1. Introduction
Marginal Fitness of Crown Restoration One of the crucial factors for the success of prosthetic restoration, clinical quality, longevity, and predictability of a dental prosthesis. Accurate assessment and quantification of marginal parameters are needed for its measurement to distinguish between fit and misfit [1]. Poor marginal fit of restoration can cause harm to the tooth, periodontal tissue, and even the restoration itself. A significant marginal discrepancy can cause cement to dissolve, microleakage to occur, and plaque to build up, which causes pulpal lesions, caries, and gingival inflammation [2,3].
A marginal gap (MG) is a vertical measurement from the restoration margin till the outermost edge of the finish line of the tooth margin. The absolute marginal discrepancy (AMD) means the distance between the crown's margins to the preparation's Cavo surface angle or is the angular combination of the vertical and horizontal marginal discrepancies [4]. Different studies have recommended marginal space between 50 μm and 120 μm as being acceptable, while other studies have recommended spacing of fewer than 100 μm [5,6]. Authors found that restorations with an MD of less than 120 μm had a higher success rate in vivo research involving more than 1000 crowns [7]. The reported MD for crowns made using CAD/CAM technology ranges from 50 to 100 μm [8,9]. Dental professionals were able to employ new treatment modalities and altered the design and application parameters of all-ceramic restorations with the advent of computer-aided design/computer-aided manufacturing (CAD/CAM) technology, which coincided with an increase in posterior oral aesthetic demand [10]. Clinical evidence supports the use of CAD/CAM machining for the manufacture of dental restorations. When compared to the use of Impression Materials, the digital System has many Advantages Over the traditional Method, such as the possibility of digital Artikulation, reduced cost, procedural complexity, and waste, enhanced patient acceptance, and the removal of the necessity for Manual pouring with cast trimming and Impression Desinfection [11]. A single-use, disposable camera sleeve is all that is needed for infection control. The digital system also does away with the need for trays for impression, delivers digital files electronically, and eliminates the need for physical shipping, which would subject a physical impression to humidity fluctuations, temperature, and time. The digital impression is then ready for design without the dimensional changes that are anticipated in the conventional system [12]. For fixed partial dentures (FPDs) and crowns, all-ceramic systems offer an attractive option to metal-ceramic systems in terms of restorative materials. Numerous advancements in ceramic restoration have resulted from growing demands for great aesthetics, biocompatibility. German scientist Martin Heinrich Klaproth first recognized zirconia in 1789. Then, in 1824, a Swedish chemist named Jons Jakob Berzelius was the first to create impure zirconium metal by boiling potassium and potassium fluoride [13]. High-strength zirconia is now being used in the production of fixed partial prostheses, even in load-bearing areas. Materials based on zirconia offer a number of benefits, including ideal mechanical qualities, limited bacterial adherence, conventional cementation, and biocompatibility. However, mechanical characteristics are not the sole factor contributing to dental restorations' excellent endurance. Zirconia CAD/CAM crown restoration can be classified according to the type of fabrication either Partial contour zirconia: Veneered zirconia crowns were created using partially sintered Y-TZP blocks. A partial contour zirconia restoration involves milling a durable zirconia framework and covering it in a more aesthetically pleasing porcelain veneer [14]. Or Full contour zirconia: Partially sintered Y-TZP blocks created full contour anatomical crowns. One material block can mill a monolithic unit for full contour restorations without porcelain overlays [15,16]. It was approved for use with crowns over implants, posterior crowns, full-arch bridges up to 14 units, and crowns with limited occlusal clearance. It is also advised that any anterior restoration made of zirconia employ a porcelain face veneer for aesthetic purposes. It has various characteristics, including strong flexural strength and fracture toughness, low thermal expansion numbers, resistance to thermal shock, better esthetics, and wear compatibility [17]. Full contour zirconia, on the other hand, could be utilized in particular anterior situations when the dentist wants to prioritize the restoration's strength over its aesthetics. Numerous qualities are included in it, including enhanced aesthetics, wear compatibility, resistance to thermal shock (low thermal expansion numbers), high flexural strength, and fracture toughness. Even if the material used for the indirect restoration plays a crucial role in its performance, it is useless without high-quality cement and the right cementing technique to avoid oral fluids getting into the space between the restoration and the tooth. Dental cements are divided into two categories: resin-based and water-based polymerizing cements [18]. Zinc phosphate cement and glass Ionomer cement are examples of water-based cement, whereas resin-based cement includes resin composites, resin-modified glass Ionomer cement, and adhesive cement [19]. The chemical attachment of water-based cement to tooth structures or restoration materials is minimal or nonexistent [20]. Resin cement is the newest type of cement for indirect restorations; it can bond to the tooth structure and the restoration's inner surface. These cements are utilized for cementation of all types of restoration since they are more complex, non-resorbable in oral fluid, and highly technique sensitive than conventional cement, despite having stronger tensile, compressive, and flexural properties than other types of cement [21].
