1. Introduction
Keratoconus is a progressive disorder that causes irregular astigmatism due to thinning and protrusion of corneal stroma [
1,
2,
3]. According to a meta-analysis of more than 7 million patients in 15 countries, the prevalence of the disease is estimated as 1.38 per 1000 people (approximately 1 in 700 – 800 people) worldwide [
4]. In early to moderate cases with keratoconus, hard contact lens (HCL) is the most general method of vision correction because HCL has advantages to correct refractive error even in the cases with irregular astigmatism or higher-order aberration. However, blepharoptosis has been reported as a complication associated with long-term wear of HCL [
5,
6,
7,
8]. Blepharoptosis not only has cosmetic consequences, but also affects visual function [
9,
10,
11]. Although this complication is well-known in patients with myopia who wear HCLs, to the best of our knowledge, relationship between keratoconus and HCL-induced blepharoptosis has not been known yet. Therefore, in this study, we tried to examine the blepharoptosis in keratoconus patients who ordinary wear HCL.
2. Materials and Methods
The subjects were 37 eyes (2 pseudophakic eyes are included) of 22 patients who were diagnosed as keratoconus with HCL wearing who visited the International University of Health and Welfare Narita Hospital from December 2020 to August 2023. A mean age is 41.6±17.2. The average duration of HCL wear was 19.1±15.5 years. Of the 37 eyes, 35 eyes have worn HCL every day, and 2 eyes have worn HCL more than 4 days a week. We compared the blepharoptosis with HCL wearing periods or age. In this study, we measured eyelid margin distance (EMD), margin reflex distance-1 (MRD-1), and lavator function (LF). EMD was measured from the