1. Introduction
Combating COVID-19 has posed a significant challenge during the pandemic. Individual preventive actions and community involvement played a crucial role in reducing transmission, especially in early epidemic waves when vaccines were not yet available [
1].
These actions included the use of personal protective equipment like masks and practicing hand hygiene; environmental measures such as disinfection and improving ventilation, maintaining social distancing in public places, schools closures, and imposing travel restrictions [
1]. The use of facemasks has been one of the main individual preventive practices to reduce COVID-19 transmission [
2,
3] . Additionally, quarantine was an effective intervention to reduce virus transmission, as demonstrated in Wuhan, where its early and strict application significantly reduced the reported cases [
4]. One study indicated a 35% reduction in COVID-19 incidence with ventilation measures in classrooms [
5], though assessing ventilation independently is complex [
6]. Non-pharmacological interventions are challenging as they require changes in personal behavior. However, a systematic review concluded that combining such measures can significantly reduce infections and transmission of COVID-19 [
7].
The implementation of these measures has varied based on the epidemiological situation of the disease and the political guidelines of each country, as well as the public adherence to the recommendations from authorities [
8]. Adoption of preventive measures depends on the population's knowledge [
9] and individual perception of disease risk. Studies show that individuals with low risk perception are less likely to follow preventive measures [
10], while those with chronic diseases have higher adherence to care [
11].
The World Health Organization (WHO) has provided recommendations according to the epidemiological stage of the disease. Currently, some recommendations persist due to the endemicity and epidemic cycles of SARS-CoV-2. These WHO guidelines focus on individual health protection and preventing the spread of the disease including maintaining a physical distance of at least one meter, wearing masks when physical distancing is not possible and in poorly ventilated environments, frequent handwashing, covering the mouth and nose with the elbow or tissue when coughing or sneezing, and isolating in case of illness [
12].
Upholding these preventive measures is a challenge even with the availability of vaccines [
13], due to the emergence of new SARS-COV-2 variants reducing vaccines effectiveness and the fact that vaccination does not prevent mild infections, as well as low vaccination coverage [
14,
15].
Variations in adherence to non-pharmacological measures (NPMs) have been described throughout the pandemic, due to vaccination, decreased risk perception, or pandemic fatigue [
16,
17,
