INTRODUCTION:
ASPECTS (Alberta Stroke Program Early CT Score) is a quantitative method to measure early ischemic changes in the brain in a stroke patient. It is a 10-point scoring system based on different anatomical regions supplied by the middle cerebral artery. For the posterior cerebral artery, pc-ASPECTS is used. ASPECTS plays a crucial role in deciding the treatment options for stroke. A higher score (more than 7) suggests that patients will benefit from thrombolytic therapy and have a good prognosis [
1]. A score of 7 or less than 7 indicates excessive ischemic changes in the brain. Such patients will not have any benefit from thrombolytic therapy. The territory of the middle cerebral artery and posterior cerebral is divided into 10 regions, and points are subtracted for areas with early ischemic signs, such as focal swelling or parenchymal hypoattenuation [
2]. The score was originally designed to help identify patients likely to demonstrate the most clinical benefit from intravenous thrombolysis. Subsequently, this score was applied in imaging selection for endovascular therapies to isolate patients with the greatest extent of ischemic damage, in whom recanalization would be futile or harmful. Rapid screening of patients for thrombectomy without the need for more advanced imaging modalities, such as computerised tomography (CT) based perfusion – or magnetic resonance imaging (MRI)–based perfusion, is the main advantage of using ASPECTS in clinical practice [
3].
PURPOSE OF STUDY:
This study aimed to study the effectiveness of the ASPECTS scoring in the assessment of the anterior and posterior cerebral circulation stroke and for standardization of the reporting system using ASPECTS scoring in stroke patients.
METHODOLOGY:
We performed a retrospective study at our centre involving patients referred to NCCT with the clinical diagnosis of acute stroke. Total number of patients: 40, mean age in years: 59 +/- 3 years.
Inclusion criteria: Every consecutive patient (August 2022- November 2022) was included in the study.
Exclusion criteria: Patients with intracranial hemorrhage or hemorrhagic transformation of infarct were excluded.
Scans were performed on a 128-slice multidetector CT PHILIPS Perspective scanner. ASPECTS scoring for anterior and posterior circulation was evaluated separately.
The ASPECTS was determined from two standardized axial CT cuts one at the level of the thalamus and basal ganglion and one adjacent to the most superior margin of the ganglionic structures, such that they were not seen.