The aim of this study to assess the impact of different occlusal reduction scheme combined with different types of cement on the marginal fit of full contour zirconia crowns.
2. Materials and Methods
Forty human maxillary first premolars of similar size and form were chosen. The teeth were taken out of patients between the ages of 18 and 27 to undergo orthodontic therapy. To reduce the number of variables in the study, every tooth needed to have a crown that was measured using a digital caliper, and every tooth needed to be free of cavities, restorations, cracks, and abnormalities in the enamel [22]. the teeth were split into two major groups at random [23]. The roots of the teeth were embedded in cold acrylic resin (20 mm in height and 10 mm in width) up to 2 mm below the cementoenamel junction to simulate the level of alveolar bone height in a healthy tooth, with the help of a plastic mold to facilitate the preparing procedures [24].
Samples grouping: Two primary groups will be formed from the samples of twenty samples in each group according to occlusal reduction scheme:
Group A: chamfer finishing line design with planar (anatomical) occlusal reduction scheme.
Group B: chamfer finishing line design with flat (non-anatomical) occlusal reduction scheme.
Next, each primary group will be split into two subgroups based on the type of cement that was utilized.
Subgroup A1 red: crowns will be cemented by using Glass Ionomer cement (Fuji plus).
Subgroup A2 green: crowns will be cemented by using the Universal adhesive system (Duo estecem Universal).
Subgroup B1 blue: crowns will be cemented by using Glass Ionomer cement (Fuji plus).
Subgroup B2 yellow: crowns will be cemented using the Universal adhesive system (Duo estecem Universal)
For standardization, the same operator prepared each sample with the help of a dental surveyor. The surveyor was changed to hold the turbine (110.000 round rpm). The bur's long axis would be perpendicular to the tooth's long axis and the bur's convergence with the axial wall of the tooth would be uniform of the teeth were preparing to receive zirconia crown following the recommendations made for Ivoclar Vivadent that include the following preparation features: axial reduction of 1 to 1.5 mm, a chamfer finishing line of 0.8 to 1.5 mm in depth, the occlusal-gingival height of 4 mm, convergence angle of 3 o for each axial wall (the total convergence angle of 6 o), and a chamfer height of 0.8 to 1.5 mm above the cemento-enamel junction. these dimensions were examined using a digital caliper. Following the axial reduction of each tooth following its group, the occlusal surface was prepared to create a smooth occlusal reduction scheme using a diamond wheel bur no. (824 047) from Komet, Germany. Rugby ball bur no. (899 314 027), (Komet, Germany), was used to reduce further the occlusal surface of all the teeth samples in subgroups A1 and A2 to alter the design into a planar shape. To keep the crown restoration from experiencing stress concentration, all internal line angles and sharp angles were rounded. All fabrication processes, including model scanning, milling, and sintering protocols, were carried out by the Open Techniques-Desktop