upper eyelid to the lower eyelid with a ruler (Distantometer, Handaya, Tokyo, Japan). MRD-1 was measured from the pupil center to the upper eyelid with a Distantometer and anterior segment optical coherence tomography (AS-OCT, SS-1000, CASIA2, TOMEY, Nagoya, Japan). In AS-OCT, the capture mode was sagittal (B-scan range was 16mm, C-scan range was 16mm, the number of A/B scan was 800, and the number of B/C scan was 32, respectively). For the analysis, the measurement position was moved to the center of the pupil and the distance from the pupil center to the upper eyelid was manually analyzed using the built-in calipers with the angle set at 90 degree [
12]. LF was measured with a Distantometer as the distance that was moved from the position of the upper eyelid when viewed downward to the position of the upper eyelid when viewed upward. The measurement was performed by gently holding the upper part of the eyebrow with a finger to prevent elevation using frontalis muscle. Statistics were performed using the Kruskal-Wallis test with Bonferroni correction.
3. Results
3.1. EMD, MRD-1, LF in Patients with Keratoconus Who Wear HCL
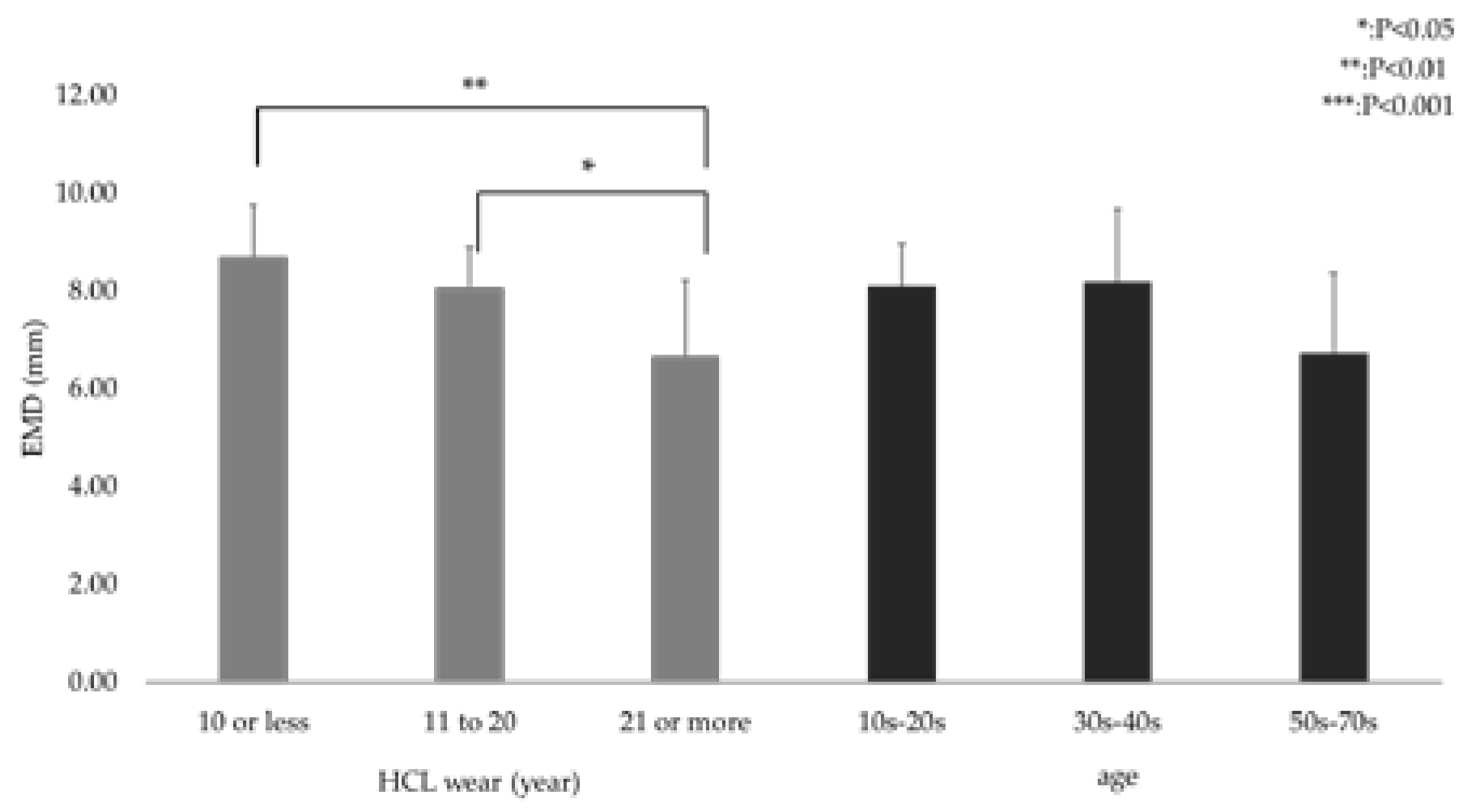
The average EMD was 8.68±1.07 mm within 10 years wearing, 8.05±0.83 mm from 11 to 20 years wearing, and 6.65±1.55 mm with 21 years or more wearing, respectively (
Figure 1). There were statistically significant between within 10 years wearing and with 21 years or more wearing (P<0.01), and from 11 to 20 years wearing and with 21 years or more wearing (P<0.05). The average EMD was also 8.09±0.86 within 29 years old, 8.18±1.49 from 30 years old to 49 years old, and 6.72±1.64 with 50 years or more, respectively (
Figure 1). There was no significant difference among these age groups.