On these two sections, which were, by definition, not continuous, the MCA territory was allotted 10 points. A single point was subtracted for an area of early ischemic change, such as focal swelling or parenchymal hypoattenuation, for each of the defined regions. A normal CT scan received an ASPECTS of 10 points.
A similar evaluation for the Posterior cerebral artery was done using axial sections.
A single point was subtracted for an area of early ischemic change, such as focal swelling or parenchymal hypoattenuation, for each of the defined regions. A normal PCA territory score is 10 points.
CASE PRESENTATION:
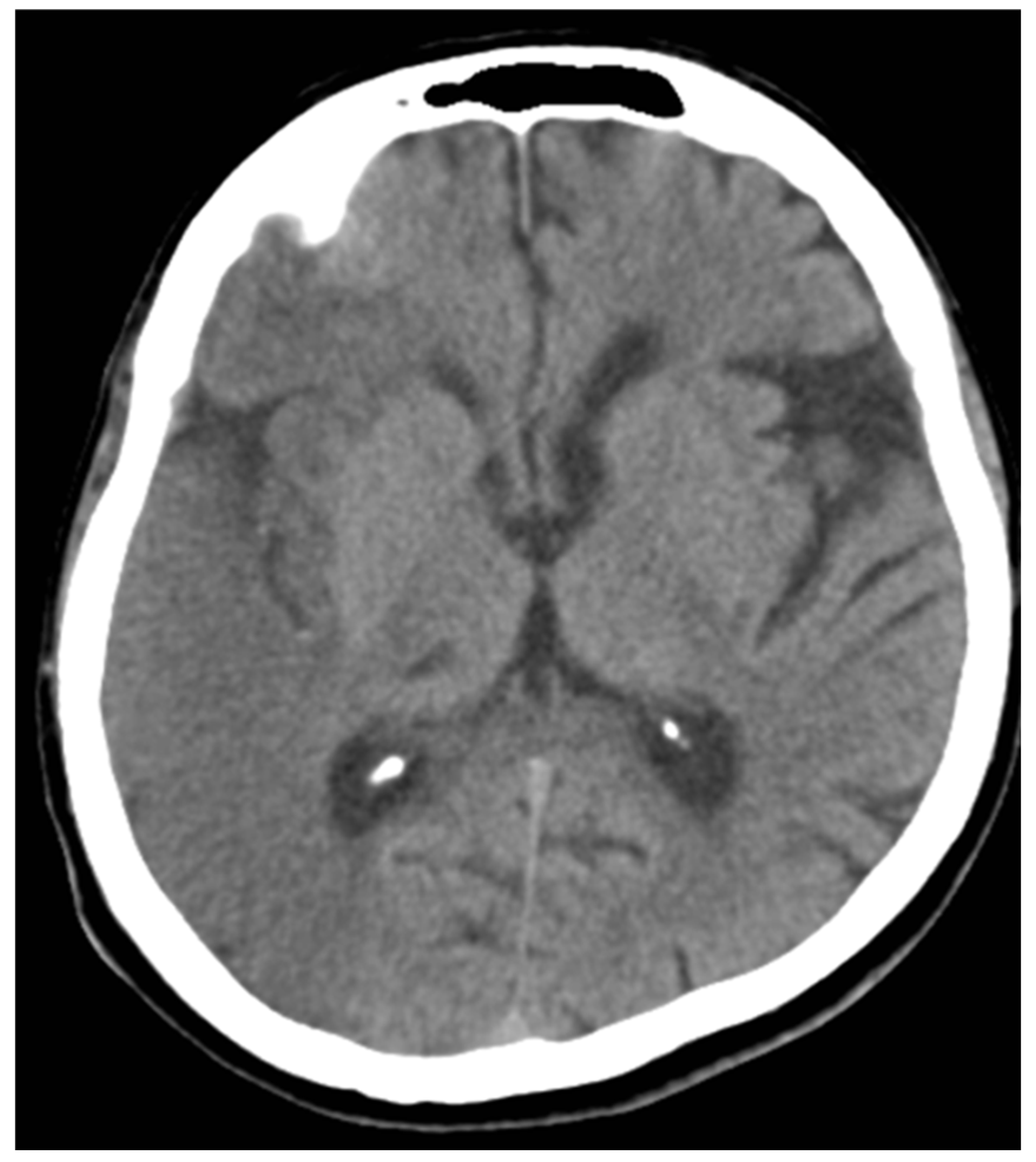
Case 1: A 61-year-old man with complaints of left-sided hemiplegia for 4 hours.
He was presented to the clinic with a loss of consciousness. The CT scan shows a large hypodensity involving the entire right temporal lobe, extending superiorly to the right parietal lobe.
ASPECTS MCA- 6, ASPECTS PCA- 10
The patient was admitted to the ICU, intubated for 2 weeks with no improvement and expired on day 17 of admission.
Figure 1.
NCCT of case 1.
Figure 1.
NCCT of case 1.
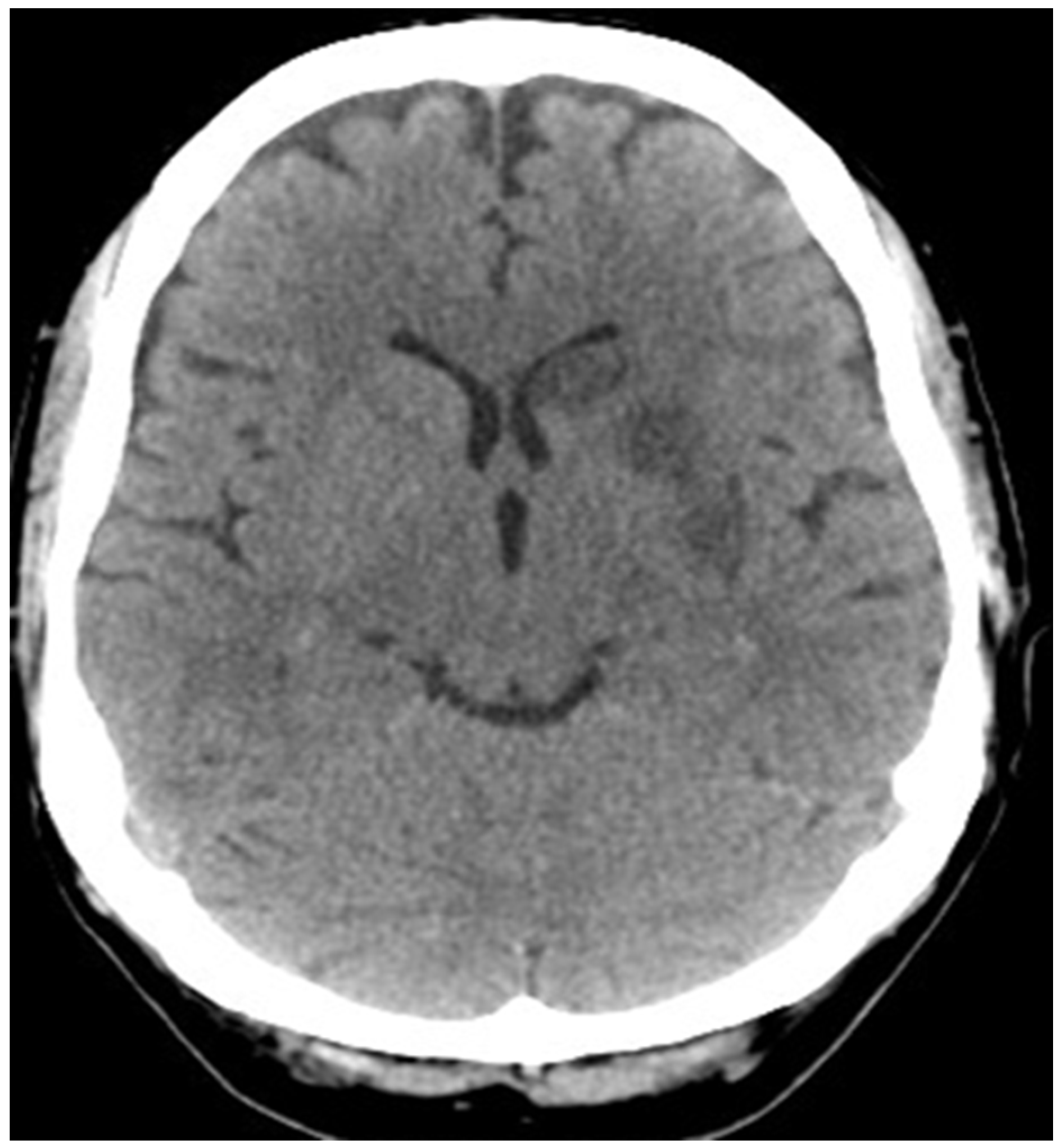
Case 2: A 67 -year-old man with cognitive dysfunction and minimal motor speech disorder since 1 day. CT shows an ill-defined hypodensity in the left caudate and left putamen region.