18]. In Chile, the Ministry of Health followed up COVID 19 patients and their contacts during the pandemic. A study in Chile showed a decrease in compliance with some NPMs in the post-vaccination stage in 2021, but the 2020 measurement (pre-vaccination) was retrospective. No studies in Chile have measured adherence to NPMs during the vaccination stage, especially with the implementation of booster doses for the entire population. Understanding adherence to NPMs for COVID-19 is critical as evidenced by the 16% increase in SARS-CoV-2 infections in Chile in November [
19].
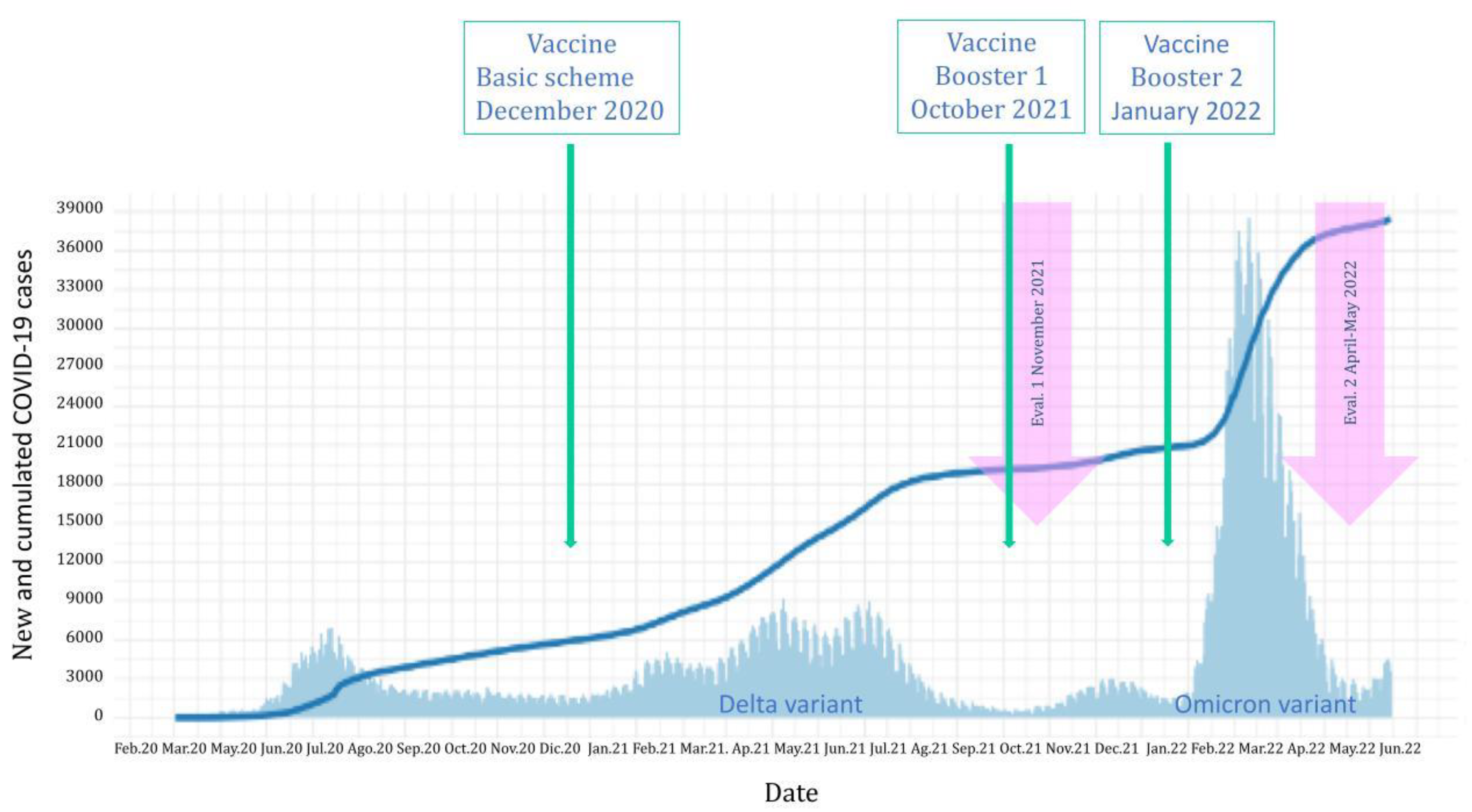
This research aims to explore public adherence to non-pharmacological measures (NPMs) across two distinct stages of the COVID-19 pandemic, using a cohort from 2021 to 2022 in a country with high vaccine coverage levels. The first stage in 2021 coincided with the completion of the basal vaccination schedule and the circulation of the Delta variant. Conversely, the second stage in 2022 took place amidst the implementation of vaccine boosters and the circulation of the Omicron variant. (November 2021 and April-May 2022).
The analysis of behavioral changes over time and the identification of factors that influence compliance with NPMs provide a deeper understanding of how individuals respond to health crises like the COVID-19 pandemic. This study is particularly relevant in the context of vaccine rollouts and booster implementations, as it highlights the ongoing importance of NPMs even in the presence of pharmacological interventions. The findings from Chile, which has closely followed WHO recommendations and achieved high vaccination rates, offer a unique perspective on the effectiveness of various strategies. Understanding these dynamics is crucial not only for managing the current pandemic, but also for preparing for future health emergencies. By learning from these patterns of adherence, we can develop more effective approaches to prevent and mitigate the impact of new disease outbreaks, ensuring a more resilient public health response in the future.
2. Materials and Methods
We followed 386 individuals aged 7 and older who participated in three seroprevalence studies against SARS-CoV2 between 2020 and 2022 in two Chilean cities: Talca and Coquimbo - La Serena. Self-care measures were assessed in the second (November 2021) and the third round (April-May 2022) using the same core questionnaire in both rounds. Epidemiological characteristics in these two years were different (
Figure 1). The questions included frequency of (a) hand washing; (b) avoiding handshakes, kisses, or hugs; (c) ventilating the environment where you are; (d) mask usage in public or enclosed places less than 1 meter apart. In addition, three other questions were used differently in each round to capture different stages of the recommendations defined by the health authority.
To describe the result, the following scoring was considered for the answers: never=0 points; rarely=1 point; frequently=3 points, and always=4 points. The total score was evaluated continuously with central tendency and position measures. Cut-off points were established to compare both rounds: 14 as a low level, 15-19 points as a medium level, and 20 or more as a high level. Additionally, the difference in change between self-care measures from one round to the next was assessed.
