Submitted:
26 December 2023
Posted:
10 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Method
3. Results
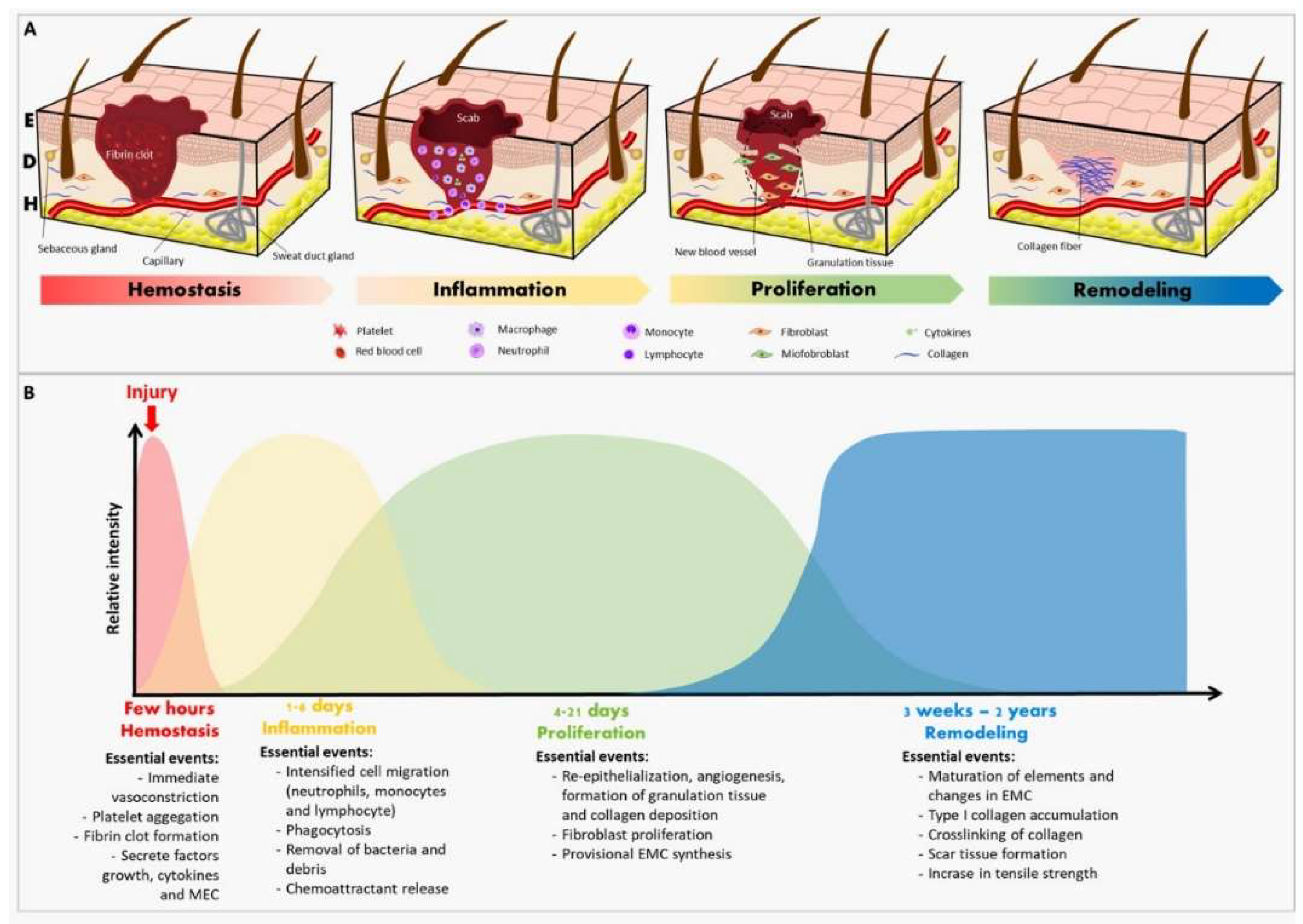
3.1. Wound healing process
3.2. Biotechnological application of natural products
3.3. Extracts from medicinal plants
3.4. Nanotechnology
3.5. Synthesis of nanoparticles
3.5.1. Physicochemical methods of production of NPs
3.5.2. Green synthesis
3.5.2.1. Green synthesis from plant extracts
3.6. Metallic nanoparticles and the wound healing
3.6.1 Silver nanoparticles (AgNPs)
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beyene, R.T; Derryberry JR, S.L.; Barbul, A. The Effect of Comorbidities on Wound Healing. Surg. Clin. North Am. 2020, 100, 4, 695-705. [CrossRef]
- Oliveira, A. et al. Therapeutic advances in wound healing. J. Dermatolog. Treat. 2022, 33, 1, 2-22. [CrossRef]
- Veith, A.P. et al. Therapeutic strategies for enhancing angiogenesis in wound healing. Adv. Drug Deliv. 2019, 146, 97-125. [CrossRef]
- Olsson, M. et al. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regener. 2019, 27, 1, 114-125. [CrossRef]
- Rodrigues, M. et al. Wound Healing: A Cellular Perspective. Physiological reviews 2019, 99, 1, 665-706. [CrossRef]
- Kushwaha, A.; Goswami, L.; Kim, B.S. Nanomaterial-Based Therapy for Wound Healing. Nanomaterials, 2022, 12, 4, 618. [CrossRef]
- Mendes, C. et al. The Use of Metallic Nanoparticles in Wound Healing: New Perspectives. Int. J. Molec. Sci. 2022, 23, 23, 15376. [CrossRef]
- Khorrami, S. et al. Selective cytotoxicity of green synthesized silver nanoparticles against the MCF-7 tumor cell line and their enhanced antioxidant and antimicrobial properties. Int. J. Nanomed. 2018, 13, 8013–8024. [CrossRef]
- Veeraraghavan, V.P. et al. Green synthesis of silver nanoparticles from aqueous extract of Scutellaria barbata and coating on the cotton fabric for antimicrobial applications and wound healing activity in fibroblast cells (L929). Saudi J. Biology. Sci. 2021, 28, 7, 3633-3640. [CrossRef]