ASPECTS MCA- 8/10, ASPECTS PCA-10
The patient showed a good prognosis during follow-up after 15 days.
Figure 2.
NCCT of case 2.
Figure 2.
NCCT of case 2.
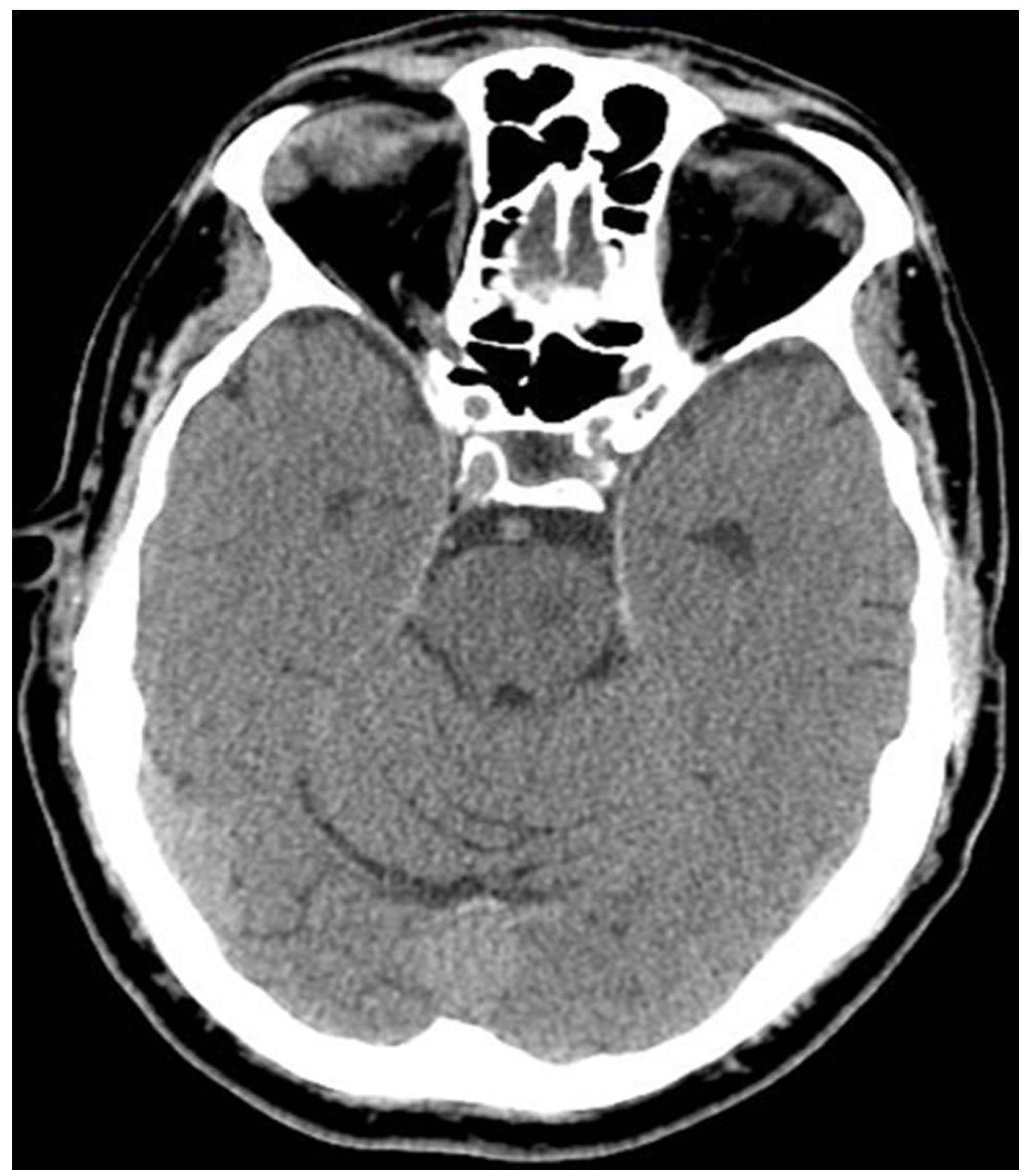
Case 3: A 50-year-old man with left-sided hemiparesis and loss of balance for 1 day. CT shows an ill-defined hypodensity in the right superior cerebellar hemisphere with adjacent sulcal effacement, extending to the left cerebellar hemisphere.
ASPECTS MCA- 10, ASPECTS PCA- 8
The patient showed a good prognosis during follow-up after 15 days.
Figure 3.
NCCT of case 3.
Figure 3.
NCCT of case 3.
Case 4: A 65-year-old man with diplopia and loss of balance for 3 days. CT shows an ill-defined hypodensity in the left half of the Pons region.
ANTERIOR MCA- 10, ASPECTS PCA-8
The patient showed a good prognosis during follow-up after 10 days.
Figure 4.
NCCT of case 4.
Figure 4.
NCCT of case 4.
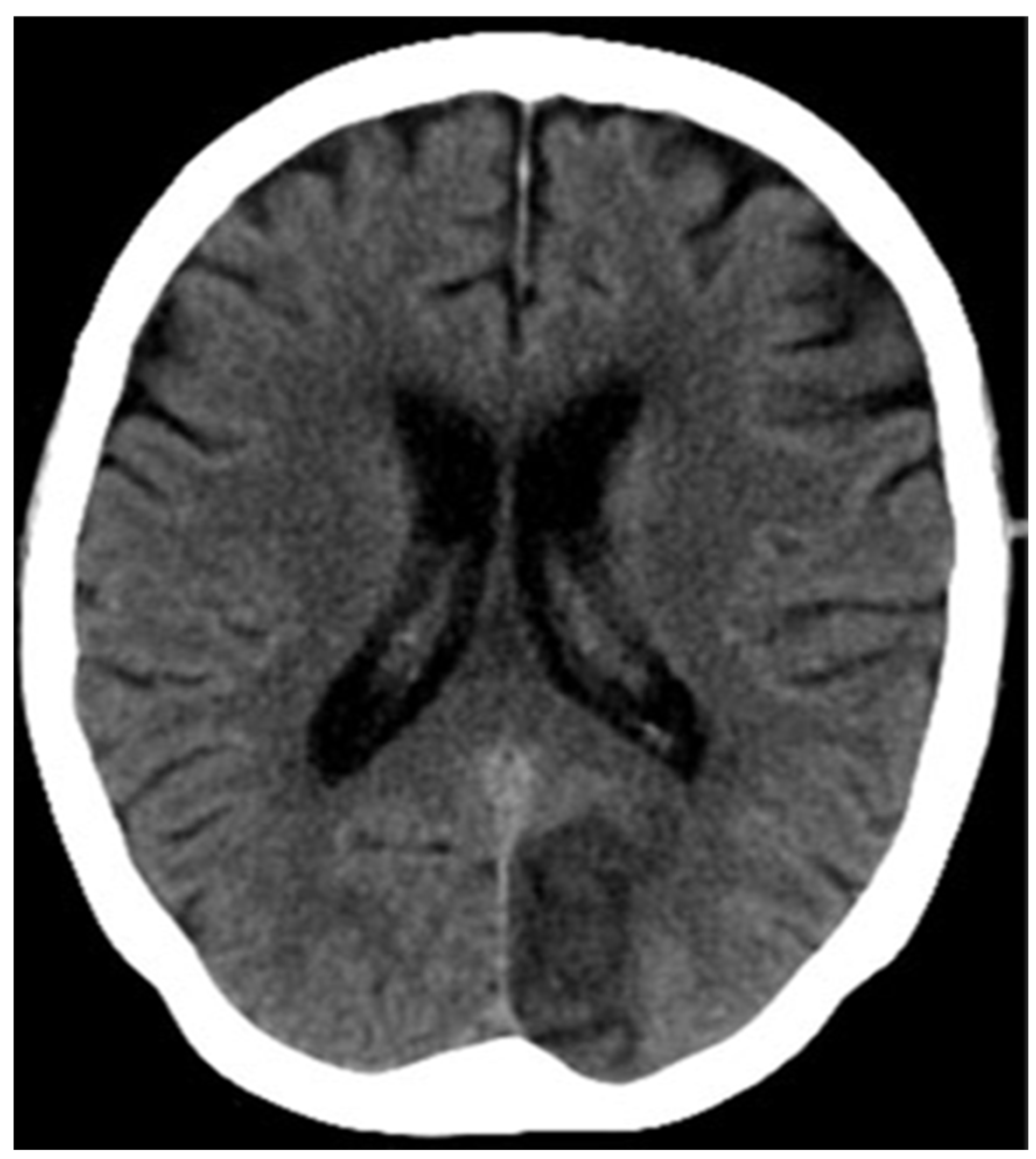
Case 5: A 61-year-old man with a complaint of left-sided hemiplegia for 4 hours,
presented to the clinic with altered sensorium
CT scans show a large hypodensity involving the entire right frontoparietotemporal lobe, insular cortex, putamen and internal capsule.
ASPECTS MCA- 3, ASPECTS PCA- 10
