might consider it a viable option. However, a recent study showed that almost half of patients were dissatisfied with the worsening results over time, even though partial repair could improve selected outcomes at a two-year follow-up.[7]
In recent years, arthroscopic biceps rerouting (BR) has been introduced as a novel technique for large irreparable rotator cuff tears, and a cadaveric study reported that it was effective in providing biomechanically valid results.[8] A few studies have introduced the use of the long head of biceps tendon (LHBT) for treating massive rotator cuff tears.[9,10,11,12,13] In other studies, LHBT was tenotomized distally, and the patient was at risk of having unexpected disadvantages of biceps tenotomy.[11,12,13] In contrast, Kim et al. [14] proposed a novel technique called "arthroscopic biceps rerouting" (BR) to treat LMRCTs that maintain the original continuity of the LHBT. With the BR technique, the LHBT is rerouted to a new groove posterior to the original groove without distal tenotomization. Recent studies have reported favorable preliminary outcomes.[8,15]This study aimed to compare the clinical and radiological outcomes between the two techniques. We hypothesized that BR would show better clinical and radiological outcomes than partial repair in LMRCTs.
2. Materials and Methods
This retrospective comparative study of partial repair and BR performed by a senior surgeon at a single institution was conducted between December 2013 and June 2019. The lesions were checked preoperatively using magnetic resonance imaging (MRI) and visualized arthroscopically during surgery. The indication for surgery was rotator cuff tear that did not respond to medication.
Inclusion criteria were as follows: [1] patients who underwent incomplete rotator cuff repair with the articular surface of the humeral head exposed, that is, footprint coverage of <80%.[16]
[2] patients who were followed-up for at least one year after surgery and underwent MRI preoperatively and at one year postoperatively.