- Raziyeva, K. et al. Immunology of Acute and Chronic Wound Healing. Biomolecules, 2021, 11, 5, 700. [CrossRef]
- Sorg, H. et al. Skin Wound Healing: An Update on the Current Knowledge and Concepts. Eur. Surg. Res. 2017, 58, 1-2, 81-94. [CrossRef]
- Kimura, S.; Tsuji, T. Mechanical and Immunological Regulation in Wound Healing and Skin Reconstruction. Int. J. Molec. Sci. 2021, 22, 11, 5474. [CrossRef]
- Lux, C.N. Wound healing in animals: a review of physiology and clinical evaluation. Vet. Dermatol. 2022, 33, 1, 91-e27. [CrossRef]
- Wang, P.-H. et al. Wound healing. J Chin Med Assoc, 2018, 81, 2, 94-101. [CrossRef]
- Wilkinson, H.N.; Hardman, M.J. Wound healing: cellular mechanisms and pathological outcomes. Open Biol. 2020, 10, 9, 200223. [CrossRef]
- Nowak, N.C. et al. Cutaneous innervation in impaired diabetic wound healing. Translational research. J. Lab. clin. Med. 2021, 236, 87-108, 2021. [CrossRef]
- Thulabandu, V.; Chen, D.; Atit, R.P. Dermal fibroblast in cutaneous development and healing. Wiley interdisciplinary reviews. Dev. Biol. 2018, 7, 2. [CrossRef]
- Li, J. et al. Regulatory T-Cells: Potential Regulator of Tissue Repair and Regeneration. Front. Immunol. 2018, 9, 585. [CrossRef]
- Zaiss, D.M. et al. Immune- and non-immune-mediated roles of regulatory T-cells during wound healing. Immunology, 2019, 157, 3, 190-197. [CrossRef]
- desJardins-Park, H.E.; Foster, D.S.; Longaker, M.T. Fibroblasts and wound healing: an update. Reg. Med. 2018, 13, 5, 491-495. [CrossRef]
- Rousselle, P.; Braye, F.; Dayan, G. Re-epithelialization of adult skin wounds: Cellular mechanisms and therapeutic strategies. Adv. Drug Del. Rev. 2019, 146, 344-365. [CrossRef]
- Blanco-Fernandez, B. et al. Nanotechnology Approaches in Chronic Wound Healing. Adv. Wound Care. 2021, 10, 5, 234–256. [CrossRef]
- Woo, K.; Santos, V.L.C.G.; Alam, T. Optimising quality of life for people with non-healing wounds. Wounds Asia, 2018, 1, 2, 18-26.