The patient was admitted to the ICU, intubated for 5 days with no improvement and expired on day 5 of admission.
Figure 5.
NCCT of case 5.
Figure 5.
NCCT of case 5.
Case 6: A 67-year-old man with complaints of diplopia, illusions and hallucinations followed by vision loss on his right side for 4 hours, presented to the clinic.
CT scans show a large hypodensity involving the left occipital lobe.
ASPECTS MCA- 10, ASPECTS PCA- 9
The patient showed a good prognosis in terms of visual improvement during follow-up after 1 month.
Figure 6.
NCCT of case 6.
Figure 6.
NCCT of case 6.
RESULTS:
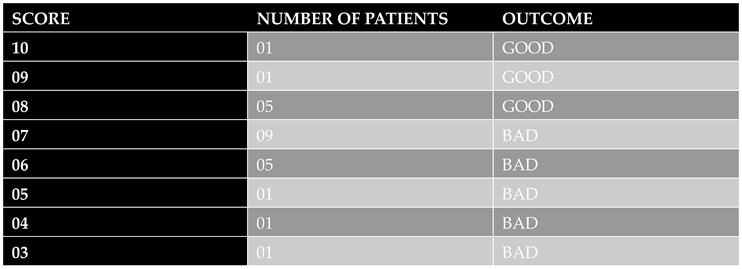
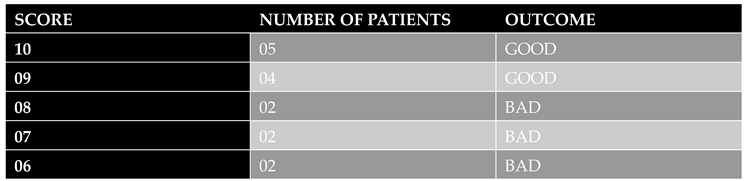
A total of patients 28 ( 70 %) had ASPECTS scores of 7 or more. These patients had good prognoses while admitted in our institution or on sequential follow-up in the OPD.
In our study, a total of 12 patients (30 %) had an ASPECT score of 7 or less. These patients had poor prognoses (no neurological recovery/ death) while admitted to our institution or on sequential follow-up in the OPD.
A total score of 7 or less of either the MCA or PCA indicates a poor prognosis, with minimal benefits of employing thrombolytic therapy.
Table 1.
Score of patients with MCA stroke.
Table 1.
Score of patients with MCA stroke.