Patients with a history of trauma, labral or biceps lesions, glenohumeral arthritis, concomitant shoulder stiffness, or subscapularis tears requiring repair were excluded. This study was approved by the Institutional Review Board of our hospital (No. CHOSUN 2021-08-001-001).
Baseline characteristics
In total, 132 patients underwent partial repair or BR. Nineteen patients were lost to follow-up one year after surgery, and five patients declined participation in the study. Moreover, 36 patients who underwent subscapularis repair were excluded. Finally, 72 patients were included in this study. Group I (n=31) included patients who underwent partial rotator cuff repair without any LHBT procedures. Group II (n=41) included patients who had undergone BR. There was no specific selection method for the surgical procedures. Since March 2017, BR has been performed in patients with similar condition in the absence of the biceps long head tendon lesions.
One senior surgeon performed all the operations at a single institute. All the arthroscopic procedures were performed with the patient under general anesthesia in the lateral decubitus position. We used a standard posterior portal to check the glenohumeral joint in order to address associated intra-articular lesions. An anterior portal was routinely created through the rotator interval for the working portal using a spinal needle. A probe was used to check for the presence of LHBT. Arthroscopic debridement was performed on partial-thickness subscapularis tears less than the superior third. The subacromial space was examined using a posterior viewing portal. An anterolateral working portal was created by using a spinal needle. Debridement, bursectomy, and acromioplasty were also performed. We switched the viewing portal to a posterolateral rear-viewing portal and checked the tear size and reducibility of the tendon.
In group I, partial repair was performed if excessive tension occurred to cover the footprint, even after sufficient tendon release. A modified Mason-Allen single-row or transosseous-equivalent technique was used. It was performed considering tendon tear geometry, tissue quality condition, and force couple.
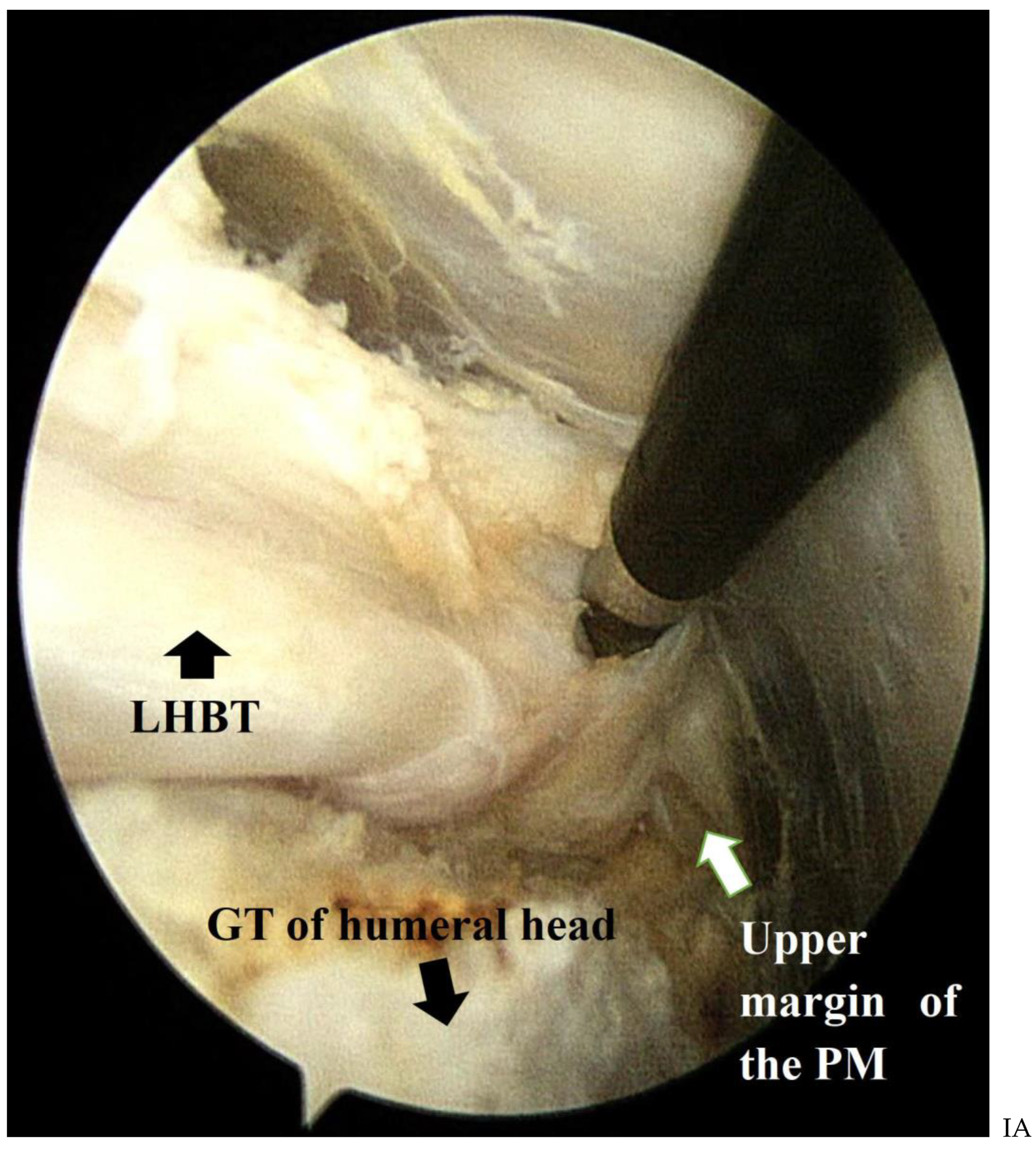
