1. Introduction
Being diagnosed with an incurable chronic disease such as multiple sclerosis (MS) can significantly alter an individual's life, resulting in physical limitations and profound psychological effects. As the prevalence of MS increases worldwide [
1], it is becoming increasingly important to identify and implement accessible ways to enhance patients' resilience so that they can effectively cope with the challenges of the disease and strengthen their ability to overcome it.
Resilience refers to an individual's ability to adapt and withstand life's challenges. It has become increasingly important, particularly during the COVID-19 pandemic [
2]. Improving psychological resilience in patients with multiple sclerosis may be a promising approach to enhancing their quality of life.
Previous studies have suggested that resilience may be a stable personality trait. However, it is now understood that resilience is dynamic and focused on individual development [
3] rather than a fixed perspective. Foundational studies [
4,
5,
6] have collectively influenced the concept of resilience as being malleable and flexible, challenging the original notion that it is a fixed personality trait. As resilience is not a stable trait, it can be improved through training. The current research literature indicates that such interventions are promising.
A pilot evaluation was conducted to assess the effectiveness and feasibility of a group resilience training for individuals with MS. The training was based on acceptance and commitment therapy (ACT) and showed promising results [
7]. Furthermore, a study examined the relationship between psychological resilience and social and occupational performance in people with MS, highlighting the importance of resilience in this population [
8]. Arab et al. [
9] conducted a study on the effects of a distancing program on the sense of coherence in MS patients. The study highlights the relevance of resilience-promoting interventions in this population.
Additionally, Ploughman et al. [
10] investigated the impact of resilience on healthy aging in MS, suggesting the potential role of resilience in improving the overall well-being of people with MS. Broche-Pérez et al. [
11] investigated the mediating role of psychological resilience in the relationship between fear of relapse and quality of life in individuals with MS. The study highlights the significance of resilience in managing disease-related concerns. Furthermore, a study discovered that psychological resilience played a mediating role in the correlation between perceived neuropsychological impairment and quality of life in individuals with MS. This implies that interventions aimed at building resilience may have a positive impact on the psychological well-being and quality of life of those with MS [
12].
In summary, the literature provides evidence for studies that focus on resilience training and interventions tailored to people with MS. These studies suggest that interventions aimed at enhancing resilience have the potential to positively impact the well-being and quality of life of people with MS.
The study aimed to investigate the effects of an online self-directed training on enhancing personal resilience and reducing stress perception in individuals with MS. The training is designed to be easily incorporated into daily life, making these benefits accessible to a wider audience.
2. Materials and Methods
The Euro-FH Ethics Committee approved the study (EKEFH04/23), and all participants provided informed written consent. The study is a randomized controlled trial with three assessment points: baseline (T1), post-intervention (T2), and long-term (T3), conducted between March and July 2023.
A total sample size of n = 44 was determined using a priori paired sample power analysis (G*Power) with an effect size of d = 0.20, a-error = 0.05, and b-error = 0.95. The study recruited 94 people with MS from the Department of Neurology, Bundeswehrkrankenhaus Hamburg, and the German Multiple Sclerosis Society (DMSG). Patients at the Department of Neurology at Bundeswehrkrankenhaus Hamburg were personally contacted and informed about the study's procedure and purpose. Consent for data use was obtained from the internal data protection officer of the hospital. Additionally, the project was communicated to the regional associations of the DMSG via email, with a clear and transparent explanation of the aim and content of the study. The DMSG distributed the information to its members and advertised the study to those who were interested. All participants were randomly assigned to either the experimental or control group using an online randomization tool.
A total of 64 participants completed a 28-day resiliency training course. At T1, T2, and T3, all participants were required to complete two questionnaires. However, thirty participants did not complete all three questionnaires and were therefore excluded from the study. Of the remaining 64 participants who completed all three questionnaires, 30 were assigned to a waitlist control group, while 34 were assigned to an experimental group. The waitlist control group underwent the course immediately after T2.
It is based on established stress theories, such as Lazarus & Folkman [
13], and current research on resilience and the effects of online training [
14,
15,
16,
17,
18]. The course was created by a psychologist and mindfulness trainer. The course is designed to cultivate resilience and mindfulness in adult participants as they navigate daily life. The eligibility criteria excluded individuals with pre-existing mental health conditions. The experimental group received daily videos via email in the morning and evening. The morning videos included resilience learning nuggets, daily prompts, and relaxation exercises that progressed sequentially over several weeks. The evening videos encouraged participants to practice gratitude journaling and compassion to promote self-reflection and a positive attitude. Participants were instructed to spend a total of 20 minutes each day, with 15 minutes in the morning and five minutes in the evening. The first week of the course curriculum covered neuropsychological principles, stress management, and emotional regulation [
13,
19,
20]. The second week focused on solution orientation, coping strategies, and acceptance [
21,
22]. The third week focused on re-framing techniques to counteract irrational thoughts and promote self-regulation [
23,
24]. The final week aimed to foster relationships, with an emphasis on belonging, empathy, and self-efficacy [
25,
26]. The training aimed to enhance individuals' stress perception and resilience through daily engagement with tailored exercises and content. Participants evaluated their stress perception and resilience using a combined questionnaire comprising two assessments. The first assessment was the Resistance Orientation-Regeneration Orientation Scale (Re-Re Scale), developed by Otto and Linden [
27], which measures responses to stress through a 20-item questionnaire with two subscales. The Resistance Orientation subscale evaluates behaviours related to resilience and goal pursuit, while the Regeneration Orientation subscale measures tendencies towards self-care. The internal consistency of the scales was found to be strong, with Cronbach's alpha reliability analysis indicating α = .93 for the Resistance Orientation scale and α = .92 for the Regeneration Orientation scale.
The study employed Fliege et al.'s [
28] Perceived Stress Questionnaire (PSQ) as the second questionnaire. The PSQ evaluates an individual's subjective perception of stress and consists of 20 items divided into four subscales: 'worry', 'tension', 'joy', and 'demands'. Cronbach's alpha was calculated to be .86 for the total score of the PSQ.
