Submitted:
27 December 2023
Posted:
28 December 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
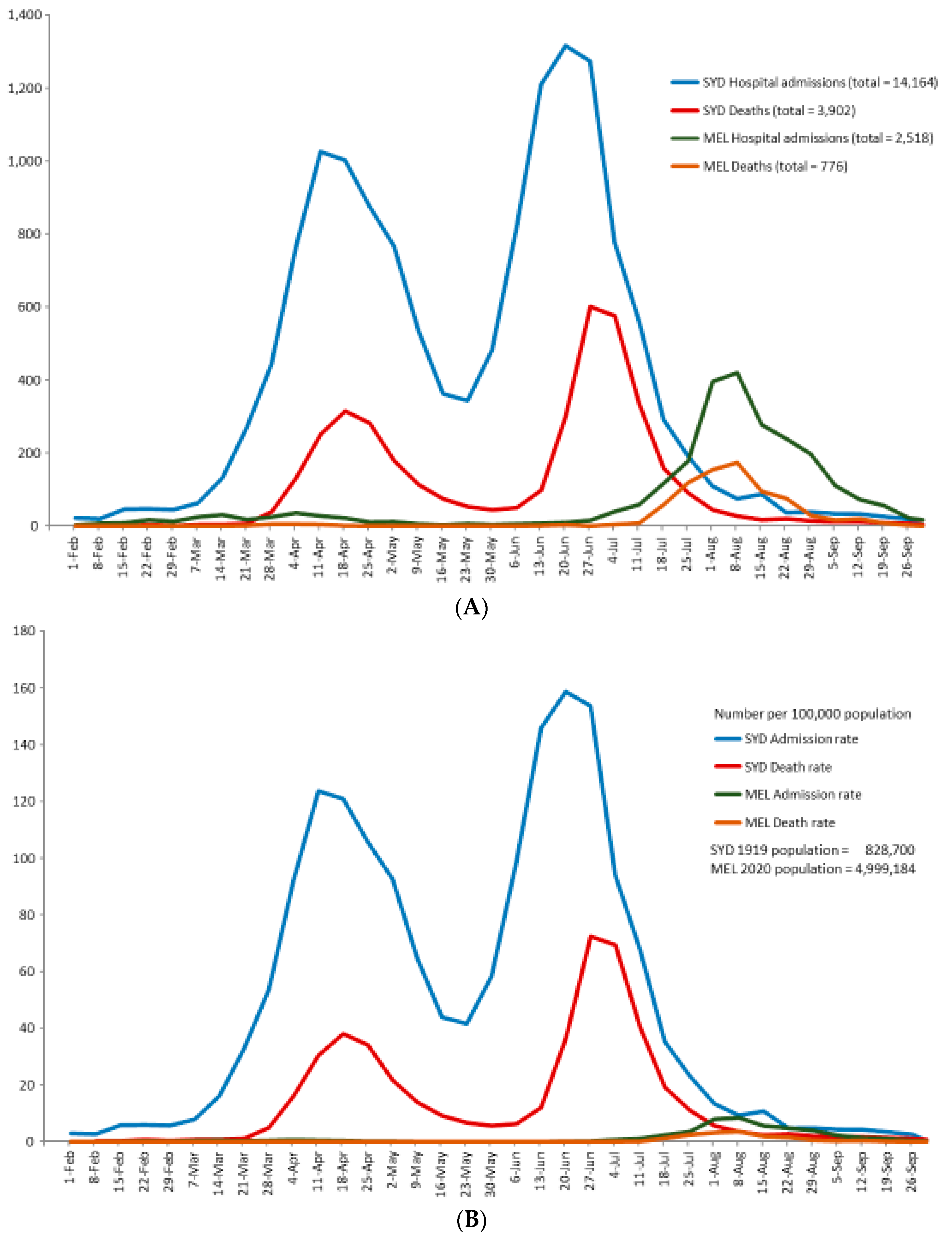
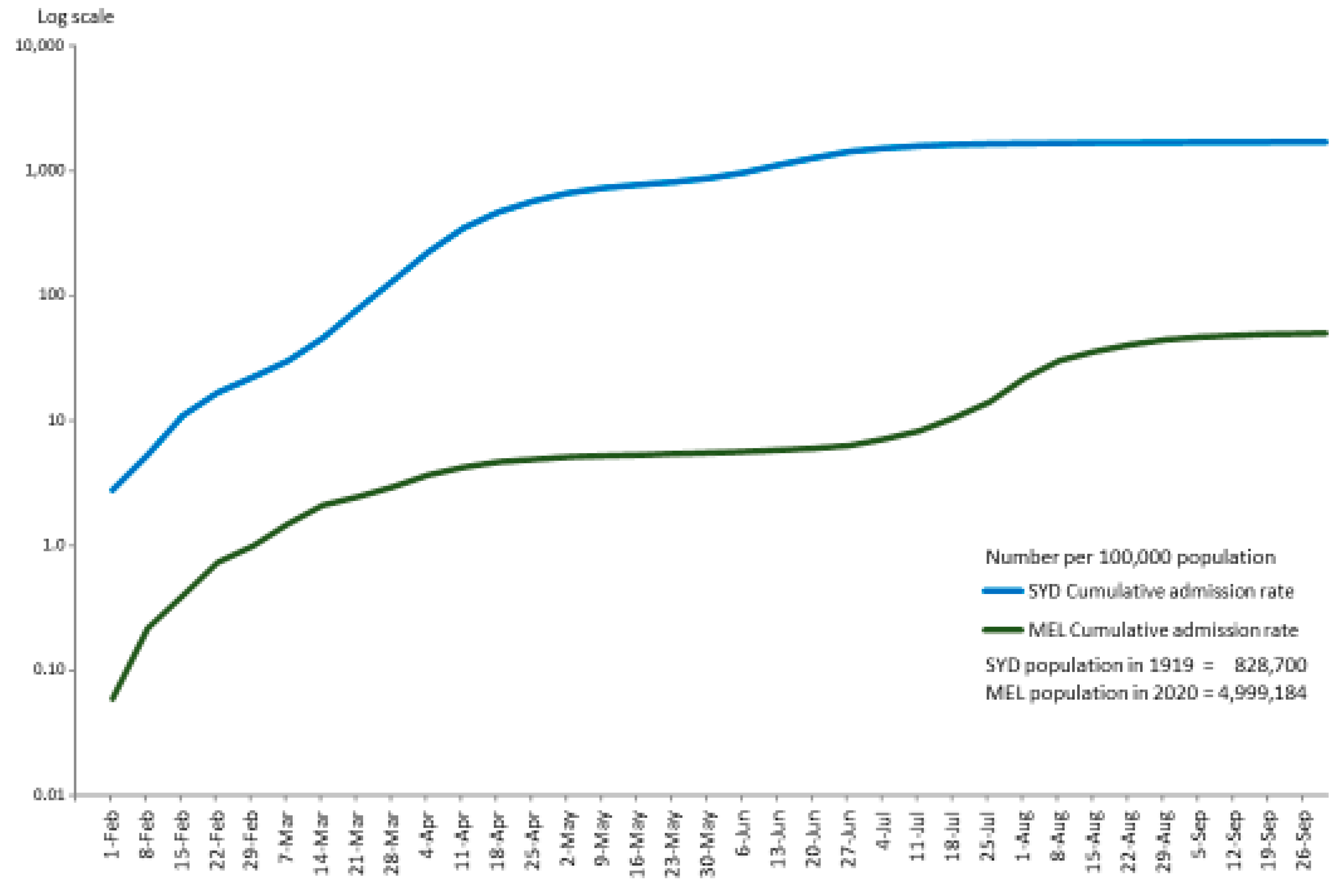
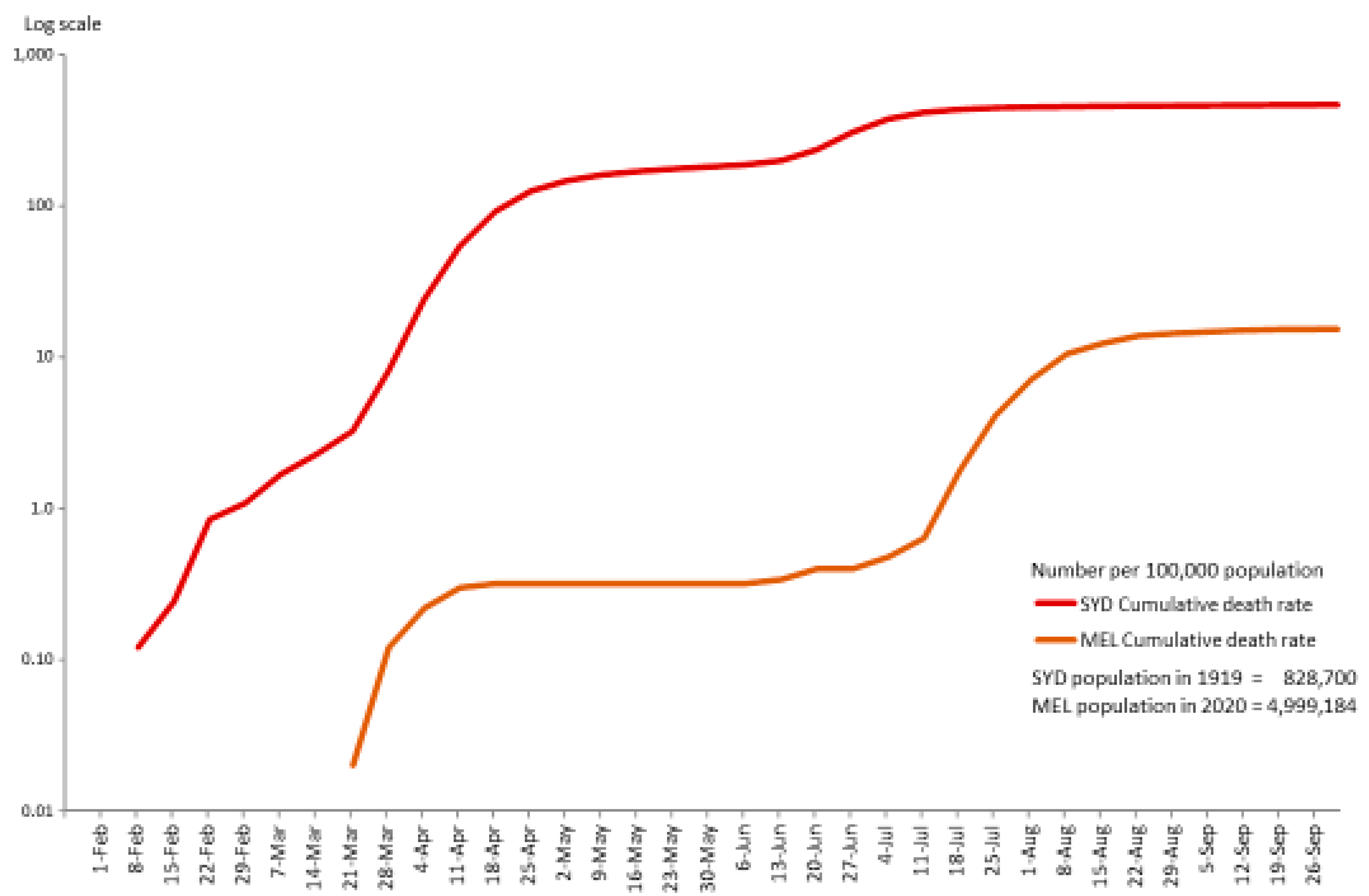
3.1. Crude Death Rates per 100,000 population in the epicentres of Sydney (1919) and Melbourne (2020)
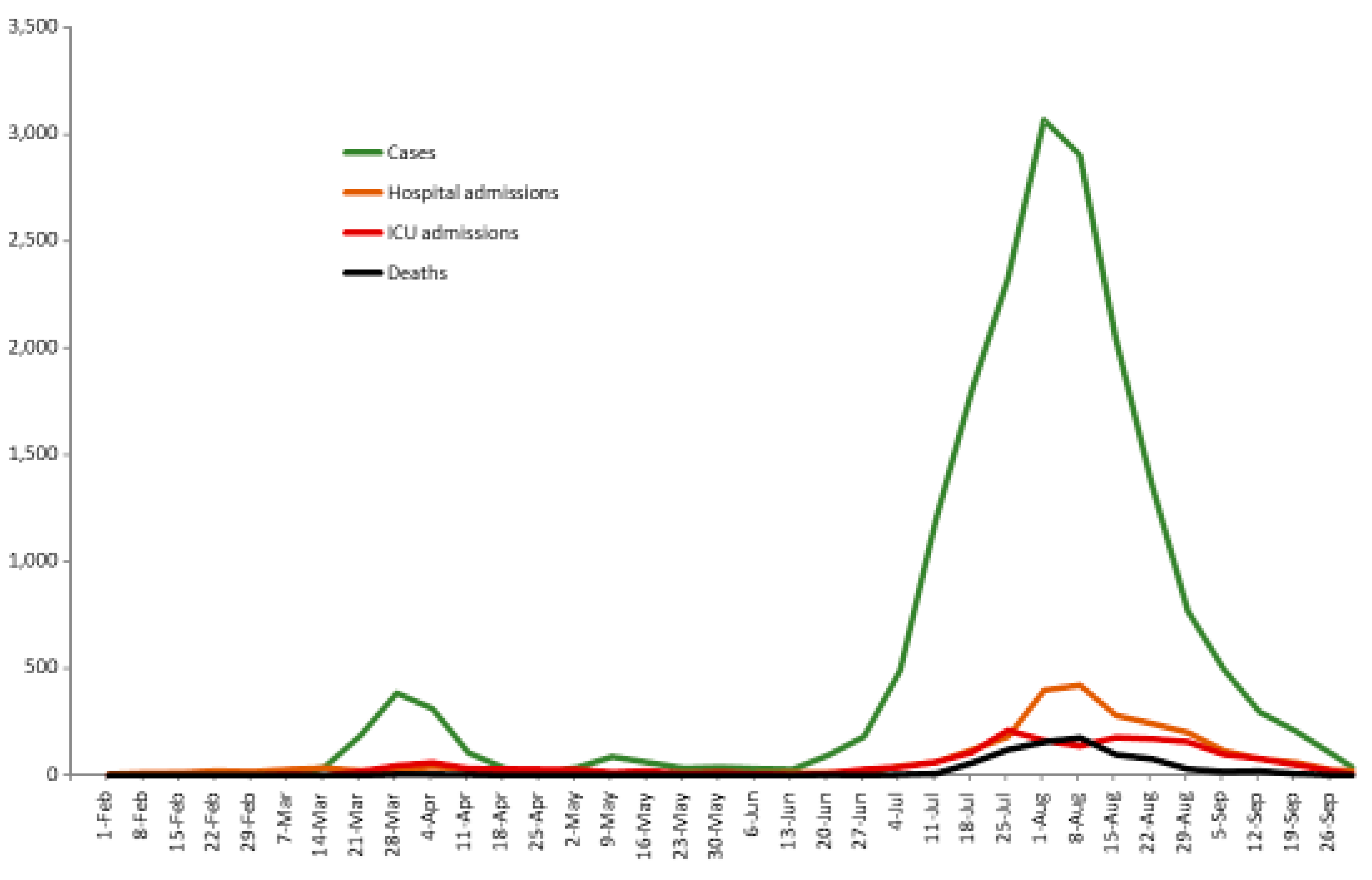
3.2. Contrasting patterns of hospitalisations as a proxy for infections
3.3. Contrasting patterns of death
3.4. Summary of the results
- The cumulative death rate per 100,000 from Spanish Flu in Sydney in 1919 was about 30 times higher than the death rate from COVID-19 in Melbourne in 2020.
- Per 100,000 the rate of infection in the general community in 1919 was about 87 times higher than in 2020.
- The cumulative hospital admission rate per 100,000 was 34 times higher in 1919 than in 2020.
- The weekly patterns of mortality in 1919 and 2020 were significantly different – Sydney experienced 11 weeks of triple-digit deaths in two distinctive waves compared with Melbourne’s single wave of only three weeks with triple-figure deaths. In other words, the greater lethality of the Spanish Flu in Sydney in 1919 was linked to the elevated levels of mortality in 1919 that were more persistent and lasted longer than was true of Melbourne in 2020.