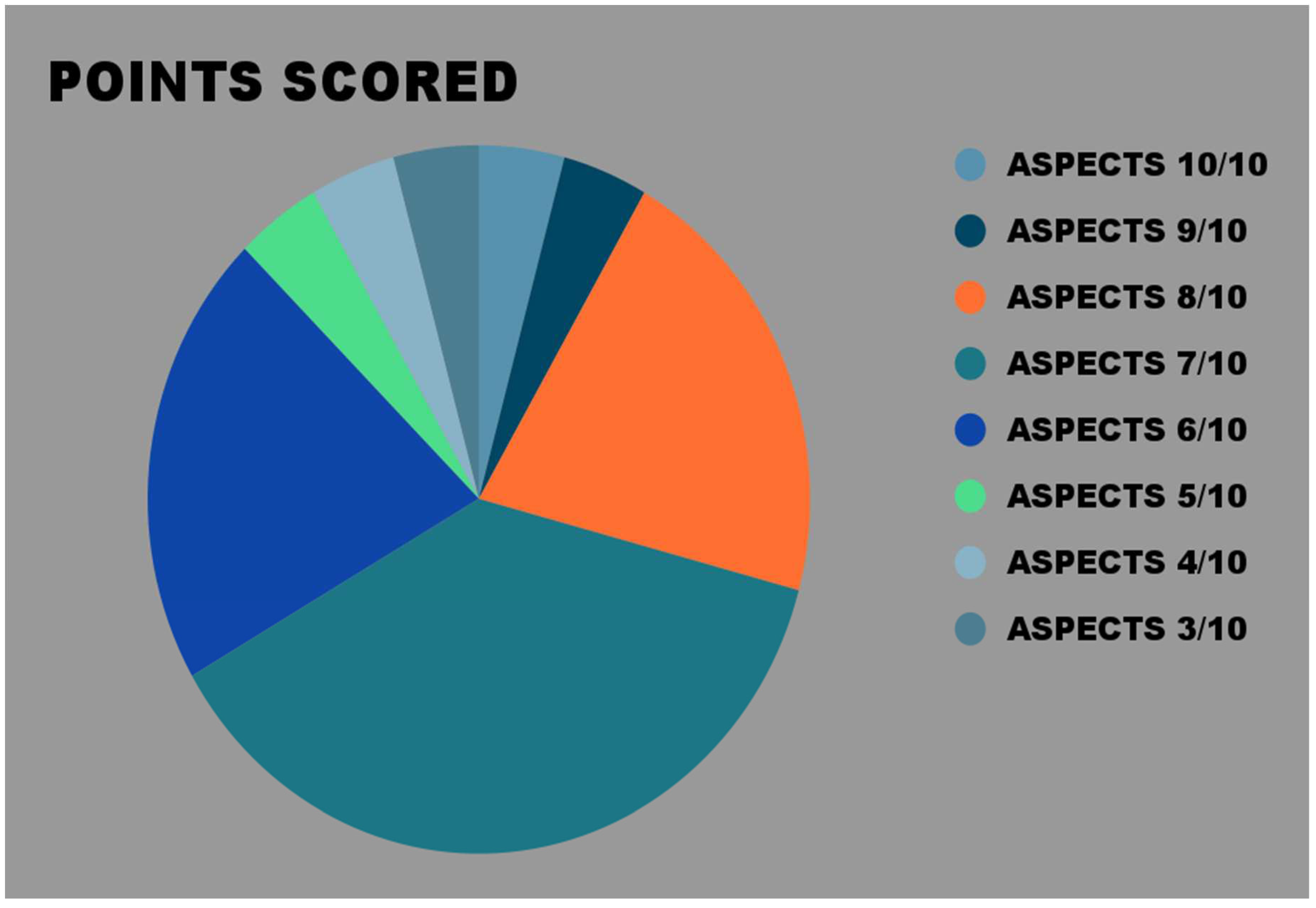
Figure 7.
Chart showing points scored in MCA stroke patients.
Figure 7.
Chart showing points scored in MCA stroke patients.
Table 2.
Score of patients with PCA stroke.
Table 2.
Score of patients with PCA stroke.