A mixed factorial repeated measures analysis of variance (ANOVA) was conducted to examine differences over time. Outliers were removed as needed during the analysis. Violations of sphericity were addressed using the Greenhouse-Geisser correction for values less than 0.75 or the Huynh-Feldt correction for values greater than 0.75 [
29]. Levene's test was used to assess the assumption of homogeneity of variance. If the assumption of homogeneity of variance was met, we performed post hoc multiple comparison tests using Tukey's approach [
30]. If homogeneity was not found, we used Holm's method for post-hoc tests [
31]. To evaluate the internal consistency of the PSQ and Re-Re scores and their respective scales, we conducted a reliability analysis using Cronbach's alpha, following the interpretation recommendations provided by Vaske et al. [
32]. We set the significance level for the mixed factorial repeated measures ANOVA and its associated post hoc tests at 0.05, based on our a priori power analysis.
3. Results
The study involved an experimental group of 34 participants, with 74% of them being female (n=25) and 26% male (n=9). The mean age of this group was 49.1 years (SD = 11.139), ranging from 27 to 65 years. The waiting list control group comprised of 62% female (n=18) and 38% male (n=11) with a mean age of 49.31 (SD = 9.111) ranging from 30 to 67 years.
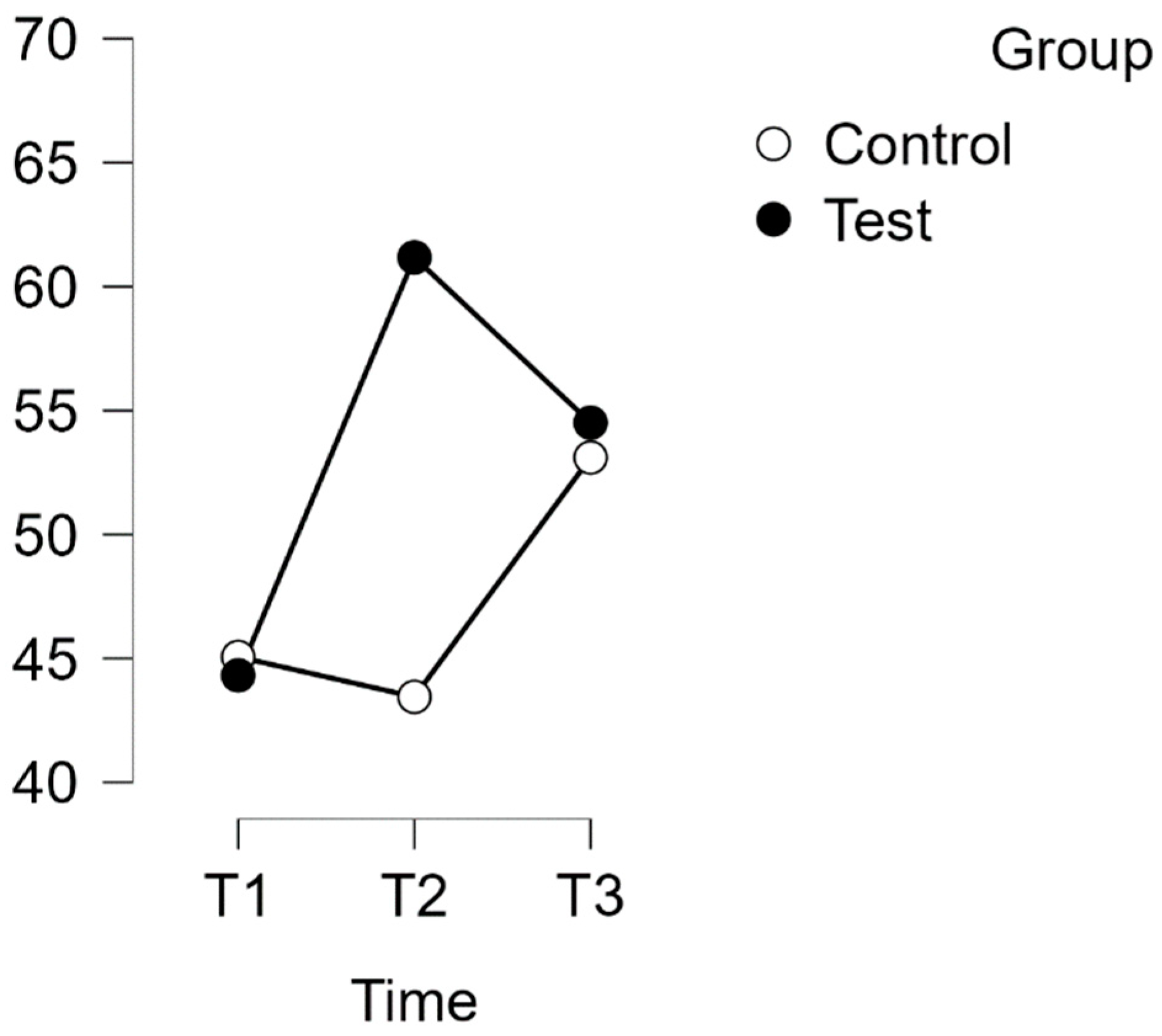
Both scales exhibited a normal distribution (p > 0.05), except for the control group T1 for the PSQ. Assuming homogeneity of variance on all scales, a repeated measures ANOVA with Huynh-Feldt correction revealed a significant interaction between time and group in relation to the PSQ score (F(1,854, 113,076) = 13,880, p < 0.001, η
2p = 0.185) as shown in Figures 2 and 3. Please refer to
Figure 1 for more details.