- Bhattacharya, D.; Ghosh, B.; Mukhopadhyay, M. Development of nanotechnology for advancement and application in wound healing: a review. IET nanobiotechnology 2019, 13, 8, 778–785. [CrossRef]
- Chopra, B.; Dhingra, A.K. Natural products: A lead for drug discovery and development. PTR. 2021, 35, 9, 4660-4702. [CrossRef]
- Taylor, D.M.; Werneke, U. Ethnopharmacology. Nord J Psychiatry 2018, 72, S30-S32. [CrossRef]
- Falzon, C.C.; Balabanova, A. Phytotherapy: an introduction to herbal medicine. Prim. Health Care 2017, 44, 2, 217-227. [CrossRef]
- Renard, C. Extraction of bioactives from fruit and vegetables: State of the art and perspectives. LWT-Food Sci. Technol. 2018, [s. l.], 93, 390-395. [CrossRef]
- Santos, M.O. et al. Medicinal Plants: versatility and concordance of use in the caatinga area, Northeastern Brazil. An. Acad. Bras. Cienc. 2018, 90, 3, 2767-2779. [CrossRef]
- Valli, M.; Russo, H.M.; Bolzani, V.S. The potential contribution of the natural products from Brazilian biodiversity to bioeconomy. An. Acad. Bras. Cienc. 2018, 90, 1, 763-778. [CrossRef]
- Abubakar, A.R.; Haque, M. Preparation of Medicinal Plants: Basic Extraction and Fractionation Procedures for Experimental Purposes. J. Pharm. Bioallied Sci. 2020, 12, 1, 1–10. [CrossRef]
- Hussain, M.K.; Saquib, M.; Khan, M.F. Techniques for Extraction, Isolation, and Standardization of Bio-active Compounds from Medicinal Plants. Natural Bio-active Compounds 2019, [s. l.], 2, 179–200.
- Rasul, M.G. Extraction, Isolation and Characterization of Natural Products from Medicinal Plants. IJBSAC 2018, [s. l.], 2, 6, 1-6.
- Fonmboh, D.J. et al. An Overview of Methods of Extraction, Isolation and Characterization of Natural Medicinal Plant Products in Improved Traditional Medicine Research. Asian J. Med. Res. 2020, [s. l.], 9, 2, 31-57. [CrossRef]
- Mehnath, S. et al. Biosynthesized/greensynthesized nanomaterials as potential vehicles for delivery of antibiotics/drugs. Compr. Anal. Chem. 2021, [s. l.], 94, 363-432. [CrossRef]
- Bayda, S. et al. The History of Nanoscience and Nanotechnology: From Chemical–Physical Applications to Nanomedicine. Molecules 2020, 25, 1, 112. [CrossRef]
- Garg, P. et al. Influence of Nanotechnology and the Role of Nanostructures in Biomimetic Studies and Their Potential Applications. Biomimetics 2017, 2, 2, 7. [CrossRef]
- Huynh, K.-H. et al. Synthesis, Properties, and Biological Applications of Metallic Alloy Nanoparticles. Int. J. Mol. Sci. 2020, 21, 14, 5174. [CrossRef]
- Gutiérrez-Wing, C.; Velázquez-Salazar, J.; José-Yacamán, M. Procedures for the Synthesis and Capping of Metal Nanoparticles. Methods Mol. Biol. 2020, 2118, 3-20. [CrossRef]
- Hossain, Z.; Yasmeen, F.; Komatsu, S. Nanoparticles: Synthesis, Morphophysiological Effects, and Proteomic Responses of Crop Plants. Int. J. Mol. Sci. 2020, 21, 9, 3056. [CrossRef]
- Naganthran, A. et al. Synthesis, Characterization and Biomedical Application of Silver Nanoparticles. Materiais 2022, [s. l.], 15, 2, 427. [CrossRef]
- Sadeghi-Aghbash, M.; Rahimnejad, M. Zinc Phosphate Nanoparticles: A Review on Physical, Chemical, and Biological Synthesis and their Applications. Curr. Pharm. Biotechnol. 2022, 23, n. 10, p. 1228-1244. [CrossRef]
- Xu, L. et al. Silver nanoparticles: Synthesis, medical applications and biosafety. Theranostics 2020, 10, 20, 8996–9031. [CrossRef]
- Ielo, I. et al. Synthesis, Chemical-Physical Characterization, and Biomedical Applications of Functional Gold Nanoparticles: A Review. Molecules 2021, 26, 19, 5823. [CrossRef]
- Lee, S.H.; Jun, B.-H. Silver Nanoparticles: Synthesis and Application for Nanomedicine. Int. J. Mol. Sci. 2019, 20, 4, 865. [CrossRef]