Surgical techniques in group II (cases of BR) are described in detail in the arthroscopy techniques paper.[14] The soft tissues around the LHBT were released to the upper margin of the pectoralis major, which was located approximately 6 cm distal to the anterolateral portal (
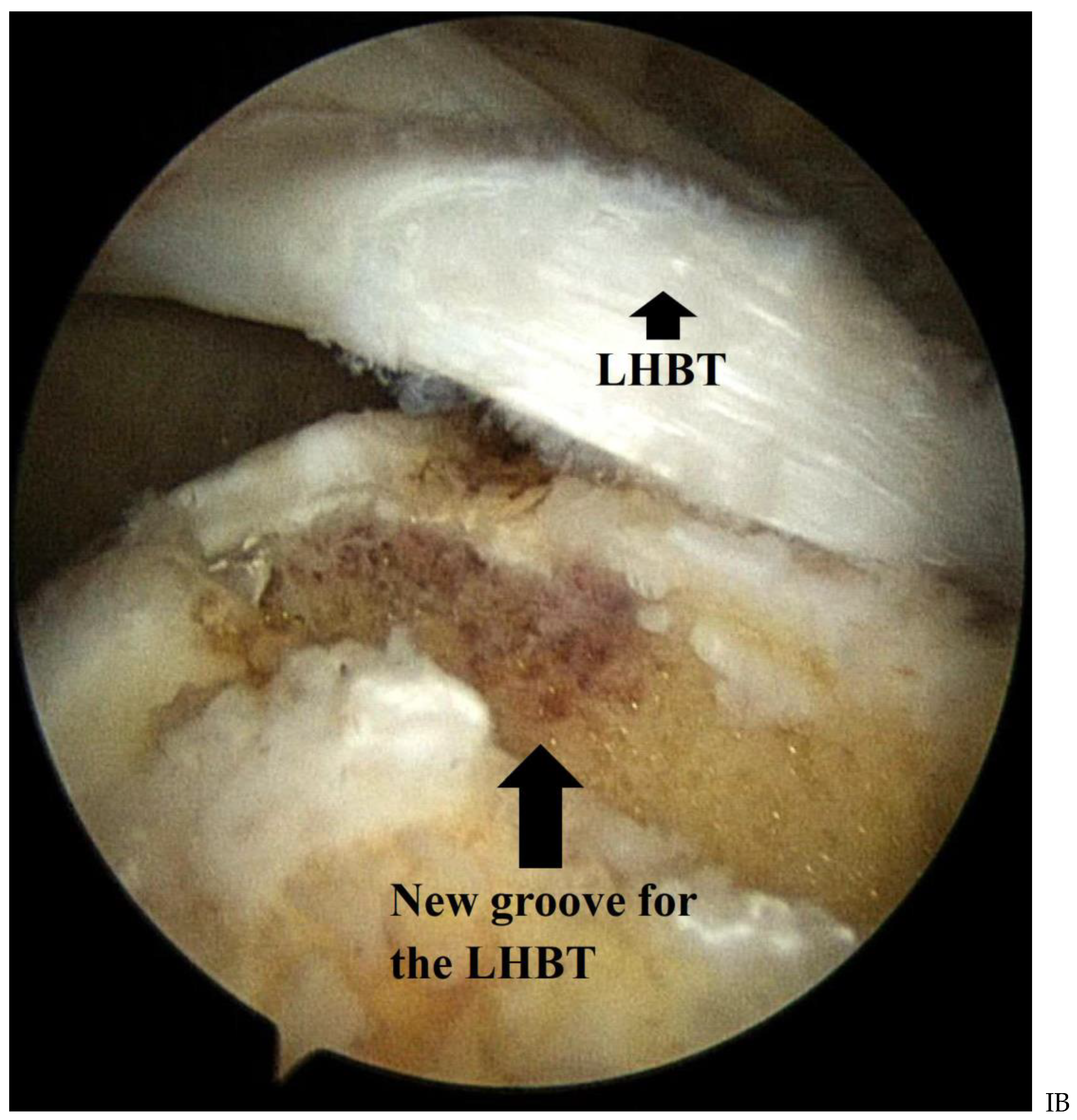
Figure 1-A). We created a new groove to place the released biceps tendon by using an elliptical burr (
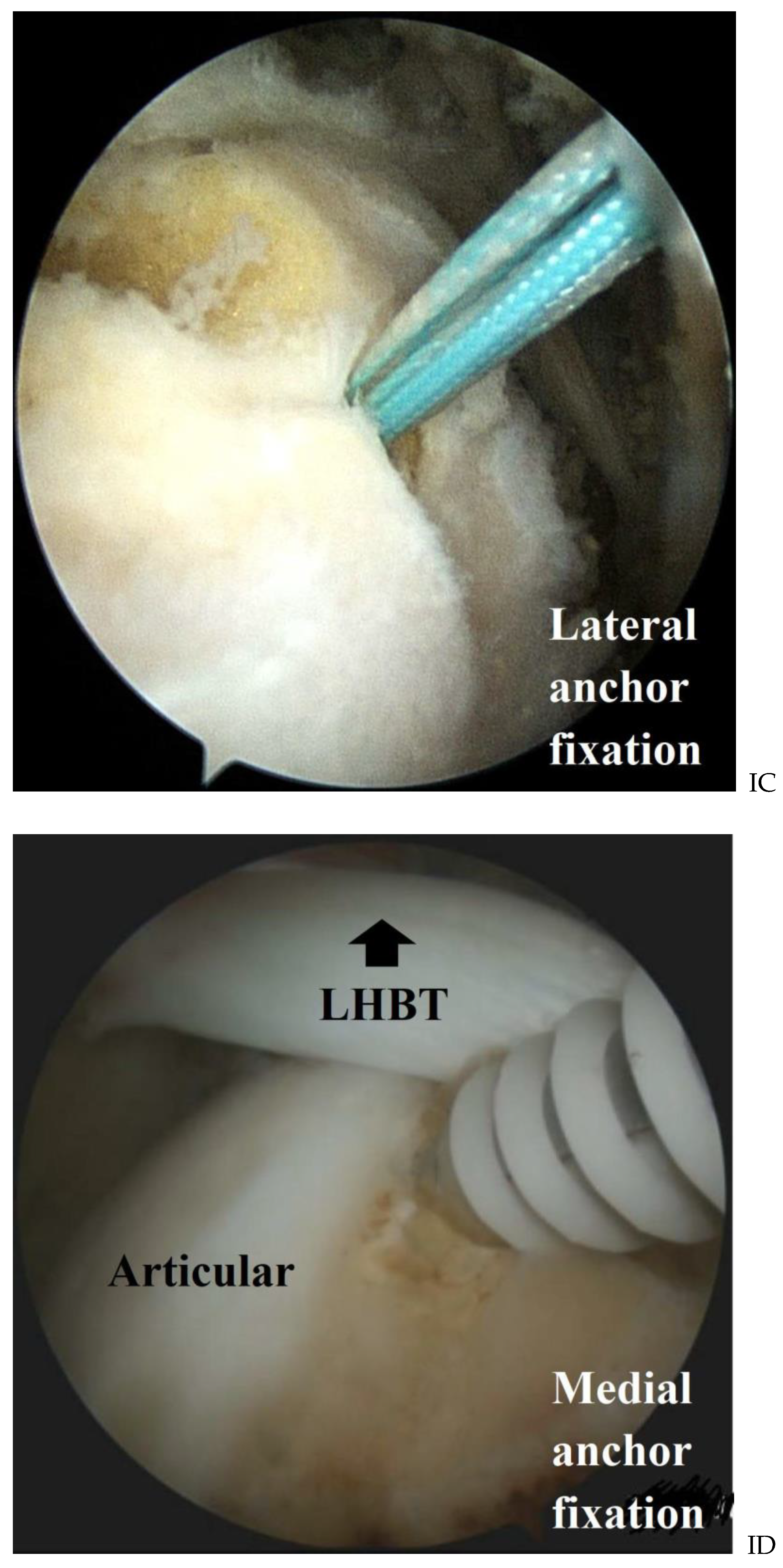
Figure 1-B). Two anchors were used to fix the biceps tendon to the new groove. One anchor was inserted at the lateral margin of the newly created biceps groove. Another anchor was placed in the medial part of the rerouted biceps tendon at the cartilage margin (
Figure 1-C, D). Lateral and medial ties at each side were performed to fix the rerouted biceps tendon on the newly made groove. One or more anchors were used to repair the rotator cuff tendon.
The American Shoulder and Elbow Surgeons (ASES) score, Korean Shoulder Score (KSS), and Visual Analog Scale (VAS) pain score (0–10) were used to assess clinical outcomes. A goniometer measured the range of motion (ROM) of forward flexion (FF), external rotation at the side, and external rotation at 90° of abduction. Internal rotation was defined as the highest vertebral level at which the tip of the thumb could reach a sedentary position. The vertebral levels were numbered serially from below the sacrum (level 0) to the 7th thoracic vertebra (level 12). Clinical evaluations, including ROM, were performed before surgery, at 3, 6, and 12 months after surgery and at the last follow-up. Radiological evaluation was performed using plain anteroposterior radiographs and MRI. The acromiohumeral interval (AHI), which is the smallest distance from the superior margin of the humeral head to the undersurface of the acromion, was checked preoperatively and three months postoperatively. Magnetic resonance imaging was performed 12 months postoperatively. We used the Sugaya classification[17] to evaluate the repaired cuff tendon and considered Sugaya classification types 4 and 5 as retears. Clinical and radiological evaluations were performed by a physician blinded to the study.