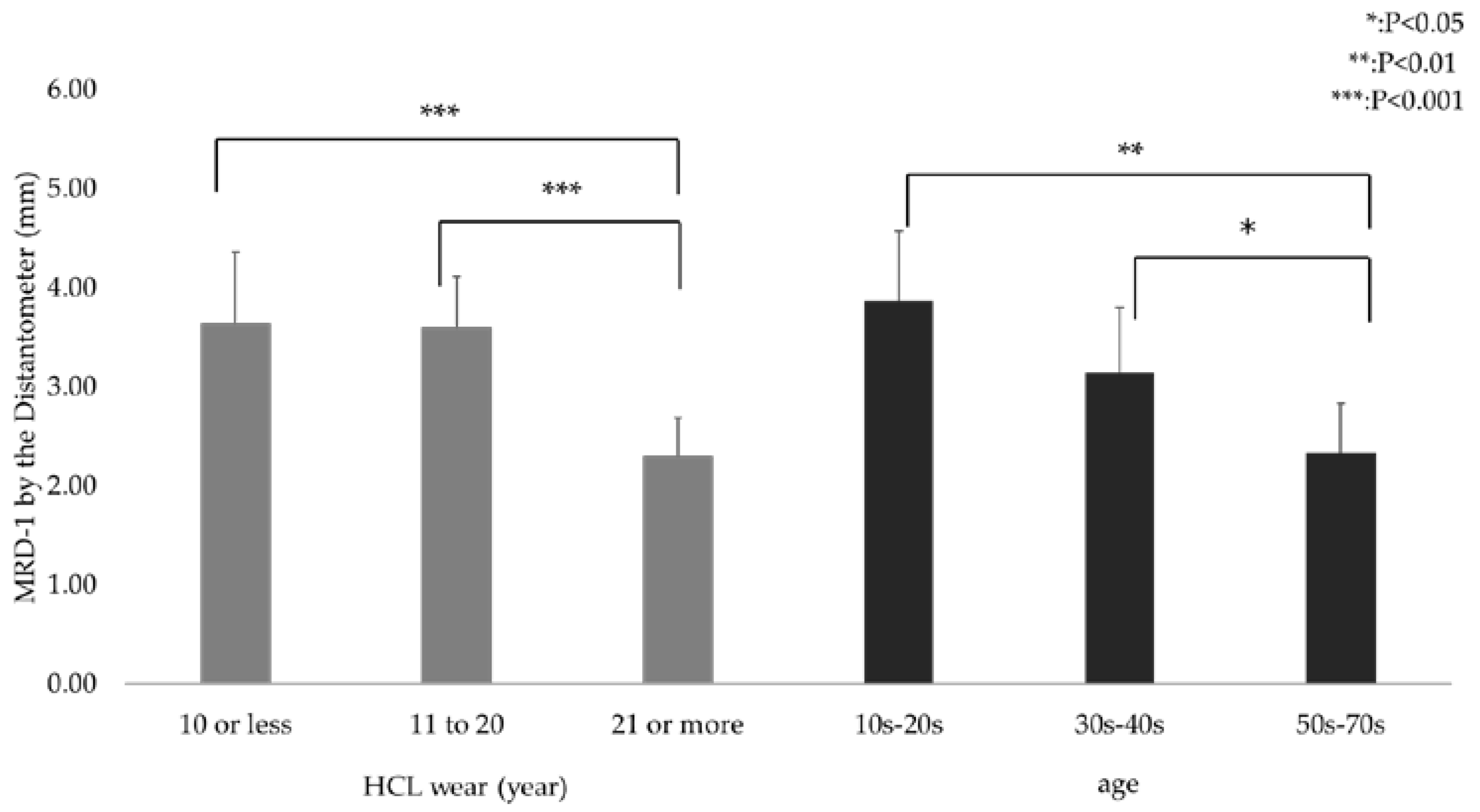
The average MRD-1 using Distantometer was 3.64±0.72 mm within 10 years wearing, 3.60±0.52 mm from 11 to 20 years wearing, and 2.31±0.38 mm with 21 years or more wearing, respectively (
Figure 2). There were statistically significant between within 10 years wearing and with 21 years or more wearing (P<0.001), and from 11 to 20 years wearing and with 21 years or more wearing (P<0.001). The average MRD-1 using Distantometer was also 3.86±0.71 within 29 years old, 3.15±0.66 from 30 years old to 49 years old, and 2.33±0.50 with 50 years or more, respectively (
Figure 2). There were statistically significant between within 29 years old and with 50 years or more (P<0.01), and from 30 years old to 49 years old and with 50 years or more (P<0.05).