scanner (Open Technology, Italy). Open scanner is highly customizable and proves to be the best scanning solution for any restoration. The 3d scanner supports must rest on a perfectly horizontal flat surface (leveling machine). The cementation process was based on the manufacturer's leaflet for both cements. The inner surface of the crown was filled with cement once the cement material had been mixed. Cement was injected into each crown's intaglio surface using a disposable mixing tip. First, finger pressure was applied to ensure the crown was firmly in place. Subsequently, a vertical static force of 5 kg (about 50 N) was applied to the occlusal surface for 5 minutes using a specimen-holding apparatus specially made for the purpose. To replicate the biting force during cementation was done clinically [25]. To reproduce the cushioning effect of the cotton roll used in clinical crown seating and to evenly distribute the load throughout the occlusal surface of the tested crown, a rubber piece was placed between the load applicator and the crown during cementation [26]. The Samples cemented with the Universal adhesive system utilizing an alight cure unit to spot-cure the cement for 2 seconds; a probe removed the surplus cement. The sample then given a 20-second curing treatment on each surface. While the samples cemented with Fuji plus Glass Ionomer cement, approximately 2 minutes after starting the mixing, the excess was removed as manufacturer's instruction. All specimens were kept in distilled water at room temperature and evaluated 24 hours following cementation [27]. Marginal gap measurements were taken at two distinct times: before and after cementing. Measurements were taken by connecting the Dino-lite digital microscope to a PC using a USB with 230 X magnification by Holmes et al. (1989), the definition of the marginal gap (perpendicular distance from the margin of the finishing line preparation to the margin of the restoration). The measurements taken at four spots on each tooth surface (two line's margins, two points marked with permanent marker in the middle of the surface, and two additional points on the left and right sides, separated by one millimeter from the preceding two points).By keeping the crown-tooth assembly in place using a specimen-holding device that was specifically designed for this purpose and initially applying steady finger pressure for seating during cementation, the measurements obtained perpendicular with the tooth axis [28]. Largest gap was selected to reflect the sample's marginal gap [4,29]. Every measurement was carried out by the same researcher [30]. The digital microscope was positioned so that its long axis lined up with the long axis of the tooth. The handle was secured, preventing it from being changed vertically without altering the microscope's horizontal tilt. The images opening in an image-processing application (Image J 1.50i, USA) allowed for measurement of the marginal gap in pixels after Dino-capture software had processed two photographs for each surface of the tooth sample. To convert the measurements to micrometers, a digital microscope was used to take a picture of one millimeter of a