1. Introduction
Antibiotic misuse and overuse have resulted in the rise of drug-resistant bacteria, viruses, fungi, and parasites, which hastens the spread of illness and increases the difficulty of treating common infections [
1]. Antimicrobial resistance has a major influence on global health and it has been deemed a global health emergency by the World Health Organisation, which estimates that it could cause up to 10 million deaths annually by 2050 [
1,
2].
Misuse of antimicrobials, such as self-medication, using antibiotics in excess, and taking dosages that are too high, is thought to be a major factor in the development and spread of antimicrobial resistance [
3]. Prior research on community antibiotic usage has mostly concentrated on attitudes, beliefs, and knowledge; personality or emotions have received far less consideration [
4].
As a long-lasting general assessment, attitudes can affect the use of antibiotics. Previous research on the attitudes towards antibiotics among doctors, Pharmacist, Nurses, Biologist, chemist and the general public revealed that interventions aimed at reducing antimicrobial resistance and fostering positive attitudes towards antibiotic use could impact prescription practices as well as the way the general public uses antibiotics [
4].
Knowing the frequency of antibiotic usage in the community is helpful information for creating stewardship programmes to reduce community resistance and for better medical treatment in healthcare institutions [
5]. The immediate actions required to avoid AMR include surveillance, lowering the use of antibiotics in healthcare and agriculture, granting access to affordable, high-quality prescription drugs, immunisations, and diagnostics, as well as enforcing legal requirements. To solve this issue, collaboration between international and national organisations is necessary [
1].
There is little data on the frequency of antibiotic use in the community in Hargeisa, Somaliland. This Qualitative study was done to provide evidence-based communication intervention techniques for safer antibiotic use, know level of awareness on antibiotic use and potential risks associated with improper antibiotic use among Community live in Capital City of Somaliland Hargeisa.
2. Methods
This qualitative study was carried out in Hargeisa, Republic of Somaliland, between November 1 and December 1, 2023. There are currently no published research or formal reports outlining the usage of community antibiotics in this area.
Globally, there is an increasing need for improved disease identification and control, which has led to an expansion of diagnostic and research capabilities. However, the ability to guarantee the safe use of antibiotics has not always kept pace with the ability to identify infectious diseases, particularly in low-resource countries [
6].
Using a semi-structured interview guide, in-depth interviews were used to gather data. The authors particularly created the interview guide for this study, drawing from a review of scientific literature found on PubMed, web of science database, and Google Scholar.
The interviews, which took place one interviewer per participant, lasted an average of twenty-five minutes. The interviews took place at different places in Hargeisa, where Somali is the most widely spoken language.
A smartphone was used to digitally record each interview, which was then verbatim transcribed and translated into English. By contrasting them with the recordings, every transcript was examined for accuracy. The data was analysed using a theme analysis technique. As stated by Braun & Clarke in 2006 [
7].
3. Ethics
Before starting the interviews, we got each participant’s signed informed consent. Every participant received information on the study’s goals, confidentiality, and their freedom to refuse to answer any questions and to leave the study at any moment without facing any repercussions. Some potential subjects were not included in the study because they refused to complete the written informed consent forms.
4. Results
4.1. Knowledge of antibiotics uses for community in Hargeisa Somaliland
Overall, 20 respondents (households) were interviewed to assess the level of awareness on antibiotic use (
Table 1). Of these, 17 (85%) of the respondents became aware of the term of antibiotic itself were 7 (35%) are prescribed by physician, of these 9(45%) respondents are get laboratory diagnosis when they are using antibiotics, out of 6 (30%) of the respondents were aware of the potential risks associated with improper use of antibiotics.