- From the start of our study period in Melbourne up to 11 July 2020, there were 15 weeks when no deaths occurred (7 weeks in Stage 1 and 8 weeks in Stage 2) compared with the persistent increase in mortality from the start of the pandemic in Sydney. Up to the week ending 11 July there were only 32 cumulative deaths in Melbourne in 2020 compared with 3,477 in Sydney in 1919.
4. Discussion
4.1. The critical role of non-pharmaceutical interventions (NPIs) in 1919 and 2020
4.1.1. Protective sequestration as an NPI
4.1.2. Contemporary, scientific ‘protective sequestration’ via contact tracing and genomic sequencing
4.1.3. Cloth masks as NPIs
4.1.4. NPIs in Melbourne in 2020 and 2022
“If vaccine and antivirals are not effective, we have to resort to NPIs and we need to know this before the pandemic hits because NPI is costly and socially disruptive; so we need to have a plan and rationale for using them”.(9)
4.2. Transparency and data reliability were better in 2020 than in 2021-2022
5. Conclusion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walker, J. Chilling evidence of COVID-19’s potency. The Weekend Australian. 4 April 2020. Available at: www.theaustralian.com.au/science/coronavirus-is-just-as-lethal-as-spanish-flu-nobel-laureate-peter-doherty-warns/news-story/351d7fc88c012d7f4a4b2d1659f12942 (Accessed 18 October 2020).
- Utzet M, Benavides FG, Villar R, Burón A, Sala M, López L-E, et al. Non-Pharmacological Preventive Measures Had an Impact on COVID-19 in Healthcare Workers before the Vaccination Effect: A Cohort Study. Int J Environ Res Public Health (2022) 19(6):3628. [CrossRef]
- Young, S. Fauci Q&A: On masking, vaccines, and what keeps him up at night. WebMD Health News. 30 January 2023. Available at: https://www.medscape.com/viewarticle/987658?src=WNL_trdalrt_pos1_ous_230202&uac=398377DN&impID=5133523%20-%20vp_4 (Accessed 3 February 2023).
- Huf B, Mclean H. Epidemics and pandemics in Victoria: Historical perspectives. Melbourne, Victoria, Australia: Department of Parliamentary Services, Parliament of Victoria (2020). Available at: https://apo.org.au/sites/default/files/resource-files/2020-05/apo-nid303897.pdf (Accessed 1 April 2023).
- Piterman L, Vicziany M, Yang H. Questioning quarantine: There is a better way to do this: Medical Republic (2020). Available at: https://www.medicalrepublic.com.au/questioning-quarantine-there-is-a-better-way-to-do-this/33884 (Accessed 30 March 2023).