All the patients underwent similar rehabilitation protocol after the surgery. An abduction brace was applied for six weeks after the surgery. After the brace was discarded, the patients were taught the sleeper-stretch and pulley exercises. Two months after the surgery, the patients started pendulum exercises. Three months after the surgery, the patients underwent muscle-strengthening exercises using Theraband. After six months, the patients were able to engage in preoperative and sports activities.
All statistical analyses were performed using SPSS (version 24.0; SPSS Inc., Chicago, IL, USA). A paired t-test (two-tailed t-test) was used to compare ROM and functional scores at each time point between the two groups. The Mann-Whitney U-test was used to compare the integrity of the repaired cuff tendon with the Sugaya classification. Statistical significance was set at P<0.05.
3. Results
Demographic parameters showed no significant differences between the two groups (P>0.05,
Table 1). Group I included 10 males and 21 females with a mean age of 67.1 years (range, 45–77 years). Group II included 15 males and 26 females with a mean age of 65.5 years (range, 54–82 years). The mean follow-up period was 23.25 (range, 12–53 months) in group I and 21.24 months (range, 12–35 months) in group II. In Group I, there was a significant improvement in the clinical outcomes preoperatively and at the last follow-up (VAS, 3.57 ± 1.87 to 1.57 ± 0.98; ASES score, 55.86 ± 13.38 to 79.94 ± 11.17; CS, 62.50 ± 16.38 to 81.56 ± 11.25; and KSS, 60.73 ± 14.51 to 81.31 ± 16.87; P<0.001), and there was no significant difference in ROM (P>0.05) (