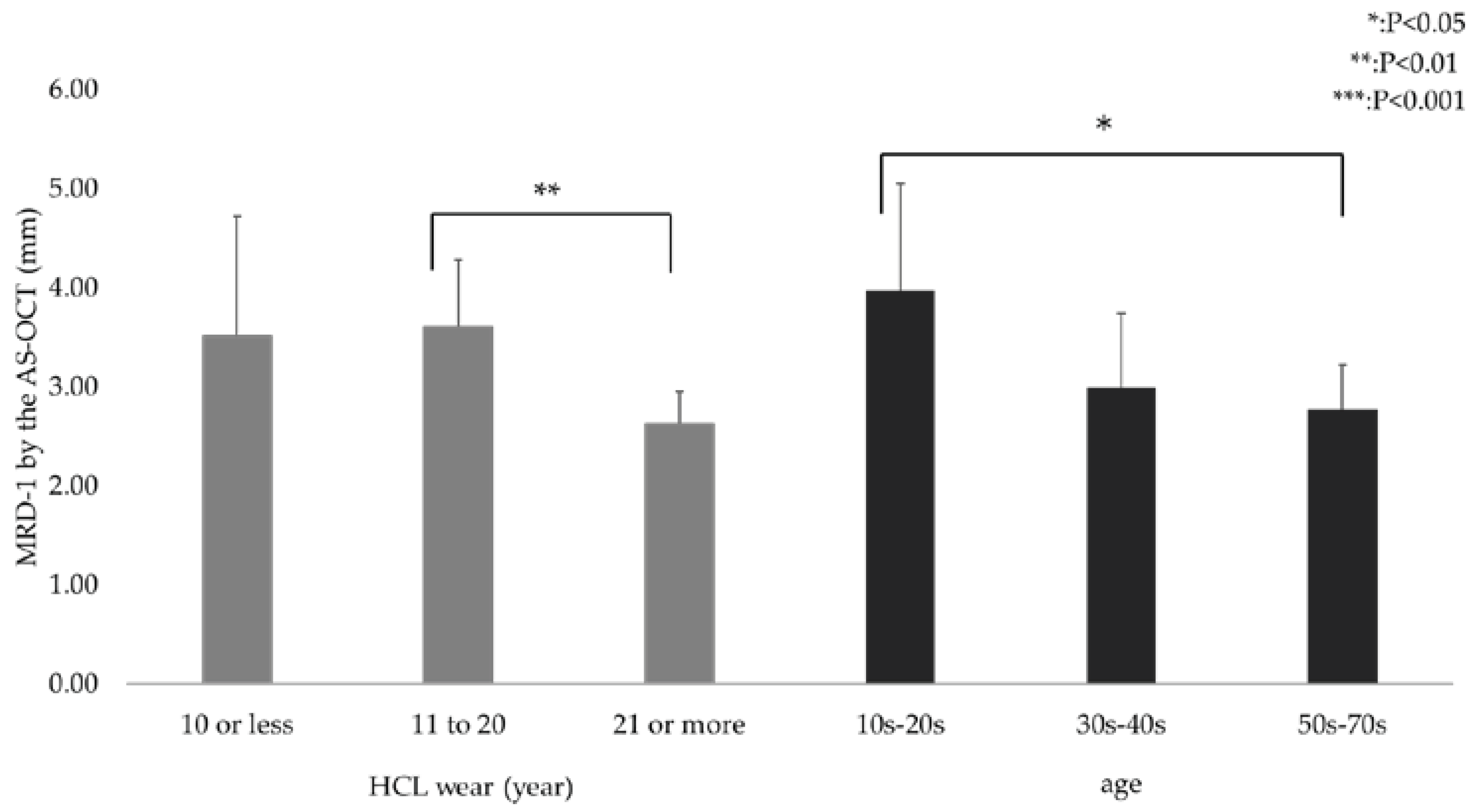
The average MRD-1 using AS-OCT was 3.52±1.21 mm within 10 years wearing, 3.61±0.68 mm from 11 to 20 years wearing, and 2.63±0.32 mm with 21 years or more wearing, respectively (
Figure 3). There were statistically significant between from 11 to 20 years wearing and with 21 years or more wearing (P<0.01). The average MRD-1 using AS-OCT was also 3.97±1.08 within 29 years old, 2.99±0.75 from 30 years old to 49 years old, and 2.78±0.44 with 50 years or more, respectively (
Figure 3). There were statistically significant between within 29 years old and with 50 years or more (P<0.05).