4.2. Demographic description of participants
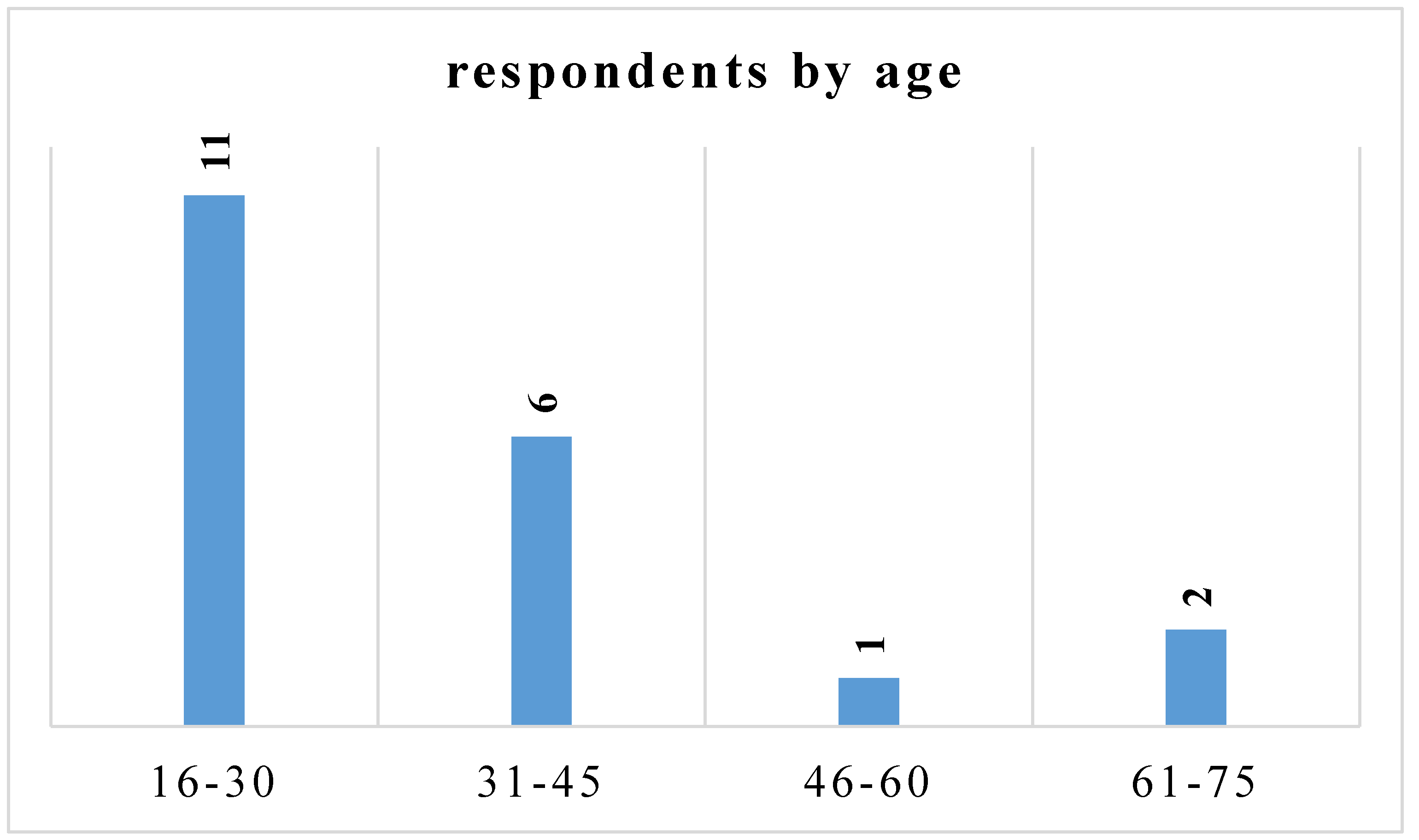
Twenty people in all were questioned, with the majority of participants (55%) being between the ages of 16 and 30. Those in the 31–45 age range came next (30%).
Figure 1.
Age Distribution of participants.
Figure 1.
Age Distribution of participants.