Post hoc analysis using Bonferroni correction supported implicit differences between the experimental and waitlist control groups over time. The intervention led to a significant improvement in scores (t(34) = -6.702, p < .001, MD = -18.822 points, 95% CI [-27.231, -10.413], d = 0.984) from T1 to T2, indicating a substantial effect. Additionally, there was a significant difference between T1 and T3, with a mean difference of -13.235 points, 95% CI [-21.644, -4.826], d = 0.692, t(34) = -4.712, p < .001.
However, there was no discernible difference between T1 (control) and T2 (control). After the waitlist control group completed the intervention, their scores showed a notable increase. The mean difference (MD) from T2 (control) to T3 (control) was -12.071 points, with a 95% confidence interval of -21.176 to -2.966, and d = -0.631. This resulted in a significant improvement in scores, t(29) = -3.969,
p = .002, indicating a substantial effect (
see Table 1).
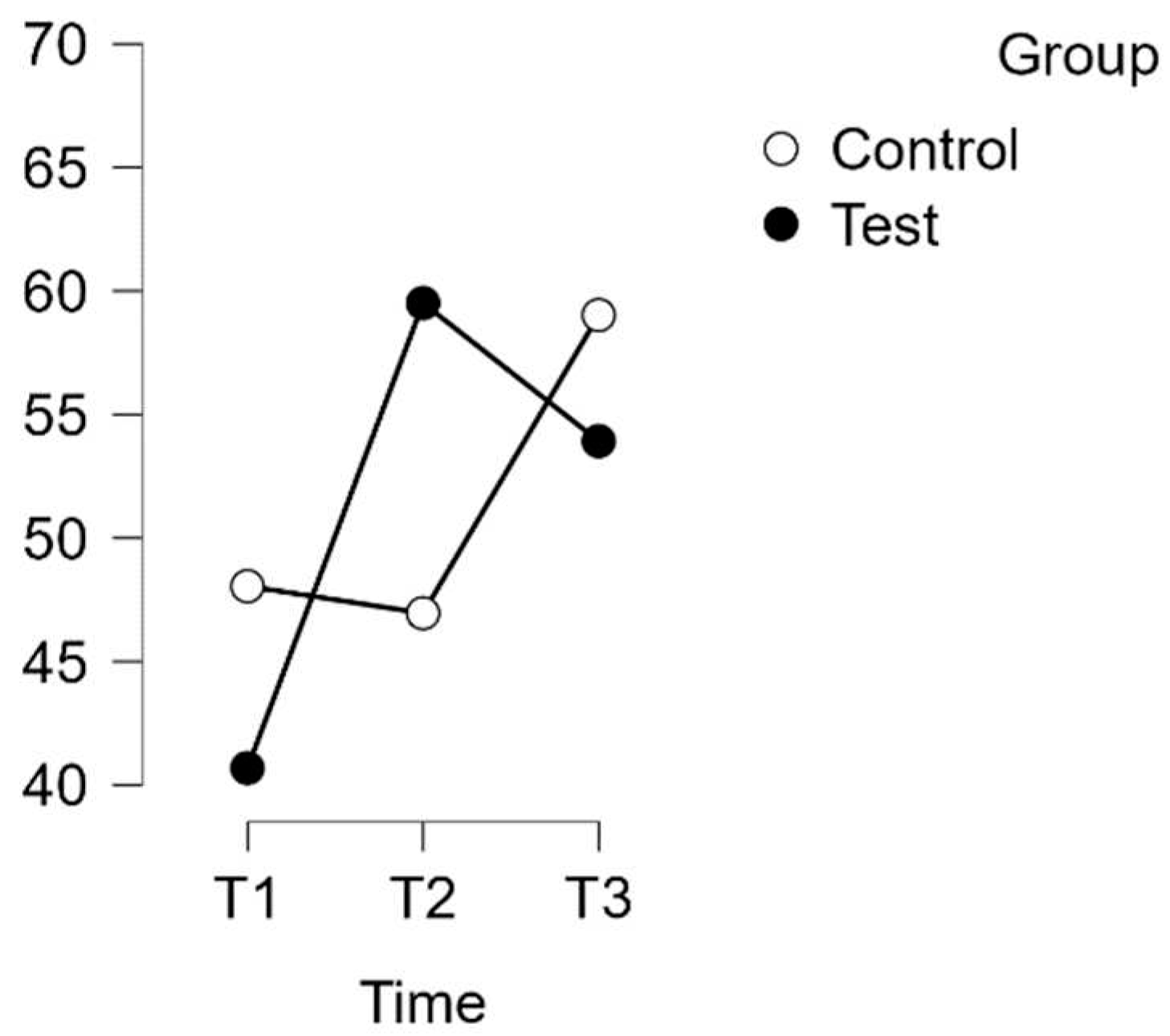
3.1. Subscale PSQ-Worries
A repeated measures analysis of variance (ANOVA) was conducted to investigate the relationship between time and group on the PSQ score for the Worries subscale, with a Huynh-Feldt correction applied. The results indicated a statistically significant interaction between time and group on the PSQ score (F(1.729, 241.168) = 13.880,
p = 0.003, η
2p = 0.099), as shown in
Figure 2.
Post hoc tests with Bonferroni correction revealed significant differences over time between the experimental and waitlist control groups. The intervention led to a significant increase in scores, with a mean difference of -17.843 points (95% CI [-28.328, -7.358], d = 0.740, t(34) = -5.095, p < .001) from T1 to T2. This effect size is considered large. Additionally, there was a significant difference between T1 and T3, with a mean difference of -11.764 points (95% CI [-22.249, -1.279], d = -0.488, t(34) = -3.359, p = .013).
No significant difference was observed between T1 (control) and T2 (control), or between T2 (control) and T3 (control).