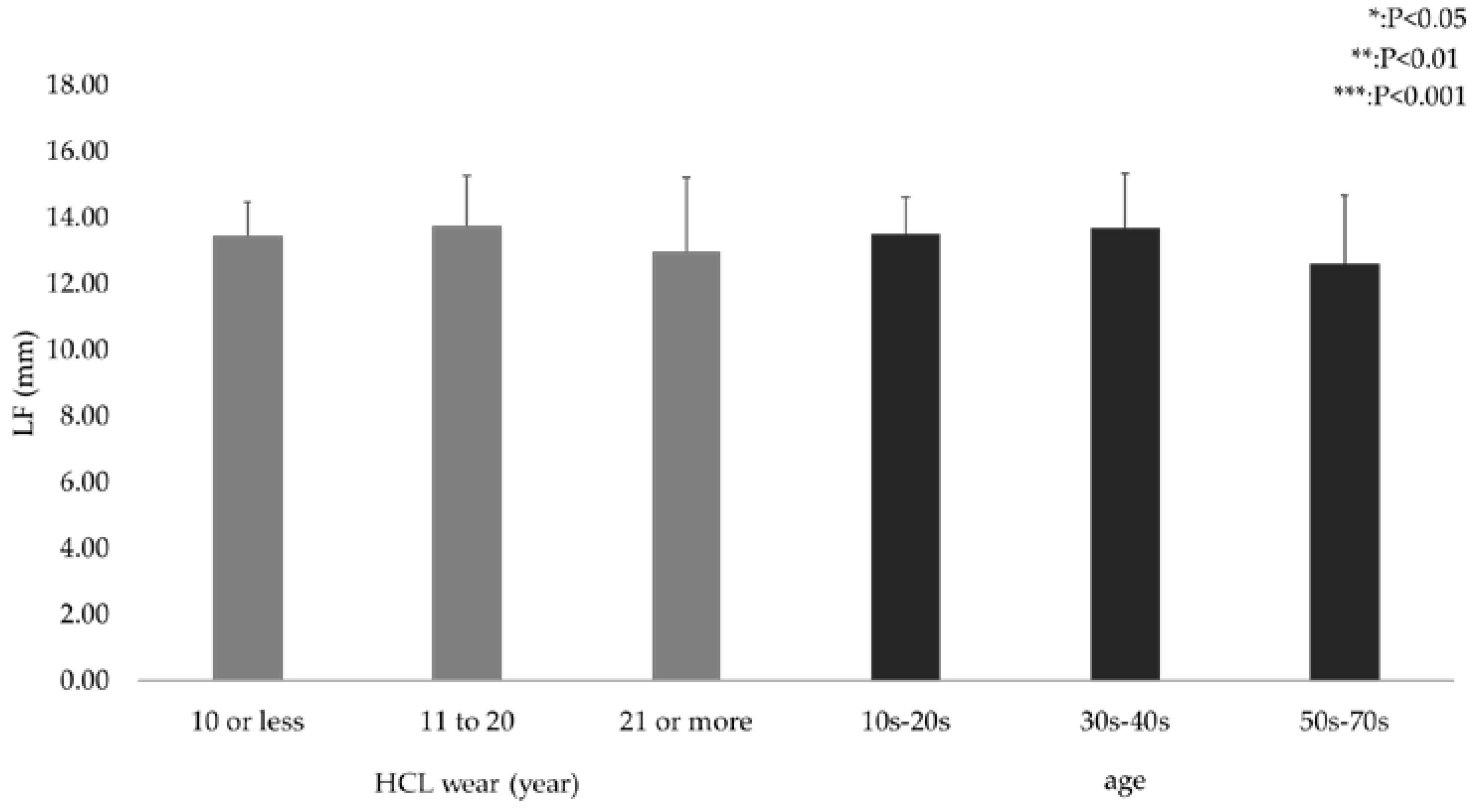
The average LF was 13.46±1.01 mm within 10 years wearing, 13.75±1.51 mm from 11 to 20 years wearing, and 12.96±2.24 mm with 21 years or more wearing, respectively (
Figure 4). There was no significant difference among these groups due to wearing periods. The average LF was also 13.50±1.12 within 29 years old, 13.68±1.67 from 30 years old to 49 years old, and 12.61±2.06 with 50 years or more, respectively (
Figure 4). There was no significant difference among these age groups as well.