Table 2). Similarly, in group II, there was a significant improvement in clinical outcomes preoperatively and at the last follow-up (VAS, 2.96 ± 2.05 to 1.33 ± 1.34; ASES score, 54.67 ± 22.33 to 82.83 ± 11.94; CS, 60.08 ± 19.18 to 82.94 ± 7.17; and KSS, 53.38 ± 19.71 to 85.69 ± 10.21; P<0.001), but there was no significant difference in ROM (P>0.05) (
Table 3).
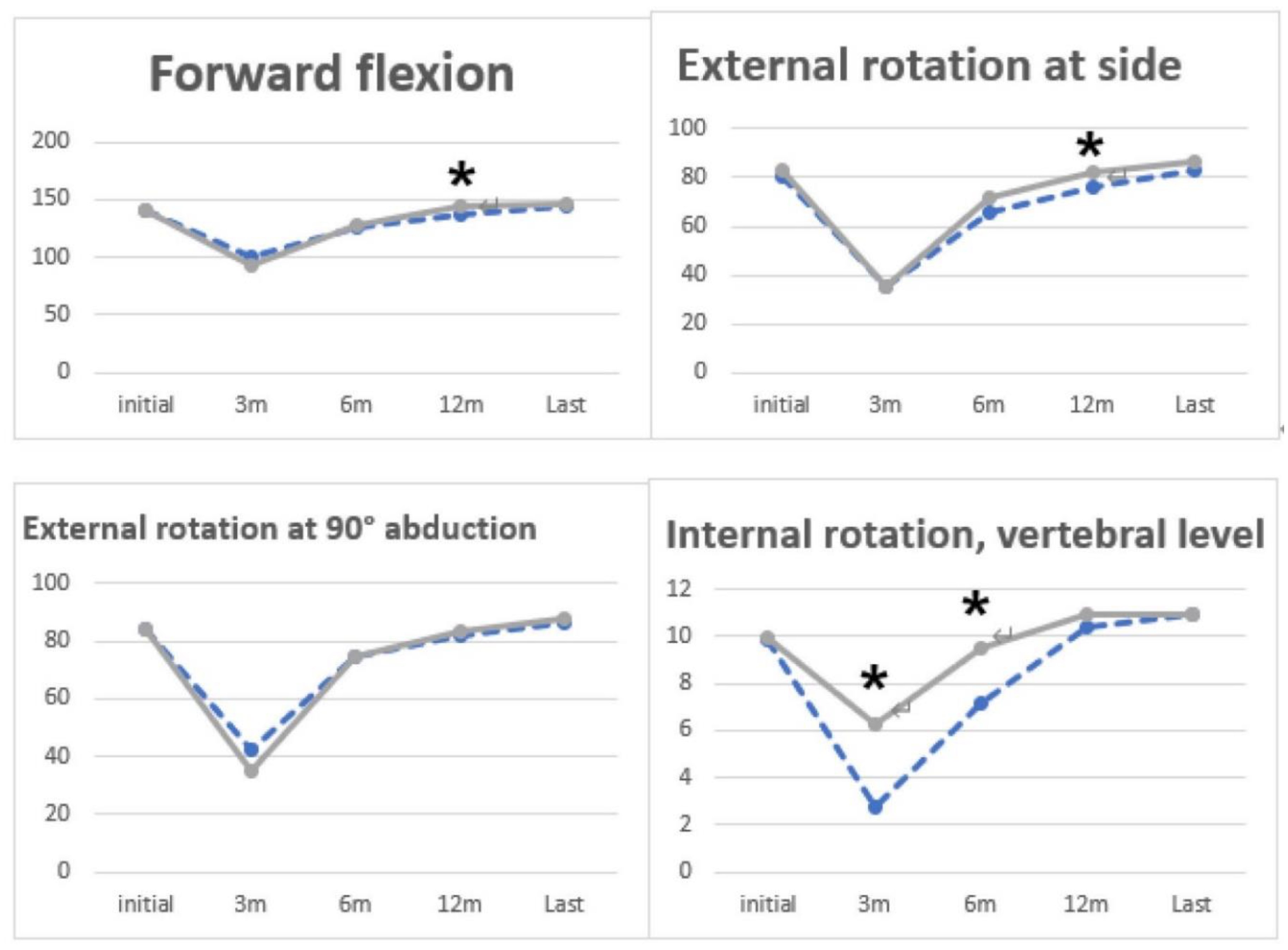
In group I, compared to group II, FF (P=0.02, group I: 137.24 ± 9.87 and group II: 143.79 ± 8.09,
Figure 2 and
Table 4) and external rotation at the side (P=0.04, group I: 75.71 ± 12.60 and group II: 82.14 ± 6.86;
Figure 2 and
Table 4) at 12 months postoperatively and internal rotation on POD 3 (P=0.002, group I: 2.74 ± 2.99 and group II: 6.26 ± 3.37;
Figure 2 and
Table 4) and at six months (P=0.01, group I: 7.16 ± 3.33 and group II: 9.48 ± 2.26;
Figure 2 and
Table 4) showed significantly better ROM. There was no significant difference in ROM between the two groups at the last follow-up (P>0.05). There were significantly better clinical outcomes in ASES (P=0.047, group I: 71.25 ± 21.72 and group II: 83.13 ± 12.89) and KSS (P=0.048, group I: 70.60 ± 15.72 and group II: 80.67 ± 14.30) at 12 months postoperatively (
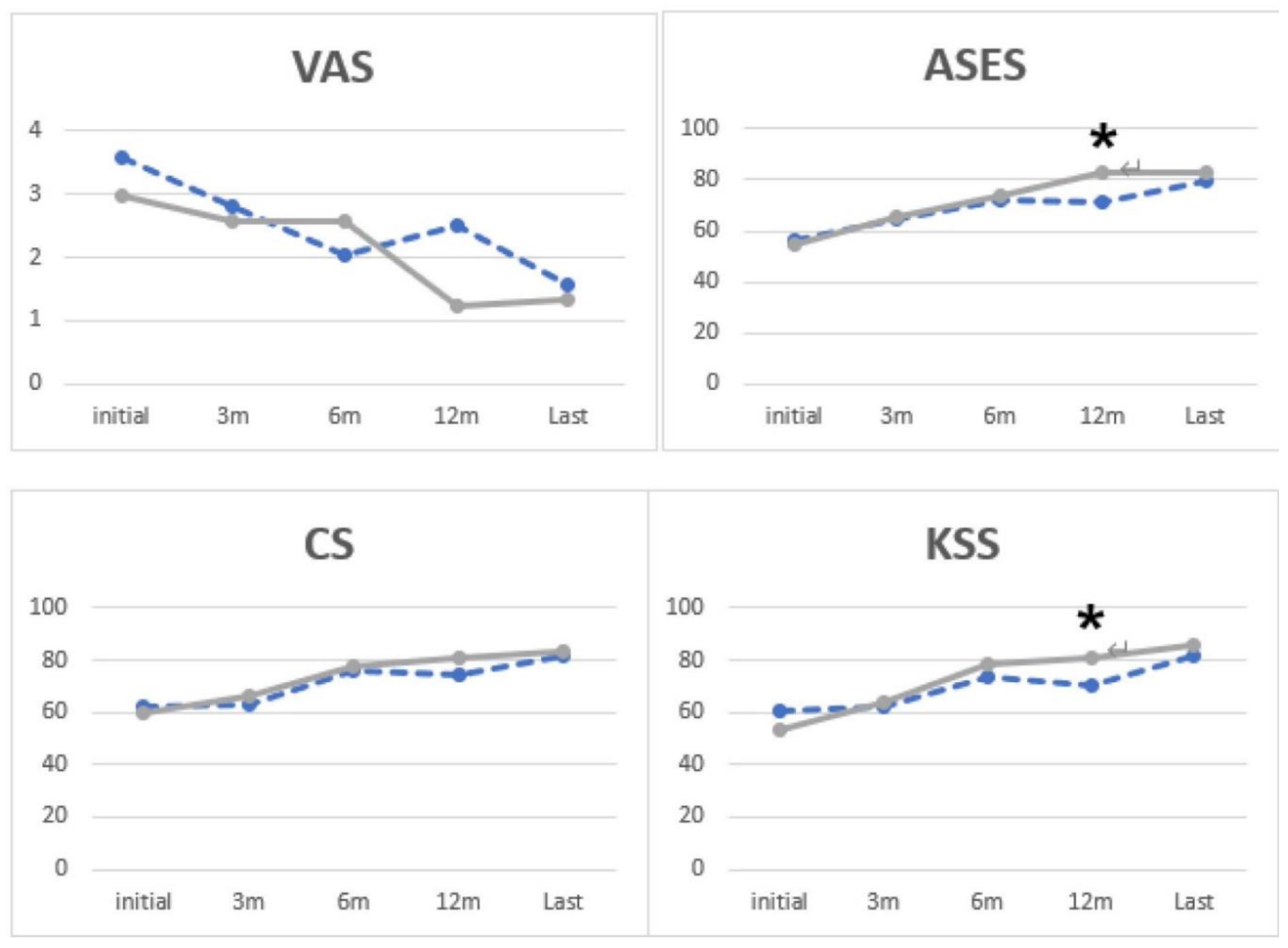
Figure 3 and Table 5).