ruler at a magnification of 230X. After that, the picture was opened in the (Image J) application, and a line that matched a known distance of one millimeter was created using the straight-line selection tool. All estimated measurements were transformed from pixels to (um) by opening the (Set scale) window after selecting the (analyze) option from the main menu while keeping the microscope's calibration and magnification intact [31]. The known distance and measurement unit (1000 and um, respectively) entered the dialog box. The distance was automatically entered into the pixels field based on the length of the chosen line [32].
Statistical Analysis
The statistical analysis was done using SPSS.Shapiro-Wilk test: test the normality of the distribution of variables. The student’s t-test was used to investigate the causes of the difference and identify any significant differences between the two categories. The marginal gaps for each sample were compared using a Paired-sample t-test. Level of significance as Not significant P>0.05, Significant P<0.05.
3. Results
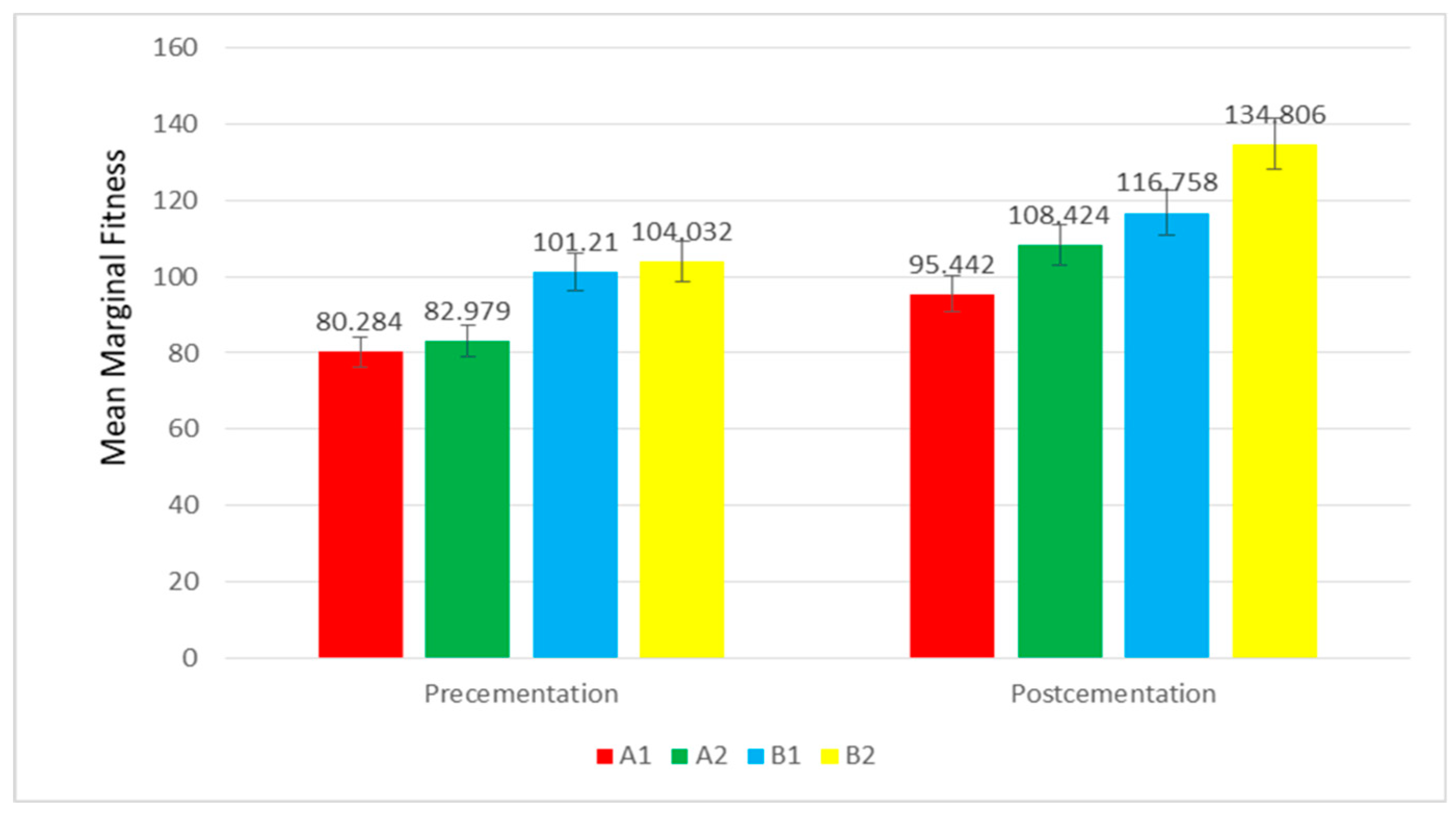
The lowest mean of vertical marginal gap precementation was scored in Group A1 (planar occlusal reduction scheme group) (80.284±23.021µm), while the highest mean was recorded by Group B2(flat occlusal reduction scheme group) (118.597±9.956µm) (
Table 1). Marginal fitness when compared from pre cementation to post cementation in each group and subgroup, it increases with significant change and highest increase in B1 with slightly different in other groups. subgroup A1 (chamfer finishing line with planar occlusal reduction scheme) scored the lowest mean of vertical marginal gap values (95.45±17.598), while subgroup B2 (chamfer finishing line with flat occlusal reduction scheme) had the highest mean (134.806 ±8.114).
Figure 1.
Bar-chart showing the mean values of the vertical marginal gap of the four groups.
Figure 1.
Bar-chart showing the mean values of the vertical marginal gap of the four groups.
Student’s t-test was performed to investigate the causes of variations and identify noteworthy distinctions between every two distinct subgroups as Shown in (
Table 2 and
Table 3). Among groups (A1-B1, A2-B2), both B1 and B2 have MF higher than A1 and A2 with significant difference in both pre and post cementation and higher difference in A2 - B2 and A1-B1 post cementation. Among subgroups, although A2 and B2 have higher MF than A1 and A2 respectively in both pre and post cementation but with no significant difference in pre cementation while in post cementation in A1-A2, its practically significant (Cohen D=1.026, large effect size) and between B1-B2 also its result is significant.
4. Discussion
The most popular technique for determining how accurately crown restorations fit is the vertical marginal gap measurement [33]. The "perfect margin" means two adjacent surfaces (cement ceramic, cement tooth) that blend into one another without any variation in level and have a continuous margin [34]. The finishing line design (chamfer) and occlusal surface reduction schemes (planar or flat) were advised for zirconia-based restorations, per manufacturer recommendations.