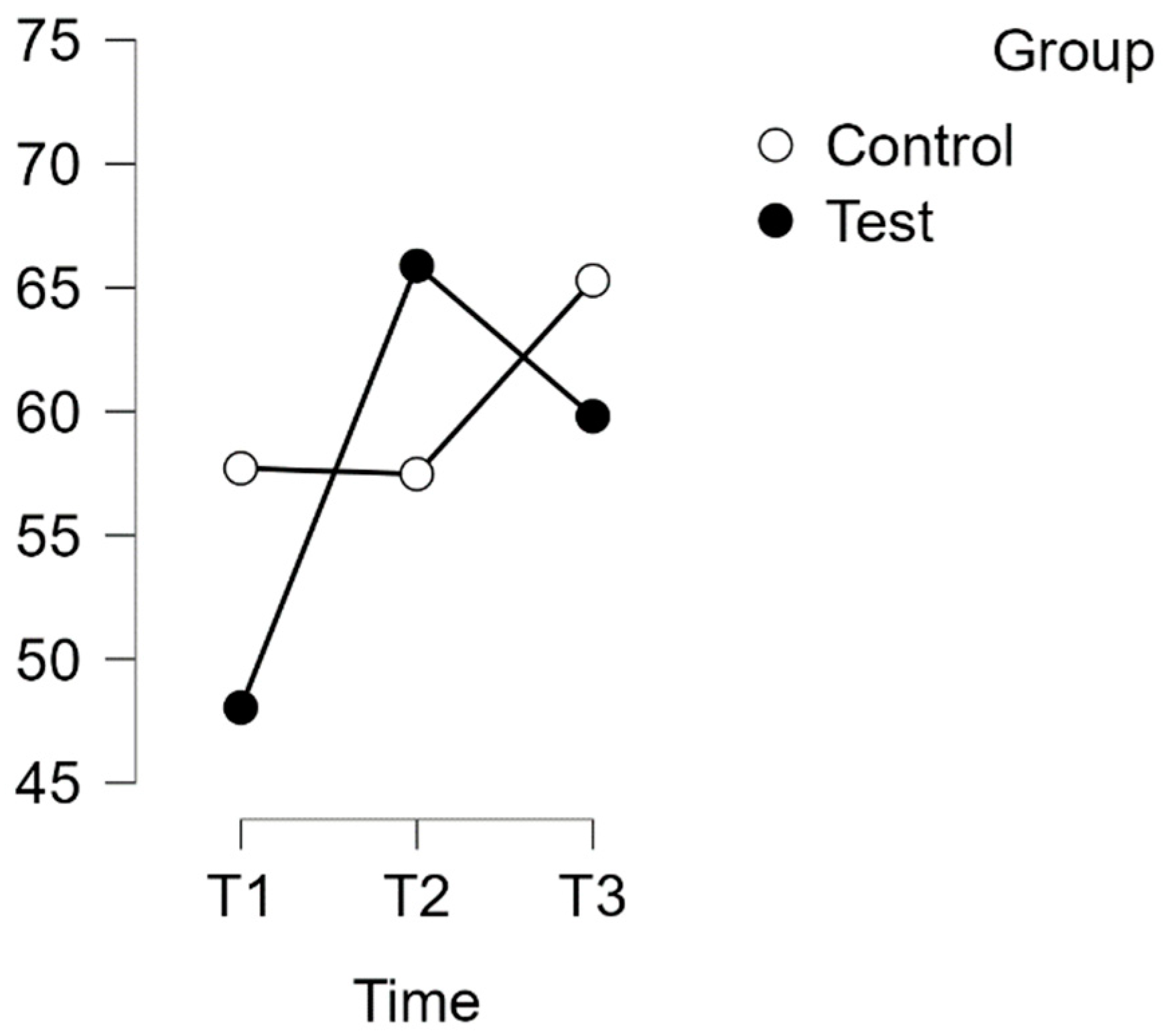
3.2. Subscale PSQ-Tension
A repeated measures analysis of variance (ANOVA) was conducted on the PSQ Tension subscale, with a Huynh-Feldt correction. The results showed a significant interaction between time and group on PSQ score [F(1.868, 113.924) = 12.774,
p = 0.001, η
2p = 0.173], as illustrated in
Figure 3.
Post hoc tests with Bonferroni correction revealed significant differences between the experimental and waitlist control groups over time. The intervention led to a significant increase in scores. The mean difference was -21.176 points (95% CI [-30.784, -11.567], d = -1.011) from T1(test) to T2(test), indicating a large effect size (t(34) = -6.599, p < .001). Additionally, there was a significant difference between T1(test) and T3(test), with a mean difference of -16.862 points (95% CI [-26.470, -7.254], d = -0.805, t(34) = -5.254, p < .001).
No significant difference was found between T1 (control) and T2 (control). However, a significant difference was found between T2 (control) and T3 (control) (t(29) = -4.102, p = .001). The mean difference (MD) was -14.254 points with a 95% confidence interval (CI) of [-24.658, -3.850], indicating a large effect size (d = -0.681).