We used the Sugaya classification system to assess the integrity of the repaired cuff tendon. Type IV or V was considered a retear. Retear was found in nine patients in group I (29.03%, 9/31) and eight in group II (19.51%, 8/41, P=0.35; Table 6). Rupture of the LHBT was confirmed in six of eight cases of retears in group II. Long head of biceps tendon rupture around the medial anchor was observed in five cases, and rupture around the lateral anchor was observed in one case. Nevertheless, Popeye deformity was not observed, and none of the patients complained of upper arm pain related to the bicep tendon. In both groups, no significant difference in AHD, or the occurrence of glenohumeral joint osteoarthritis was observed during the follow-up period.
This section may be divided by subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
3.1. Figures, Tables and Schemes
Figure 1.
Subacromial space of right shoulder viewing from the posterior portal with left side down lateral decubitus position. (A) Soft tissue removal around the LHBT to make its mobility until the upper maring of the PM. (B) A New groove was placed posterior to the original groove of the LHBT. (C, D) Medial and lateral anchor fixation for rerouted LHBT. (LHBT, long head of biceps tendon; GT, greater tuberosity; PM, pectoralis major).
Figure 1.
Subacromial space of right shoulder viewing from the posterior portal with left side down lateral decubitus position. (A) Soft tissue removal around the LHBT to make its mobility until the upper maring of the PM. (B) A New groove was placed posterior to the original groove of the LHBT. (C, D) Medial and lateral anchor fixation for rerouted LHBT. (LHBT, long head of biceps tendon; GT, greater tuberosity; PM, pectoralis major).
Figure 2.
Range of motion at each time point. The text ‘*’ means a P-value under 0.05.(dotted line: Group I, solid line: Group II). The vertebral level was numbered serially as follows: 0 point for any level below the sacral region and 1 point for each level above the sacrum.
Figure 2.
Range of motion at each time point. The text ‘*’ means a P-value under 0.05.(dotted line: Group I, solid line: Group II). The vertebral level was numbered serially as follows: 0 point for any level below the sacral region and 1 point for each level above the sacrum.
Figure 3.
Clinical score at each time point. The text ‘*’ means a P-value under 0.05. (dotted line: Group I, solid line: Group II). VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons; CS, Constant Score; KSS, Korean Shoulder Score.
Figure 3.
Clinical score at each time point. The text ‘*’ means a P-value under 0.05. (dotted line: Group I, solid line: Group II). VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons; CS, Constant Score; KSS, Korean Shoulder Score.
Table 1.
Preoperative demographic data.
Table 1.
Preoperative demographic data.
| |
group I (n=31) |
group II (n=41) |
P value |
| Age, years |
67.10 |
65.49 |
0.87 |
| Sex, male/female, n |
10/21 |
15/26 |
0.69 |
| Follow-up period (range), months |
23.25 [12–36] |
21.24 [12–34] |
0.93 |
| Tear size, mm |
|
|
|
| medial to lateral |
31.9 |
31.3 |
0.14 |
| anterior to posterior |
26.1 |
27.4 |
0.71 |
| Acromiohumeral interval |
7.89 |
7.91 |
0.83 |
Fatty infiltration
(Goutallier classification), n (%) |
|
|
0.13 |
| Grade 1 |
0 (0) |
0 (0) |
|
| Grade 2 |
4 (14.8) |
10 (11.1) |
|
| Grade 3 |
19 (59.2) |
25 (66.6) |
|
| Grade 4 |
8 (25.9) |
6 (22.2) |
|
| Initial ROM |
| Forward flexion, ˚ |
140.38±9.89 |
140.19±18.35 |
0.97 |
| External rotation at side, ˚ |
80.38±10.76 |
82.69±14.02 |
0.52 |
| External rotation at 90 ˚ of abduction, ˚ |
83.85±7.52 |
84.23±13.01 |
0.90 |
| Internal rotation, vertebral level |
9.88±2.79 |
9.92±2.81 |
0.96 |
| Initial clinical score |
| VAS score for pain |
3.57±1.87 |
2.96±2.05 |
0.06 |
| ASES score |
55.86±13.38 |
54.67±22.33 |
0.80 |
| Constant score |
62.50±16.38 |
60.08±19.18 |
0.49 |
| Korean Shoulder Score |
60.73±14.51 |
53.38±19.71 |
0.24 |
Table 2.
Comparison of outcomes after partial repair.
Table 2.
Comparison of outcomes after partial repair.
| |
Preoperative |
Last follow-up |
P value |
| Range of motion |
|
|
|
| Forward flexion,˚ |
140.38±9.89 |
145.18±6.57 |
0.48 |
| External rotation at side, ˚ |
80.38±10.76 |
82.92±9.99 |
0.56 |
| External rotation at 90 ˚ of abduction |
83.85±7.52 |
86.54±6.29 |
0.21 |
| Internal rotation, vertebral level |
9.88±2.79 |
10.95±1.39 |
0.08 |
| Clinical outcome |
|
|
|
| VAS |
3.57±1.87 |
1.57±0.98 |
<0.001 |
| ASES score |
55.86±13.38 |
79.94±11.17 |
<0.001 |
| CS |
62.50±16.38 |
81.56±11.25 |
<0.001 |
| KSS |
60.73±14.51 |
81.31±16.87 |
<0.001 |
Table 3.
Comparison of outcomes after biceps rerouting.
Table 3.