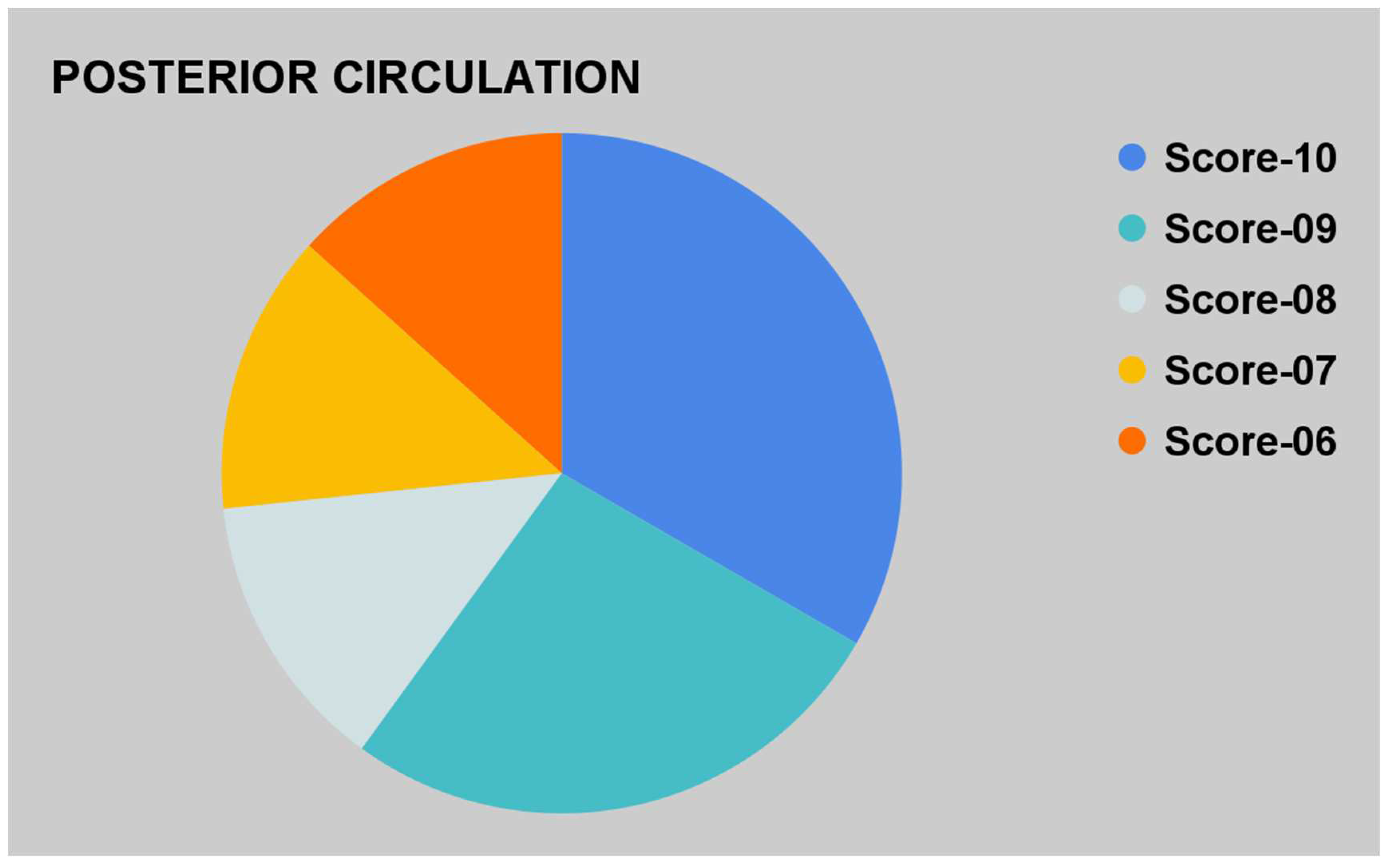
Figure 8.
Chart showing points scored in PCA stroke patients.
Figure 8.
Chart showing points scored in PCA stroke patients.
DISCUSSION AND LITERATURE:
ASPECTS (Alberta Stroke Program Early CT score) is a 10-point quantitative topographic CT scan score used to detect early ischemic changes in MCA (middle cerebral artery) stroke patients. It is also adjusted for PCA (posterior cerebral artery) stroke patients, named pc-ASPECTS [
4]. There are many advantages of using ASPECTS in neuroradiology fields:
Earlier, the 1/3 MCA rule was used to decide whether thrombolysis therapy should be used. This means that if more than 1/3
rd territory of MCA circulation was affected then tissue plasminogen activators were given [
6]. The thrombolysis therapy breaks blood clots and restores blood flow to the brain. Thus, it plays a crucial role in treating stroke patients [
7].
The first ASPECTS score was introduced by researchers at University of Calgary, Canada. Following this, it has undergone many revisions and updates to improve its accuracy and applicability worldwide [
8].
ASPECTS is a 10-point scale that assesses ischemic changes in specific regions of the brain. The following regions are evaluated [
9]:
Caudate
Lentiform
Internal capsule
Insular ribbon
M1 segment: anterior MCA cortex, corresponding to the frontal operculum.
M2 segment: MCA cortex lateral to the insular ribbon, corresponding to the anterior temporal lobe.
M3 segment: posterior MCA cortex, corresponding to the posterior temporal lobe.
M4 segment: anterior MCA territory immediately superior to M1.
M5 segment: lateral MCA territory immediately superior to M2.
M6 segment: posterior MCA territory immediately superior to M3.
Each region is assigned a score from 0-1. A score of 1 means there are no early ischemic changes while a score of 0 means the presence of early ischemic changes. All these scores are summed together and ideally, the score is 10 in people with normal CT scans. Scores lower than or equal to 7 are suggestive of extensive ischemic damage [
1]. Scores more than 7 have a better prognosis due to lesser ischemia. The ones with lower scores are at higher risk of suffering from symptomatic hemorrhage as a side effect of thrombolysis therapy.