- Jara, N. et al. Photochemical Synthesis of Gold and Silver Nanoparticles—A Review. MOLEFW. 2021, 26, 15, 4585. [CrossRef]
- Kirchhoff, M.M. Topics in Green Chemistry. J. Chem. Educ. 2001, [s. l.], 78, 12, 1577. [CrossRef]
- Raveendran, P.; Fu, J.; Wallen, S.L. Completely “Green” Synthesis and Stabilization of Metal Nanoparticles. J. Am. Chem. Soc. 2003, 125, 46, 13940-13941. [CrossRef]
- Flieger, J. et al. Green Synthesis of Silver Nanoparticles Using Natural Extracts with Proven Antioxidant Activity. Molecules 2021, 26, 16, 4986. [CrossRef]
- Tiwari, S. et al. An overview of the phytosynthesis of various metal nanoparticles. 3 Biotech 2021, 11, 11, 478. [CrossRef]
- Vanlalveni, C. et al. Green synthesis of silver nanoparticles using plant extracts and their antimicrobial activities: a review of recent literature. RSC adv. 2021, 11, 5, 2804-2837. [CrossRef]
- Marslin, G. et al. Secondary Metabolites in the Green Synthesis of Metallic Nanoparticles. Materials 2018, 11, 6, 940. [CrossRef]
- Nande, A. et al. Green Synthesis of Nanomaterials Using Plant Extract: A Review. Curr. Pharm. Biotech. 2021, 22, 13, 1794-1811. [CrossRef]
- Shumail, H. et al. Review on Green Synthesis of Silver Nanoparticles through Plants. Endocr. 2021, 21, 6, 994-1007. [CrossRef]
- Nqakala, Z.B. et al. Advances in Nanotechnology towards Development of Silver Nanoparticle-Based Wound-Healing Agents. Int. J. Mol. Sci. 2021, 22, 20, 11272. [CrossRef]
- Choudhury, H. et al. Silver nanoparticles: advanced and promising technology in diabetic wound therapy. Mater. Sci. Eng. C 2020, [s. l.], 112, 110925. [CrossRef]
- Paladini, F.; Pollini, M. Antimicrobial Silver Nanoparticles for Wound Healing Application: Progress and Future Trends. Materiais 2019, 12, 16, 2540. [CrossRef]
- Boomi, P. et al. Phyto-Engineered Gold Nanoparticles (AuNPs) with Potential Antibacterial, Antioxidant, and Wound Healing Activities Under in vitro and in vivo Conditions. Int. J. Nanomed. 2020, 15, 7553-7568. [CrossRef]
- Korani, S. et al. Evaluation of Antimicrobial and Wound Healing Effects of Gold Nanoparticles Containing Abelmoschus esculentus (L.) Aqueous Extract. Bioinorg. Chem. Appl. 2021, 2021, 7019130. [CrossRef]
- Ponnanikajamideen, M.I. et al. In-Vivo Anti-Diabetic and Wound Healing Effect of Antioxidant Gold Nanoparticles Synthesized Using Insulin Plant (Chamaecostus Cuspidatus). Can. J. Diabetes 2019, 43, 2, 82-89, 2019. [CrossRef]
- Irfan, M.; Munir, H.; Ismail, H. Characterization and fabrication of zinc oxide nanoparticles by gum Acacia modesta through green chemistry and impregnation on surgical sutures to boost up the wound healing process. IJBIOMAC. 2022, 204, 466-475. [CrossRef]
- Rasha, E. et al. Biosynthesis of Zinc Oxide Nanoparticles from Acacia nilotica (L.) Extract to Overcome Carbapenem-Resistant Klebsiella Pneumoniae. Molecules 2021, 26, 7, 1919. [CrossRef]
- Ahmad, M.Z. et al. Green Synthesis of Titanium Dioxide Nanoparticles Using Ocimum sanctum Leaf Extract: In Vitro Characterization and Its Healing Efficacy in Diabetic Wounds. Molecules 2022, 27, 22, 7712. [CrossRef]
- Ahmed, H.E. et al. Green Synthesis of CeO2 Nanoparticles from the Abelmoschus esculentus Extract: Evaluation of Antioxidant, Anticancer, Antibacterial, and Wound-Healing Activities. Molecules 2021, 26, 15, 4659. [CrossRef]
- Chinnasamy, G. et al. Synthesis, Characterization, Antibacterial and Wound Healing Efficacy of Silver Nanoparticles From Azadirachta indica. Front. Microbiol. 2021, 12, 611560. [CrossRef]
- Desai, A.S. et al. An In Vitro and In Vivo Study of the Efficacy and Toxicity of Plant-Extract-Derived Silver Nanoparticles. J. Funct. Biomater. 2022, 13, 2, 54. [CrossRef]