Comparison of outcomes after biceps rerouting.
| |
Preoperative |
Last follow-up |
P value |
| Range of motion |
|
|
|
| Forward flexion,˚ |
140.19±18.35 |
146.48±6.32 |
0.15 |
| External rotation at side, ˚ |
82.69±14.02 |
86.67±6.37 |
0.16 |
| External rotation at 90 ˚ of abduction |
84.23±13.01 |
87.69±5.14 |
0.63 |
| Internal rotation, vertebral level |
9.92±2.81 |
10.95±2.01 |
0.09 |
| Clinical outcome |
|
|
|
| VAS |
2.96±2.05 |
1.33±1.34 |
<0.001 |
| ASES score |
54.67±22.33 |
82.83±11.94 |
<0.001 |
| CS |
60.08 ±19.18 |
82.94±7.17 |
<0.001 |
| KSS |
53.38±19.71 |
85.69±10.21 |
<0.001 |
Table 4.
Range of motion at each time point.
Table 4.
Range of motion at each time point.
| |
Preoperative |
3 months |
6 months |
12 months |
Last follow-up |
| Forward flexion,˚ |
|
|
|
|
|
| Group I |
140.38±9.89 |
99.82±22.21 |
126.72±15.59 |
137.24±9.87 |
145.18±6.57 |
| Group II |
140.19±18.35 |
92.07±29.20 |
128.44±19.04 |
143.79±8.09 |
146.48±6.32 |
| P value |
0.97 |
0.25 |
0.69 |
0.02 |
0.47 |
| External rotation at side, ˚ |
|
|
|
|
|
| Group I |
80.38±10.76 |
35.20±21.63 |
66.00±17.93 |
75.71±12.60 |
82.92±9.99 |
| Group II |
82.69±14.02 |
35.60±23.11 |
72.00±12.43 |
82.14±6.86 |
86.67±6.37 |
| P value |
0.52 |
0.95 |
0.13 |
0.04 |
0.19 |
| External rotation at 90 ˚ of abduction |
|
|
|
|
|
| Group I |
83.85±7.52 |
42.40±23.50 |
74.84±14.35 |
81.79±8.63 |
86.54±6.29 |
| Group II |
84.23±13.01 |
35.20±22.94 |
74.52±12.34 |
83.57±9.89 |
87.69±5.14 |
| P value |
0.90 |
0.30 |
0.92 |
0.50 |
0.50 |
| Internal rotation, vertebral level |
|
|
|
|
|
| Group I |
9.88±2.79 |
2.74±2.99 |
7.16±3.33 |
10.43±1.86 |
10.95±1.39 |
| Group II |
9.92±2.81 |
6.26±3.37 |
9.48±2.26 |
10.90±1.61 |
10.95±2.01 |
| P value |
0.96 |
0.00 |
0.01 |
0.45 |
1.00 |
4. Discussion
In our study, both the partial repair and BR groups showed significant improvements in clinical outcomes of LMRCTs. The BR group showed an earlier recovery of ROM after the surgery than the partial repair group, and it showed significantly better results in internal rotation at three and six months postoperatively and FF and external rotation at 12 months postoperatively. Additionally, clinical scores, such as the ASES and KSS were significantly better in the BR group than in the partial repair group at 12 months postoperatively. This suggests that the BR group recovered faster than the partial repair group with respect to ROM and clinical outcomes.
The retear rate in the partial repair group was higher than that in the BR group, although there was no statistically significant difference between the two groups. Additionally, the BR group gave more weight to overall good results in the Sugaya classification than the partial repair group. There was no rupture of the LHBT in well-healed patients in the BR group. Long head of bicep tendon rupture was observed in the retears of patients with repaired cuff tendons. We can deduce that the rerouted LHBT is closely related to the cuff healing process. A recent animal study showed that rerouted LHBT increased load-bearing strength compared to the native superior capsule. It was also confirmed that the rerouted LHBT could engraft into the new groove for the LHBT and show excellent biomechanical performance.[18]
Partial repair is a relatively simple and easy technique that restores the force couple by replacing a non-functional tear with a functional tear. Numerous clinical and biomechanical studies have been conducted on this technique.[2] Kim et al. reported a significant improvement after arthroscopic partial repair in patients diagnosed with LMRCTs, and 81% of the patients who underwent surgery were satisfied.[6,19]A study by Yoo et al. [16] showed that approximately 50% of patients showed deterioration in clinical scores and poor satisfaction in long-term follow-up. Additionally, a decrease in AHI was observed in patients with exacerbation. Similarly, another study confirmed a decrease in AHI at a long-term follow-up after partial repair.[20] Many recent reports have argued that partial repair showed good results at short-term follow-up, but there is a possibility that it may worsen over time.
Recently, BR has been introduced as an innovative method for the treatment of LMRCTs.[14] After creating a new groove for the LHBT at the mid-portion of the footprint, move the LHBT to the new groove and repair the remaining rotator cuff. According to the preliminary outcomes of 61 patients who underwent BR followed up for >18 months, good results were found for pain VAS, ASES, and KSS. Acromiohumeral interval increased from 7.1 mm to 9.7 mm, and 16 (26%) patients showed retear of the repaired rotator cuff.[21] Most recently, there was a study comparing BR and conventional repair, and both groups showed good clinical results after surgery, but there was no significant difference between the two groups. However, the retear rate in the BR group was 18.6% and 48.1% in the conventional repair group, showing a significant difference between the two groups.[15]
We can postulate several possible reasons why the BR group showed better results in the early postoperative period than did the partial repair group. One reason is that the proximal portion of the biceps in the intra-glenohumeral joint can biomechanically act like the superior capsule of the glenohumeral joint.[21] In our previous cadaveric biomechanical study, BR showed a significant decrease in superior humeral translation and reduced subacromial contact pressure compared with the partial repair group.[8] Arthroscopic biceps rerouting stabilizes the glenohumeral joint, which reduces the load on the repaired tendon and lowers tension to facilitate blood supply. It also reduces acromial contact pressure, thereby reducing the stress on the repaired tendon. Ultimately, this provides a suitable environment for tendon healing. These can promote reinforcement of the repaired cuff and are thought to serve as an internal splint during the critical period of cuff healing. In addition to these mechanical effects, the use of biceps without cutting positively affected the blood supply required for cuff healing.[15] Furthermore, creating a new groove for the biceps, which is the core technique of BR, will help cuff healing by creating materials, such as stem cells from the bone marrow, fibroblasts, and chemical mediators, such as various growth factors and cytokines for tissue healing. According to a recent animal study, the rerouted biceps tendon can be remodeled progressively. Over time, it heals into new grooves in the tendon, resulting in bone-tendon healing that improves biomechanical performance.[18]
5. Conclusions
Both partial repair and repair with the BR technique for LMRCTs were effective in improving clinical and radiologic outcomes at the short-term follow-up. However, the BR technique yielded early recovery of ROM and better clinical outcomes than partial repair until at one year postoperatively. Retear occurred at a higher probability in group I than in group II. This may be a useful method for repairing LMRCTs.