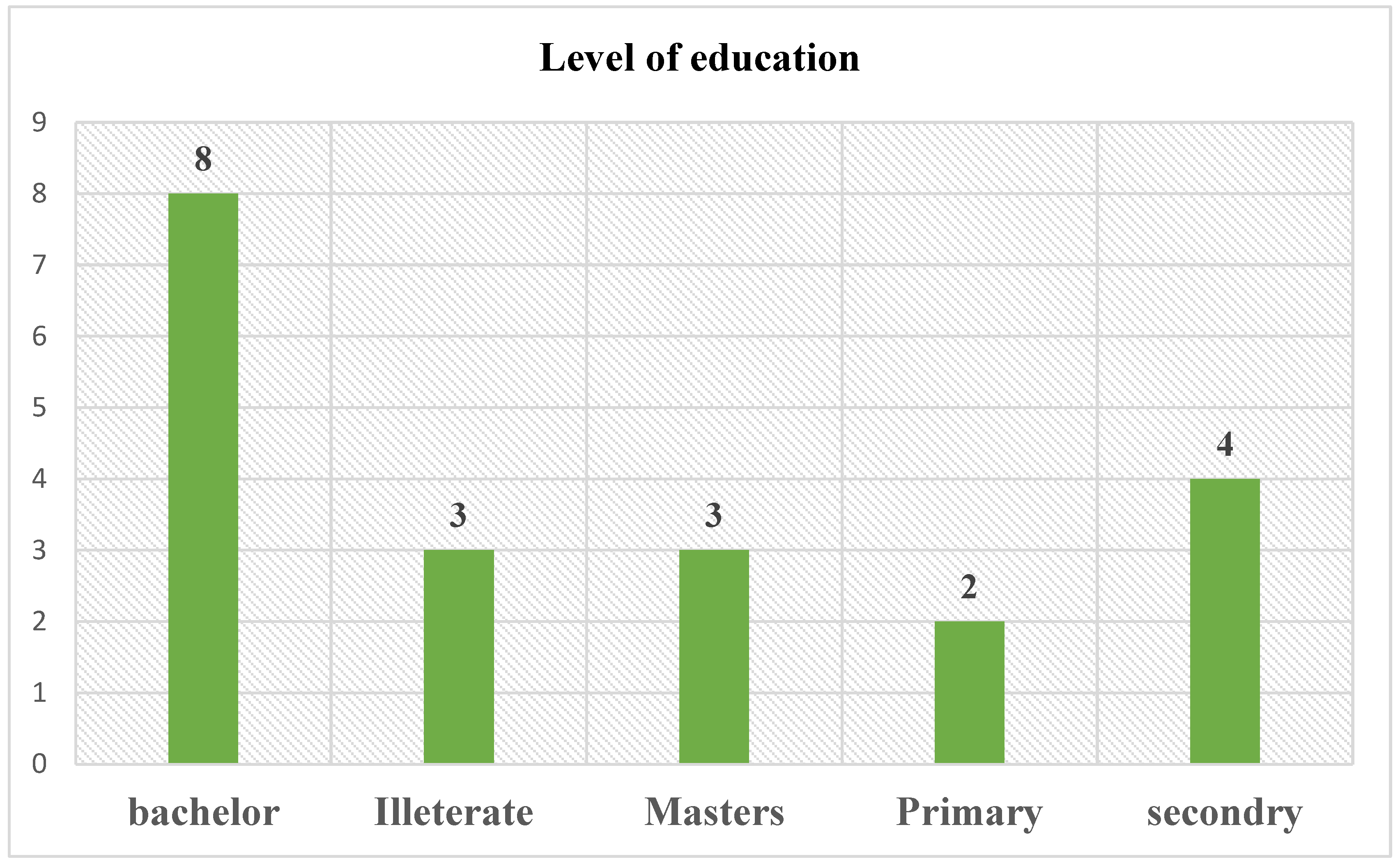
Among total number of participants 8(40%) had bachelor level of education, 3 (15%) had a master level and 4 (20%) about completed at least secondary school, while 3 (15%) did not attend school.
Figure 2.
Participants Level of Education.
Figure 2.
Participants Level of Education.