3.2. Figures
Average EMD was 8.68±1.07 mm within 10 years wearing, 8.05±0.83 mm from 11 to 20 years wearing, and 6.65±1.55 mm with 21 years or more wearing, respectively. There were statistically significant between within 10 years wearing and with 21 years or more wearing (** P<0.01), and from 11 to 20 years wearing and with 21 years or more wearing (*P<0.05). Average EMD was 8.09±0.86 within 29 years old, 8.18±1.49 from 30 years old to 49 years old, and 6.72±1.64 with 50 years or more, respectively. There was no significant difference among these age groups.
Average MRD-1 was 3.64±0.72 mm within 10 years wearing, 3.60±0.52 mm from 11 to 20 years wearing, and 2.31±0.38 mm with 21 years or more wearing, respectively. There were statistically significant between within 10 years wearing and with 21 years or more wearing (***P<0.001), and from 11 to 20 years wearing and with 21 years or more wearing (***P<0.001). Average MRD-1 was 3.86±0.71 within 29 years old, 3.15±0.66 from 30 years old to 49 years old, and 2.33±0.50 with 50 years or more, respectively. There were statistically significant between within 29 years old and with 50 years or more (**P<0.01) and from 30 years old to 49 years old and with 50 years or more (*P<0.05).
The average MRD-1 was 3.52±1.21 mm within 10 years wearing, 3.61±0.68 mm from 11 to 20 years wearing, and 2.63±0.32 mm with 21 years or more wearing, respectively. There were statistically significant between from 11 to 20 years wearing and with 21 years or more wearing (P<0.01). The average MRD-1 was also 3.97±1.08 within 29 years old, 2.99±0.75 from 30 years old to 49 years old, and 2.78±0.44 with 50 years or more, respectively. There were statistically significant between within 29 years old and with 50 years or more (**P<0.05)
Average LF was 13.46±1.01 mm within 10 years wearing, 13.75±1.51 mm from 11 to 20 years wearing, and 12.96±2.24 mm with 21 years or more wearing. There was no significant difference among these groups due to wearing periods. Average LF was also 13.50±1.12 within 29 years old, 13.68±1.67 from 30 years old to 49 years old, and 12.61±2.06 with 50 years or more, respectively. There was no significant difference among these age groups as well.
4. Discussion
Blepharoptosis associated with long-term wear of HCLs is a well-known complication [
5,
6,
7,
8], but its etiology has not been well understood. Multiple factors have been proposed, including thinning of the elevator tendon membrane and detachment from the eyelid plate due to the outward pulling motion of the upper eyelid when insertion or removal [
13], inflammation due to deposits on the edge of the HCL or on the HCL surface [
14], and/or fibrosis of the Müller muscle [
8]. If these factors are the causes, then it is conceivable that the same insertion and removal methods are used in keratoconus as in normal myopia and thus, even in keratoconic eyes, blepharoptosis may occur due to long-term wear of the HCL.