The planar occlusal reduction scheme of teeth samples is recommended because it entails removing less tooth structure (conservative preparation) in accordance with clinical circumstances, increasing structural durability with a lower risk of dental pulp exposure or injury [35]. In clinical situations involving deep bite, attrition, and insufficient space, which are indicated for full contour zirconia material due to its superior mechanical properties compared to other dental ceramics, tooth samples with overly simplified shapes and a flat occlusal reduction scheme may be necessary. This was consistent with the findings that showed a satisfactory marginal fit was achieved by the flat occlusal scheme [36]. Since the digital microscope is regarded as a direct and non-destructive technology that won't disrupt the specimens, it was utilized to measure the marginal gap. Additionally, this technique could be used in clinical settings and was the most popular way to measure the vertical gap [37]. The magnification of 230X used in this study was large enough to view the vertical marginal discrepancies accurately. The vertical marginal gap was measured at the midpoint of each tooth surface by Berger (1977), as this is where the most shrinkage occurs due to the increased bulk of ceramic material. Holden et al. 2009 utilized four distinct points at four locations to assess the marginal gaps. In this current study, the luting agent was a resin-modified GIC-Fuji plus compared to resin cement from tokoyama (EsteCem® II plus). EsteCem® II plus is a dual-cure resin cement that simplifies indirect restorations. Does not require additional primers or activators and is compatible with all restorative materials. For long-lasting and aesthetically pleasing results, the key characteristics are minimum water absorption, easy cleanup, and exceptional bond strength. (Tokuyama Dental America Inc.,2023). Resin-modified glass Ionomer cement, Due to the chelating between the carboxyl groups of the cement and the calcium and phosphorus of the dentin and enamel apatite, Ionomer cement sticks to the tooth surface after forming ionic bonds. Nonetheless, because of their composite component, RMGICs have a stronger bond with dentine [38].
The outcomes of this in vitro study revealed statistically significant differences for each of the investigated groupings; however, they were all still within the clinically acceptable limit (120 um) only subgroup B2 where the marginal gap was 134.806 after cementation. The study's mean marginal gap values were lower for teeth generated with both types of cement and a chamfer finishing line utilizing a planar occlusal reduction approach than for teeth made using a flat occlusal reduction technique according to a statistical analysis of the study's data. This could result from the occlusal-axial line angle of the flat occlusal reduction scheme being at a straight angle, which could impede the proper seating of the crown repair. A planar occlusal reduction approach and Chamfer's finishing line indicate lower mean marginal gap values. This could be due to the chamfer finishing line design, which has a more rounded angle between the gingival and axial seats to allow for a more precise seat for crown repair.
During the setting of the crown, Luting agents undergo dimensional changes, being soluble in the fluid of the oral cavity and having distinct viscosity and film thickness affecting the marginal gap. Comparing the pre-cementation results with those recorded post-cementation for all examined subgroups demonstrated that the luting cement and cementation process plays a significant impact in the ultimate precision of the marginal fit for all ceramic crown restorations. The viscosity of the resin cement increased too quickly to flow toward the cervical area and pushed outside the boundaries of the crown [39]. As a result, more cement is released, and pressure is applied, pushing the cement upward, which leads to a significant buildup of luting cement on the prepared tooth's occlusal surface and may prevent the crown restoration from properly seating post cementation [40]. Several studied concluded marginal gap values for all ceramic crown restorations were significantly higher after cementation but within the acceptable clinical limit (120 um) [41,42].
In this current study, microleakage is seen with all types of cement; however, resin modified glass Ionomer cement has minimum microleakage compared to resin cement. GU et al. (2005), and Suarez MJ, et al. (2011) reported results that were consistent with this [43,44]. The impact of cement kind, viscosity, and cementation process could cause this. The adhesion of resin-modified glass-inomer cement is affected by the molecular interactions between the glass Ionomer particles and the tooth substance. Using various ceramic materials with varying degrees of precision is just one factor in producing a better seal; other factors include cement's solubility and film thickness.
5. Conclusions
Within the limitations of this in-vitro investigation, it can be concluded that both occlusal reduction schemes (planar and flat) exhibit statistical differences in terms of marginal accuracy. The planar occlusal reduction scheme with Fuji plus cement showed the lowest mean marginal gap. In contrast, the flat occlusal reduction scheme with DuoEstacem II cement showed the highest marginal gap after cementation.