- McCracken K, Curson P. “Flu downunder: A demographic and geographic analysis of the 1919 epidemic in Sydney, Australia”. In: Killingray D, Oxford JS, Phillips H, Ranger T, editors. The Spanish Influenza Pandemic of 1918-1919: New Perspectives. 1st ed. London, UK: Routledge, Taylor and Francis Group (2003). p. 110-3.
- State Government of Victoria Department of Health and Human Services. Face coverings mandatory for Melbourne and Mitchell Shire. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.dhhs.vic.gov.au/updates/coronavirus-covid-19/face-coverings-mandatory-melbourne-and-mitchell-shire (Accessed 6 June 2023).
- State Government of Victoria Department of Health and Human Services. Statement from the Premier - 22 November 2020. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.dhhs.vic.gov.au/updates/coronavirus-covid-19/statement-premier-22-november-2020 (Accessed 6 June 2023).
- Markel H, Stern AM, Navarro JA, Michalsen JR. A historical assessment of nonpharmaceutical disease containment strategies employed by selected U.S. communities during the second wave of the 1918-1920 influenza pandemic: Final report. Defense Threat Reduction Agency, Advanced Systems and Concepts Office (2006). Available at: https://hdl.handle.net/2027/mdp.39015064102463 (Accessed 6 March 2023).
- Hobbins P, McWhinney G, Wishart A. An intimate pandemic: Creating community histories of the 1918–19 influenza pandemic. Sydney, NSW, Australia: Royal Australian Historical Society (2019). Available at: https://www.rahs.org.au/wp-content/uploads/2019/01/Research-guide-final-version.pdf (Accessed 8 February 2023).
- Commonwealth Government of Australia. Official Year Book, 1901-1919. Melbourne, Victoria, Australia: Commonwealth Government of Australia (1920). Available at: https://www.ausstats.abs.gov.au/ausstats/free.nsf/0/74934FD052EE5A3BCA257AEF001938FF/$File/13010_1901_1919_bk13.pdf (Accessed 7 August 2023).
- Smith, HA. “Part II.- Mortality statistics”. In: Report on the influenza epidemic in New South Wales in 1919. Report of Director-General of Public Health: NSW Department of Health (1920). p. 173-80. Available at: http://pandora.nla.gov.au/pan/83132/20080410-1521/influenza_report_full_36-44.pdf (Accessed 7 August 2023).
- Australian Bureau of Statistics (ABS). Victorian Year-Book 1919-20. Melbourne, Victoria, Australia: Australian Bureau of Statistics (1921). Available at: www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1301.21919-20?OpenDocument (Accessed 7 August 2023).
- Australian Bureau of Statistics (ABS). Australian Demographic Statistics, June 2019. Estimated resident population. Australian Bureau of Statistics (2019). Available at: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3101.0Main+Features1Jun%202019?OpenDocument (Accessed 7 August 2023).
- Australian Bureau of Statistics (ABS). Regional population, 2018-2019. Canberra, ACT, Australia: Australian Bureau of Statistics (2020). Available at: www.abs.gov.au/statistics/people/population/regional-population/2018-19 (Accessed 7 August 2023).
- Australian Government Department of Health. Coronavirus (COVID-19) at a glance – 31 December 2020. (2020). Available at: https://www.health.gov.au/resources/publications/coronavirus-covid-19-at-a-glance-31-december-2020 (Accessed 7 August 2023).
- Australian Institute of Health and Welfare. “The impact of a new disease: COVID-19 from 2020, 2021 and into 2022”. In: Australia’s health 2022: Data insights. catalogue number AUS 240, Australia’s health series number 18. Canberra, ACT, Australia AIHW, Australian Government (2022). p. 1-60. [CrossRef]
- Jordan, D. The deadliest flu: The complete story of the discovery and reconstruction of the 1918 pandemic virus: Centers for Disease Control and Prevention, US Department of Health and Human Services (2019). Available at: www.cdc.gov/flu/pandemic-resources/reconstruction-1918-virus.html (Accessed 17 June 2023).
- Armstrong, WG.; “Part I. - Epidemiology and Administration”. In: Report on the influenza epidemic in New South Wales in 1919. Report of Director-General of Public Health: NSW Department of Health (1920). p. 144-72. Available at: http://pandora.nla.gov.au/pan/83132/20080410-1521/influenza_report_full_6-35.pdf (Accessed 7 August 2023).
- State Government of Victoria Department of Health and Human Services. Public Health Events Surveillance System, Notifiable Conditions dataset for COVID-19 [Unpublished data received]. 1 October 2020.
- Australian Bureau of Statistics (ABS). A caring nation – 15 per cent of Australia’s workforce in Health Care and Social Assistance industry. Canberra, ACT, Australia: Australian Bureau of Statistics. 12 October 2022. Available at: https://www.abs.gov.au/media-centre/media-releases/caring-nation-15-cent-australias-workforce-health-care-and-social-assistance-industry (Accessed 12 July 2023).
- MacKinnon, K.; Healthcare worker infections dashboard. Analytics: Health Care Workers Australia (2021). Available at: https://healthcareworkersaustralia.com/analytics/ (Accessed 20 July 2023).
- State Government of Victoria Department of Health and Human Services. Victorian Healthcare Worker Coronavirus (COVID-19) Data, 30 September 2020. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.dhhs.vic.gov.au/victorian-healthcare-worker-covid-19-data (Accessed 30 September 2020).
- Buising KL, Williamson D, Cowie BC, MacLachlan J, Orr E, MacIsaac C, et al. A hospital-wide response to multiple outbreaks of COVID-19 in health care workers: lessons learned from the field. Med J Aust (2021) 214(3):101-4.e1. [CrossRef]
- Morens DM, Taubenberger JK. Understanding Influenza Backward. JAMA (2009) 302(6):679-80. [CrossRef]
- Taubenberger JK, Morens DM. Pandemic influenza—including a risk assessment of H5N1. Rev Sci Tech (2009) 28(1):187-202. [CrossRef]
- Short KR, Kedzierska K, Van de Sandt CE. Back to the future: Lessons learned from the 1918 influenza pandemic. Front Cell Infect Microbiol (2018) 8:343. [CrossRef]
- Lacombe K, Bhagani S. COVID-19 prevention strategies from real-world data. Medscape. 27 June 2023. Available at: https://reference.medscape.com/recap/989356 (Accessed 25 August 2023).