4.3. Knowledge and use of antibiotics
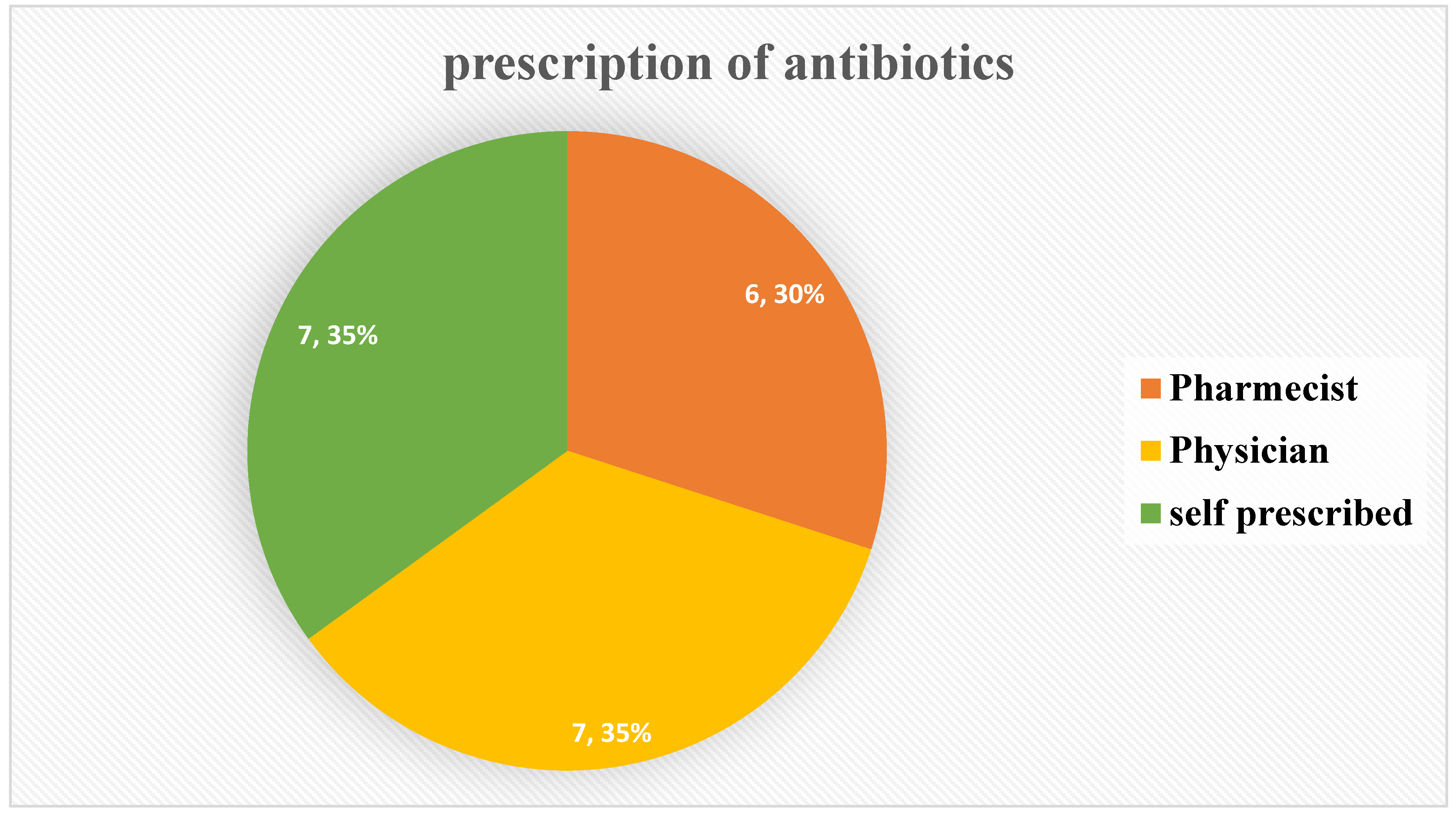
Despite being aware that antibiotics were only available with a prescription, a 7.35% percentage of respondents continued to obtain antibiotics without physician prescription. Around 7.35% which was equal proportion with that of self-prescription follow standard guideline for antibiotic use, which is physician prescription. While about 6.30% prescribed by pharmacist and other professional.
Figure 3.
Professional participated in Antibiotic prescription.
Figure 3.
Professional participated in Antibiotic prescription.