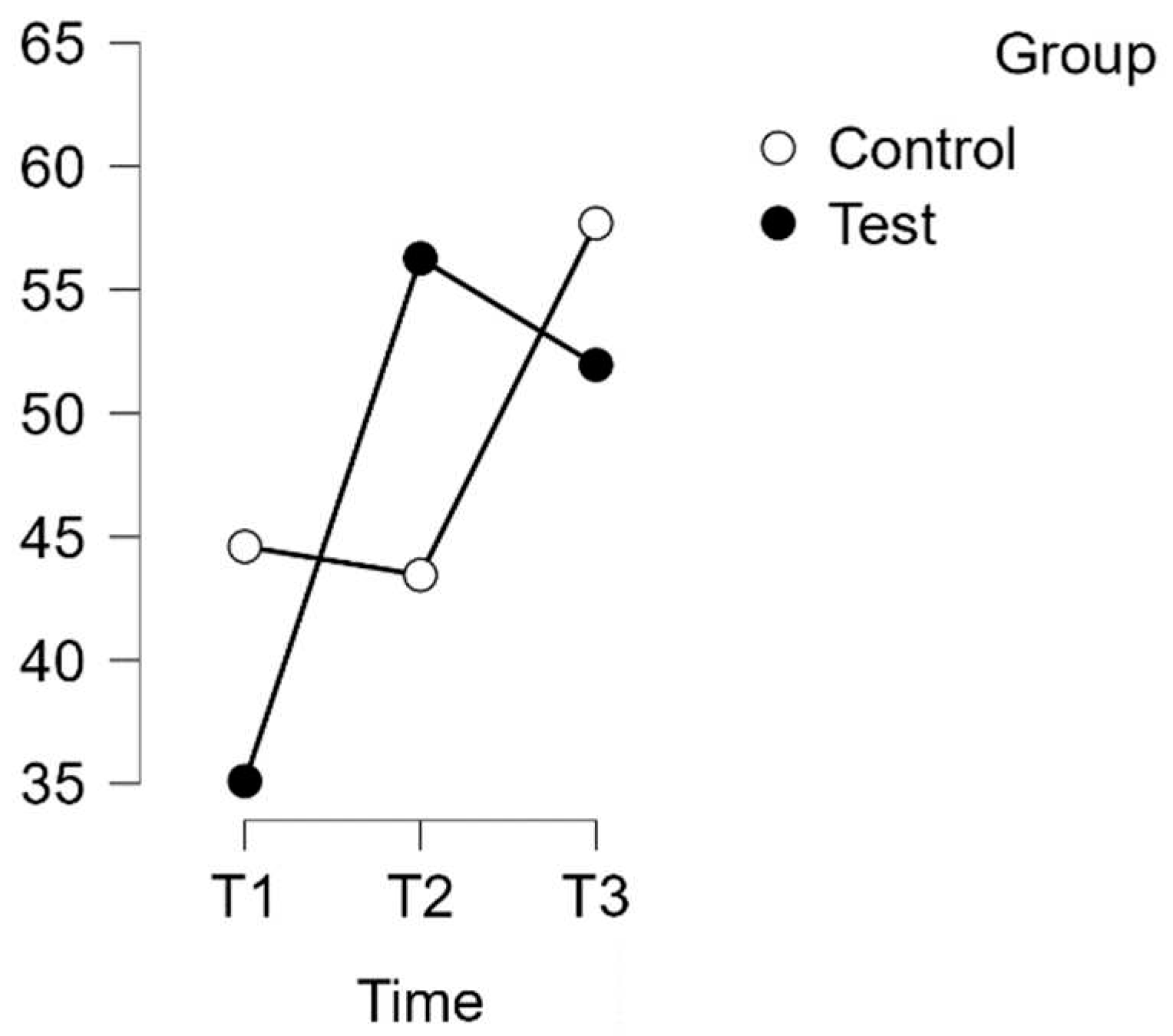
3.3. Subscale PSQ-Joy
A repeated measures analysis of variance (ANOVA) was conducted on the Joy subscale of the Perceived Stress Questionnaire (PSQ) with a Huynh-Feldt correction. The results revealed a significant interaction effect between time and group (F(1,996, 121,774) = 13,798, p < 0.001, η
2p = 0.184), as shown in
Figure 4.
Subsequent post hoc tests with Bonferroni correction confirmed time-related differences between the experimental and wait-list control groups. The intervention resulted in a significant improvement in scores (MD = -19.411 points, 95% CI [-28.939, -9.884], d = -0.920, t(34) = -6.100, p < .001), indicating a large effect size. Furthermore, there was a substantial difference between T1(test) and T3(test) (MD = -14.118 points, 95% CI [-23.645, -4.590], d = -0.669, t(34) = -4.436, p < .001).
There was no significant difference found between T1 (Control) and T2 (Control). However, T2 (Control) showed a significant difference from T3 (Control) (t(29) = -4.804, p < .001, MD = -16.552 points, 95% CI [-26.869, -6.236], d = -0.784), representing a large effect size.
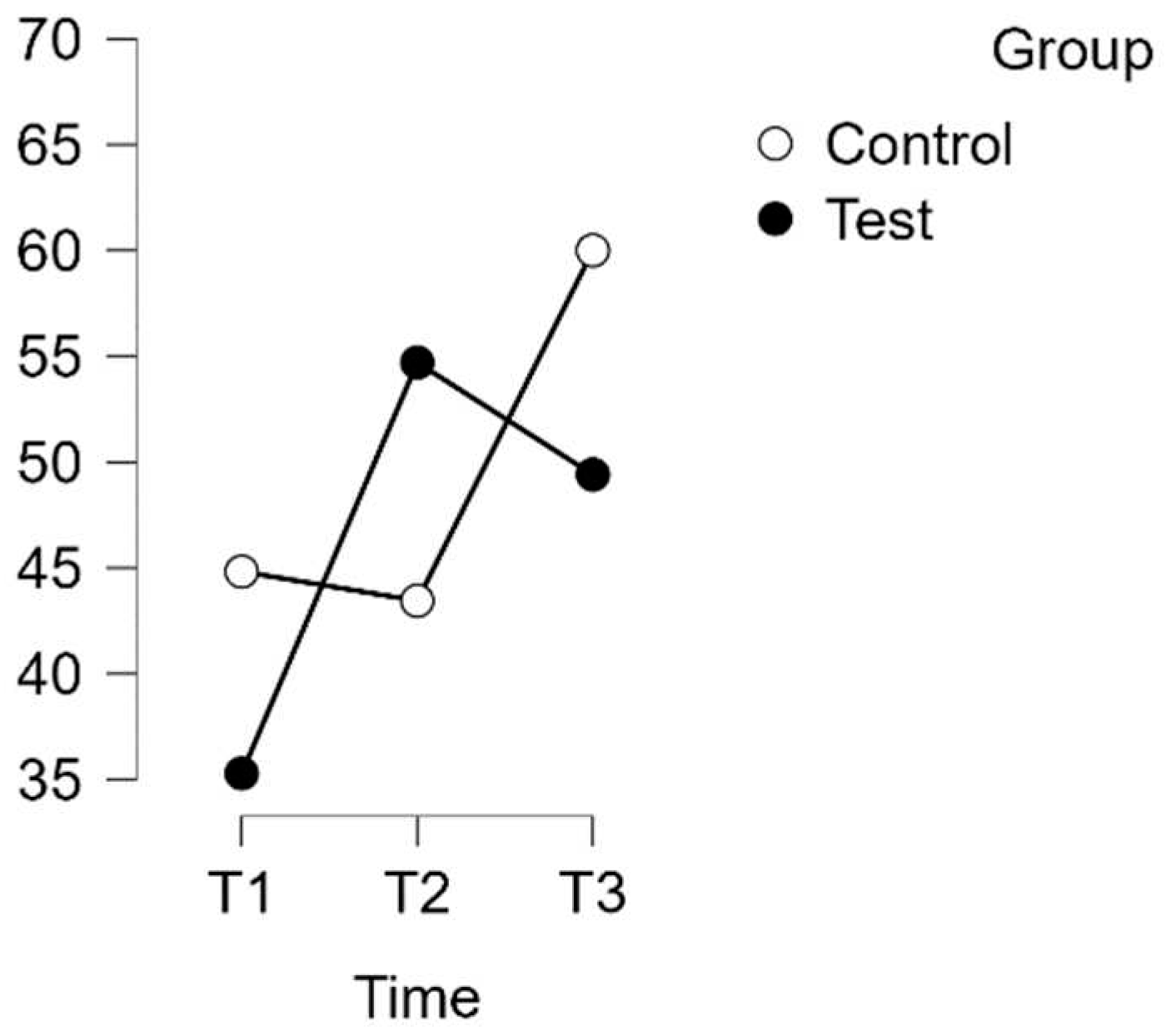
3.4. Subscale PSQ-Demands