Finally, after analyzing the response variable for both rounds with a normality test, non-parametric bivariate analysis was performed: Wilcoxon rank-sum (Mann-Whitney) test for categorical variables, and Kruskal-Wallis for variables with three or more categories. Additionally, we evaluated whether there was contact from the health authority for isolation following a COVID-19 diagnosis and quarantine for being a close contact across the three study rounds.
3. Results
In our sample, 52.3% were residents of Talca and 67.4% were women. The median age was 49 years (IQR=33-64). 85.8% were covered by public health insurance, and 9.6% identified as belonging to an ethnic group. 53.3% of people aged 18 and over completed secondary education and 22.2% have completed professional education.
During the 2021 evaluation, 35 individuals received a positive COVID-19 diagnosis and 88 in 2022. Health personnel contacted 94.3% in 2021 and 81.8% in 2022 to assess isolation status. The cases not contacted in 2021 were mainly women and residents of Talca. In 2022, cases not contacted were predominantly women, people between 30 to 39 years old, and residents of Coquimbo-La Serena. There were no significant differences for these variables in the follow-up of COVID-19 cases in both years.
Among the participants who were advised to remain in quarantine for being in contact with a COVID-19 positive case 83.0% were contacted by health personnel to assess quarantine compliance in 2021 and 33.3%. in 2022. Contacts not reached out in 2021 were mainly men, individuals with basic education, and residents of Coquimbo-La Serena. In 2022, most contacts not reached out were also men, people between 30 to 49 years old and over 60 years old, also residents of Coquimbo-La Serena. In both rounds, there were no significant differences for these variables in the monitoring of COVID-19 contacts.
Table 1 presents the frequency of preventive NPMs, total and separated according to diagnosis of COVID-19. In 2021, the prevention practices that participants indicated they "always" performed were wearing masks in public places (95.9%), complying with step-by-step mobility restrictions (95.1%), and adhering to curfew (94.6%). For the 2022 assessment, it was also wearing masks in public places and wearing masks in public with people outside the household (90.7% and 89.9%, respectively).
However, the measures with lower levels of high compliance were wearing masks with people outside the household (55.3%) and avoiding greetings with handshakes, kisses, or hugs (61.4%), the latter also having the lowest frequency for 2022 (59%). The only measure that was individually related to the COVID-19 diagnoses was the ventilation of closed spaces (p=0.006), people who rarely ventilated spaces presented the disease in a higher proportion, compared to those who ventilated frequently or often.
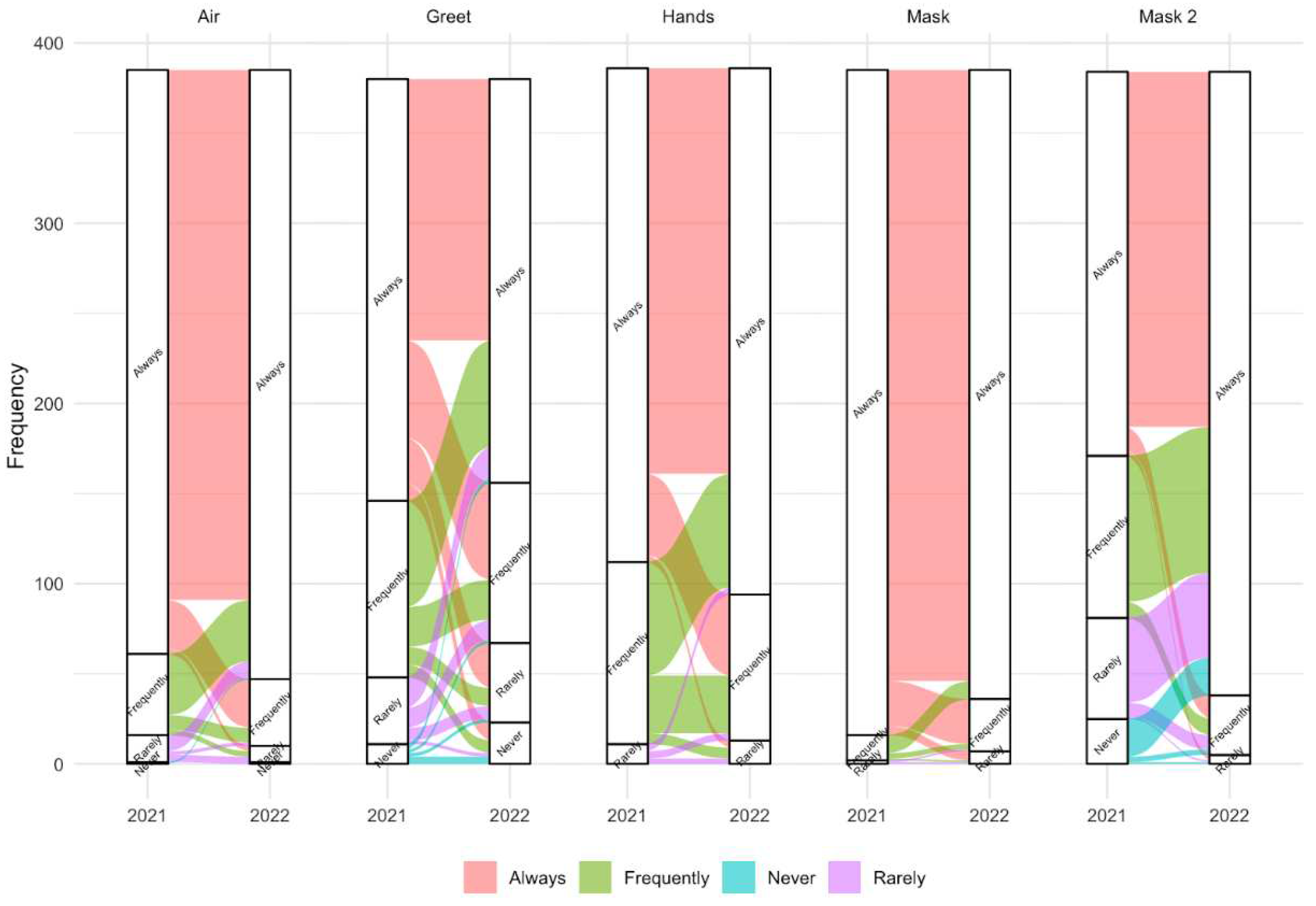