- Chai, S.H. et al. Bio fabrication of silver nanoparticles as an effective wound healing agent in the wound care after anorectal surgery. J. Photochem. Photobiol. 2018, 178, 457-462. [CrossRef]
- Ahn, E.-Y.; Jin, H.; Park, Y. Assessing the antioxidant, cytotoxic, apoptotic and wound healing properties of silver nanoparticles green-synthesized by plant extracts. Mat. Sci. Eng. C-Mater. 2019, 101, 204-216. [CrossRef]
- Sharma, M. et al. Biofabrication and characterization of flavonoid-loaded Ag, Au, Au-Ag bimetallic nanoparticles using seed extract of the plant Madhuca longifolia for the enhancement in wound healing bio-efficacy. Prog. Biomat. 2019, 8, 1, 51-63. [CrossRef]
- Al-Shmgani, H.S.A. et al. Biosynthesis of silver nanoparticles from Catharanthus roseus leaf extract and assessing their antioxidant, antimicrobial, and woundhealing activities. Artif. Cells Nanomed. Biotechnol. 2017, 45, 6, 1-7. [CrossRef]
- Arya, G. et al. Catalytic, antibacterial and antibiofilm efficacy of biosynthesised silver nanoparticles using Prosopis juliflora leaf extract along with their wound healing potential. J. Photochem. Photobiol. 2019, 190, 50-58. [CrossRef]
- Alsareii, S.A. et al. Synthesis and Characterization of Silver Nanoparticles from Rhizophora apiculata and Studies on Their Wound Healing, Antioxidant, Anti-Inflammatory, and Cytotoxic Activity. Molecules 2022, 27, 19, 6306. [CrossRef]
- Maghimaa, M.; Alharbi, S.A. Green synthesis of silver nanoparticles from Curcuma longa L. and coating on the cotton fabrics for antimicrobial applications and wound healing activity. J. Photochem. Photobiol. 2020, 204, 111806. [CrossRef]
- Mohanta, Y.K. et al. Phyto-assisted synthesis of bio-functionalised silver nanoparticles and their potential anti-oxidant, anti-microbial and wound healing activities. IET Nanobiotech. 2017, 11, 8, 1027-1034. [CrossRef]
- Ali, S. et al. Green synthesized silver nanoparticles (AgNPs) from Parrotiopsis jacquemontiana (Decne) Rehder leaf extract and its biological activities. Microsc. Res. Techniq. 2022, 85, 1, 28-43. [CrossRef]
- Gong, C.-P.; Li, S.-C.; Wang, R.-Y. Development of biosynthesized silver nanoparticles based formulation for treating wounds during nursing care in hospitals. J. Photochem. Photobiol. 2018, 183, 137-141. [CrossRef]
- Parveen, A. et al. In vivo efficacy of biocompatible silver nanoparticles cream for empirical wound healing. J. Tissue Viability 2018, 27, 4, 257-261. [CrossRef]
- Fatima, F. et al. Green Synthesized Silver Nanoparticles Using Tridax Procumbens for Topical Application: Excision Wound Model and Histopathological Studies. Pharmaceutics 2021, 13, 11, 1754. [CrossRef]
- Lakkim, V. et al. Green Synthesis of Silver Nanoparticles and Evaluation of Their Antibacterial Activity against Multidrug-Resistant Bacteria and Wound Healing Efficacy Using a Murine Model. Antibiotics 2020, 12, 902. [CrossRef]
- Kannaiyan, S. et al. Pisonia Alba Assisted Synthesis of Nanosilver for Wound Healing Activity. Bioinorg. Chem. Appl. 2022, 2022, 1775198. [CrossRef]
- Tyavambiza, C. et al. The Antioxidant and In Vitro Wound Healing Activity of Cotyledon orbiculata Aqueous Extract and the Synthesized Biogenic Silver Nanoparticles. Int. J. Mol. Sci., 23, 24, 16094. [CrossRef]
- Ali, S.; Khan, M.R.; Khan, R. Green synthesized AgNPs from Periploca hydaspidis Falc. and its biological activities. Microsc. Res. Techniq. 2021, 84, 10, 2268-2285. [CrossRef]
| Metal | Plant | Experimental model | Phytochemicals | Methodology | Results | References |
|---|---|---|---|---|---|---|