A repeated measures analysis of variance (ANOVA) with a Huynh-Feldt correction was conducted on the PSQ Demands subscale. The results revealed a statistically significant interaction between time and group on the PSQ score [F(1,910,116,434) = 6,758,
p = 0.002, η
2p = 0.100], as shown in
Figure 5.
Bonferroni post hoc tests indicated significant differences between the experimental and waitlist control groups over time. The intervention led to a significant improvement in scores (mean difference = -16.864 points, 95% CI [-28.027, -5.700], d = -0.719, t(34) = -4.523, p < .001) from T1(Test) to T2(Test). However, there were no significant differences between T1(Test) and T3(Test), nor between T2(Control) and T3(Control).
3.5. Resistance Orientation-Regeneration Orientation Scale (Re-Re)
The scale comprises two subscales: Resistance and Regeneration. A repeated measures ANOVA for the Re-Re scale as a whole did not reveal any statistically significant interaction between time and group. However, the Resistance Orientation subscale demonstrated significant improvement, whereas the Resilience-Regeneration subscale did not.
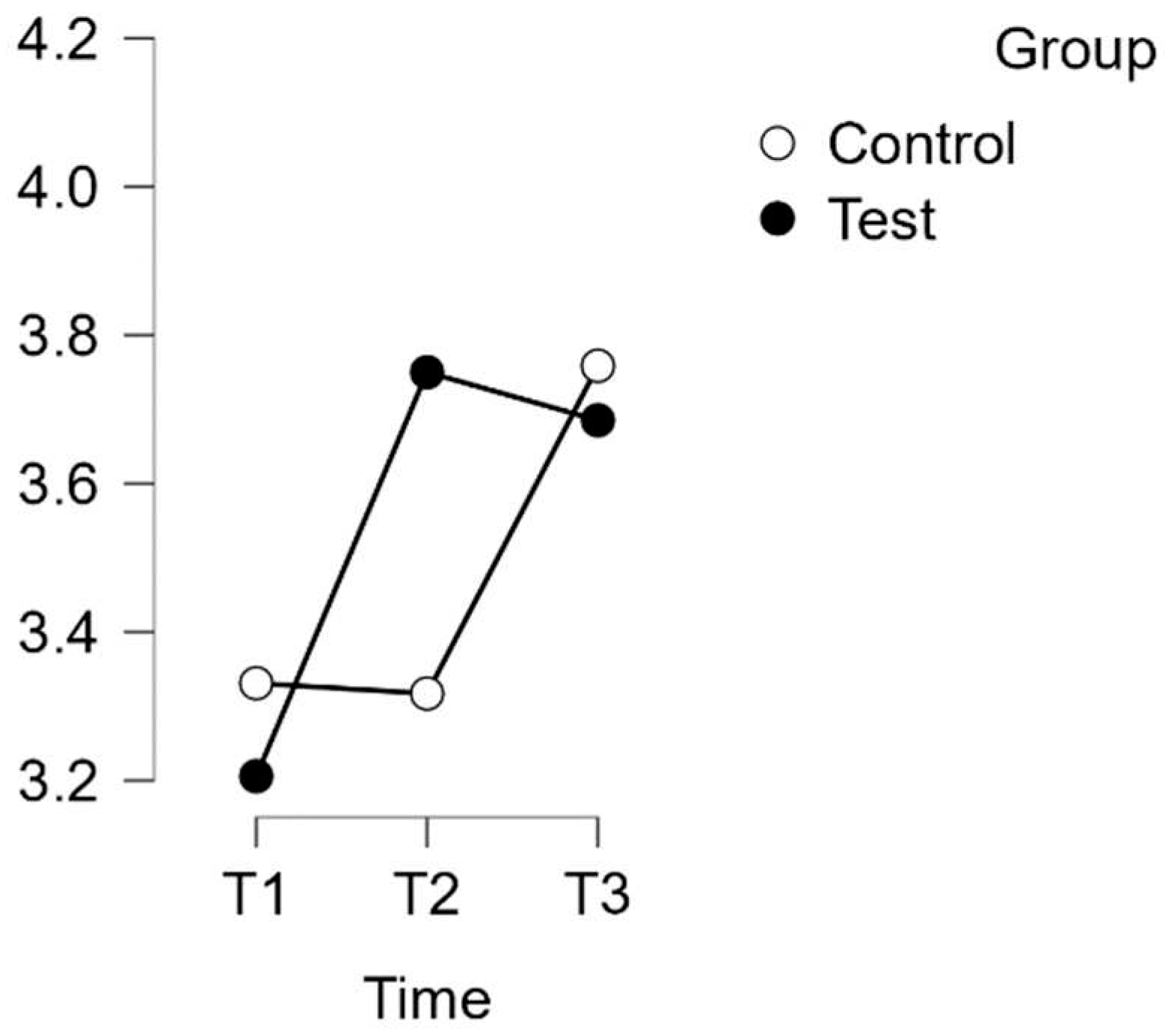
A repeated measures ANOVA with a Huynh-Feldt correction revealed a significant interaction between time and group on the PSQ score for the Re-Re subscale of Regeneration Orientation (F(1.817, 110.845) = 10.094,
p = 0.001, η
2p = 0.142). The results are presented in
Figure 6.