Figure 2 represents the changes experienced by people followed from one year to the next, concerning the adoption of non-pharmacological preventive measures for the spread of COVID-19. We observed that the most used measure was the use of masks in public spaces, and it was also the one that showed the least change in the second evaluation. Then follows ventilation of closed spaces, whose variation in the second year indicates that people who always ventilated changed their behavior towards frequently and a greater number of those who ventilated frequently or rarely moved to always ventilate. Hand washing presents a pattern in which people who always did it switched to washing their hands frequently, many of those who did it frequently continued doing it or started always washing their hands in the second measurement.
Even a certain number of people who rarely washed their hands in 2021 started to always do so in 2022. The use of masks with people outside of household members presents an interesting pattern, given that a low proportion of people lower their level of use in the second year and a relatively high proportion of people increase their level of use in the second evaluation, from frequently, rarely and even from never to always. Finally, regarding the way of greeting, it is the measure that presents the greatest variety of changes from one year to the next, minimally altering the frequencies of the categories between one year and the next.
Regarding the score of preventive practices, significant differences were observed in 2021 according to the city, given that the city of Coquimbo-La Serena presented a lower median score for preventive practices; in the 2022 evaluation, the score improved, equaling Talca. Similarly, in the se2021 assessment, men were observed with a lower median score, which subsequently increased and equaled that of women. For both years, it was observed that the age groups of 7-19 and 20-29 years presented lower scores in relation to the other ages. In 2022, the age groups under 49 years old increased the score, however, in those over 50 years old, no changes in the median were observed. In 2021, a higher score was observed in people who had overweight and obese BMI, that situation was not present in 2022 where the score is equal. In both years a higher score was observed in those with some comorbidity. Likewise, differences were observed depending on the dose of vaccine administration for each round. For the 2021 measurement, having administered a booster indicated a higher score, however, for the 2022, it was observed (except for the unvaccinated), that the more doses of vaccine the score was higher. For further details, see
Table 2.
The results of the multiple linear regression model are presented in
Table 3. The factor that predicted preventive practices in the 2021 assessment was gender. Women scored 0.61 points higher than men on average. In the subsequent evaluation, the preventive measures score was solely explained by age, where individuals aged 30-49 years exhibited the highest scores. This difference was more pronounced when compared to other age groups, especially those aged 50-59 years.