In fact, in this study, the average MRD-1 values by Distantometer and AS-OCT were 2.88 mm and 3.02 mm, respectively, in patients with keratoconus who had worn HCL for more than 10 years, which were approximately 0.5 mm lower than the average MRD-1 value of 3.50 mm for normal subjects. Regarding HCL-induced ptosis for normal myopia, Bosch et al. reported that MRD-1 was 0.5 mm lower in HCL wearers with more than 10 years of wear and a mean wear duration of 16.3 years compared to non-wearing patients [
5].
In the report by Watanabe et al, the degree of ptosis was classified into four group according to the MRD-1 values: no ptosis (2.8 mm or more), mild (1.5 mm to 2.8 mm), moderate (0 mm to 1.5 mm), and severe (0 mm or less) [
8]. Applying this classification to the present study, 13 eyes had mild ptosis, 0 had moderate ptosis, 0 had severe ptosis, and 24 had no ptosis as measured by the distant meter, while 14 eyes had mild ptosis, 2 had moderate ptosis, 0 had severe ptosis, and 23 had no ptosis as measured by the AS-OCT. Thus, there were no severe cases and most of the cases were mild. The fact that there were no significant differences in any of the parameters between the two groups of patients who had worn HCL for 10 years or less and those who had worn HCL for 11 to 20 years or less suggests that HCL-induced ptosis may be less severe in patients with keratoconus.
In this study, MRD-1 was measured with both a Distantometer and AS-OCT. The Distantometer is a manual method and has a measurement error of 0.5 mm, while the AS-OCT method has a measurement error of 0.01 mm, making it useful for accurate and objective evaluation. The MRD-1 can be easily measured in patients with moderate and severe blepharoptosis, and the measurability rate is stable at 100%, suggesting that this is a clinically significant MRD-1 measurement method [
15].
The reason why ptosis is less severe with long-term use of HCL in keratoconic eyes is not well understood. However, the fitting of the HCL on the ocular surface is different for normal and keratoconus corneas. In normal corneas, the posterior surface of the HCL and corneal curvature match not only at the center of the lens but also at the periphery, but such fitting is difficult in keratoconic eyes due to the non-uniformity of corneal curvature. Therefore, a spherical HCL with a larger size than usual is often used for the HCL prescription for keratoconus [
16]. Although these differences in fitting methods and HCL size may have different effects on the eyelid, it is not clear how these differences affect the development of ptosis. The fitting of the HCL in keratoconic eyes is such that it is supported by the lower eyelid, and is expected to have little impact on the upper eyelid, such as friction. Therefore, there is little effect on Muller's muscle, which can be seen from the fact that levator muscle function has not decreased (
Figure 4). As a limitation of this study, we have not been able to confirm the detailed daily duration of HCL use and care, or the size of the HCL. Including the clarification of pathogenesis why the ptosis is mild in keratoconic eyes, further studies are needed in the future.
5. Conclusions
In conclusion, the older the patient and the longer the wearing period, the lower the MRD-1 value, and the more likely the patient was to develop ptosis in keratoconus eyes. However, compared to normal eyes with HCLs, the incidence of ptosis may be less severe, suggesting the need for further investigation.
Author Contributions
Conceptualization, T.U. and K.D.; methodology, K.H.; software, K.H. and H.N.; validation, K.H., K.D., H.N. and T.U.; formal analysis, K.D.; investigation, K.H. and K.D; resources, T.U.; data curation, K.H.; writing—original draft preparation, K.H. and K.D.; writing—review and editing, T.U., J.Y. and H.N.; supervision, T.U. and J.Y.; project administration, T.U.; funding acquisition, T.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of International University of Health and Welfare Narita Hospital (protocol code XXX and date of approval).