Author Contributions
M.S.: methodology, investigation, data curation, writing—original draft preparation. A.A.: methodology, resources, analysis. L.A.-T.: conceptualization, methodology, writing—review and editing, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Teeth were collected using an ethics protocol approved by the health research committee of Greifswald University (Ref No. 165492).
Data Availability Statement
Not applicable.
Acknowledgments
This work was supported by the Greifswald University
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHITE, S. N., INGLES, S. & KIPNIS, V. (1994). Influence of marginal opening on microleakage of cemented artificial crowns. J Prosthodont Mater, 71(3), 257-64. [CrossRef]
- TAN, P. L., GRATTON, D. G., DIAZ-ARNOLD, A. M. & HOLMES, D. C. (2008). An in vitro comparison of vertical marginal gaps of CAD/CAM titanium and conventional cast restorations. J Prosthodont, 17(5), 378- 83. [CrossRef]
- Demir N, Ozturk AN, Malkoc MA. Evaluation of the marginal fit of full ceramic crowns by the microcomputed tomography (micro-CT) technique. Eur J Dent 2014; 8:437-44. [CrossRef]
- HOLMES, J. R., BAYNE, S. C., HOLLAND, G. A. SULIK, W. D. (1989). Considerations in measurement of marginal fit. J Prosthet Dent, 62(2), 405- 8. [CrossRef]
- Suarez, M. J., Villaumbrosia, D., González, P., Pradíes, G., and Lozano, J. F. 2003. Comparison of the marginal fit of Procera All Ceram crowns with two finish lines. International Journal of Prosthodontics, 16, 229-232.
- Neves FD, Prado CJ, Prudente MS, Carneiro TA, Zancopé K, Davi LR, et al. Micro-computed tomography evaluation of marginal fit of lithium disilicate crowns fabricated by using chairside CAD/CAM systems or the heat-pressing technique. J Prosthet Dent 2014; 112:1134- 40. [CrossRef]
- MCLEAN, J. W.VONFRAUNHOFER, J. A. (1971). The estimation of cement film thickness by an in vivo technique. Brit J Dent, 131,107-11.
- Akbar JH, Petrie CS, Walker MP, Williams K & Eick JD (2006) Marginal adaptation of Cerec 3 CAD/CAM composite crowns using two different finish line preparation designs Journal of Prosthodontics 15() 155-163. [CrossRef]
- URAL, C., BURGAZ, Y. SARAC, D. (2010). In vitro evaluation of marginal adaptation in five ceramic restoration fabricating techniques. Int J Quintessence, 41, 585-90.
- Kassem As, Atta O, El-Mowafy O. Fatigue resistance and microleakage of CAD/CAM ceramic and composite molar crowns. J Prosthodont 2012; 21:28-32. [CrossRef]
- CHRISTENSEN, G. J. (2009). Impressions are changing deciding on conventional, digital or digital plus in office milling. J ADA, 140, 1301-4. [CrossRef]
- LOGOZZO, S., KILPELA, A., MAKYNEN, A. ZANETTI, E. M. (2014). Recent advances in dental optics-part II: experimental tests for a new intraoral scanner. Optics and Lasers in Engineering, (54), 187-96.
- RAIGRODSKI, A. J. (2004). Contemporary materials and technologies for all ceramic fixed partial dentures: a review of the literature. Int J Prosthodont, 92, 557-62. [CrossRef]
- RAMOS, G. F., MONTEIRO, E. B., BOTTINO, M. A., ZHANG, Y., MARQUES, D. E. & MELO, R. (2015). Failure probability of three designs of zirconia crowns. Int J Periodont Restor Dent, 35(6), 843-9. [CrossRef]
- BEUER, M., STIMMELMAYR, J. F., GUETH, D., EDELHOFF, M. NAUMANN, M. (2012). In vitro performance of full contour zirconia single crowns. J Dent Mater, 28(4), 449-56. [CrossRef]
- REICH, S. (2015). Tooth colored CAD/CAM monolithic restorations. Int J Comput Dent, 18(2), 131-46. [PubMed]
- CARDEN, R. A. (2011). A changing direction in dentistry: full contour zirconia. J Dent Tech, 14-6.