4. Discussion
The score of adherence to non-pharmacological measures (NPMs) recommended against SARS-CoV-2 increased from 2021 to 2022. Being a woman was associated with a higher score in preventive behaviors at both time points, and, for 2022, being a young adult (30-49 years) was predictive of the use of NPMs. Conversely, the proportion of COVID-19 cases isolated by the health authority decreased from 94.3% in 2021 to 81.8% in 2022.
In our study, 46.1% of participants improved their adherence to preventive measures during the pandemic period, while 29% maintained them. A study conducted in Thailand found that, upon the implementation of vaccination, adherence improved by 12-18% in social activity avoidance, physical distancing, and hand washing (in 2021 and 2022), which is lower than in our study. Moreover, the proportion of individuals who maintained preventive measures was 70-90%, higher than in our study [
20]. Another study in Israel showed that mask usage was maintained at 75.7%, and social distancing at 48.8%. However, the proportion showing improvement was only 3.2% for mask use and 4.3% for social distancing [
21]. Unlike the studies mentioned above, our study did not specifically hypothesize changes in adherence due to vaccination, as the first measurement of preventive behavior was conducted in 2021 when basal scheme coverage was at 80%. In 2022, coverage of the basal scheme exceeded 90%, and 60% of the population received one or two boosters. Thus, we observed that despite the increase in vaccination coverage, adherence to preventive measures was higher, similar to findings reported in the Wright et al. study in the United Kingdom [
22].
On the one hand, several studies have indicated that non-pharmacological measures reduced the incidence of COVID-19 [
23,
24]. In contrast, between the two periods in which we measured adherence to non-pharmacological measures (NPMs), the incidence of COVID-19 reported by the Chilean Ministry of Health increased[
25,
26,
27]. This increase could be attributed to the arrival of the Omicron variant in Chile in December 2021, noted for its rapid transmissibility and mutational capacity, which is associated with a potential for immune escape [
28]. It quickly became the dominant circulating variant [
29]. In this context, the increased risk perception among the Chilean population may have contributed to greater adherence to the preventive behaviors reported in this study, especially since the study was conducted during a new epidemic wave.
Mask use in public places was the behavior with the highest adherence in both 2021 (95.9%) and 2022 (90.7%). Indeed, some studies have found that mask use is the measure with the highest adherence [
8,
15]. One study reported a mask use proportion of 81.9% between 2020-2022 and also noted an increase in the likelihood of its use when mandatory [
30]. Although it was the measure with the highest adherence, we observed a slight decrease in the proportion of use by 2022, differing from Petherick et al., who reported an increase in adherence to mask-wearing over time. However, their study was conducted in the first year of the pandemic when awareness was higher [
17]. Additionally, when analyzing the relationship between preventive measures and having contracted COVID-19, ventilating the home was the only measure that showed a statistically significant association, but only in 2022. Those who ventilated less frequently had a higher proportion of the disease [
17]. This reinforces the notion that air is a mode of transmission of this disease, making this behavior effective in preventing COVID-19 [
31]. Avoiding greetings with handshakes, kisses, or hugs remained with low adherence compared to the other measures asked, at both times of the survey, which may be due to cultural practices in Chile. A study in Ethiopia showed a similar proportion to the second wave of our study (53.8%) [
32].
In both series of this study, women were the key explainers of the score for non-pharmacological measures (NPMs), exhibiting higher adherence than men. Regarding the adoption of protective masks and attitudes towards respiratory epidemics, a pre-COVID-19 study found that women were more inclined to adopt NPMs such as wearing masks, washing hands, and avoiding public transportation [
13]. Gender, followed by age, had a strong association with mask use [
33]. Studies from various countries have demonstrated that men adhere less to preventive behavior, being less likely to use face masks, wash their hands, and more likely to breach rules of physical distancing and isolation [
34]. In our study, during the first measurement, adults (over 30 years of age) had the best score; in the second measurement, all age groups under 50 years improved their score, with the best score observed in adults aged 30-49 years. This change in preventive behavior has been indicated in other studies as well [
34]. This could be attributed to the fact that this demographic is more likely to be working and commuting, hence more aware of the importance of health precautions.