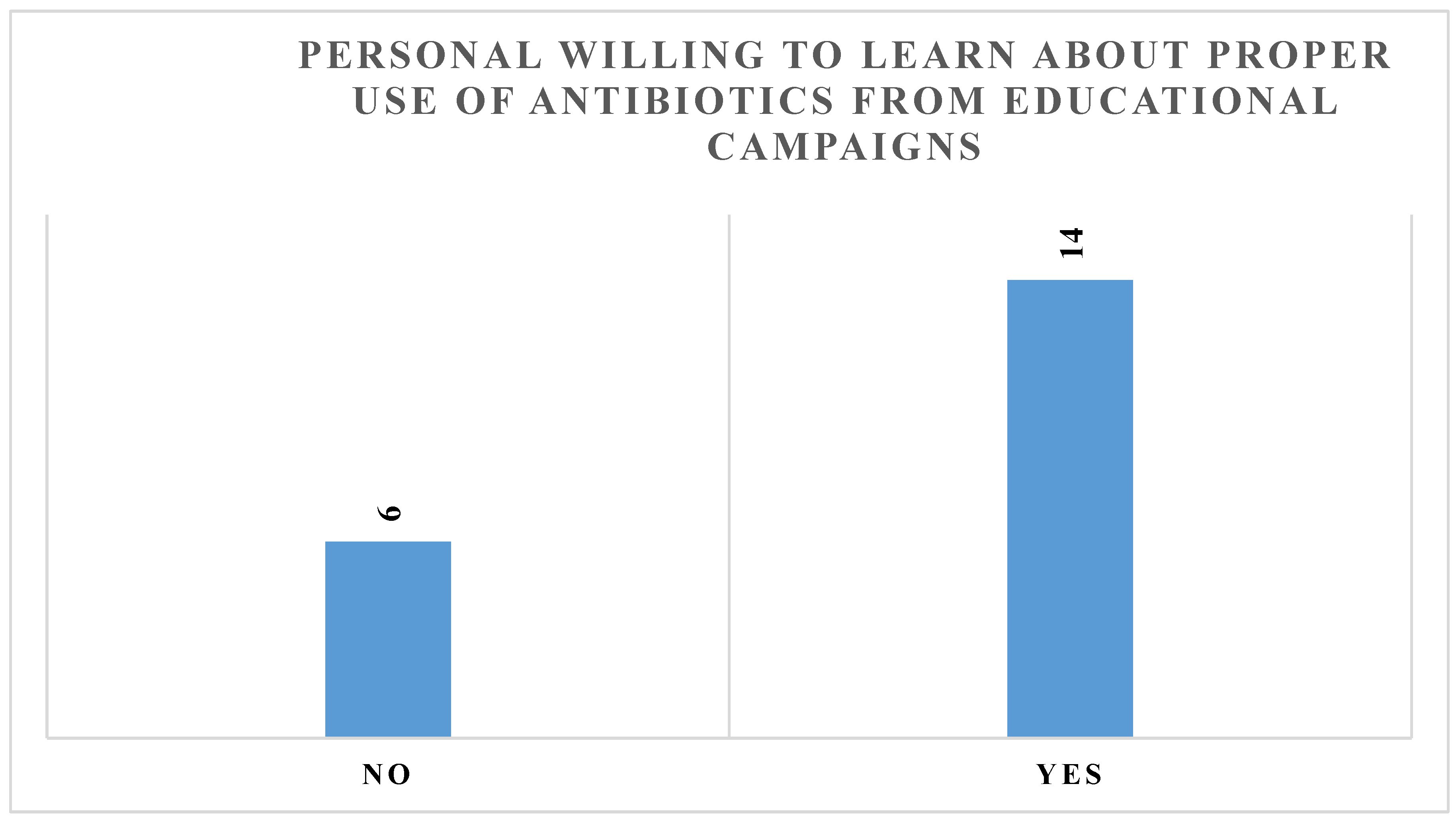
Figure 4.
Show Community need assessment about Awareness creation Education.
Figure 4.
Show Community need assessment about Awareness creation Education.
Most of the participants which was around 70% of the total participants need awareness creation or health education campaign about antibiotic use from health professionals.
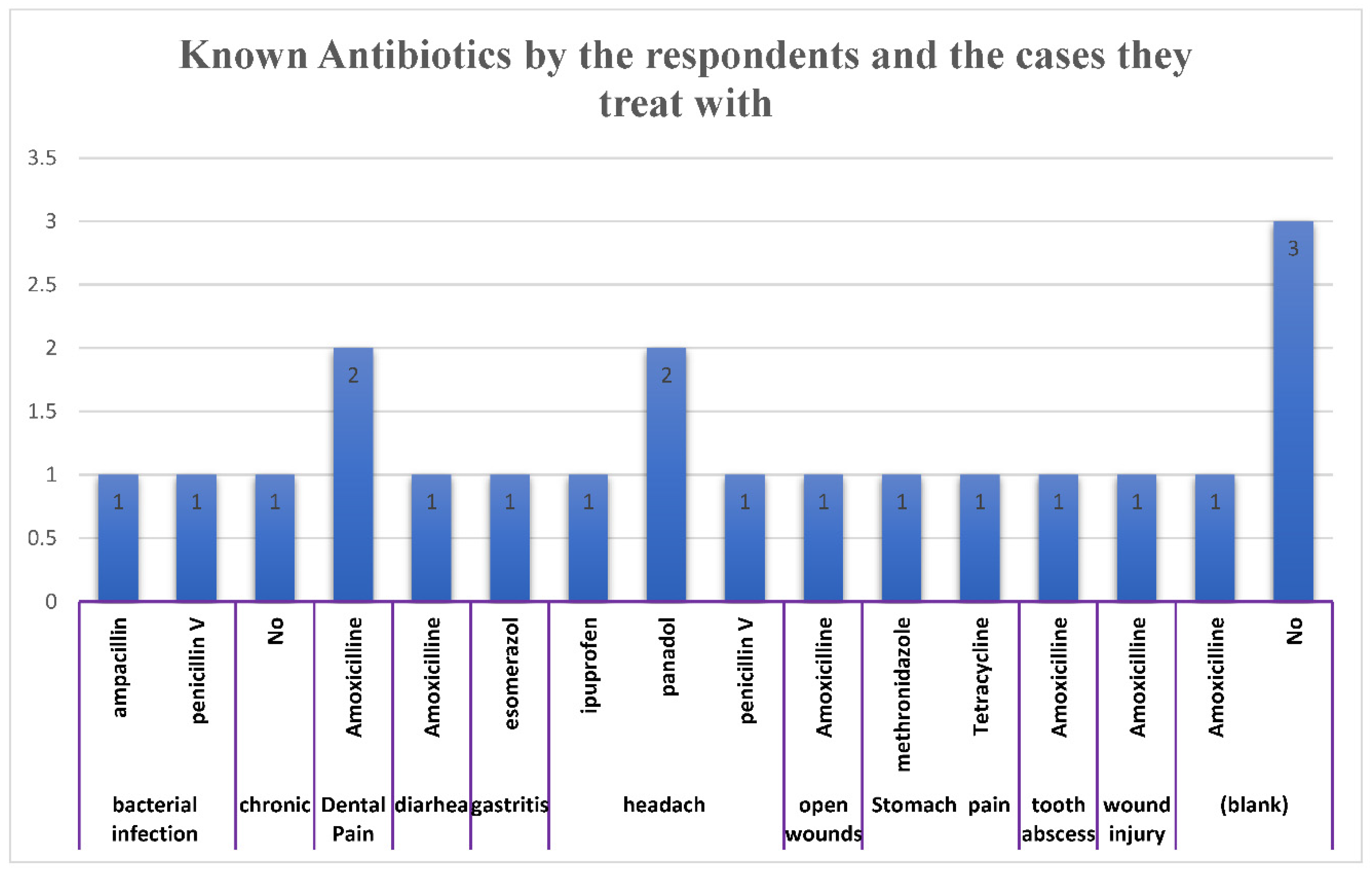
4.4. Antibiotic types and Disease Used for by Community
Every participant stated that they had given or taken antibiotics to a household member or themselves. Antibiotics such as amoxicillin, ampicillin, ciprofloxacin, and tetracycline could be cited by the participants.
The participants indicated a range of signs and symptoms of infection for which they utilised antibiotics. These included bacterial infection, dental pain, headache, unknown fever and wound infection.
Figure 5.
Antibiotic and type of diseases used for.
Figure 5.
Antibiotic and type of diseases used for.
4.5. Antibiotic risks
Relying on participant responses, we found various sources that recommend the usage of antibiotics. The following were listed in priority order: self-medication, advice from non-medical family members, chemists or drugstore salespeople, nurses, and physicians. Additionally, nurses were mentioned as significant contributors to the community’s antibiotic prescription practice.