Author Contributions
Conceptualization, Yang-Soo Kim; methodology, Yang-Soo Kim; software, Kwon-Hyoung Ham; validation, Kwon-Hyoung Ham; formal analysis, Hyung-Seok Park; investigation Hyung-Seok Park; resources, Kwon-Hyoung Ham; data curation, Kwon-Hyoung Ham; writing—original draft preparation, Hyung-Seok Park; writing—review and editing, Yang-Soo Kim; visualization, Hyung-Seok Park; supervision, Yang-Soo Kim; project administration, Yang-Soo Kim; funding acquisition, Hyung-Seok Park. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by research fund from Chosun University Hospital, 2022.
Institutional Review Board Statement
This study was approved by the IRB of Chosun university hospital (CHOSUN 2021-08-001-001)
Informed Consent Statement
Patient consent was waived due to retrospective study
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92(9):1894-908. [CrossRef]
- Kim SJ, Kim YH, Chun YM. Arthroscopic Partial Repair of Massive Contracted Rotator Cuff Tears. Clinics in Shoulder and Elbow. 2014;17(1):44-7. [CrossRef]
- Rho JY, Kwon YS, Choi S. Current Concepts and Recent Trends in Arthroscopic Treatment of Large to Massive Rotator Cuff Tears: A Review. Clin Shoulder Elb. 2019;22(1):50-7. [CrossRef]
- Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10(1):4-19. [CrossRef]
- Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991(267):45-56.
- Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28(6):761-8. [CrossRef]
- Shon MS, Koh KH, Lim TK, Kim WJ, Kim KC, Yoo JC. Arthroscopic Partial Repair of Irreparable Rotator Cuff Tears: Preoperative Factors Associated With Outcome Deterioration Over 2 Years. Am J Sports Med. 2015;43(8):1965-75.
- Han SY, Lee TQ, Wright DJ, Park IJ, Mauro M, McGarry MH, et al. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: a cadaveric biomechanical study. J Shoulder Elbow Surg. 2020;29(7):1425-34. [CrossRef]
- Veen EJD, Stevens M, Diercks RL. Biceps Autograft Augmentation for Rotator Cuff Repair: A Systematic Review. Arthroscopy. 2018;34(4):1297-305. [CrossRef]
- Park SR, Sun DH, Kim J, Lee HJ, Kim JB, Kim YS. Is augmentation with the long head of the biceps tendon helpful in arthroscopic treatment of irreparable rotator cuff tears? J Shoulder Elbow Surg. 2018;27(11):1969-77.
- Lin J, Qi W, Liu Z, Chen K, Li X, Yan Y, et al. An arthroscopic technique for full-thickness rotator cuff repair by transposition of the long head of biceps. Orthop Traumatol Surg Res. 2019;105(2):265-9. [CrossRef]
- Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105(2):257-63. [CrossRef]
- El-Shaar R, Soin S, Nicandri G, Maloney M, Voloshin I. Superior Capsular Reconstruction With a Long Head of the Biceps Tendon Autograft: A Cadaveric Study. Orthop J Sports Med. 2018;6(7):2325967118785365. [CrossRef]
- Kim YS, Lee HJ, Park I, Sung GY, Kim DJ, Kim JH. Arthroscopic In Situ Superior Capsular Reconstruction Using the Long Head of the Biceps Tendon. Arthrosc Tech. 2018;7(2):e97-e103. [CrossRef]
- Rhee SM, Youn SM, Park JH, Rhee YG. Biceps Rerouting for Semirigid Large-to-Massive Rotator Cuff Tears. Arthroscopy. 2021. [CrossRef]
- Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25(10):1093-100. [CrossRef]
- Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307-16. [CrossRef]
- Xu J, Li Y, Zhang X, Han K, Ye Z, Wu C, et al. The Biomechanical and Histological Processes of Rerouting Biceps to Treat Chronic Irreparable Rotator Cuff Tears in a Rabbit Model. Am J Sports Med. 2022;50(2):347-61. [CrossRef]
- Mori D, Funakoshi N, Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: patch autograft procedure versus partial repair procedure. Arthroscopy. 2013;29(12):1911-21. [CrossRef]
- Wellmann M, Lichtenberg S, da Silva G, Magosch P, Habermeyer P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy. 2013;29(8):1275-82. [CrossRef]
- Kim JH, Lee HJ, Park TY, Lee JU, Kim YS. Preliminary Outcomes of Arthroscopic Biceps Rerouting for the Treatment of Large to Massive Rotator Cuff Tears. J Shoulder Elbow Surg. 2020. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).