In the bivariate analysis, we found significant differences between cities; in 2021, Coquimbo presented a lower score than Talca. This may be due to structural determinants of health such as poverty; La Serena/Coquimbo has an 11.8% income poverty rate, while Talca has 8% [
35]. These factors could affect the ability to purchase masks and necessitate working outside the home. Additionally, having comorbidity was significantly associated with higher adherence to NPM, likely due to an increased perception of disease risk [
36], similar to a U.S. study showing that adults with comorbidities were more likely to adhere to preventive measures [
11]. Lastly, those who complied with the administration of more vaccine doses than the current recommendation were always more adherent to preventive measures, demonstrating a coherent attitude towards prevention [
37,
38]. A high proportion of COVID-19 cases and contacts were followed up in both 2021 and 2022 by the health authority. Although it was lower in 2022, probably due to the 2 to 3 times higher frequency of COVID-19 cases [
25,
26,
27], prioritizing case follow-up over contacts [
39]. In January 2022, the Chilean Minister of Health delegated the responsibility for contact tracing to individuals with COVID-19 [
40].
The limitations of this study include that preventive behaviors were self-reported and may be affected by recall and social desirability bias, although interviewers were trained to minimize it. The strengths of this study include a population-based sample with an adequate response rate (63%), allowing for the follow-up of participants under fluctuating epidemic conditions.
5. Conclusions
Public health measures intended to minimize the spread of infectious diseases are essential, even in the presence of vaccination. Mask-wearing was the most utilized measure, characterized by high acceptability and relatively low cost compared to vaccines. Health authorities should improve adherence among the population, with special priority given to those less likely to adhere. Encouraging men and young people to adhere to preventive measures should be emphasized in risk communication strategies. Preventive measures, particularly air ventilation, should be promoted for all airborne diseases. Simultaneously, it is necessary to continue research to better understand the factors that predict and enhance adherence to preventive behaviors.
Author Contributions
Considering CRediT taxonomy, Conceptualization MRS, LN, and PR; data curation, PR, MA and LC; formal analysis, PR, MA, and XM; funding acquisition, MRS and LN; Investigation, MRS and LN; methodology, MRS, LN, and PR; software, PR and MA; supervision MRS; visualization PR and MA; writing - original draft PR and LN; writing - review & editing, PR, LN, MA, MRS, and XM. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Chilean National Research Agency, Grants code COVID-19-0589 and FONIS SA21I0009. The research has been supported by WHO Unity Studies, a global sero-epidemiological standardization initiative, with funding to WHO by the COVID-19 Solidarity Response Fund and the German Federal Ministry of Health (BMG) COVID-19 Research and Development Fund.
Institutional Review Board Statement
This research was approved by the Ethics Committees of the Universidad de Talca and the Facultad de Medicina of the Universidad Católica del Norte in all the three phases. First round Statement numbers 34-2020 and 21-2020; second round, 38-2021 and 34-2021; and third round Statement numbers 50-2021 and 38-2021, respectively.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The authors acknowledge the WHO for the donation of tests to measure SARS-CoV-2 antibodies.
Conflicts of Interest
The authors declare no conflict of interest. At the same time, the funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Etemad K, Mohseni P, Shojaei S, Mousavi SA, Taherkhani S, Atatalab FF, et al. Non-Pharmacologic Interventions in COVID-19 Pandemic Management; a Systematic Review. Arch Acad Emerg Med 2023, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Andrejko KL, Pry JM, Myers JF, Fukui N, DeGuzman JL, Openshaw J, et al. Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021. MMWR Recomm Reports 2022, 71, 212–216. [Google Scholar] [CrossRef]
- Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: Systematic review and meta-analysis. BMJ 2021, 375, 1–15. [Google Scholar] [CrossRef]
- Cui Q, Hu Z, Li Y, Han J, Teng Z, Qian J. Dynamic variations of the COVID-19 disease at different quarantine strategies in Wuhan and mainland China. J Infect Public Health 2020, 13, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Gettings J, Czarnik M, Morris E, Haller E, Thompson-Paul AM, Rasberry C, et al. Mask Use and Ventilation Improvements to Reduce COVID-19 Incidence in Elementary Schools — Georgia, November 16–December 11, 2020. MMWR Morb Mortal Wkly Rep 2021, 70, 779–784. [Google Scholar] [CrossRef] [PubMed]
- 6. Madhusudanan A, Iddon C, Cevik M, Naismith JH, Fitzgerald S. Non-pharmaceutical interventions for COVID-19: A systematic review on environmental control measures. Philos Trans R Soc A Math Phys Eng Sci, 2023; 381. [CrossRef]
- Silubonde-Moyana TM, Draper CE, Norris SA. Effectiveness of behavioural interventions to influence COVID-19 outcomes: A scoping review. Prev Med (Baltim) 2023, 172, 107499. [Google Scholar] [CrossRef] [PubMed]
- Tong KK, Chen JH, Yu EW yat, Wu AMS. Adherence to COVID-19 Precautionary Measures: Applying the Health Belief Model and Generalised Social Beliefs to a Probability Community Sample. Appl Psychol Heal Well-Being 2020, 12, 1205–1223. [Google Scholar] [CrossRef] [PubMed]
- Beca-Martínez MT, Romay-Barja M, Falcón-Romero M, Rodríguez-Blázquez C, Benito-Llanes A, Forjaz MJ. Compliance with the main preventive measures of COVID-19 in Spain: The role of knowledge, attitudes, practices, and risk perception. Transbound Emerg Dis 2022, 69, e871–82. [Google Scholar] [CrossRef] [PubMed]
- Wise T, Zbozinek TD, Michelini G, Hagan CC, Mobbs D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States: COVID-19 risk perception and behavior. R Soc Open Sci 2020, 7. [Google Scholar] [CrossRef]
- Islam JY, Vidot DC, Camacho-Rivera M. Determinants of COVID-19 preventive behaviours among adults with chronic diseases in the USA: An analysis of the nationally representative COVID-19 impact survey. BMJ Open 2021, 11, 1–9. [Google Scholar] [CrossRef]
- World Health Organization. Infection prevention and control in the context of coronavirus disease (COVID-19): a living guideline. 2023, 78.
- Aho Glele LS, de Rougemont A. Non-Pharmacological Strategies and Interventions for Effective COVID-19 Control: A Narrative Review. J Clin Med 2023, 12. [Google Scholar] [CrossRef]
- Wu N, Joyal-Desmarais K, Ribeiro PAB, Vieira AM, Stojanovic J, Sanuade C, et al. Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: findings from a rapid living systematic evidence synthesis and meta-analysis up to December, 2022. Lancet Respir Med 2023, 11, 439–452. [Google Scholar] [CrossRef]
- Si R, Yao Y, Zhang X, Lu Q, Aziz N. Investigating the Links Between Vaccination Against COVID-19 and Public Attitudes Toward Protective Countermeasures: Implications for Public Health. Front Public Heal 2021, 9, 1–11. [Google Scholar] [CrossRef]
- Agurto-Ramírez A, Pino-Rosón C, Ayala A, Falcón M, Rodríguez-Blázquez C, Forjaz MJ, et al. Association Between Pandemic Fatigue and Disease Knowledge, Attitudes, Concerns, and Vaccination Intention at Two Key Moments of the COVID-19 Pandemic. Int J Public Health 2023, 68, 1–10. [Google Scholar] [CrossRef]
- Petherick A, Goldszmidt R, Andrade EB, Furst R, Hale T, Pott A, et al. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat Hum Behav 2021, 5, 1145–1160. [Google Scholar] [CrossRef]
- 18. Gassen J, Nowak TJ, Henderson AD, Weaver SP, Baker EJ, Muehlenbein MP. Longitudinal changes in COVID-19 concern and stress: Pandemic fatigue overrides individual differences in caution. J Public Health Res. [CrossRef]
- Ministerio de Salud de Chile. Reporte diario 30 de noviembre de 2021. Santiago: 2021.