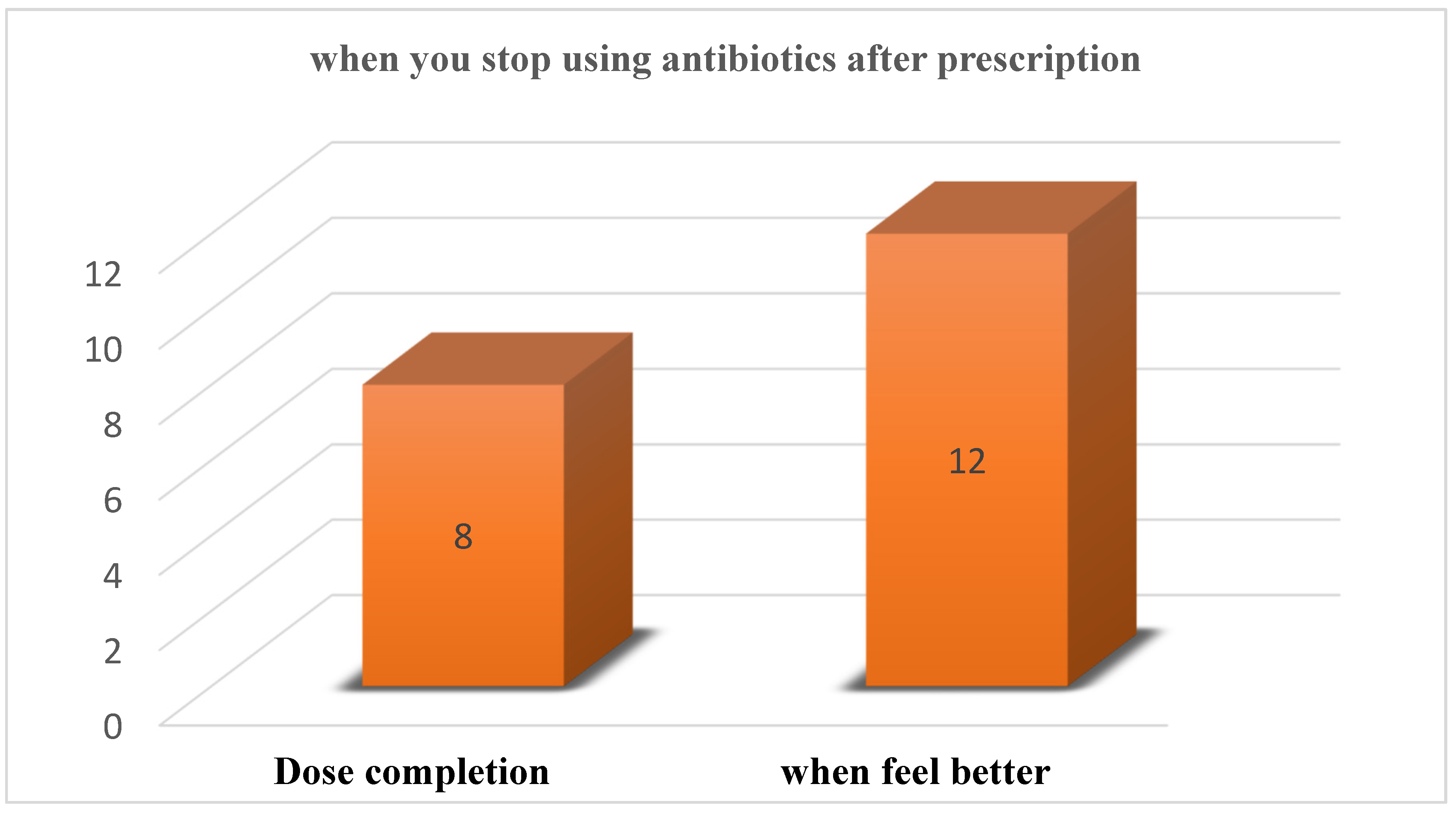
The quality of the medications on the market worried the participants. Some reported using medications they believed to be less effective because of low concentrations of the active ingredient in the medication or buying antibiotics with manipulated expiration dates. The end of treatment was frequently dependent upon the resolution of the symptoms:
Figure 6.
show Antibiotic risk.
Figure 6.
show Antibiotic risk.
5. Discussion
In Hargeisa, the Republic of Somaliland, this is the first qualitative study looking into community understanding of antibiotics and practices surrounding antibiotic use. Overall, the results of this study demonstrated the widespread inappropriate use of antibiotics, which can be attributed to a variety of factors such as a lack of knowledge about the risks and indications of antibiotics, easier access to antibiotics, self-medication using over-the-counter medications or prescriptions written by unqualified individuals (such as relatives, nurses or pharmacy outlet salespeople), participant perceptions of their increased risk of infection due to living conditions and environments.
The increasing demand for improved disease detection and control on a worldwide scale has led to an expansion in the capacity for diagnosis and research. However, the ability to detect infectious diseases has not always grown in tandem with the ability to maintain biosafety and biosecurity, particularly in low-resource countries. Many barriers seriously obstruct the development or expansion of sustainable capacity in biosafety and biosecurity management in Africa and other low-resource nations [
6]. The majority of survey participants knew what a “antibiotic” was, but they didn’t know much about the dangers and indications of using pharmaceuticals. It was not well known among the participants that antibiotics were useless against viral infections.