- Edelhoff, D., and Özcan, M. 2007. To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: cementation. Clinical Oral Implants Research, 18, 193-204. [CrossRef]
- Hitz, T., Stawarczyk, B., Fischer, J., Hämmerle, C. H. and Sailer, I., 2012. Are self-adhesive resin cements a valid alternative to conventional resin cements? A laboratory study of the long-term bond strength. Dental Materials, 28(11), pp. 1183-1190. [CrossRef]
- Burke F. J. 2005. Trends in indirect dentistry: 3. Luting materials. Dental Update, 32(5):251-4, 7-8, 60. [CrossRef]
- Sunico-Segarra M. & Segarra A. 2015. Resin cements: factors affecting clinical performance. In A Practical Clinical Guide to Resin Cements (pp. 9-22). Springer, Berlin, Heidelberg. 100. Simon J. F. & Darnell L. A. 2012. Consideration for proper selection of dental cements. Compendium Continuing Education in Dentistry, 33:28–36. [CrossRef]
- Kocaagaoglu H., Kilinc H. I. & Al-bayrak H. 2017. Effect of digital impressions and production protocols on the adaptation of zirconia copings. The Journal of Prosthetic Dentistry, 117(1): 102-108. [CrossRef]
- EL-HELALI, R., DOWLING, A. H., MCGINLEY, E. L., DUNCAN, H. F. & FLEMING, G. J. 2013. Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. Journal of Dentistry, 41, 216-22. [CrossRef]
- Korkut L., Cotert H. S., Kurtulumus H. 2011. Marginal, internal fit and microleakage of zirconia infrastructures: An in vitro study. Operative Dentistry, 36(1):72-79. [CrossRef]
- ANUNMANA, C., CHAROENCHITT, M. & ASVANUND, C. 2014. Gap comparison between single crown and three-unit bridge zirconia substructures. The journal of advanced prosthodontics, 6, 253. [CrossRef]
- Dimashkieh, M., 2010. The Effect of Veneering Porcelain on the Marginal Fit of Cercon Zirconia Copings (Doctoral dissertation, Department of Prosthetic Dental Science Collage of Dentistry, King Saud University Riyadh, Saudi Arabia).
- Shahrbaf, S., Van Noort, R., Mirzakouchaki, B., Ghassemieh, E., and Martin, N. 2014. Fracture strength of machined ceramic crowns as a function of tooth preparation design and the elastic modulus of the cement. Dental Materials, 30, 234-241. [CrossRef]
- ORTORP, A., ONSSON, D. J., MOUHSEN, A. VULT VON STEYERN, P. (2011). The fit of cobalt chromium three unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. J Dent Mater, 27(4), 356-63. [CrossRef]
- HOLDEN, J. E., GOLDSTEIN, G. R., HITTELMAN, E. L. CLARK, E. A. (2009). Comparison of the marginal fit of pressable ceramic to metal ceramic restorations. J Prosthodont, 18(8), 645-8. [CrossRef]
- Lombardas P., Carbunaru A., McAlarney M. E. & Toothaker R. W. 2000. Dimensional accuracy of castings produced with ringless and metal ring investment systems. The Journal of prosthetic dentistry, 84(1):27-31. [CrossRef]
- ROMEO, E., IORIO, M., STORELLI, S., CAMANDONA, M. ABATI, S. (2009). Marginal adaptation of full coverage CAD/CAM restorations: in vitro study using a non-destructive method. J Minerva Stomatologica, 58(3), 61-72. [PubMed]
- JONATHAN, N. G. (2013). A comparison of crown marginal fit fabricated using digital and conventional methods. A master thesis, department of maxillofacial prosthodontics, university of British Columbia. [CrossRef]
- WOLFART, S., WEGNER, S. M., AL-HALABI, A. KERN, M. (2003). Clinical evaluation of marginal fit of a new experimental all ceramic system before and after cementation. Int J Prosthodont, 16, 587-92. [PubMed]
- ASCHENBRENNER, C. M., LANG, R., HANDEL, G. BEHR, M. (2012). Analysis of marginal adaptation and sealing to enamel and dentin of four self-adhesive resin cements. J Clin Oral Investig, 16, 191–200. [CrossRef]