| Gold | Acalypha indica | In vivo assay with BALB/c mice | Absent | A 20 mm wound was made on the animal’s back, treated with AuNPs and excised to histological evaluation. | AuNPs accelerated the inflammatory stage, thus initiating blood vessel formation and collagen matrix remodeling faster than in control animals. Skin regeneration and wound contraction of treated animals were also faster than the control ones. | [58] |
| Gold | Abelmoschus esculentus | In vivo assay with male Sprague Dawley adult rats | Absent | A 2cm full-thickness skin excision was performed on the animals´ back and treated for 12 days with a colloidal solution of AuNPs synthesized with fresh okra. | AuNPs increased the percentage of wound contraction in treated animals. | [59] |
| Gold | Chamaecostus cuspidatus | In vivo assay with male Wistar rats | Absent | Absent | Rats treated with AuNPs and plant extract presented a better wound healing when compared to control rats after 4 weeks of the surgery. | [60] |
| Zinc | Acacia modesta | In vivo assay with Sprague Dawley rats | Absent | The wounds were performed on surgical sutures and treated with zinc oxide nanoparticles (ZnO-NPs). | Treated rats demonstrated a rapid rate of epithelialization, faster wound contraction, mild inflammation, and absence of infection at the wound site. Histopathology showed increased collagen fibers, fibroblastic cells, lower inflammatory cells, and rapid angiogenesis when compared to the standard surgical treatment. | [61] |
| Zinc | Acacia nilotica | In vivo assay with rats | Absent | A 2cm skin excision was performed on the animal’s back. KPC infection was induced by inoculation of 20 μL of KPC bacterial suspension (CFU 108) on the day of surgery (day 0). On day 3, the treatment based on an ointment containing the synthesized ZnO-NPs was started. | On the 14th day after surgery, the infected and uninfected control animals presented 63% and 64% of wound contraction, respectively, while the infected animals treated with the ointment based on imipenem presented 54% of contraction. Infected animals treated with ZnO-NPs presented a higher value of 98%. | [62] |
| Titanium | Ocimum sanctum | In vivo assay with diabetic male albino Wistar rats | Alkaloid, flavonoids, saponins, tannins, terpenoids, steroids, phenols, anthraquinones, proteins, and carbohydrates | A dorsal excision was performed on animals´ back and treated with chitosan gel containing TiO2 NPs. The analysis of wound area contraction, the epithelialization time, and the wound closure time. Were also evaluated. | Animals treated with the gel containing TiO2 NPs presented a faster (p<0.05) epithelialization when compared to the animals treated with the chitosan gel. | [63] |
| Cerium |
Abelmoschus esculentus |
In vivo assay with male albino rats | Absent | Rat skin incisions were performed and treated with chitosan hydrogel membrane loaded with 1% and 5% cerium nanoparticles | Animals treated with cerium nanoparticles presented a maximum wound contraction, while the group treated with the chitosan membrane had a visibly larger wound size. | [64] |
| Plant | Experimental model | Phytochemicals | Methodology | Results | References |
|---|---|---|---|---|---|
| Azadirachta indica | In vivo assay with adult male albino mice | Flavonoids, phenolics, terpenoids, and terpenes. | Wounds treated with AI-AgNPs (0.3, 1, and 3 mg) immobilized in the PF127 hydrogel. | Almost complete wound closure with on day 10 of the group treated with 1.0 mg AI-AgNPs-PF127 hydrogel | [65] |
| Aloe barbadensis miller and Curcuma longa | In vitro wound healing and cytotoxicity assays using human embryonic kidney cell lines (HEK-293) | Absent | Inoculation of AgNPs in cell culture. Cellular modifications were observed by using an optical microscope, while the area covered by cells was measured using Image-J software. | AgNPs with turmeric extract presented non-toxic pattern, in addition to faster and more sustained cell growth compared to other AgNPs | [66] |