Similarly, for posterior circulation strokes, pc-ASPECTS is calculated. It also assesses 10 anatomical regions within the posterior circulation [
4]:
Its interpretation is like the original ASPECTS score.
Despite being a valuable tool in guiding treatment options and predicting patient outcomes, the ASPECTS scoring system still has many limitations [
10]. Firstly, a certain level of clinical skills is needed to correctly diagnose ischemic changes on CT scans. Ischemia must be distinguished from old infarct, brain atrophy, etc. This results in the variation of scores among different observers. Secondly, this scoring system doesn’t take into consideration other factors like the patient’s age, comorbid conditions, time from symptom onset, etc. These also influence treatment outcomes. To overcome these limitations, we should make automated scoring system devices that would eliminate the bias. Also, the addition of other scoring factors can increase the reliability of the ASPCETS scoring system.
CONCLUSION:
The availability and speed of CT scanners make them the modality of choice for assessing acute ischemic stroke in many hospitals. ASPECTS is a CT-based system that provides a more accurate, and practical method for assessing acute ischemic stroke. It is an effective scoring system in emergency radiology practice with accuracy in the delineation of infarcted areas by easy visual mapping and better standardization. It predicts the outcomes of thrombolytic therapy in stroke patients. It also provides for easy and efficient communication with the treating physicians, which is very crucial in acute stroke and should be documented in every acute stroke report. However, some pitfalls of this system must be addressed to make it more effective. The variation of scores among observers and the lack of inclusion of other factors in the scoring system are some such limitations of this study.
Funding
None of the authors are financially interested in any of the products, devices or drugs mentioned in this manuscript.
Institutional Review Board Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pexman JHW, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for Assessing CT Scans in Patients with Acute Stroke. AJNR Am J Neuroradiol [Internet]. 2001 [cited 2023 Dec 29];22(8):1534. Available from: /pmc/articles/PMC7974585/.
- Mokin M, Primiani CT, Siddiqui AH, Turk AS. ASPECTS (Alberta Stroke Program Early CT Score) Measurement Using Hounsfield Unit Values When Selecting Patients for Stroke Thrombectomy. Stroke [Internet]. 2017 Jun 1 [cited 2023 Dec 29];48(6):1574–9. Available from: https://www.ahajournals.org/doi/abs/10.1161/STROKEAHA.117.016745. [CrossRef]
- Pop NO, Tit DM, Diaconu CC, Munteanu MA, Babes EE, Stoicescu M, et al. The Alberta Stroke Program Early CT score (ASPECTS): A predictor of mortality in acute ischemic stroke. Exp Ther Med [Internet]. 2021 Sep 27 [cited 2023 Dec 29];22(6). Available from: /pmc/articles/PMC8515558/. [CrossRef]
- Kuybu O, Tadi P, Dossani RH. Posterior Cerebral Artery Stroke. StatPearls [Internet]. 2023 Aug 8 [cited 2023 Dec 29]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK532296/.
- Maegerlein C, Fischer J, Mönch S, Berndt M, Wunderlich S, Seifert CL, et al. Automated calculation of the Alberta stroke program early CT score: Feasibility and reliability. Radiology [Internet]. 2019 Apr 1 [cited 2023 Dec 29];291(1):141–8. Available from: https://pubs.rsna.org/doi/10.1148/radiol.2019181228. [CrossRef]
- Kalafut MA, Schriger DL, Saver JL, Starkman S. Detection of Early CT Signs of >1/3 Middle Cerebral Artery Infarctions. Stroke [Internet]. 2000 [cited 2023 Dec 29];31(7):1667–71. Available from: https://www.ahajournals.org/doi/abs/10.1161/01.str.31.7.1667. [CrossRef]
- Wood L. Thrombolysis for acute stroke. JAMA [Internet]. 1996 Apr 3 [cited 2023 Dec 29];275(13):983; author reply 984-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8596248. [CrossRef]
- Menon BK, Puetz V, Kochar P, Demchuk AM. ASPECTS and other neuroimaging scores in the triage and prediction of outcome in acute stroke patients. Neuroimaging Clin N Am [Internet]. 2011 May [cited 2023 Dec 29];21(2):407–23. Available from: https://pubmed.ncbi.nlm.nih.gov/21640307/.
- Bell D, Sair H. Alberta stroke programme early CT score (ASPECTS). Radiopaedia.org. 2008 Nov 7; Available from: https://radiopaedia.org/articles/alberta-stroke-programme-early-ct-score-aspects.
- Schröder J, Thomalla G. A Critical Review of Alberta Stroke Program Early CT Score for Evaluation of Acute Stroke Imaging. Front Neurol [Internet]. 2016 Jan 12 [cited 2023 Dec 29];7(JAN):245. Available from: /pmc/articles/PMC5226934/.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).