Furthermore, post hoc tests using the Bonferroni correction confirmed significant differences between the experimental test group and the waitlist control group over time. The intervention led to a significant increase in test scores, with a large effect size (d=-0.789), t(34)=-5.845, p <.001, and a mean difference (MD) of -0.544 points, 95% CI [-0.823, -0.265], between T1(test) and T2(test). Additionally, a significant difference was observed between T1(test) and T3(test) with a mean difference of -0.479 points, 95% CI [-0.758, -0.201], d=-0.695, t(34)=-5.150, p<.001.
No significant difference was found between the T1 and T2 control groups. However, the control group T3 exhibited a significant difference compared to T2. The mean difference (MD) was -0.441 points with a 95% confidence interval (CI) of [-0.743, -0.140]. This resulted in a t-value of -4.379 and p-value of less than .001. The effect size was considered medium with d = -0.640.
4. Discussion and Conclusion
The study results demonstrate a consistent improvement in various aspects of psychological well-being for the experimental group. The significant increase in all PSQ scales from T1 to T2 highlights the immediate positive effect of the intervention. Furthermore, the long-term improvement in the Worries, Joy, and Tension subscales suggests a sustained benefit in these key dimensions of psychosocial health. Although the Demands subscale did not demonstrate a sustained effect, the positive trend observed in other subscales suggests an overall positive impact.
The experimental group showed significant improvement on the Regeneration subscale in both the short and long term on the Re-Re scale, demonstrating the effectiveness of the intervention in promoting psychological recovery. However, the subscale measuring resilience did not show a significant improvement, and the overall Re-Re scale did not show a sustained effect. These nuanced findings suggest that although the intervention has positive effects in certain areas, its effects may vary across different domains of psychological well-being. Furthermore, the results suggest that certain aspects of resilience may require further attention or a different approach.
The findings of the current study are consistent with and contribute to the growing body of evidence supporting the importance of resilience in people with multiple sclerosis (MS). The study emphasizes the potential effectiveness of resilience-focused interventions for those facing the challenges of MS, as demonstrated in Al & Alqudah's (2023) review. Furthermore, this study reinforces the importance of resilience-building interventions in improving the well-being of people with MS, as supported by Arab et al.'s (2023) findings on the effects of a distancing programme on the sense of coherence in people with MS. Additionally, Ploughman et al. (2020) and Broche-Pérez et al. (2022a, 2022b) investigated the impact of resilience on healthy ageing in MS. The study's results demonstrate the positive impact of resilience-building interventions on the psychological well-being and overall quality of life of individuals with MS. These findings support the relevance of resilience-focused interventions and their potential to improve the well-being of those coping with MS challenges.
The study suggests that online self-directed interventions have the potential to improve resilience in people with MS, in addition to offering a promising opportunity to enhance their quality of life. Online self-directed training programmes are accessible and affordable, making them a practical tool to help individuals cope with the psychological barriers associated with the disease. The intervention has the potential to alleviate the psychological distress commonly experienced by people with MS, by providing a low-cost and easily accessible method of increasing resilience. This could contribute to their overall well-being and benefit a wide audience. The evidence presented in this paper suggests the need for further research and the development of targeted, self-directed online interventions to promote resilience in people with MS. This will ultimately contribute to the advancement of comprehensive care strategies for this population.
Author Contributions
Conceptualization, L. Bock; methodology, L. Westemeyer; software, L. Bock; validation, L. Bock, L. Westemeyer and Mrs. M. Rana.; formal analysis, L. Bock; investigation, L. Westemeyer; resources, L. Bock; data curation, L. Westemeyer; writing—original draft preparation, L. Bock; writing—review and editing, Mrs. M. Rana; visualization, L. Bock; supervision, Mrs. M. Rana; project administration, L. Bock; funding acquisition, Mr. M. Rana. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The Euro-FH Ethics Committee approved the study (EKEFH04/23).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available on request due to restrictions privacy. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to data protection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Walton, C., King, R., Rechtman, L., Kaye, W., Leray, E., Marrie, R. A., Robertson, N., La Rocca, N., Uitdehaag, B., van der Mei, I., Wallin, M., Helme, A., Angood Napier, C., Rijke, N., & Baneke, P. (2020). Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Multiple Sclerosis (Houndmills, Basingstoke, England), 26(14), 1816–1821. [CrossRef]
- Seaborn, K., Henderson, K., Gwizdka, J., & Chignell, M. (2022). A meta-review of psychological resilience during COVID-19. Npj Mental Health Research, 1(1). [CrossRef]
- Masten, A. S. (2007). Resilience in developing systems: Progress and promise as the fourth wave rises. Development and Psychopathology, 19(3), 921–930. [CrossRef]
- Selye, H., & Fortier, C. (1950). Adaptive reaction to stress. Psychosomatic Medicine, 12(3), 149–157. [CrossRef]
- Antonovsky, A. (1987). Unravelling the mystery of health: How people manage stress and stay well. Jossey-Bass.