| Delonix elata | In vivo treatment of anorectal wounded area in patients weighing 64 kg | Alkaloids, saponins, theroids, tannins, carotene, phenolics, anthocyanins, glycosides, flavonoids, and others. | Diary treatment with the application of cloths coated with AgNPs. The percentage of wound closure was calculated daily. | The AgNPs synthesized by the aqueous extract of the D. elata leaf presented healing properties after anorectal surgical wounds in humans. | [67] |
| Lindera strychnifolia | Cell culture in NIH3T3 cell line | Absent | Cell scraping method in NIH3T3 cells | AgNPs presented a wound closure percentage of 64% compared to the control | [68] |
| Madhuca longifolia | In vivo wound healing bioassay in Swiss albino mice | 3-hydroxy flavones, 3,6 dihydroxyflavone, dihydroquercetin, Quercetin, Myricetin 3-O-arabinoside, Myricetin 3-O-galactoside, and dihydroxyl quercetin | A 100 mm2 excision was performed and treated with paraffin-based ointment containing 70 mg/g of AgNPs. The percentage of wound closure in each case was calculated from the reduction in the wounded area | The percentage of wound closure was 80.33% for the group of ointment containing the AgNPs | [69] |
| Catharanthus roseus | In vivo assay with male albino mice using an excision wound model | Absent | A 2x2 cm2 excision was performed on the animal’s back and treated with 2 mL of the synthesized AgNP (2 mM), once a day for 12 days | Animals of the test group (treated with AgNP) presented better wound healing activity (98% of wound closure) compared to control group (85% of wound closure) | [70] |
| Prosopis juliflora | Excision wound model performed in mice | Absent | A 10 mm skin excision was performed and treated topically with an ointment containing AgNPs and Carbopol. The treatment was regular and the reduction in the wound area was measured and photographed on the 1st, 6th, 10th, and 15th days | The percentage of wound closure in animals treated with AgNPs and Carbopol was significantly higher than in the other two groups (treated only with Carbopol or povidone-iodine) | [71] |
| Rhizophora apiculata | Cell culture in murine L929 cell line | Glycosides, saponins, terpenoids, flavonoids, and phenols. | Scratch wound migration assay | AgNPs presented better potent cell migration and wound closure than the plant extract. | [72] |
| Curcuma longa L | Cell culture in murine L929 cell line | Absent | Scratch wound migration assay | AgNPs increased cell migration in the injured area, thus indicating active proliferation and growth of fibroblastic cells | [73] |
| Ardisia solanacea | Cell culture in human fibroblasts BJ-5Ta | Alkaloids, tannins, phenolic compounds, and flavonoids | Scratch wound migration assay | Authors reported a positive effect of the wound healing activity of the synthesized AgNPs | [74] |
| Parrotiopsis jacquemontiana | Skin excision in male rats | Flavonoids, tannins, coumarins, phlobatannins, steroids, phenols, alkaloids, saponins, sterols, betacyanin, vitamin C, proteins, oils, and resins | The wound area was measured in mm every 5 days, and the contraction was calculated using the measurements | The wound closure rate increased over time for all of the groups, being the values from AgNPs higher than the positive control, and these higher from the negative control. No scar formation was observed at the end of day 15 with AgNPs. | [75] |