The abuse and misuse of antibiotics has led to the rise of drug-resistant fungi, viruses, bacteria, and parasites, which speeds up the spread of disease and makes common infections more difficult to treat. Antimicrobial resistance is a global health problem, according to the World Health Organisation, which has stated that it might cause up to 10 million deaths annually by the year 2050. The World Health Organisation lists the rise of antibiotic resistance as one of the biggest threats to food security, development, and global health today [
8].
One factor that leads to the improper use of antibiotics is lack of awareness. Afari-Asiedu et al. discovered that stomach-aches and body sores were being treated with antibiotics in Ghana [
3]. The majority of participants in our survey were not aware that improper use of antibiotics could result in antibacterial resistance, and there was a low level of awareness of the hazards associated with antibiotics. One of the main reasons for the incorrect use of antibiotics was the increased perceived danger of infections.
The incorrect use of antibiotics along with numerous other factors accelerate the global development of antibiotic resistance, even though it can develop spontaneously. Often called the “Silent Pandemic,” antimicrobial resistance is an issue that needs to be addressed right now and managed more skilfully rather than being written off as a predicament for the future [
6,
8].
7. Conclusion and Recommendations
The majority of survey participants knew what an “antibiotic” was, but they didn’t know much about the dangers and indications of using pharmaceuticals. It was not well known among the participants that antibiotics were useless against viral, bacterial and fungal infections infections.
Antibiotic abuse is undoubtedly one of the main causes of antimicrobial resistance (AMR), but there are other factors in action as well. Globally, the usage of antibiotics increased by 65% in 2000 and 2015, primarily as a result of a notable increase in LMICs. It was estimated that 4.95 million deaths globally would result from drug-resistant diseases in 2019, with the majority of the clinical burden falling on low- and middle-income countries (LMICs), especially in Sub-Saharan Africa [
8].
The advantage of this study is that it is the first to examine the improper use of antibiotics in the Hargeisa Somaliland. The inappropriate usage of antibiotics requires more research to strengthen the body of data supporting this claim.
Funding
No funding was received for this work.
Conflicts of Interest
The authors declares no conflict of interest.
References
- Mahammed Abdi, A.; et al. Antimicrobial Resistance Impact in Global Health: A One Health Approach. 2023.
- Tang, K.W.K.; Millar, B.C.; Moore, J.E. Antimicrobial resistance (AMR). British Journal of Biomedical Science 2023, 80, 11387. [Google Scholar] [CrossRef] [PubMed]
- Shembo, A.K.P. A qualitative study on community use of antibiotics in Kinshasa, democratic Republic of Congo. PLoS ONE 2022, 17(4), e0267544. [Google Scholar] [CrossRef] [PubMed]
- Gaygısız, Ü.; Lajunen, T.; Gaygısız, E. Community use of antibiotics in Turkey: the role of knowledge, beliefs, attitudes, and health anxiety. Antibiotics 2021, 10(10), 1171. [Google Scholar] [CrossRef] [PubMed]
- Saito, N.; et al. Frequent community use of antibiotics among a low-economic status population in Manila, the Philippines: a prospective assessment using a urine antibiotic bioassay. The American journal of tropical medicine and hygiene 2018, 98(5), 1512. [Google Scholar] [CrossRef]
- Abdi, A.M.; Abdiweli, S.A.; Sheban, H.; Abdale, A.; Sead, H.; Hussein, M.; Mohamed, Z.; Dayib, M.; Kosar, H. Biosafety and Biosecurity in Africa: Challenges and Future Perspectives. Preprint 2024. [Google Scholar]
- Horumpende, P.G.; et al. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: A simulated clients approach. PLoS ONE 2018, 13(11), e0207465. [Google Scholar] [CrossRef] [PubMed]
- Am, A.; et al. Antimicrobial Resistance Impact in Global Health: A One Health Approach. 2023.
Table 1.
Knowledge of antibiotics uses for community in the study area.
Table 1.
Knowledge of antibiotics uses for community in the study area.
Knowledge examined
in Questionnaire
|
Number
interviewed
|
Response (%) |
| Dou you Know about antibiotics |
20 |
17 (85%) |
| Who prescribes of antibiotics |
20 |
7 (35%) |
| Do you get laboratory diagnosis |
20 |
9 (45%) |
| Do you consult infectious Diseases expert. |
20 |
7 (35%) |
| At what time do you stop antibiotics usage |
20 |
8 (40%) |
| Know the potential risks associated with improper antibiotic usage. |
20 |
6 (30%) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).