- Contrepois M., Soenen A., Bartala M. & Laviole O. 2013. Marginal adaptation of ceramic crowns: a systematic review. The Journal of Prosthetic Dentistry, 110 (6):447-454. [CrossRef]
- Podhorsky A, Rehmann P, Wöstmann B. Tooth preparation for full-coverage restorations—a literature review. Clinical oral investigations. 2015 Jun;19:959-68. [CrossRef]
- Karatasli, Ö., Kursoglu, P., Capa, N., and Kazazoglu, E. 2011. Comparison of the marginal fit of different coping materials and designs produced by computer aided manufacturing systems. Dental materials journal, 30, 97-. [CrossRef]
- Malhotra S, Bhullar KK, Kaur S, Malhotra M, Kaur R, Handa A. Comparative evaluation of compressive strength and flexural strength of gc gold hybrid, gic conventional and resin-modified glass-ionomer cement. Journal of Pharmacy & Bioallied Sciences. 2022 Jul;14(Suppl 1): S214. [CrossRef]
- WANG, C. J., MILLSTEIN, P. L. NATHANSON, D. (1992). Effects of cement, cement space, marginal design, seating aid materials, and seating force on crown cementation. J Prosthet Dent, 67(6), 786-90. [CrossRef] [PubMed]
- D ̓ SOUZA, R., SHETTY, O., PUPPALA, P. SHETTY, N. (2012). A better bond: luting simplified. Int J Prsthodont Restor Dent, 2(2), 77-81. [CrossRef]
- STAPPERT, C. F., DAI, M., CHITMONGKOLSUK, S., GERDS, T. STRUB, JR. (2004). Marginal adaptation of three unit fixed partial dentures constructed from pressed ceramic systems. Brit J Dent, 196(12), 766-70. [CrossRef]
- OKUTAN, M., HEYDECKE, G., BUTZ, F. STRUB, J. R. (2006). Fracture load and marginal fit of shrinkage free ZrSiO4 all ceramic crowns after chewing simulation. J Oral Rehabil, 33(11), 827-32. [CrossRef]
- Gu XH, Kern M. Marginal discrepancies and leakage of all ceramic crowns: Influence of luting agents and aging conditions. Int J Prosthodontic 2003; 16:109-16.
- Suarez MJ, Rivera B, Pradies G. Evaluation of the absolute marginal discrepancy of zirconia-based ceramic copings. J Prosthetic Dent 2011; 105:108–114. [CrossRef]
Table 1.
Descriptive statistics of the vertical marginal gaps for the four different subgroups measured in micrometer.
Table 1.
Descriptive statistics of the vertical marginal gaps for the four different subgroups measured in micrometer.
| Groups |
subgroups |
pre-cementation |
post-cementation |
paired t test |
| A |
A1 |
80.284 ± 23.021 |
95.442 ± 17. 598 |
6.664 |
| |
A2 |
95.372 ± 13.407 |
108.424 ± 8.807 |
6.830 |
| B |
B1 |
101.210 ± 14.278 |
116.758 ± 16.151 |
8.660 |
| |
B2 |
118.597 ± 9.956 |
134.806 ± 8.114 |
6.926 |
Table 2.
Student’s t-test for comparison of marginal gaps between each two different subgroups pre cementation.
Table 2.
Student’s t-test for comparison of marginal gaps between each two different subgroups pre cementation.
| |
A (1-2) |
B (1-2) |
1(A-B) |
2(A-B) |
| MD |
-2.695 |
-2.822 |
-20.926 |
-21.053 |
| T test |
0.328 |
0.549 |
-2.443 |
4.663 |
| P value |
0.746 |
0.590 |
0.02511 |
0.000193 |
| Cohen D |
0.077 |
0.129 |
1.407 |
1.099 |
Table 3.
Student’s t-test for comparison of marginal gaps between each two different subgroups post cementation.
Table 3.
Student’s t-test for comparison of marginal gaps between each two different subgroups post cementation.
| |
A (1-2) |
B (1-2) |
1(A-B) |
2(A-B) |
| MD |
-12.982 |
-18.048 |
-21.316 |
-26.382 |
| T test |
2.086 |
3.158 |
2.822 |
6.967 |
| P value |
0.05147a |
0.00545 |
0.01129 |
0.00000 |
| Cohen D |
1.026 |
2.351 |
1.877 |
11.441 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).