| Euphorbia milii | Skin excision in albino male rats | Absent | A 50 mm2 dorsal excision was performed and treated with an ointment containing 10% of the synthesized AgNPs. The wound area was analyzed from the day of excision with an interval of three days until complete epithelialization | The control group presented 77.08% of wound contraction, while group I (treated with nitrofurazone ointment) presented 82.56%, and group II (treated with the AgNPs), 91.45% | [76] |
| Scutellaria barbata | Cell culture in L929 fibroblasts cell line | Absent | Scratch wound migration assay | AgNPs induced wound healing by proliferation, differentiation, and migration of L929 fibroblast cells | [9] |
| Syzygium aromaticum | In vivo assay with male and female albino rats | Absent | A dorsal excision was performed on the animal´s back and the AgNPs formulation was applied once to the wound site for 10 consecutive days until the wound was completely healed | The wound closure was achieved in 46 days and 28 days respectively for the animals treated with AgNP 3% and AgNP 5% in base cream. On day 20, the control group presented a closure rate of 94.25%, while AgNP 5% and AgNP 3% presented 98.76% and 97.06%, respectively | [77] |
| Tridax procumbens | In vivo assay with mice | Absent | A 4.5 cm2 skin excision was performed on the animals´ back and chitosan-based gel loaded with AgNPs was applied once a day until complete healing | Animals treated with AgNPs presented significant progressive healing when compared to the groups receiving negative (placebo) and standard (1% silver sulfadiazine) treatments | [78] |
|
Catharanthus roseus and Azadirachta indica |
In vivo assay with female BALB/c mice | Absent | A 5mm excision was performed on the animals´ back and treated with the formulation containing AgNPs from C. roseus or the one containing AgNPs from A. indica. Commercially available povidone-iodine ointment was used as a positive control | The wound closure rate for the AgNPs´ treatment was significantly higher (94% ± 1% for C. roseus and 87% ± 1% for A. indica) when compared to the controls (76% ± 1% for the negative and 79 % ± 1% for the positive). Wounds treated with AgNPs did not show microbial growth, bleeding, or pus formation during the experimental period, while wounds in the negative control group showed notable irritation. | [79] |
| Pisonia Alba | Cell culture of human dermal fibroblasts (HDF) | Absent | Scratch wound migration assay and analysis of cell migration in cells treated with the AgNPs. Measurements performed at 0, 24, and 48 hours of incubation | AgNPs were reported as a stimulant for collagen production and deposition in the wound site. Wound closure rates of 23.32% ± 2.29 and 17.21% ± 1.00 were observed at a concentration of 25 μg/mL after 24 h and 48 h of incubation, respectively | [80] |
| Cotyledon orbiculata | Cell culture of HaCaT, KMST-6, and CHO | Polyphenols, flavanols, tannins, and flavonols | Scratch wound migration assay with the aqueous extract of C. orbiculata and the AgNPs | C. orbiculata aqueous extract and AgNPs presented faster closure when compared to the negative control (untreated cells) in all cell lines. In HaCaT and CHO cells, AgNPs (at 2.5 µg/mL) were more efficient than the aqueous extract and the positive control (allantoin) | [81] |
| Periploca hydaspidis | In vivo assay with Sprague-Dawley rats | Tannins, flavonoids, phenols, coumarins, alkaloids, anthocyanins, saponins, glycosides, vitamin C | A cut was performed on the animal’s back and treated with the plant extract or the AgNPs | Plant extract (20%, 35%, and 75%) and AgNPs (30%, 60%, and 100%), presented a higher wound closure rate when compared to the negative control (25%, 45%, and 85%) for specific experimental days, in this case 5, 10, and 15 days, respectively | [82] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