Informed Consent Statement
Informed consent was obtained from optout involved in the study.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bui A., D.; Truong, A.; Pasricha N., D.; Indaram, M. Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions. Clin. Ophthalmol. 2023, 17, 2705–18. [Google Scholar] [CrossRef] [PubMed]
- Maeda, N.; Klyce S., D.; Smolek M., K.; Thompson H., W. Automated Keratoconus Screening with Corneal Topography Analysis. Invest. Ophthalmol. Vis. Sci. 1994, 35, 2749–57. [Google Scholar] [PubMed]
- Kosaki, R.; Maeda N; Bessho K; Hori Y; Nishida K; Suzaki A; Hirohara Y.Mihashi. T.; Fujikado T.; Tano Y. Magnitude and Orientation of Zernike Terms in Patients with Keratoconus. Invest. Ophthalmol. Vis. Sci. 2007, 48, 3062–8.
- Hashemi, H.; Heydarian, S.; Hooshmand, E.; Saatchi, M.; Yekta, A.; Aghamirsalim, M.; Valadkhan, M.; et al. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea 2020, 39, 263–70. [Google Scholar] [CrossRef] [PubMed]
- van den Bosch W., A.; Lemij H., G. Blepharoptosis Induced by Prolonged Hard Contact Lens Wear. Ophthalmology 1992, 99, 1759–65. [Google Scholar] [CrossRef] [PubMed]
- Thean J., H.; McNab A., A. Blepharoptosis in RGP and PMMA Hard Contact Lens Wearers. Clin. Exp. Optom. 2004, 87, 11–4. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Araki, B.; Noso, K.; Kakizaki, H.; Kinoshita, S. Histopathology of Blepharoptosis Induced by Prolonged Hard Contact Lens Wear. Am. J. Ophthalmol. 2006, 241, 1092–96. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Imai, K.; Kinoshita, S. Impact of High Myopia and Duration of Hard Contact Lens Wear on the Progression of Ptosis. Jpn. J. Ophthalmol. 2013, 57, 206–10. [Google Scholar] [CrossRef] [PubMed]
- Battu, VK.; Meyer, DR.; Wobig, JL. Improvement in subjective visual function and quality of life outcome measures after blepharoptosis surgery. Am J Ophthalmol. 1996, 121, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Yamada, H.; Mitani, A.; Shiraishi, A.; Kamao, T.; Goto, T. Improvement of visual fucntion and ocular and systemic symptoms after blepharoptosis surgery. Orbit 2021, 40, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Dannoue, K.; Takagi, S.; Uemura, K.; Takei, A.; Usui, T. Characteristics of astigmatism before and 1 month after blepharoptosis surgery in patients with acquired ptosis. PLoS One. 2021, 16, e0258688. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Goto, T.; Shiraishi, A.; Nakaoka, Y. New Method to Analyze Sagittal Images of Upper Eyelid Obtained by Anterior Segment Optical Coherence Tomography. Orbit 2019, 38, 446–52. [Google Scholar] [CrossRef] [PubMed]
- Kersten R., C.; de Conciliis, C.; Kulwin D., R. Acquired Ptosis in the Young and Middle-Aged Adult Population. Ophthalmology 1995, 102, 924–8. [Google Scholar] [CrossRef] [PubMed]
- Fonn, D.; Holden B., A. Extended Wear of Hard Gas Permeable Contact Lenses Can Induce Ptosis. Clao. J. 1986, 12, 93–4. [Google Scholar] [PubMed]
- Ogasawara, K. Application of Second-Generation Swept-Source Anterior Segment -OCT in the Measurement of Marginal Reflex Distance-1 (MRD-1). Clin. Ophthalmol. 2020, 14, 635–42. [Google Scholar] [CrossRef] [PubMed]
- Kumanomido, T.; Kamiya, K.; Takahashi, M.; Tsujisawa, T.; Hayakawa, H.; Ando, W.; Utsumi, Y.; Shoji, N. Clinical Evaluation of Flat Peripheral Curve Design with Aspherical-Curve and Multi-Curve Hard Contact Lenses for Keratoconus. PLoS One 2022, 17, e0263506. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).