- Standl F, Jöckel K-H, Brune B, Schmidt B, Stang A. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis (2021) 21(4):e77. [CrossRef]
- Zhao LP, Lybrand TP, Gilbert PB, Payne TH, Pyo C-W, Geraghty DE, et al. Rapidly identifying new coronavirus mutations of potential concern in the Omicron variant using an unsupervised learning strategy. Sci Rep (2022) 12(1):19089. 1908. [CrossRef]
- State Government of Victoria Department of Health. Chief Health Officer Update - 12 May 2023. Melbourne, Victoria, Australia: State Government of Victoria (2023). Available at: https://www.health.vic.gov.au/media-releases/chief-health-officer-update-12-may-2023 (Accessed 1 June 2023).
- Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis (2020) 20(9):e238-e44. [CrossRef]
- Nuzum JW, Pilot I, Stangl FH, Bonar BE. Pandemic influenza and pneumonia in a large civil hospital. JAMA (1918) 71(19):1562-5. [CrossRef]
- Tumpey TM, Basler CF, Aguilar PV, Zeng H, Solórzano A, Swayne DE, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science (2005) 310(5745):77-80. [CrossRef]
- Hyslop, A. “Forewarned, forearmed: Australia and the Spanish influenza pandemic, 1918–1919”. In: Lack J, editor. 1919: The Year Things Fell Apart? Melbourne, Victoria, Australia: Australian Scholarly Publishing (2019). p. 31-4.
- McQueen, H.; “The ‘Spanish’ Influenza Pandemic in Australia, 1912-19”. In: Roe J, editor. Social Policy in Australia - Some Perspectives 1901-1975. Stanmore, NSW, Australia: Cassell Australia (1976). p. 131-48. Available at: https://labourhistorycanberra.org/2018/06/the-spanish-influenza-pandemic-in-australia-1912-19/ (Accessed 7 February 2023).
- Bootsma MCJ, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci U S A (2007) 104(18):7588-93. [CrossRef]
- Markel H, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA (2007) 298(6):644-54. [CrossRef]
- Campbell K, Vines E. COVID-19: A chronology of Australian Government announcements (up until 30 June 2020). Parliamentary Library Research Paper Series (2021). Available at: https://parlinfo.aph.gov.au/parlInfo/download/library/prspub/8027137/upload_binary/8027137.pdf (Accessed 26 March 2023).
- MacIntyre, R. “Jurassic Park for viruses”. In: Dark Winter. An insider’s guide to pandemics and biosecurity. Sydney, NSW, Australia: UNSW Press (2022). p. 65-80.
- COVID-19 Hotel Quarantine Inquiry. Final Report and Recommendations. Volume 2, Chapter 9 (2020). Available at: https://content.royalcommission.vic.gov.au/sites/default/files/2020-12/0387_RC_Covid-19%20Final%20Report_Volume%201%2B2_Digital.pdf (Accessed 1 March 2023).
- Haire B, Gilbert GL, Kaldor JM, Hendrickx D, Dawson A, Williams JH. Experiences of risk in Australian hotel quarantine: a qualitative study. BMC Public Health (2022) 22(1):953. [CrossRef]
- Fowler M, Booker C. Anger at hard lockdown for towers without confirmed virus cases. The Age. 5 July 2020. Available at: https://www.theage.com.au/national/victoria/covid-public-housing-wrap-20200705-p5596z.html (Accessed 28 June 2023).
- Kelaita P, Pienaar K, Keaney J, Murphy D, Vally H, Bennett CM. Pandemic policing and the construction of publics: an analysis of COVID-19 lockdowns in public housing. Health Sociol Rev (2023):1-16. [CrossRef]
- Parliament of Victoria Public Accounts and Estimates Committee. Inquiry into the Victorian Government’s response to the COVID-19 pandemic. Findings and recommendations. Melbourne, Victoria, Australia: Victorian Government Printer (2021). p. xxiii-xlvii. Available at: https://new.parliament.vic.gov.au/49706e/contentassets/9c4e489fe9834121826347ad523e87d2/paec_59-08_vic_gov_response_to_covid-19_pandemic.pdf (Accessed 28 June 2023).
- Wikipedia contributors. COVID-19 lockdowns: Wikipedia, The Free Encyclopedia (2023). Available at: https://en.wikipedia.org/w/index.php?title=COVID-19_lockdowns&oldid=1146756105 (Accessed 4 April 2023).
- Fair Work Commission. Information note – COVID-19 situation update 28 September 2020. COVID-19 information notes and updates. Canberra, ACT, Australia: Commonwealth of Australia (2020). Available at: https://www.fwc.gov.au/documents/resources/covid-19-information/information-note-covid-19-situation-update-2020-09-28.pdf (Accessed 2 June 2023).
- Kelly, L.; Melbourne to ease world’s longest COVID-19 lockdowns as vaccinations rise. Reuters. 17 October 2021. Available at: https://www.reuters.com/world/asia-pacific/melbourne-ease-worlds-longest-covid-19-lockdowns-vaccinations-rise-2021-10-17/ (Accessed 3 February 2023).
- State Government of Victoria Department of Health and Human Services. Coronavirus update for Victoria - 1 August 2020. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.dhhs.vic.gov.au/coronavirus-update-victoria-1-august-2020 (Accessed 9 July 2023).
- COVID-19 Hotel Quarantine Inquiry. Final Report and Recommendations. Volume 1, Chapter 2 (2020). Available at: https://content.royalcommission.vic.gov.au/sites/default/files/2020-12/0387_RC_Covid-19%20Final%20Report_Volume%201%2B2_Digital.pdf (Accessed 1 March 2023).
- Parliament of Victoria Legislative Council Legal and Social Issues Committee. Inquiry into the Victorian Government’s COVID–19 contact tracing system and testing regime. Melbourne, Victoria, Australia: Victorian Government (2020). Available at: https://www.parliament.vic.gov.au/images/stories/committees/SCLSI/Inquiry_into_the_Victorian_Governments_COVID19_Contact_Tracing_System_and_Testing_Regime_/report/LCLSIC_59-05_Vic_Gov_COVID-19_contact_tracing_testing.pdf (Accessed 18 February 2023).
- State Government of Victoria. Wastewater testing. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.coronavirus.vic.gov.au/wastewater-testing (Accessed 19 February 2023).
- Breadon P, Fox L, Emslie O. The Australian Centre for Disease Control (ACDC): Highway to Health. Melbourne, Victoria, Australia: Grattan Institute (2023). Available at: https://grattan.edu.au/report/acdc-highway-to-health/ (Accessed 13 February 2023).