- Ngamchaliew P, Kaewkuea N, Nonthasorn N, Vonnasrichan T, Rongsawat N, Rattanachai L, et al. Changes in preventive behaviour after COVID-19 vaccination in Thailand: a cross-sectional study. BMC Public Health 2022, 22, 1–12. [Google Scholar] [CrossRef]
- 21. Rahamim-Cohen, D; Gazit, S; Perez, G; Nada, B; Moshe, SB; Mizrahi-Reuvenil ,M; Azuri, J; Patalon T. Survey of Behaviour Attitudes Towards Preventive Measures Following COVID-19 Vaccination. MedRxiv. [CrossRef]
- Wright L, Steptoe A, Mak HW, Fancourt D. Do people reduce compliance with COVID-19 guidelines following vaccination? A longitudinal analysis of matched UK adults. J Epidemiol Community Health 2022, 76, 109–115. [Google Scholar] [CrossRef]
- Horga NG, Cirnatu D, Kundnani NR, Ciurariu E, Parvu S, Ignea AL, et al. Evaluation of Non-Pharmacological Measures Implemented in the Management of the COVID-19 Pandemic in Romania. Healthc 2022, 10, 1–13. [Google Scholar] [CrossRef]
- Abbas Alshami; Steven Douedi; Daniel Shenouda; Ali Nadhim; Joseph Varon; , Patel Swapnil. Incidence of Influenza Virus Pneumonia During the Time of Coronovirus-2019 Pandemic. Chest 2021, 4, A589. [Google Scholar] [CrossRef]
- Ministerio de Salud de Chile. Reporte Diario. 15 De Noviembre De 2021. Santiago: 2021.
- MInisterio de Salud de Chile. Reporte Diario. 15 de abril de 2022. 2022. [Google Scholar]
- Ministerio de salud de Chile. Reporte Diario. 15 de mayo de 2022. 2022. [Google Scholar]
- Hormazábal J, Nuñez-Franz L, Rubilar P, Apablaza M, Vial C, Cortés LJ, et al. Factors influencing neutralizing antibody response to the original SARS-CoV-2 virus and the Omicron variant in a high vaccination coverage country, a population-based study. Vaccine X 2023, 15, 1–7. [Google Scholar] [CrossRef]
- Vitiello, Antonio; Ferrara, Francesco; Auti, Amogh M; Marina, Di Domenico, Marina; Boccellino M. Advances in the Omicron variant development. J Intern Med 2022, 1, 81–90. [Google Scholar] [CrossRef]
- Binka M, Adu PA, Jeong D, Vadlamudi NK, García HAV, Mahmood B, et al. The Impact of Mask Mandates on Face Mask Use During the COVID-19 Pandemic: Longitudinal Survey Study. JMIR Public Heal Surveill 2023, 9, 1–14. [Google Scholar] [CrossRef]
- Fadaei, A. Importance of ventilation to prevent spread of covid 19. Eur J Sustain Dev Res 2021, 5, em0157. [Google Scholar] [CrossRef]
- Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS One 2020, 15, 1–15. [Google Scholar] [CrossRef]
- Looi, KH. Explicating gender disparity in wearing face masks during the COVID-19 pandemic. BMC Public Health 2022, 22, 1–9. [Google Scholar] [CrossRef]
- Urbán R, Király O, Demetrovics Z. Who complies with coronavirus disease 2019 precautions and who does not? Curr Opin Psychiatry 2021, 34, 363–368. [Google Scholar] [CrossRef]
- Biblioteca del Congreso Nacional. Reportes Comunales. Indicadores demográficos 2023. https://www.bcn.cl/siit/reportescomunales/comunal.html?unidad=Comunales&anno=2023.
- Chong YY, Chien WT, Cheng HY, Chow KM, Kassianos AP, Karekla M, et al. The role of illness perceptions, coping, and self-efficacy on adherence to precautionary measures for COVID-19. Int J Environ Res Public Health 2020, 17, 1–11. [Google Scholar] [CrossRef]
- Corea F, Folcarelli L, Napoli A, del Giudice GM, Angelillo IF. The Impact of COVID-19 Vaccination in Changing the Adherence to Preventive Measures: Evidence from Italy. Vaccines 2022, 10, 1–11. [Google Scholar] [CrossRef]
- Nikoloski Z, Bain R, Elzalabany MK, Hanna P, Aynsley TR, Samhouri D, et al. Modelling COVID-19 vaccination status and adherence to public health and social measures, Eastern Mediterranean Region and Algeria. Bull World Health Organ 2023, 101, 111–120. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud. Vigilancia de salud pública en relación con la COVID-19. Vigil Salud Pública En Relac Con La COVID-19 Orientaciones Provicionales. 2020, 1, 1–12.
- Subsecretaría de Salud Pública. Actualización de la definición de caso sospechoso, confirmado, probable, personas en alerta COVID-19 y contacto estrecho de brotes confirmados y priorizados; periodos de aislamiento; para vigilancia epidemiológica ante pandemia de COVID-19 en Chile. 2021, 2021, 15.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).