- Werner, Emmy E., & Smith, R. S. (2001). Journeys from childhood to midlife: Risk, resilience, and recovery. Cornell University Press.
- Pakenham, K. I., Mawdsley, M., Brown, F. L., & Burton, N. W. (2018). Pilot evaluation of a resilience training program for people with multiple sclerosis. Rehabilitation Psychology, 63(1), 29–42. [CrossRef]
- Alsheikh Al, A. S., & Alqudah, A. (2023). Examine the role of psychological resilience in predicting social and professional performance in patients with diabetes, multiple sclerosis, and rheumatism. Health Psychology Research, 11. [CrossRef]
- Arab, F., Hekmatpou, D., & Saeedi, M. (2023). The effect of distance empowerment program on the sense of coherence among multiple sclerosis patients: a quasi-experimental study. In Research Square. [CrossRef]
- Ploughman, M., The Health, Lifestyle and Aging with MS Canadian Consortium, Downer, M. B., Pretty, R. W., Wallack, E. M., Amirkhanian, S., & Kirkland, M. C. (2020). The impact of resilience on healthy aging with multiple sclerosis. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 29(10), 2769–2779. [CrossRef]
- Broche-Pérez, Y., Jiménez-Morales, R. M., Monasterio-Ramos, L. O., & Bauer, J. (2022). Psychological resilience mediates the relationship between perceived neuropsychological impairment and quality of life in a sample of patients with multiple sclerosis. In bioRxiv. [CrossRef]
- Broche-Pérez, Y., Jiménez-Morales, R. M., Monasterio-Ramos, L. O., Vázquez-Gómez, L. A., Bauer, J., & Fernández-Fleites, Z. (2022). Fear of relapse and quality of life in multiple sclerosis: the mediating role of psychological resilience. In bioRxiv. [CrossRef]
- Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal, and Coping. Springer Publishing Company.
- Ang, W. H. D., Chew, H. S. J., Dong, J., Yi, H., Mahendren, R., & Lau, Y. (2022). Digital training for building resilience: Systematic review, meta‐analysis, and meta‐regression. Stress and Health: Journal of the International Society for the Investigation of Stress, 38(5), 848–869. [CrossRef]
- Assonov, D. (2021). Resilience-oriented interventions for patients with traumatic brain injury: Prototypes analysis and new program development. Ukrainian Scientific Medical Youth Journal, 124(2), 15–26. [CrossRef]
- Chmitorz, A., Kunzler, A., Helmreich, I., Tüscher, O., Kalisch, R., Kubiak, T., Wessa, M., & Lieb, K. (2018). Intervention studies to foster resilience – A systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review, 59, 78–100. [CrossRef]
- Díaz-García, A., Franke, M., Herrero, R., Ebert, D. D., & Botella, C. (2021). Theoretical adequacy, methodological quality and efficacy of online interventions targeting resilience: a systematic review and meta-analysis. European Journal of Public Health, 31(Supplement_1), i11–i18. [CrossRef]
- Fisher, D. M., & Law, R. D. (2021). How to choose a measure of resilience: An organizing framework for resilience measurement. Psychologie Appliquee [Applied Psychology], 70(2), 643–673. [CrossRef]
- Hoffman, R. (2004). The effect of acute stress on subsequent neuropsychological test performance (2003). Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists, 19(4), 497–506. [CrossRef]
- Thompson, R. A. (1991). Emotional regulation and emotional development. Educational Psychology Review, 3(4), 269–307. [CrossRef]
- Clark, K. K., Bormann, C. A., Cropanzano, R. S., & James, K. (1995). Validation evidence for three coping measures. Journal of Personality Assessment, 65(3), 434–455. [CrossRef]
-
Stress and coping in the time of COVID-19: Pathways to resilience and recovery. (2020, April 8). Clinical Neuropsychiatry | Journal of Treatment Evaluation; Giovanni Fioriti Editore Srl. [CrossRef]
- Ellis, A. (2023). Overcoming destructive beliefs, feelings, and behaviors: New directions for rational emotive behavior therapy. Prometheus Books.
- Vohs, K. D., & Baumeister, R. F. (Eds.). (2013). Handbook of self-regulation: Research, theory, and applications (2nd ed.). Guilford Publications.
- Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. [CrossRef]
- Gilbert, P., & Procter, S. (2006). Compassionate mind training for people with high shame and self‐criticism: overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy, 13, 353-379. [CrossRef]
- Otto, J., & Linden, M. (2018). ReRe-Skala - Resistenzorientierung-Regenerationsorientierungs-Skala. ZPID (Leibniz Institute for Psychology) - Open Test Archive. [CrossRef]
- Fliege, H., Rose, M., Arck, P., Levenstein, S., & Klapp, B. F. (2009). PSQ - Perceived Stress Questionnaire. ZPID (Leibniz Institute for Psychology) - Open Test Archive. [CrossRef]
- (N.d.). Statistical-Analysis-in-JASP-A-Students-Guide-V14-Nov2020.Pdf. Retrieved December 7, 2023, from http://Statistical-Analysis-in-JASP-A-Students-Guide-v14-Nov2020.pdf.
- Chen, T., Xu, M., Tu, J., Wang, H., & Niu, X. (2018). Relationship between Omnibus and Post-hoc Tests: An Investigation of performance of the F test in ANOVA. Psychiatry, 30, 60–64.
- Holm, K., & Christman, N. J. (1985). Post hoc tests following analysis of variance: POST HOC TESTS. Research in Nursing & Health, 8(2), 207–210. [CrossRef]
- Vaske, J. J., Beaman, J., & Sponarski, C. C. (2017). Rethinking internal consistency in cronbach’s alpha. Leisure Sciences, 39(2), 163–173. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).