- Blau A, Martino M. Coronavirus could flood our hospital ICUs with COVID-19 patients, so do we have enough beds? ABC News. 27 March 2020. Available at: https://www.abc.net.au/news/2020-03-27/coronavirus-australia-covid-19-icu-beds-ventilators-hospitals/12090420 (Accessed 17 June 2023).
- ABC News. Victorian elective surgeries suspended as coronavirus cases grow by 384 with six more deaths. ABC News. 28 July 2020. Available at: www.abc.net.au/news/2020-07-28/coronavirus-case-numbers-victoria-rise-384-with-six-new-deaths/12498024 (Accessed 17 June 2023).
- Mingyu L, Shelan L, Liebo Z, Fengying W, Kunyang W, Hanqing H, et al. Analysis of a super-transmission of SARS-CoV-2 omicron variant BA. 5.2 in the outdoor night market. Front Public Health (2023) 11:1153303. 3303. [CrossRef]
- Kellogg WH, MacMillan G. An experimental study of the efficacy of gauze face masks. Am J Public Health (1920) 10(1):34-42. [CrossRef]
- Lurie MB, Abramson S. The efficiency of gauze masks in the protection of rabbits against the inhalation of droplet nuclei of tubercle bacilli. Am Rev Tuberc (1949) 59(1):1-9. [CrossRef]
- Clase CM, Fu EL, Ashur A, Beale RCL, Clase IA, Dolovich MB, et al. Forgotten Technology in the COVID-19 Pandemic: Filtration Properties of Cloth and Cloth Masks—A Narrative Review. Mayo Clin Proc (2020) 95(10):2204-24. 2204. [CrossRef]
- Clase C, Fu E, Carrero JJ. COVID-19 masks FAQs: How can cloth stop a tiny virus? What’s the best fabric? Do they protect the wearer? The Conversation. 12 October 2020. Available at: https://theconversation.com/covid-19-masks-faqs-how-can-cloth-stop-a-tiny-virus-whats-the-best-fabric-do-they-protect-the-wearer-146822 (Accessed 7 March 2023).
- Saxena SK, Kotikalapudi R, Tiwari S, Muvva C. Influenza A(H1N1)pdm09 virus: Therapeutics and challenges. Future Virology (2012) 7(10):947-50. [CrossRef]
- Verma S, Dhanak M, Frankenfield J. Visualizing the effectiveness of face masks in obstructing respiratory jets. Phys Fluids (2020) 32(6):061708. [CrossRef]
- L’Orange, C.; What’s the best mask for COVID-19? A mechanical engineer explains the science after two years of testing in his lab. The Conversation (2022). Available at: https://theconversation.com/what-is-the-best-mask-for-covid-19-a-mechanical-engineer-explains-the-science-after-2-years-of-testing-masks-in-his-lab-175481 (Accessed 15 February 2023).
- MacIntyre, R. “The fuss about facemasks”. In: Dark Winter. An insider’s guide to pandemics and biosecurity. Sydney, NSW, Australia: UNSW Press (2022). p. 170-88.
- World Bank. Poverty and Shared Prosperity 2022: Correcting Course. Washington, DC, USA: World Bank (2022). [CrossRef]
- Lei H, Xu M, Wang X, Xie Y, Du X, Chen T, et al. Nonpharmaceutical interventions used to control COVID-19 reduced seasonal influenza transmission in China. J Infect Dis (2020) 222(11):1780-3. [CrossRef]
- State Government of Victoria Department of Health and Human Services. Victorian Weekly Influenza Report Week ending: 8 August 2020. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://content.health.vic.gov.au/sites/default/files/migrated/files/collections/research-and-reports/s/seasonal-influenza-reports/2020/2020-weekly-influenza-surveillance-report-week-ending-8-august.pdf (Accessed 13 February 2023).
- Australian Government Department of Health and Aged Care. Australian Influenza Surveillance Report, No 14, 9 October, Reporting fortnight: 26 September to 09 October 2022. Canberra, ACT, Australia: Government of Australia, (2022). Available at: https://www.health.gov.au/sites/default/files/documents/2022/10/aisr-fortnightly-report-no-14-26-september-to-9-october-2022.pdf (Accessed 22 March 2023).
- Trent MJ, Moa A, MacIntyre CR. “I’ll be back”: Australia’s experience of flu in 2022. BMJ (2022) 379:o2998. [CrossRef]
- Morawska L, Milton DK. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clin Infect Dis (2020) 71(9):2311-3. [CrossRef]
- Australian Bureau of Statistics (ABS). COVID-19 Mortality in Australia: Deaths registered until 28 February 2023. Australian Bureau of Statistics (2023). Available at: https://www.abs.gov.au/articles/covid-19-mortality-australia-deaths-registered-until-28-february-2023 (Accessed 15 June 2023).
- COVID-19 Actuaries Institute Mortality Working Group. COVID-19 Mortality Working Group Confirmation of 20,000 excess deaths for 2022 in Australia (2023). Available at: https://www.actuaries.digital/2023/04/06/covid-19-mortality-working-group-confirmation-of-20000-excess-deaths-for-2022-in-australia/ (Accessed 15 June 2023).
- Mullins A, host. The scientific reality of COVID-19 for all Australians. Uncommon Sense Podcast. 6 December 2022. Available at: https://www.rrr.org.au/explore/podcasts/uncommon-sense/episodes/6333-professor-brendan-crabb-on-the-scientific-reality-of-covid-19-for-all-australians (Accessed 13 February 2023).
- Burnet Institute. COVID isolation rule change ‘disappointing’. Burnet Institute News. Melbourne, Victoria, Australia: Burnet Institute (2022). Available at: https://burnet.edu.au/news/1677_covid_isolation_rule_change_disappointing (Accessed 13 February 2023).
- Office of the Prime Minister of Australia. Media Release on National Cabinet Meeting of 30 September 2022: COVID-19. Canberra, ACT, Australia: Commonwealth Government of Australia. 30 September 2022. Available at: https://www.pm.gov.au/media/meeting-national-cabinet-1 (Accessed 13 February 2023).
- Grafton RQ, Chu L, Kompas T, McLaws M-L, Suan D. Long COVID in Australia: Evidence and Key Findings, Inquiry into Long COVID and Repeated COVID Infections. Inquiry into Long COVID and Repeated COVID Infections. Submission 208: Australian Parliament House (2022). Available at: https://www.aph.gov.au/DocumentStore.ashx?id=17f15f1d-a2f0-4fae-bd9d-85a0918ee6ac&subId=725489 (Accessed 26 January 2023).
- Biddle N, Korda R. The experience of COVID-19 in Australia, including long-COVID – Evidence from the COVID-19 Impact Monitoring Survey Series. Centre for Social Research & Methods, ANU College of Arts & Social Sciences, Australian National University, (2022). Available at: https://csrm.cass.anu.edu.au/research/publications/experience-covid-19-australia-including-long-covid-evidence-covid-19-impact (Accessed 28 January 2023).
- Altmann DM, Whettlock EM, Liu S, Arachchillage DJ, Boyton RJ. The immunology of long COVID. Nat Rev Immunol (2023). [CrossRef]
- Rong Z, Mai H, Kapoor S, Puelles V, Czogalla J, Schädler J, et al. SARS-CoV-2 spike protein accumulation in the skull-meninges-brain axis: Potential implications for long-term neurological complications in post-COVID-19. bioRxiv (2023):2023.04.04.535604. [CrossRef]
- Hyndman, RJ. We need more open data in Australia (2022). Available at: https://robjhyndman.com/hyndsight/open-data.html (Accessed 1 March 2023).
- Briggs, C.; Australian governments have kept much of their COVID research and modelling secret. Why? ABC News. 7 January 2023. Available at: https://www.abc.net.au/news/2023-01-07/covid-data-government-secrecy/101827548 (Accessed 29 January 2023).
- MacIntyre, R. “Trust me, I’m a doctor”. In: Dark Winter. An insider’s guide to pandemics and biosecurity. Sydney, NSW, Australia: UNSW Press (2022). p. 138-51.
- MacIntyre, R. “Information warfare”. In: Dark Winter. An insider’s guide to pandemics and biosecurity. Sydney, NSW, Australia: UNSW Press (2022). p. 117-37.
- Mullins A, host. Listen to Epidemiologist Mary-Louise McLaws on how to fix Australia’s vaccine rollout. Uncommon Sense Podcast. 20 April 2021. Available at: https://www.rrr.org.au/explore/podcasts/uncommon-sense/episodes/5107-epidemiologist-mary-louise-mclaws-on-how-to-fix-australias-vaccine-rollout-wild-mushrooming-with-alison-pouliot-the-rediscovery-of-a-rare-cloaked-bee (Accessed 2 July 2023).
- ABC News. Epidemiologist says COVID-19 testing is an ‘enormous problem’. ABC News. 2 January 2022. Available at: https://www.youtube.com/watch?v=GV3i7vN8vXM&ab_channel=ABCNews(Australia) (Accessed 2 July 2023).
- Hayes, P. What is the new national definition of a COVID close contact? News GP: The Royal Australian College of General Practitioners (RACGP) (2021). Available at: https://www1.racgp.org.au/newsgp/clinical/new-national-definition-of-covid-close-contact (Accessed 2 July 2023).
- Therapeutic Goods Administration (TGA). COVID-19 rapid antigen self-tests that are approved in Australia. Australian Government, Department of Health and Aged Care (2023) [updated 17 March 2023]. Available at: https://www.tga.gov.au/products/covid-19/covid-19-tests/covid-19-rapid-antigen-self-tests-home-use/covid-19-rapid-antigen-self-tests-are-approved-australia (Accessed 26 March 2023).
- Vicziany M, Hardikar J. Can self-administered rapid antigen tests (RATs) help rural India? An evaluation of the CoviSelf kit as a response to the 2019-2022 COVID-19 pandemic. Diagnostics (2022) 12(3):644. [CrossRef]
- Royal College of Pathologists of Australia (RCPA). Position Statement: COVID-19 antigen and point of care testing. Surry Hills, New South Wales, Australia: Royal College of Pathologists of Australia. July 2022. Available at: https://www.rcpa.edu.au/getattachment/dde91525-d128-4f0a-ba47-ddea400c061b/COVID-19-Antigen-and-Point-of-Care-Testing.aspx (Accessed 27 February 2023).
- MacIntyre, R. “Epidemic detectives”. In: Dark Winter. An insider’s guide to pandemics and biosecurity. Sydney, NSW, Australia: UNSW Press (2022). p. 152-69.
- The Sydney Morning Herald. Effects of the Epidemic. The Sydney Morning Herald. 25 June 1919. Available at: https://www.newspapers.com/clip/59130451/para-4-of-25619-p-12/ (Accessed 2 April 2023).
- New South Wales Metropolitan Citizens’ Influenza Administrative Committee & New South Wales Parliament Legislative Assembly. Outbreak of pneumonic influenza in New South Wales in 1919: Report. Sydney, New South Wales, Australia: Legislative Assembly (1920). Available at: https://nla.gov.au/nla.cat-vn2062179 (Accessed 4 April 2023).
- The Sydney Morning Herald. Effects of the Epidemic. The Sydney Morning Herald. 25 June 1919. p. 12 para.5. Available at: https://www.newspapers.com/clip/59130483/para-5-of-25619-p-12/ (Accessed 2 April 2023).
- The Sydney Morning Herald. Page 1 Summary. The Sydney Morning Herald. 23 June 1919. p. 1. Available at: https://www.newspapers.com/clip/59170828/from-page-1-summary-not-picked-up-in/ (Accessed 2 April 2023).
- Caley P, Philp DJ, McCracken K. Quantifying social distancing arising from pandemic influenza. J R Soc Interface (2008) 5(23):631-9. [CrossRef]
- Foley, PB. Encephalitis lethargica and the influenza virus. II. The influenza pandemic of 1918/19 and encephalitis lethargica: epidemiology and symptoms. J Neural Transm (2009) 116(10):1295-308. 1295. [Google Scholar] [CrossRef]
- Cumpston JHL. Influenza and maritime quarantine in Australia. Commonwealth of Australia Quarantine Service Publication. Melbourne, Victoria, Australia: Commonwealth of Australia Quarantine Service (1919). Available at: https://nla.gov.au/nla.obj-192064587 (Accessed 17 June 2023).
- State Government of Victoria Department of Health and Human Services. Coronavirus update for Victoria - 30 September 2020. Melbourne, Victoria, Australia: State Government of Victoria (2020). Available at: https://www.dhhs.vic.gov.au/coronavirus-update-victoria-30-september-2020 (Accessed 17 June 2023).
- South Eastern Melbourne Primary Health Network (SEMPHN). South Eastern Melbourne COVID-19 primary care management. Heatherton, Victoria, Australia: South Eastern Melbourne PHN (2020). Available at: www.semphn.org.au/SEMPHN_GP_managment_of_COVID_ve_patients_Pathways_14092020_.pdf (Accessed 9 September 2020).
- Royal Commission into Aged Care Quality and Safety. Aged care and COVID-19: A special report: Commonwealth of Australia (2020). Available at: https://agedcare.royalcommission.gov.au/sites/default/files/2020-12/aged-care-and-covid-19-a-special-report.pdf (Accessed 4 February 2023).
- ABC News. Victorian coronavirus outbreaks in aged care homes swell as St Basil’s in Melbourne evacuated. ABC News. 31 July 2020. Available at: https://www.abc.net.au/news/2020-07-31/victorian-coronavirus-outbreaks-aged-care-homes-st-basils/12513668 (Accessed 28 February 2023).
- Handley, E. Why are there are more COVID-19 cases in private aged care than the public sector? ABC News. 1 August 2020. Available at: https://www.abc.net.au/news/2020-08-01/why-more-covid-19-cases-in-private-aged-care-than-public-sector/12503212 (Accessed 1 August 2020).
- Lunn S, Baxendale RL. Grim toll as unskilled staff put aged-aged homes at risk. The Australian. 24 July 2020. Available at: https://www.theaustralian.com.au/nation/politics/grim-toll-as-unskilled-staff-put-melbourne-agedcare-homes-at-risk/news-story/863182db7610ba22d304f82fec3cd30a (Accessed 30 March 2023).
- The Weekly Source. Department of Health extends Victorian ban on aged care staff working across multiple sites until October – but DHHS says some workers still at more than one facility. The Weekly Source. 20 September 2020. Available at: https://www.theweeklysource.com.au/department-of-health-extends-victorian-ban-on-aged-care-staff-working-across-multiple-sites-until-october-but-dhhs-says-some-workers-still-at-more-than-one-facility/ (Accessed 28 February 2023).
- Clayton R, Murray-Atfield Y. Fair Work Commission awards paid pandemic leave to aged care workers to stop staff going to work sick. ABC News. 27 July 2020. Available at: https://www.abc.net.au/news/2020-07-27/aged-care-workers-get-paid-pandemic-leave-fair-work-commission/12496342 (Accessed 28 February 2023).
- Davern M, McLaws M-L, Gudes O. Mapping COVID-19 spread in Melbourne shows link to job types and ability to stay home. The Conversation (2020). Available at: https://theconversation.com/mapping-covid-19-spread-in-melbourne-shows-link-to-job-types-and-ability-to-stay-home-143610 (Accessed 9 July 2023).
- Parliament of Victoria Public Accounts and Estimates Committee. Inquiry into the Victorian Government’s response to the COVID-19 pandemic. Chapter 6: Jobs and industry. Melbourne, Victoria, Australia: Victorian Government Printer (2021). p. 115-36. Available at: https://new.parliament.vic.gov.au/49706e/contentassets/9c4e489fe9834121826347ad523e87d2/paec_59-08_vic_gov_response_to_covid-19_pandemic.pdf (Accessed 28 June 2023).
- Piketty, T. Capital in the Twenty-First Century. Cambridge, MA, USA & London, England: Harvard University Press (2014). [CrossRef]
- Roder C, Maggs C, McNamara BJ, O’Brien D, Wade AJ, Bennett C, et al. Area-level social and economic factors and the local incidence of SARS-CoV-2 infections in Victoria during 2020. Med J Aust (2022) 216(7):349-56. [CrossRef]
- Belling N, host. The worst public health disaster in living memory... Why we need to talk about COVID. Australia Today’s Morning Agenda with Natarsha Belling Podcast. 19 December 2022. Available at: https://omny.fm/shows/your-morning-agenda-with-natarsha-belling-1/the-worst-public-health-disaster-in-living-memory (Accessed 1 January 2023).
| Spanish Flu 1919 | COVID-19 2020 | |||||
|---|---|---|---|---|---|---|
| Australia | Sydney | Melbourne | Australia | Sydney | Melbourne | |
| Population (11,14,15) | 5,217,019 | 828,700 | 743,000 | 25,364,300. | 5,312,163 | 5,078,193 |
| % Capital city population in national population | 100 | 15.9 | 14.2 | 100 | 20.9 | 20.0 |
| % Capital city population in total state population | 41.4 | 49.7 | 65.7 | 77.0 | ||
| Number of deaths (11,12,16) | 11,552 a | 3,902 b | 2,391 a | 909 a | 54 ac | 820 ac |
| % of national deaths | 100 | 33.8 | 20.7 | 100 | 5.9 | 90.2 |
| Crude Death Rate per 100,000 population | 221 | 471 | 322 | 3.6 | 1.0 | 16.1 |
| SYDNEY | MELBOURNE | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Stages | Weekly deaths | Number of weeks | Week ending dates | % of 35.5 weeks | Stages | Weekly deaths | Number of weeks | Week ending dates | % of 35.5 weeks |
| Stage 1 | Zero & Single digits | 8 | 1 Feb – 21 Mar | 23% | Stage 1 | Zero | 7 | 1 Feb – 14 Mar | 20% |
| Stage 2 | Double digits | 1 | 28 Mar | 3% | Stage 2 | Zero & single digits | 17[including 8 zero weeks] | 21 Mar – 11 Jul | 48% [22%] |
| Stage 3 | Triple digits | 6 | 4 Apr – 9 May | 17% | Stage 3 | Double digits | 1 | 18 Jul | 3% |
| Stage 4 | Double digits | 5 | 16 May – 13 Jun | 14% | Stage 4 | Triple digits | 3 | 25 Jul – 8 Aug | 8% |
| Stage 5 | Triple digits | 5 | 20 Jun – 18 Jul | 14% | Stage 5 | Double digits | 5 | 15 Aug – 12 Sep | 14% |
| Stage 6 | Double digits | 9 | 25 Jul – 19 Sep | 25% | Stage 6 | Single digits | 2.5 | 19 Sep – 30 Sep | 7% |
| Stage 7 | Single digits | 1.5 | 26 Sep – 30 Sep | 4% | |||||
| TOTAL 35.5 weeks | 100% | TOTAL 35.5 weeks | 100% | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





